Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
Definition:
Inability of a couple to conceive after one year of regular unprotected intercourse.
It affects about 15% of couples
40% are due male cause, 40% due to female cause, and 20% combined
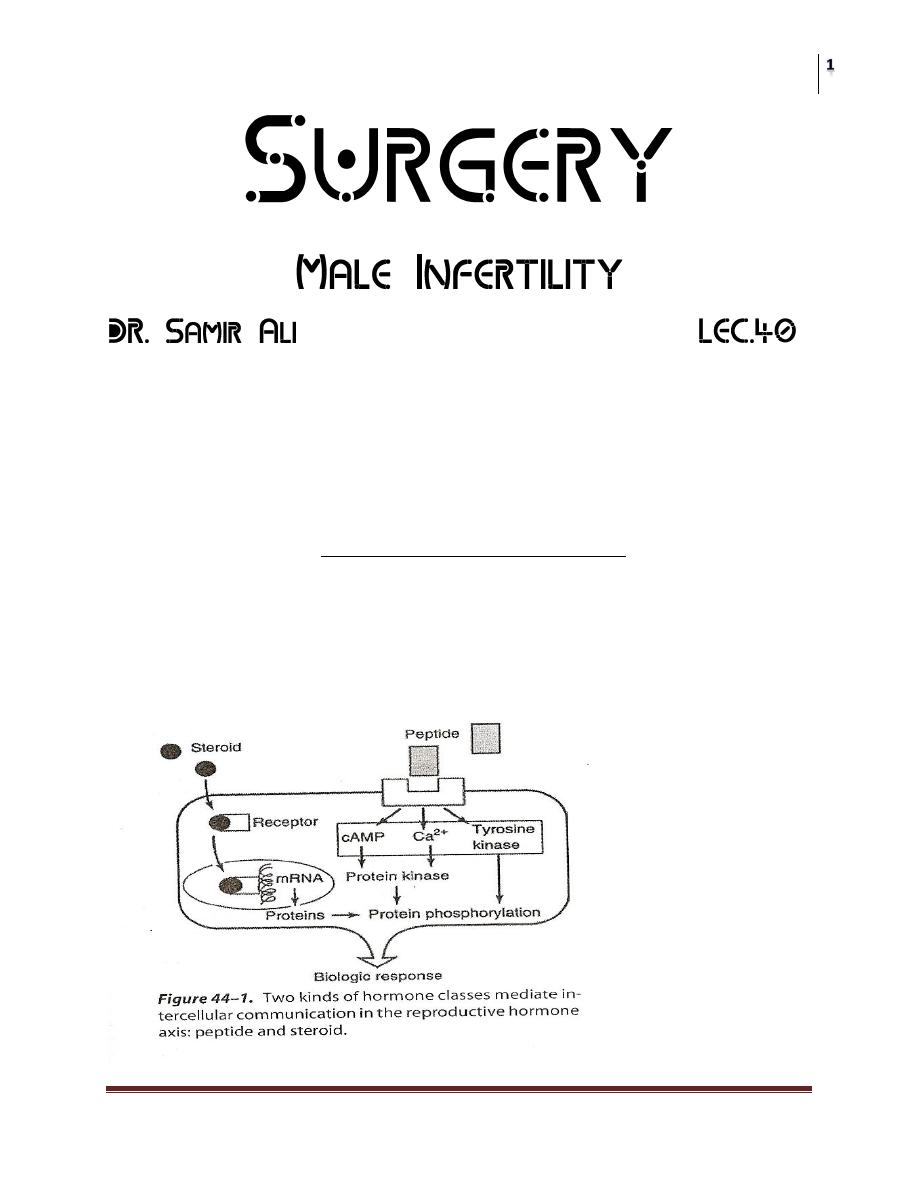
Male reproductive physiology
• The physiology of hypothalamic-pituitary-gonadal axis plays the critical
role.
• Hormone classes:
Peptides (LH, FSH): act via cell wall receptors.
Steroids (testosterone): are lipophilic so act directly on the
nucleus.
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
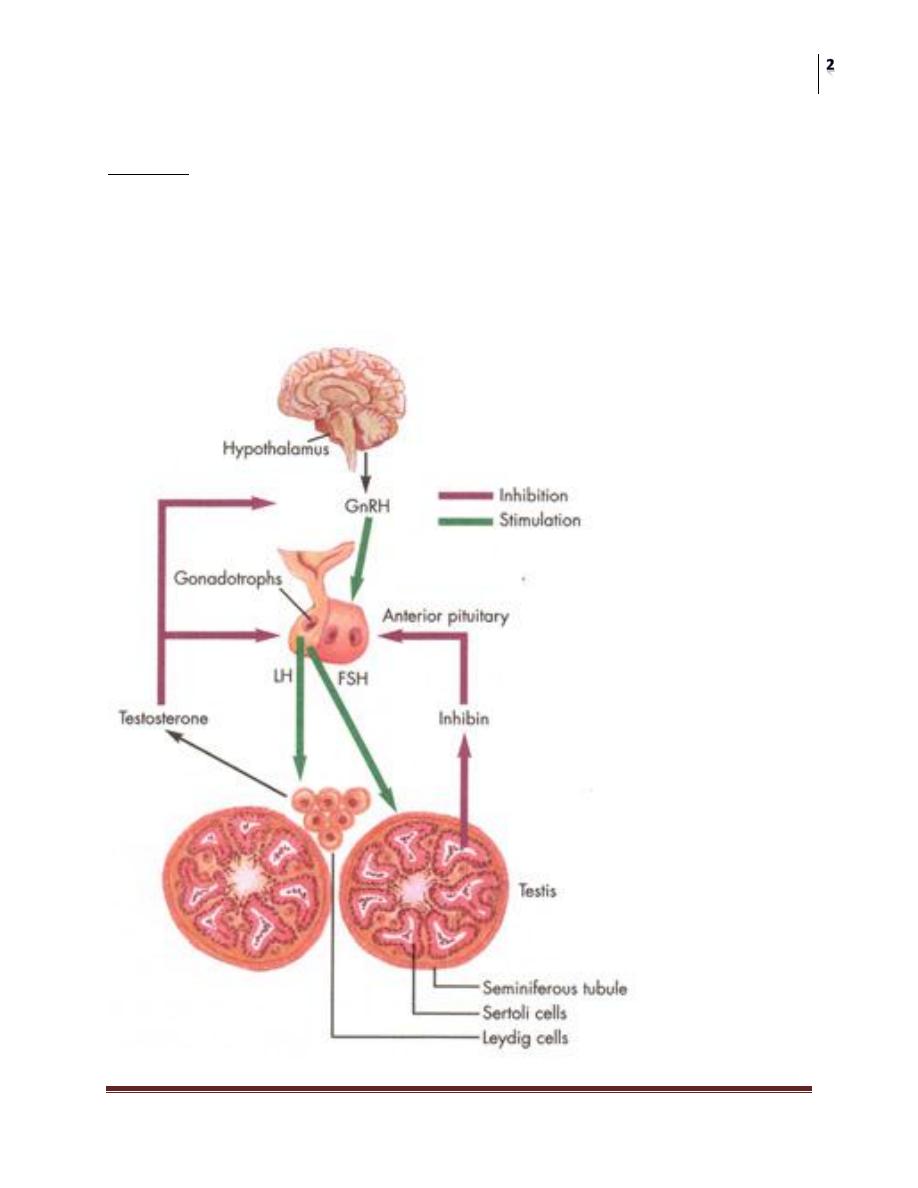
Feedback Loops
Feedback is the principal mechanism that regulate the production of various
hormones, with feedback, a hormone can regulate the synthesis and action of itself
and of other hormones.
A negative feedback is the main regulator of hormones in the HPG axis.
The HPG axis
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
Components of the HPG axis
Hypothalamus:
• Is the pulse generator for the cyclical secretion of the pituitary and gonadal
hormones.
• The most important hormone produced is GnRH (LHRH), which stimulates
the production of both LH, and FSH from the anterior pituitary.
• LHRH produced in a pulsatile manner which governs the concomitant cyclic
release of gonadotropins.
Anterior Pituitary:
• Is the site of action of LHRH, which stimulates release of LH, and FSH.
• They are glycoproteins composed of 2 peptides, α&β.
The α subunit is identical.
The β subunit is unique and responsible for the biological
action.
• LH stimulates steroidogenesis in Leydig cells. (production of testosterone)
• FSH binds to Sertoli cells and spermatogonial membrane and stimulates
semineferous tubules growth during development.
• it is essential for
initiation of spermatogenesis at puberty
Maintenance normal levels of sperm production in adults.
• Another hormone of anterior pituitary is PROLACTIN, which important for
lactating women, and although its function is not known in males, abnormal
high level may abolish gonadotropin pulsatile pattern because of the
common α subunit
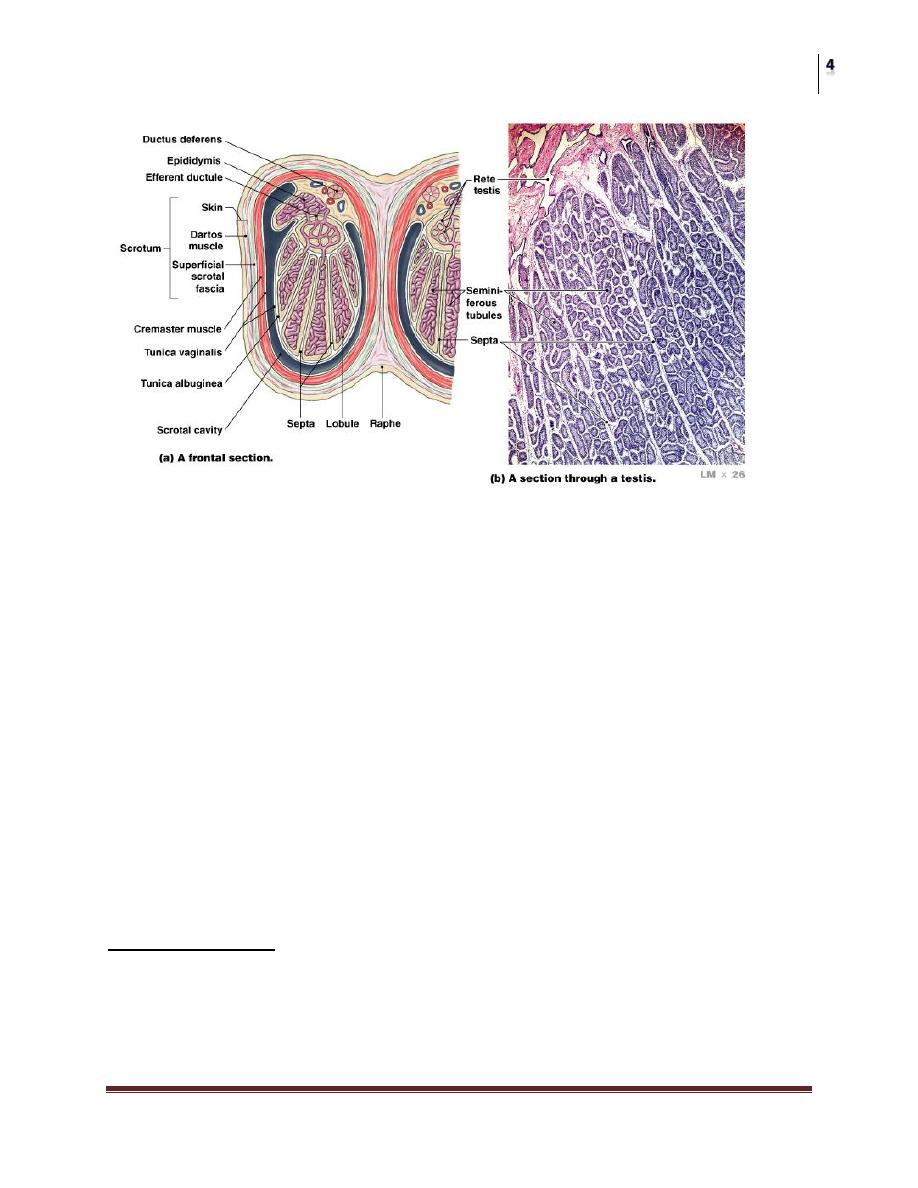
The testis
Is composed of
endocrine part (Lyedig cells)
exocrine part (seminiferous tubules)
Both under direct control of HPG axis.
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
Endocrine testis:
Responsible for testosterone production by Lyedig cells.
Only 2% of testosterone is free (unbound), and active, while the rest is
bound to either albumin or SHBG.
Testosterone is either metabolized by 5α-reductase into DHT, the
potent androgen, or by aromatase into estradiol.
Exocrine testis:
On FSH stimulation, Sertoli cells make a host of secretory
products important for germ cell growth, including androgen-
binding protein.
Through these actions seminiferous tubule growth is stimulated
during development, and sperm production is initiated during
puberty as well as a normal level of spermatogenesis is
maintained in adults.
Spermatogenesis
• Occurs in semineferous tubules
• Sertoli cells line semineferous tubules and divide them into luminal and
adluminal compartments, and function as a”nurse” norishing germ cells as
they grow.

Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
• This arrangement forms the basis of blood testis barrier.
• This allows the spermatogenesis to occur in an immunologically privileged
site.
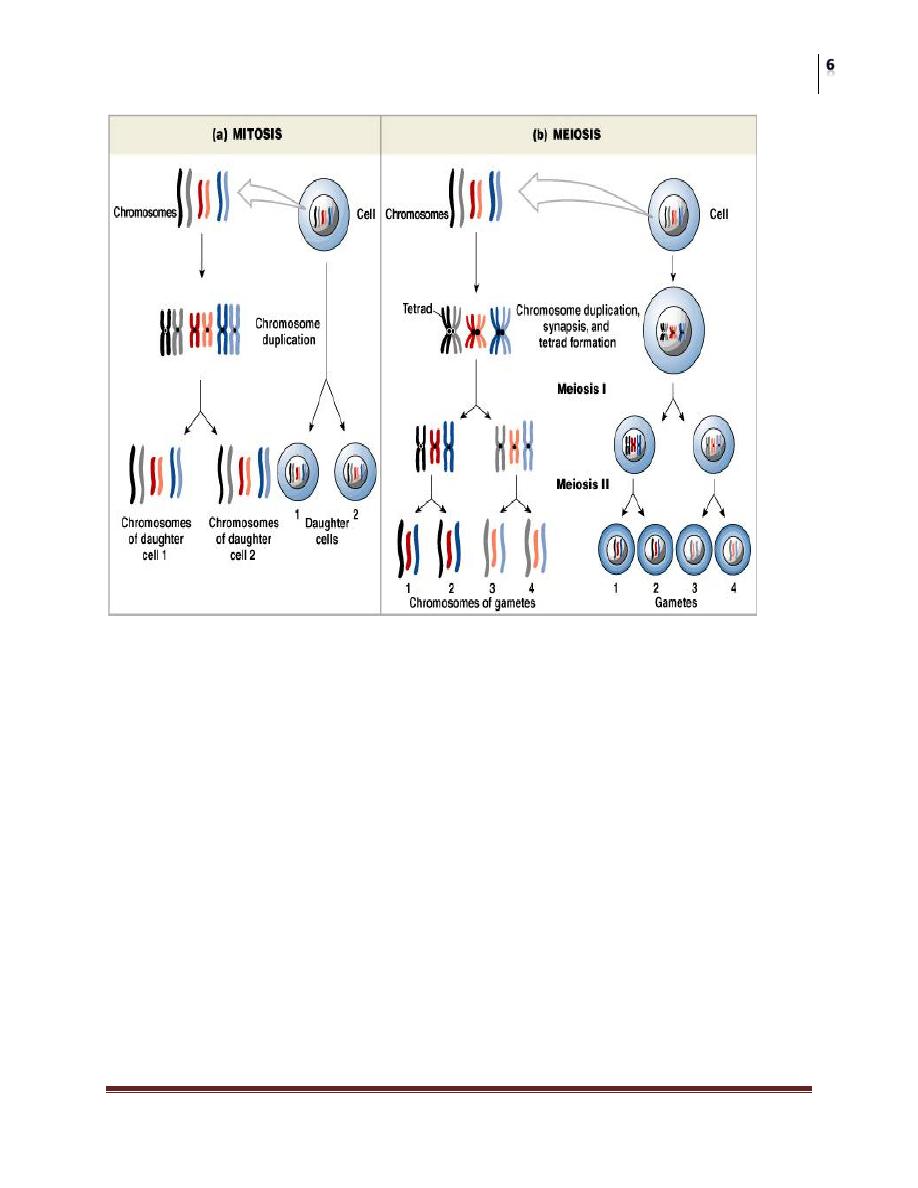
• Germ cells replicate by meiosis, in which the genetic material is halved to
allow for reproduction.
• The essential difference between mitotic and meiotic replication is that a
single DNA duplication is only one cell division in mitosis but 2 cell
divisions in meiosis, as a result daughter contains only half of the
chromosomes contained in the parent cell.
• Spermatogonia(2n) mitosis primary spermatocyte(2n) 1
st
meiosis
secondary spermatocyte(2n) 2
nd
meiosis spermatid(1n)
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
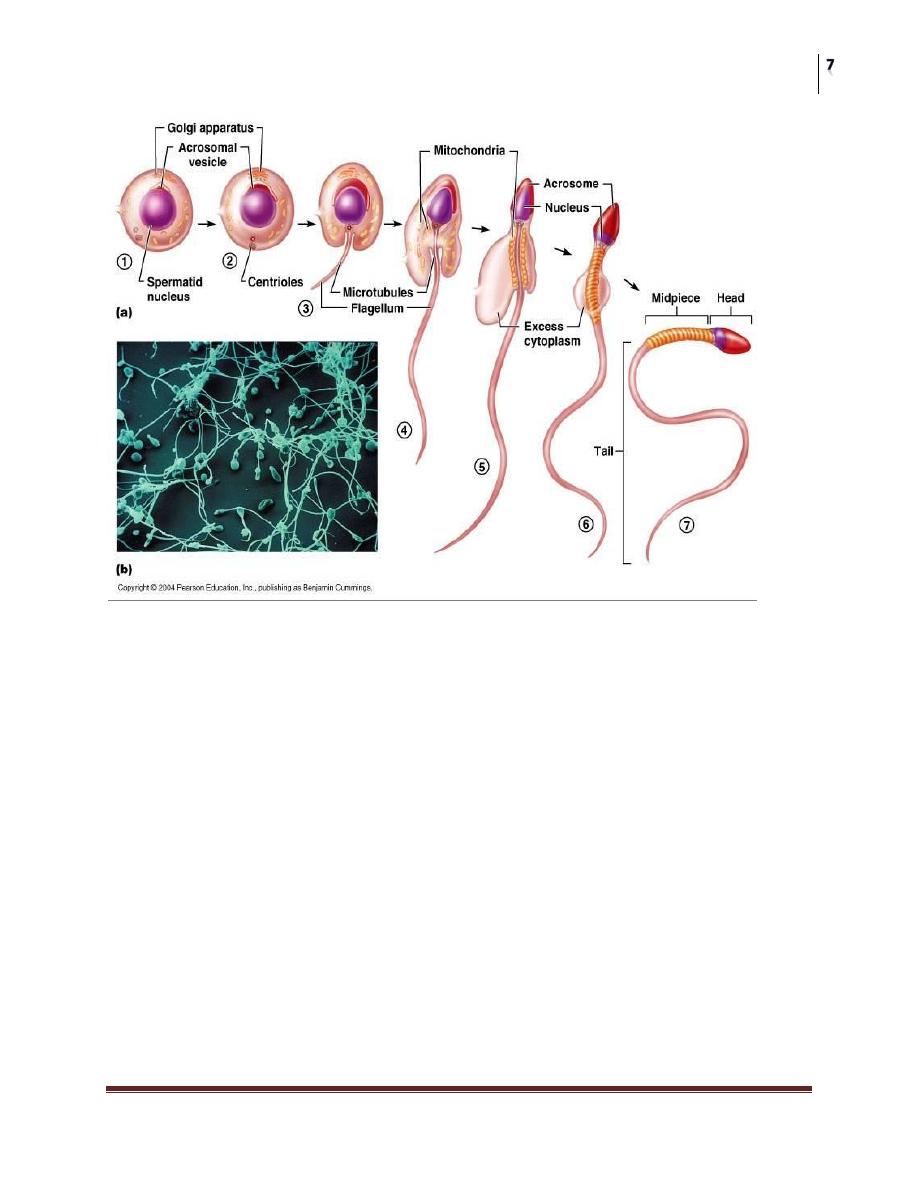
The process by which spermatids become mature spermatozoa is termed
spermiogenesis, which may take several weeks, and involves:
The acrosome is formed from Golgi complex
A flagellum is constructed from the centriole
Mitochondria reorganize around the midpiece
The nucleus is compacted to 10% of its original size
Residual cell cytoplasm is eliminated
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
• Spermatozoa within the testis have very poor or no motility and are
incapable of naturally fertilizing an egg.
• They become functional only after traversing the epididymis(10-15 days)
where further maturation occurs
• Fertilization which normally occurs in the ampullary part of the fallopian
tube requires further maturation stages that take part in the female genital
tract, called “capacitation”.
• This includes a change in the type of flagellar movement and release of lytic
enzymes from the acrosome.
Diagnosis Of Male Infertility
It is important to evaluate both partners in parallel.
If the couple are presented before one year, try to reassure them and advice them
on healthy productive sex.
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
History:
Duration of infertility
Earlier pregnancies with present of previous partner
Sexual history, timing and use of lubricants
General medical and surgical history (fever, hernial repair)
Childhood diseases as mumps
Cryptorchidism
Exposure to medications, and chemicals (anabolic steroids, pesticides)
Family history of infertility
Physical examination:
Degree of virilization
Gynecomastia
Testicular size and consistancy
Status of epididymis
Vas deferens
Varicocele
Penis and prostate
Lab investigations
• GUE: may find infection, hemturia, glycoseuria….etc
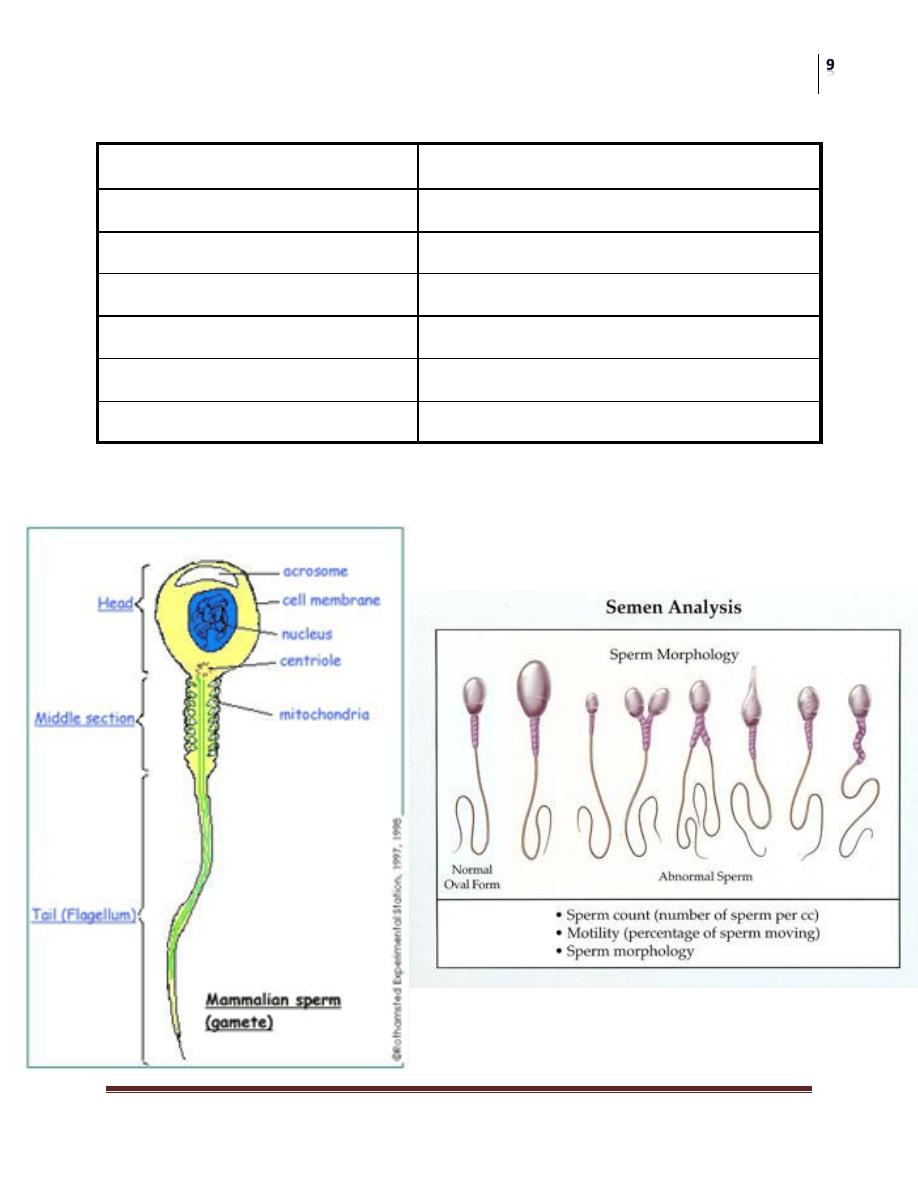
• Semen analysis: is the primary source of information on sperm production
and reproductive tract patency.
– Sample collection: semen quality vary in the same person from day
to day, the result depends greatly on collection technique. It should be
collected after a period of abstinence of 48-72 hours, the sample
should be examined within one hours, 2 samples should be taken as a
baseline, one month apart.
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
Physical characteristics of semen
Liquefaction time
15-30 min
Ejaculate vol.
1.5-5 ml
Sperm conc.
>20 millions/ml
Motility
>50%
Forward progression
2 (scale 1-4)
morphology
>30% WHO normal forms
Sperm agglutination
<2 (scale 0-3)
Sperm morphology

Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
Other semen parameters:
Fructose: if absent, seminal vesicle agenesis or obstruction of
ejaculatory ducts may be the cause.
Post ejaculate urine analysis for semen: to look for retrograde
ejaculation
Hormonal assessment:
To evaluate the HPG axis
LH, FSH, testosterone, and prolactine are assessed
Estradiol is reserved for underanderogenized males or with gynecomastia
Indications:
Low sperm count<10million/ml
Impairment of sexual function (impotence, low libido)
Other endocrinopathy (thyroid dis.)
Adjunctive tests
Semen leukocyte analysis: pyospermia is defined as >1million leukocytes /ml,
should be differentiated from round cells of immature sperms by esterase test
Antisperm antibody test: should be obtained when:
Sperm agglutination or clumping
Low sperm motility+history of testis surgery/trauma
Increased leukocyte count
Unexplained infertility
Hypoosmotic swelling: to differentiate immotile but live sperms from dead ones,
and can be used for assisted fertility techniques.
sperm chromatin structure, and chromosomal studies: to detect genetic
abnormalities
Cystic fibrosis testing: related to absent vas, and ideopathic obstruction
Radiological tests
• Scrotal US, Doppler
• Venography
• TRUS

Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
Testis biopsy
• Provides direct information about spermatogenesis.
• Usually used for azospermic patients in which it is difficult to distinguish
between failure of sperm production and obstruction.
• Now used for recovery of sperms for ICSI.
CAUSES OF MALE INFERTILITY
Pretesticular
Testicular
posttesticular
Pretesticular causes
• Hypothalamic disease:
Gonadotropin deficiency “kallmann syndrome”:
familial, x linked or autosomal,
due to disturbance of neuronal migration from the olfactory
placode which contain neurons responsible for both olfaction
and LH release.
The patient complains of hypogonadism and anosmia.
Pituitary disease:
Pituitary insufficiency: tumors, infarcts, radiation
Hyperprolactinemia: either secondary to stress, medications,
and systemic disease, or due pituitary adenoma. High prolactin
induces a negative feedback on gonadotropin secretion.
Exogenous and endogenous hormones: androgens, estrogens,
thyroid hormones, or corticosteroid.
Testicular Causes
A. Chromosomal causes
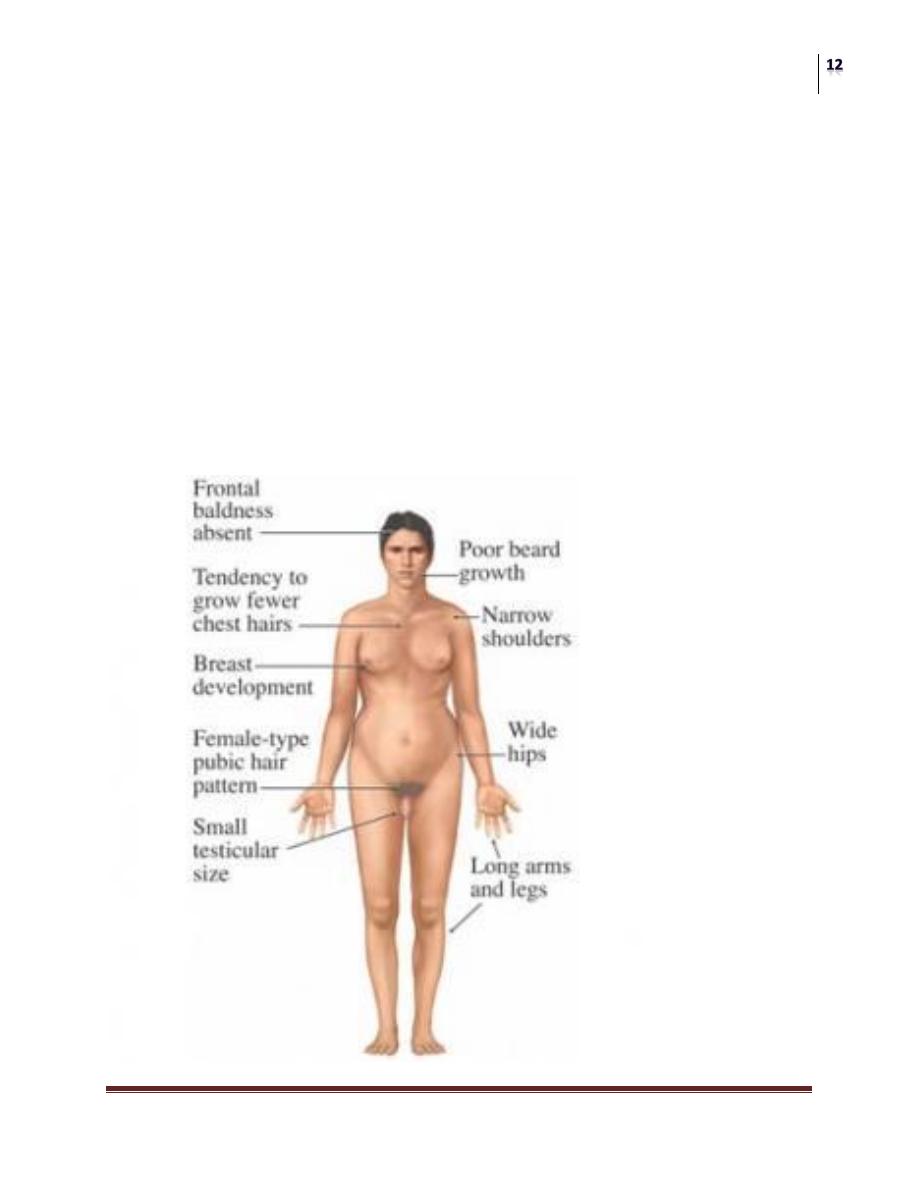
Klinefelter syndrome (47XXY):
the most common genetic cause for azospermia.
classic triad of small firm testis, gynecomastia and azospermia.
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
They have delayed sexual maturation, increased height, obesity
and diabetes.
Increased malignancy risk by 20 folds.
Sertoli cell only syndrome:
azospermic men with testicular biopsy show absence of
germinal epithelium.
The patients have normal virilization, with small testis with
normal consistency.
There is no gynecomastia

Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
B. Gonadotoxins:
Radiation
Drugs: ca
+2
channel blockers, allopurinol, cimitidine,
spironolactone, alpha blockers, TCA
Liver cirrhosis: increased s. estrogen causes testicular atrophy,
gynecomastia, and impotence.
C. Defective androgen activity
5 α reductase deficiency: causes normal internal genitalia, but
ambiguous external genitalia as hypospadias, and
cryptorchidism.
Androgen receptor deficiency: no receptor for DHT to bind, so
no action, in turn both the internal and external genitalia are
affected.
D. Testis injury:
Orchitis e.g mumps
Torsion and ischemic injury
Trauma cause either fibrosis or immune infertility
E. Cryptorchidism: about 1% of 1 year boys,20% of unilateral, and 50% of
bilateral crypt have abnormal semen count
F. Varicocele: usually left sided, it is associated with testicular atrophy which
is reversible on varicocele correction.
Post-testicular causes
A. Reproductive tract obstruction
Congenital obstruction
• Cystic fibrosis
• Young syndrome
• Adult polycystic disease
• Blockage of ejaculatory duct
Acquired blockage
• Vasectomy
• Groin and hernia surgery
• Bacterial infection
Functional blockage (nerve injury/drugs)
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
B. Disorders of sperm function or motility
Immotile cilia syndrome
Maturation defects
Immunologic infertility
Infection
C. Disorders of coitus
Impotence
Hypospadias
Timing and frequency
Treatment Of Male Infertility
Surgical treatment:
Correction of varicocele.
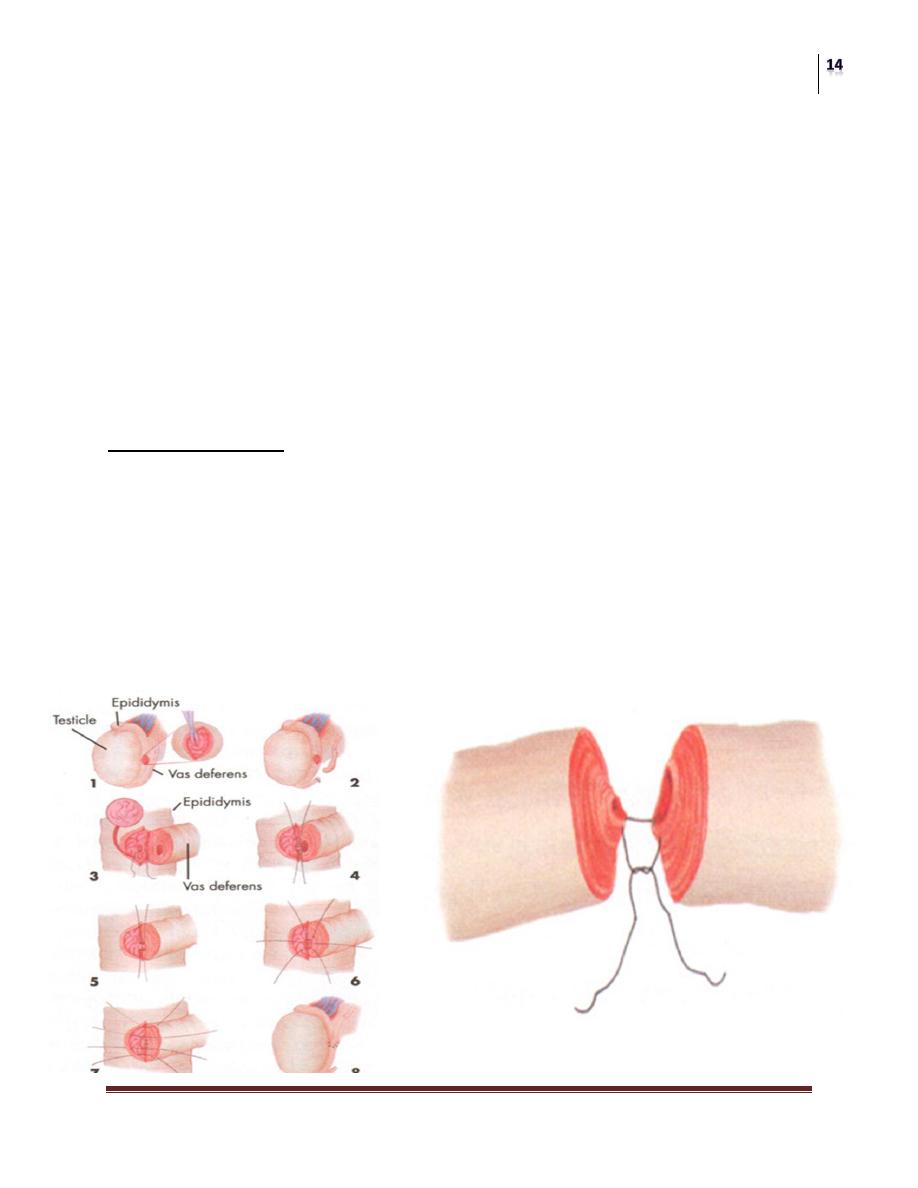
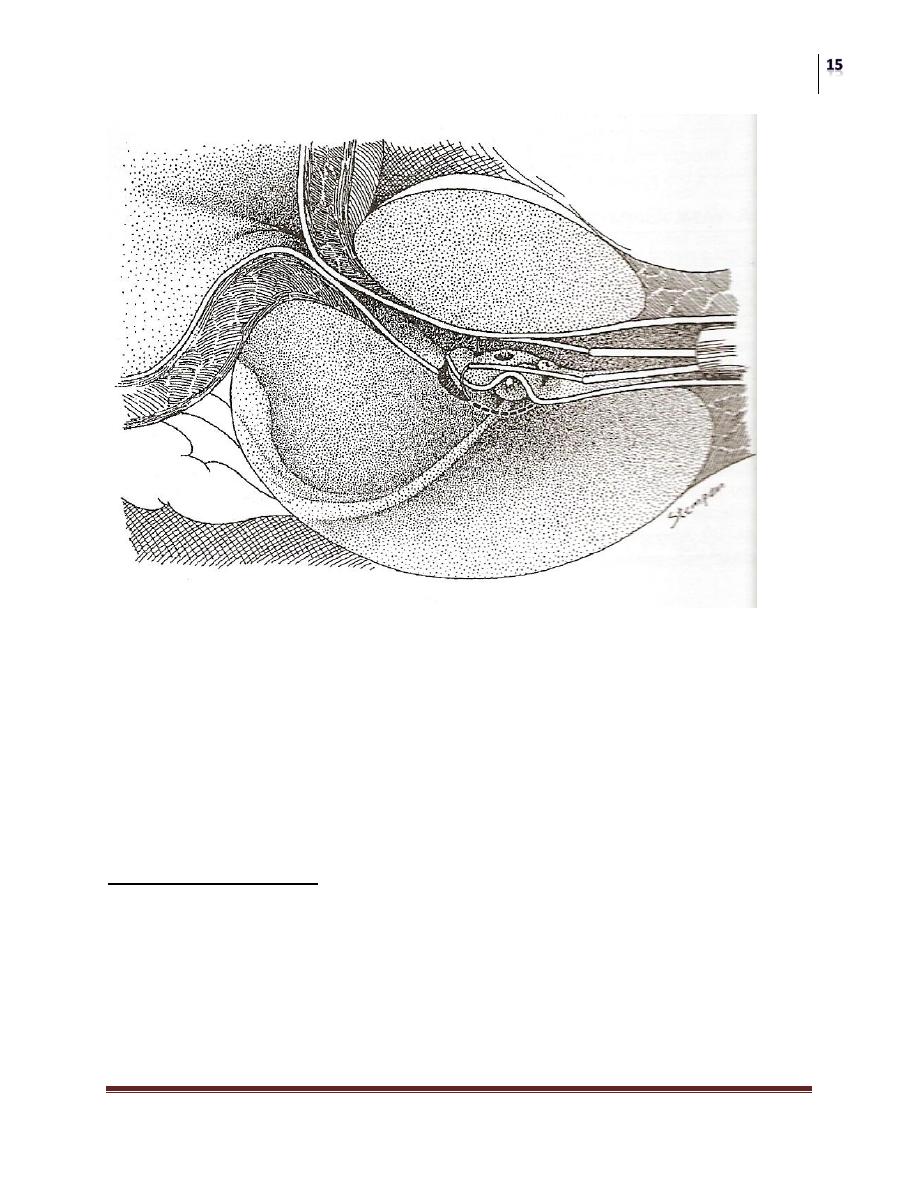
Vasovasostomy: should be done by microsurgical technique.
Transurethral resection of ejaculatory duct obstruction.
Electroejaculation: to treat an-ejaculation in patient with SC injury, done
through rectal probe to stimulate pelvic sympathetic nerves and induce
ejaculation, the ejaculate used later of ART.
Microsurgical treatment of obstructive infertility
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
Sperm aspiration: to treat patients with uncorrectable ductal obstruction, or
azospermic men to retrieve sperms for ART.
Vasal aspiration
Epididymal sperm aspiration
Testis sperm retrieval
Orchidopexy
Pituitary ablatoin
Nonsurgical Treatment
Specific therapy:
Pyospermia: by broad spectrum antibiotics as doxycyclin,or
methoprim, with frequent ejaculation and antioxidants as vit.E or
glutathione.
Coital therapy: coitus every other day around ovulation is the best.
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
Immunologic infertility: it is difficult to treat, options include steroids,
sperm wash, IUI,IVF, and ICSI.
Medical therapy: to treat specific hormonal abn.
Hyperprolactinemia: by bromocriptine
Hypo-hyperthyroidism
Hormonal deficiency: as in Kallmann syndrome, treat with GnRH in
pulsatile manner, or LH,FSH injections.
Anabolic steroids excess: stop them ,if no response within few months
jump start the testis with FSH,LH.
Empiric medical therapy
Clomiphene citrate: synthetic antiestrogen that results in increased
secretion of GnRH, LH,& FSH.
Tamoxifin.
Antioxidant therapy:
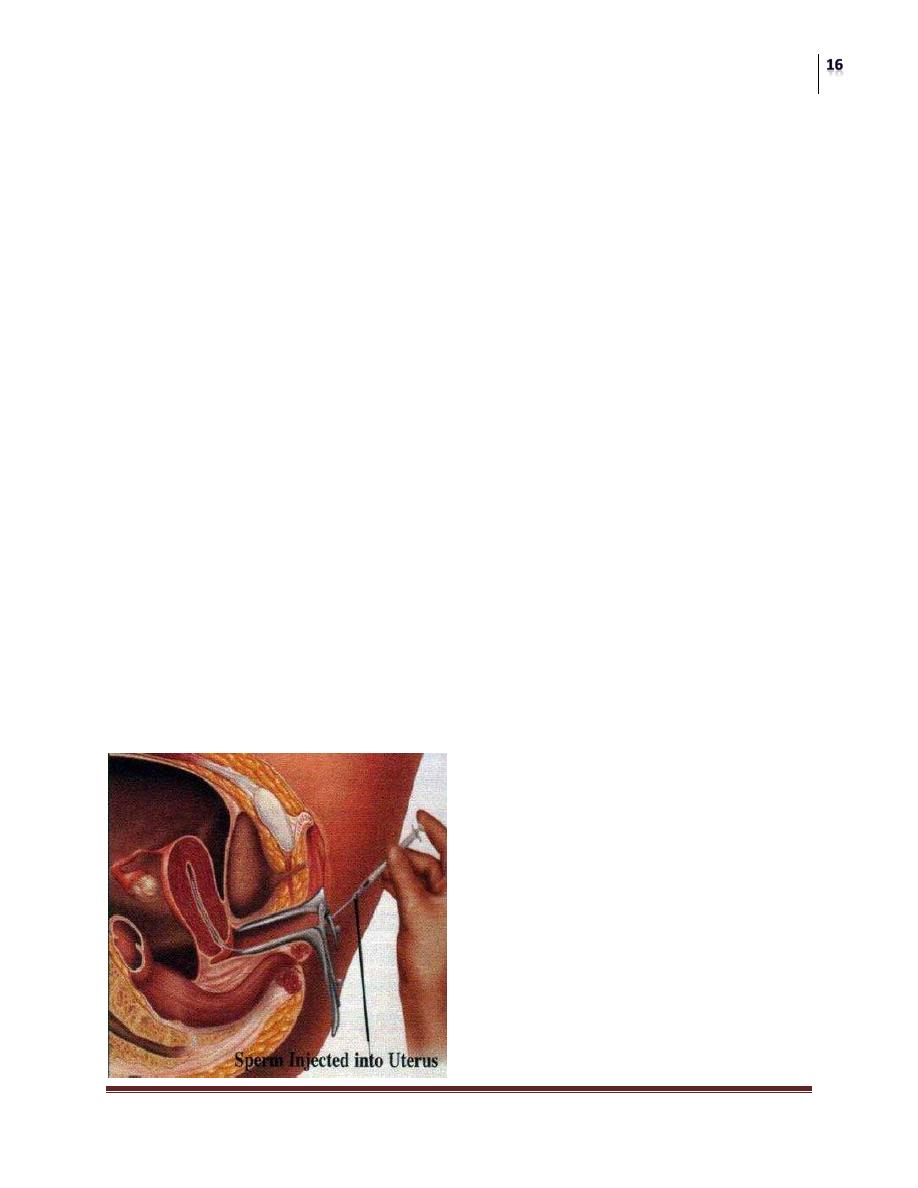
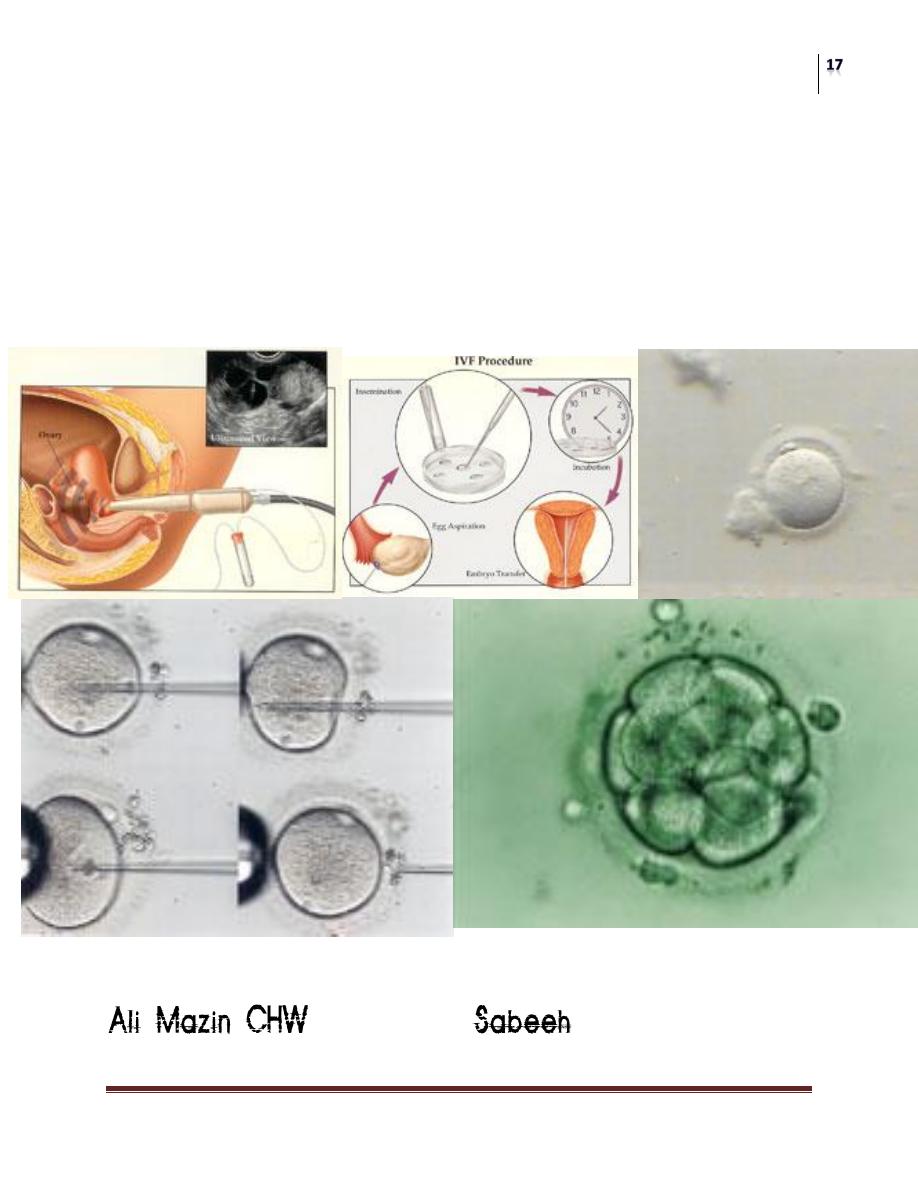
Assisted Reproductive Techniques
Used when both surgical and medical therapy fail to treat infertility, specially of
unknown cause.
Intrauterine insemination: placement of washed pellet of ejaculated
sperm within the female uterus beyond the cervical barrier. The major
indication is cervical hostility and mechanical caused as hypospadias.
Surgery
Male Infertility
Dr.Montadhar Al-Almadani
Lec. 39
In vitro fertilization: oval and sperm retrieval, then the eggs are
fertilized in petri dishes and embryo reimplanted in the uterus.
500,000 to 5,000,000 sperms are required.
Intracytoplasmic sperm injection: one sperm is enough for this
procedure.
Draw back of IVF,ICSI is that they bypass the natural selection barriers so
offspring are more liable for chromosomal abn, and genetic causes of infertility are
passed to them. So they use now preimplantation genetic diagnosis.
