Surgery
Urological Emergencies
Dr. Ismaeel
Lec. 44
Torsion of the testis and testicular appendages
Definition
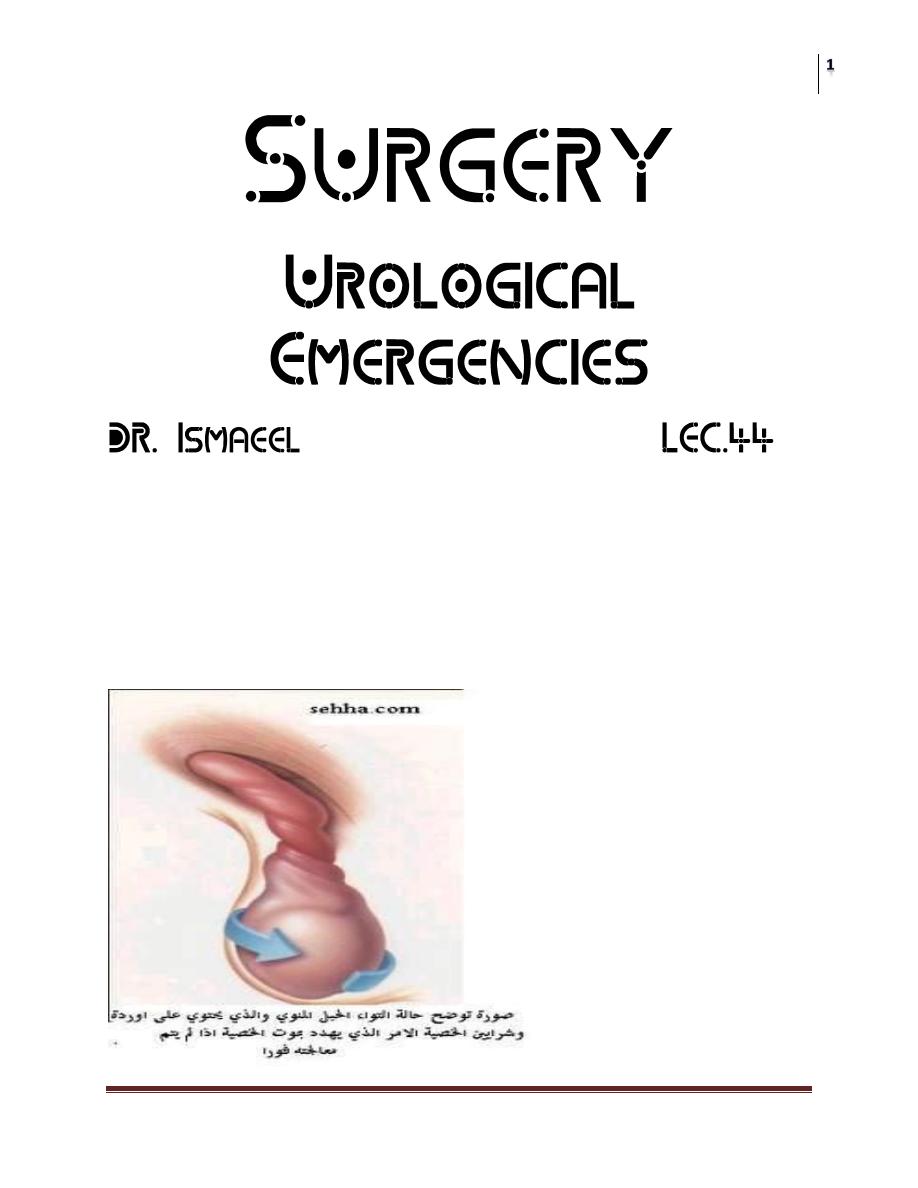
Testicular torsion is a twist of the spermatic cord, resulting in strangulation of the
blood supply to the testis and epididymis.
Testicular torsion occurs most frequently between the ages of 10 and 30 (peak
incidence 13–15 years of age), but any age group may be affected.
Surgery
Urological Emergencies
Dr. Ismaeel
Lec. 44
Pathogenesis:
1. Torsion of the spermatic cord:
Transverse lie of the testis.
High insertion of redundant tunica vaginalis.
Exacurated cremastic reflex.
BELL CLAPPER effect
2. Torsion of the testis:
Long mesentery bet. Testis and epididymus.
History and examination
There is a sudden onset of severe pain in the hemiscrotum, sometimes
waking the patient from sleep. It may radiate to the groin, flank, or
epigastrium and is often associated with nausea.
Sometimes a history of minor trauma to the testis.
Some patients report previous episodes with spontaneous resolution of the
pain.
The torsed testis is usually moderately swollen and very tender to the touch.
It may be high riding compared to the contralateral testis and may lie in a
horizontal position due to twisting of the cord.
The cremasteric reflex is nearly always absent in the event of true testicular
torsion.
Elevation of the scrotum and supporting may relieve the pain of epididymitis
but not in torsion.
Differential diagnosis
1. epididymoorchitis. MOST IMPORTANT
2. Torsion of a testicular appendage.
3. Causes of flank pain with radiation into the groin and testis (e.g., a ureteric
stone).
Surgery
Urological Emergencies
Dr. Ismaeel
Lec. 44
Investigations
Radiographic studies (ultrasound study with doppler) are generally used to
confirm the absence of torsion.
Color Doppler ultrasound (reduced arterial blood flow in the testicular
artery)
Radionuclide scanning (decreased radioisotope uptake) can be used to
diagnose testicular torsion.
In many hospitals these tests are not readily available and the diagnosis is based on
symptoms and signs.
If torsion is suspected clinically, arrangements should immediately be
made for surgical exploration and detorsion.
(Open and see better than wait and see)
Surgery
Urological Emergencies
Dr. Ismaeel
Lec. 44
Surgical management
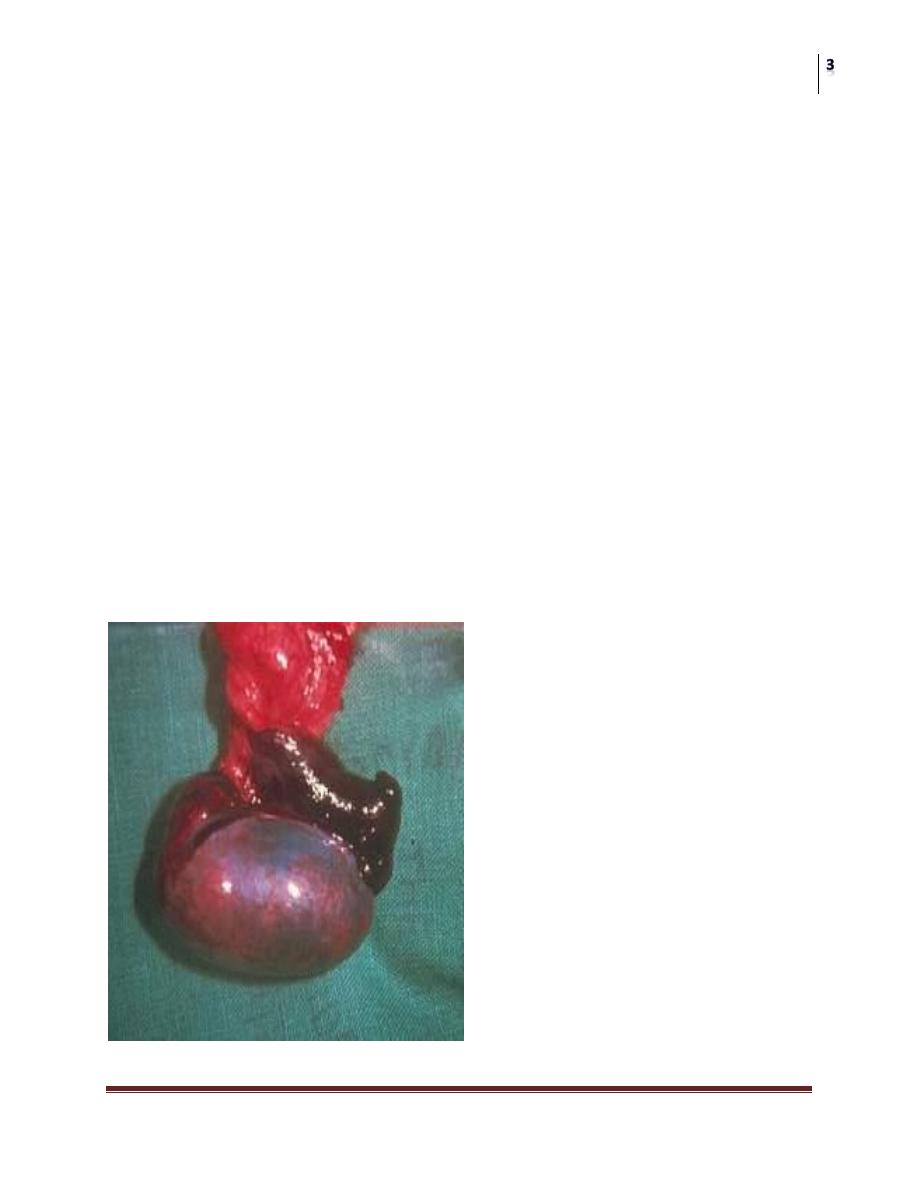
Scrotal exploration should be undertaken as a matter of urgency (golden
period is 6 hours)since delay in relieving the twisted testis results in
permanent ischemic damage to the testis, causing atrophy, loss of hormone
and sperm production, and, as the testis undergoes necrosis and the blood–
testis barrier breaks down, an autoimmune reaction against the contralateral
testis (sympathetic orchidopathy).
1. Trial of manual detorsion under sedation eg valium injection.
2. Surgical exploration:
If the testis is vaible : detorsion and fixation of the testis to the scrotal wall
(ORCHIOPEXY).
If the testis is not vaible: removal of the testis(ORCHECTOMY)
Keep in your mind that torsion of the testis is a urological emergency and
Time Factor is so critical in the management.
Infarction of testicular appendages
The appendix testis (remnant of the Müllerian duct) and the appendix
epididymis (remnant of acranial mesonephric tubule of the Wolffi an duct)
can undergo infarction, causing pain that mimics a testicular torsion.
The “blue dot” sign is the typical physical fi nding for appendix testis
infarction.
At scrotal exploration they are easily removed with scissors or
electrocautery.
If these diagnoses are confirmed radiographically, analgesics may be given
and surgical exploration is unnecessary.
