Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
APENIA:
Is extremely rare.
the urethra generally opens on the perineum or inside the rectum.
should be considered for assignment to the female gender:
Castration and vaginoplasty should be considered in combination with estrogen
treatment as the child develops.
MEGALOPENIS
The penis enlarges rapidly in childhood (megalopenis) in boys with
abnormalities that increases the production of testosterone, for example,
interstitial cell tumors of the testicle, hyperplasia, or tumors of the adrenal
cortex. Management is by correction of the underlying endocrine problem.
MICROPENIS
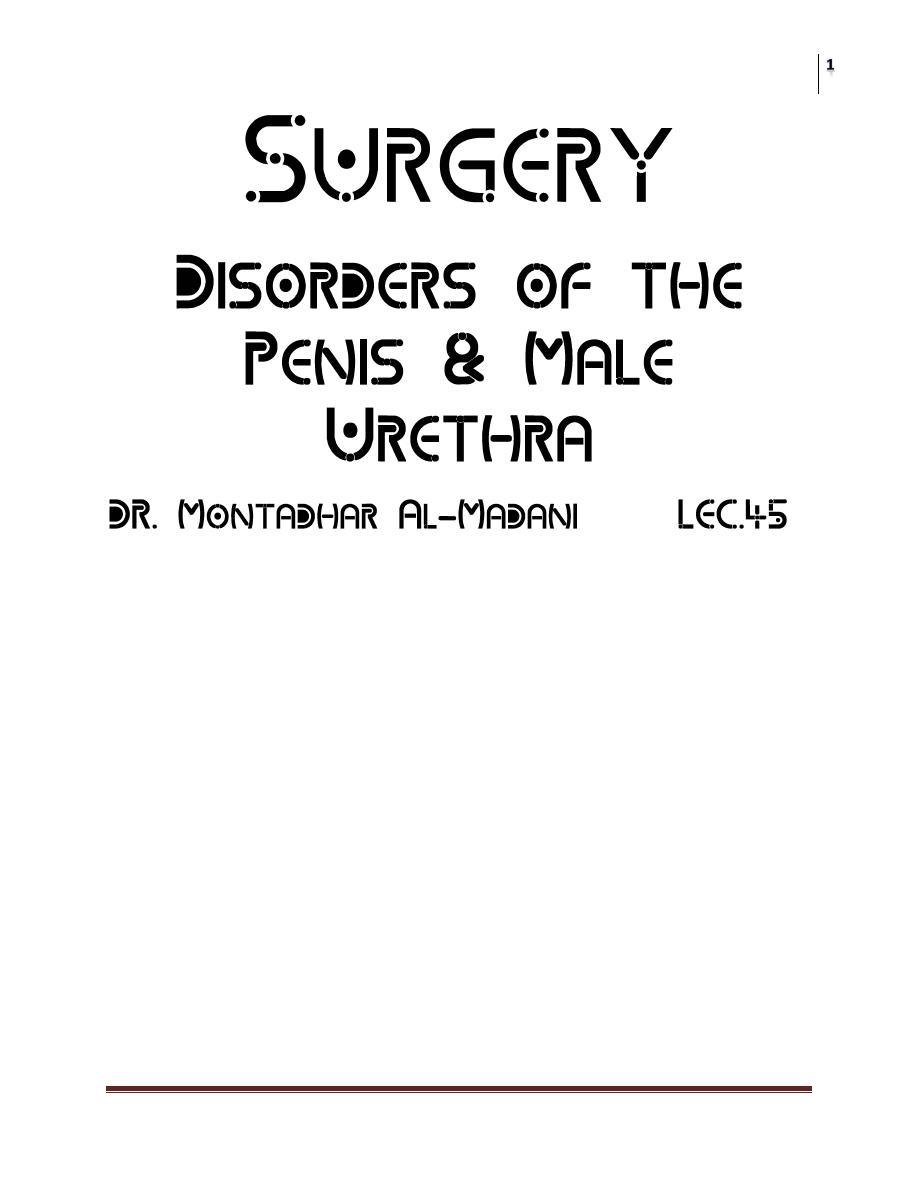
A penis smaller than 2 standard deviations from the norm is considered a
micropenis
Attributed to a testosterone deficiency those results in poor growth of organs
that are targets of this hormone.
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
The testicles are small and frequently undescended.
Early evidence suggests that the ability of the hypothalamus to secrete
(LHRH) is decreased.
topical application of 5% testosterone cream causes increased penile growth
URETHRAL STRICTURE
Congenital urethral stricture is uncommon in infant boys.
The fossa navicularis and membranous urethra are the 2 most common sites.
A careful history and physical examination.
Excretory urography, excretory voiding urethrography , Retrograde
urethrography .
urethroscopy should be performed in all patients in whom urethral stricture
is suspected.
Diaphragmatic strictures may respond to dilation or visual urethrotomy.
surgical repair by anastomotic urethroplasty, buccal mucosa graft, or penile
flap is desirable if the obstruction recurs.
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
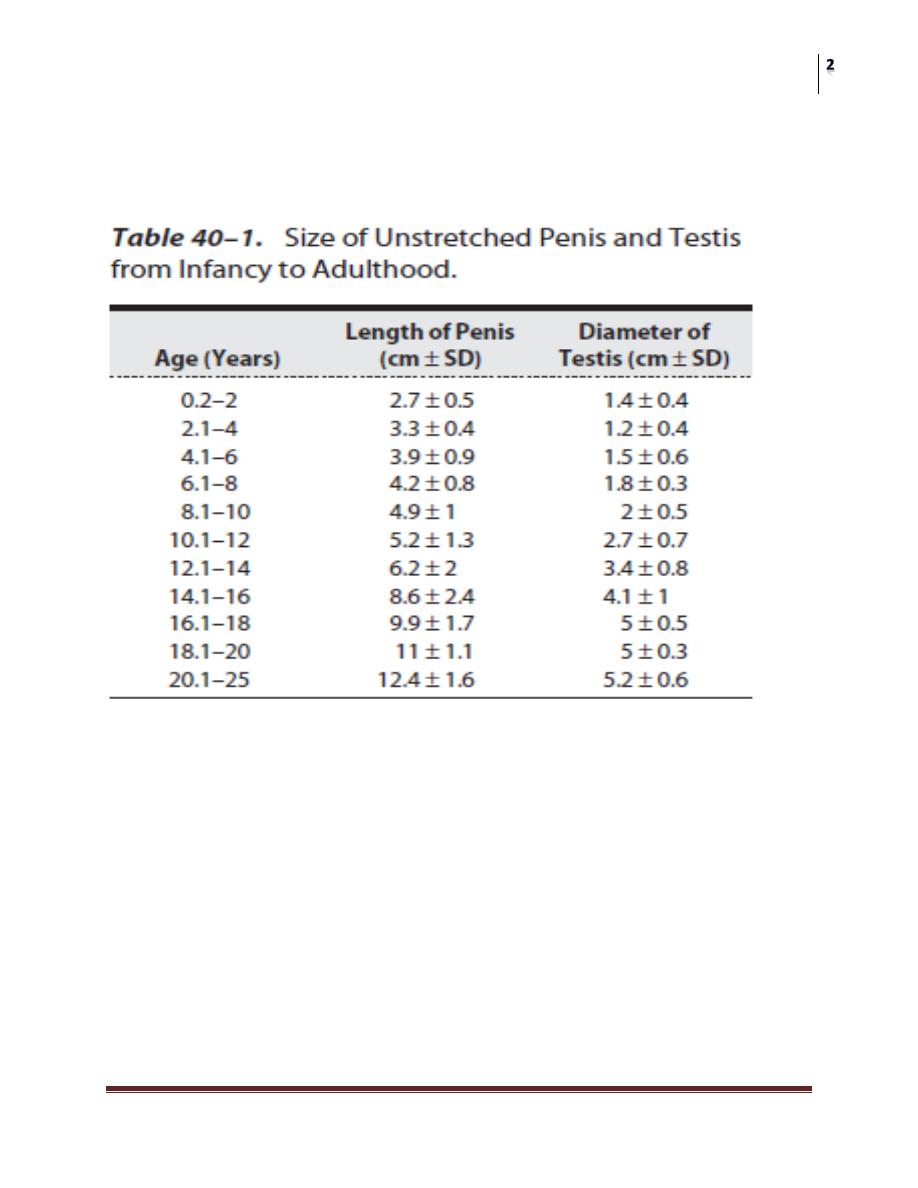
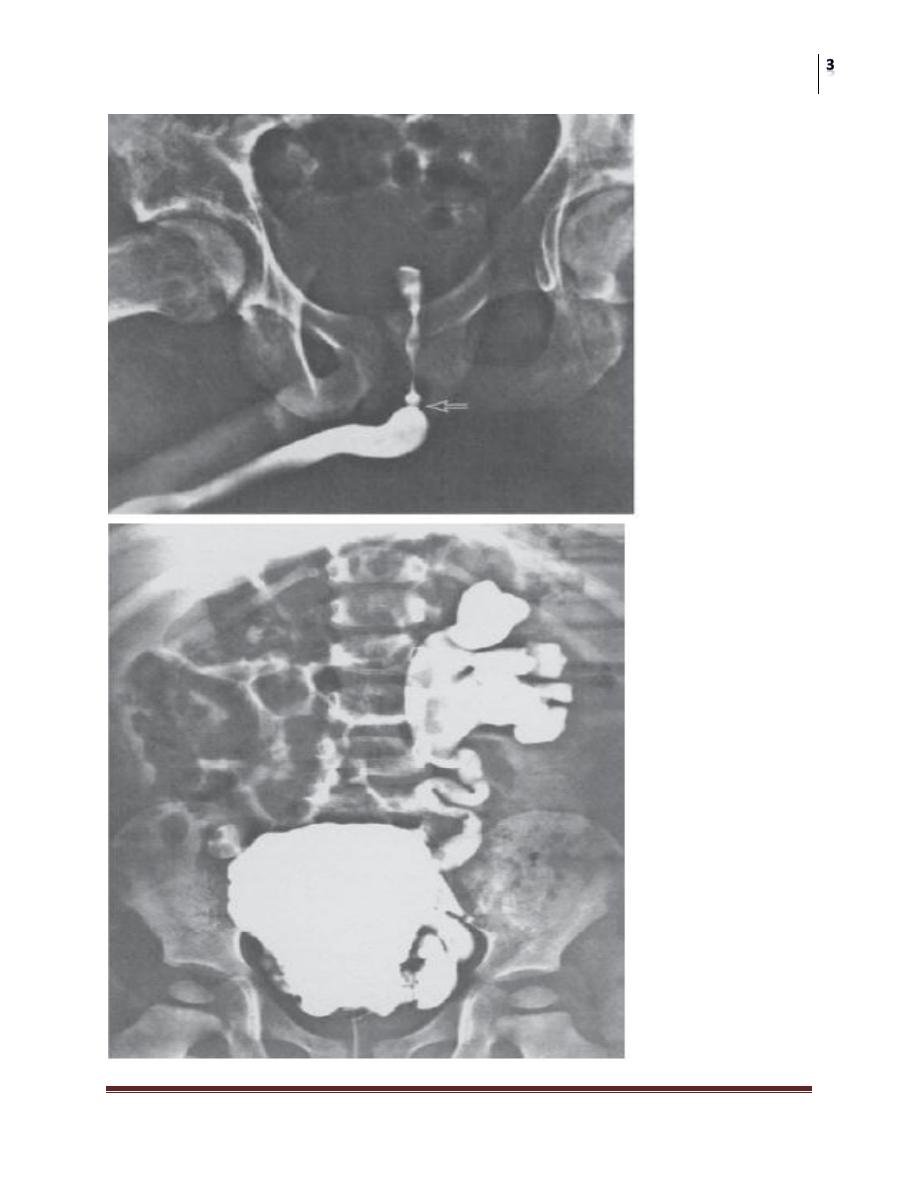
POSTERIOR URETHRAL VALVES
most common obstructive urethral lesions in infants and newborns,
Only in males and are found at the distal prostatic urethra.
The valves are mucosal folds that look like thin membranes; they may cause
varying degrees of obstruction when the child attempts to void.
A. SYMPTOMS AND SIGNS
Symptoms of obstruction.
Urinary infection and sepsis
A palpable abdominal mass.
Failure to thrive.
B. LABORATORY FINDINGS
Azotemia and poor concentrating ability of the kidney are common findings.
Infected urine and anemia.
C. X-RAY FINDINGS
VCUG.
Excretory urograms.
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
D. ULTRASONOGRAPHY
E. INSTRUMENTAL EXAMINATION
Treatment
Treatment consists of destruction of the valves
mild to moderate obstruction and minimal azotemia,
more severe degrees of obstruction
Vesicostomy
percutaneous loop ureterostomies
Treatment of vesicoureteral reflux
Long-term use of antimicrobial
HYPOSPADIAS
the urethral meatus opens on the ventral side of the penis proximal to the tip
of the glans penis
Sexual differentiation and urethral development begin in utero at
approximately 8 weeks and are complete by 15 weeks.
The urethra is formed by the fusion of the urethral folds along the ventral
surface of the penis, which extends to the corona on the distal shaft. The
glandular urethra is formed by canalization of an ectodermal cord that has
grown through the glans to communicate with the fused urethral folds
Hypospadias occurs in 1 in every 300 male children.
Estrogens and progestins given during pregnancy are known to increase the
incidence. Although a familial pattern of hypospadias has been recognized
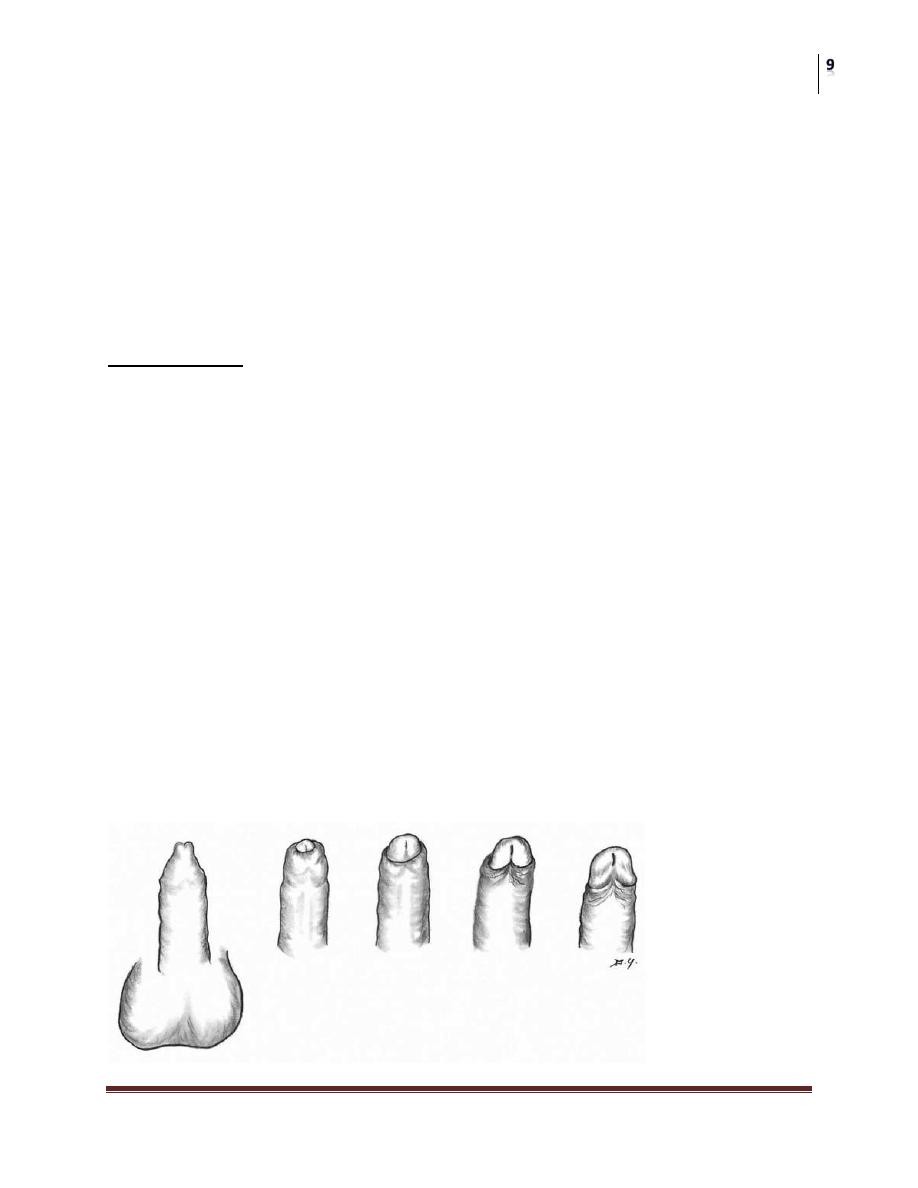
Classification
Classified according to location:
(1) Glandular, that is, opening on the proximal glans penis;
(2) Coronal, that is, opening at the coronal sulcus;
(3) Penile shaft;
(4) Penoscrotal;
(5) Perineal.
About 70% of all cases of hypospadias are distal penile or coronal.
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
SYMPTOMS AND SIGNS
difficulty directing the urinary stream
Stream spraying.
Chordee which can prevent sexual intercourse.
Perineal or penoscrotal hypospadias necessitates voiding in the sitting
position,
Infertility.
Abnormal (hooded) appearance of the penis, caused by deficient or absent
ventral foreskin.
meatus may be stenotic
increased incidence of undescended testicles in children with hypospadias;
LABORATORY, X-RAY, & ENDOSCOPIC FINDINGS
a buccal smear and karyotyping are indicated to help establish the genetic
sex.
Urethroscopy and cystoscopy are of value to determine whether internal
male sexual organs are normally developed.
Excretory urography
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
Treatment
For psychological reasons, hypospadias should be repaired before the patient
reaches school age; in most cases, this can be done before age 2.
More than 150 methods of corrective surgery for hypospadias have been
described.
Currently, 1-stage repairs with foreskin island flaps and incised urethral
plate are performed by more and more urologists.
All types of repair involve straightening the penis by removal of the chordee.
Prognosis:
After corrective surgery, most patients are able to void in the standing position as
well as to deposit semen into the vagina.
EPISPADIAS
The urethra is displaced dorsally, and classification is based on its position
in males.
The incidence of complete epispadias is approximately 1 in 120,000 males
and 1 in 450,000 females.
In glandular epispadias, the urethra opens on the dorsal aspect of the glans,
which is broad and flattened.
The penile type, the urethral meatus, which is often broad and gaping, is
located between the pubic symphysis and the coronal sulcus.
The penopubic type has the urethral opening at the penopubic junction.
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
Females with epispadias have a bifid clitoris and separation of the labia.
Most are incontinent.
Patients with glandular epispadias seldom have urinary incontinence.
However, with penopubic and penile epispadias, incontinence is present in
95% and 75% of cases, respectively.
dorsal chordee
Surgery is required to correct the incontinence, remove the chordee to
straighten the penis, and extend the urethra out onto the glans penis.
PRIAPISM
Priapism is an uncommon condition of prolonged erection.
It is usually painful for the patient, and no sexual excitement or desire is present.
Idiopathic in 60% of cases, while the remaining 40% of cases are associated
with diseases (eg, leukemia, sickle cell disease, pelvic tumors, pelvic
infections), penile trauma, spinal cord trauma, or use of medications
(trazodone). Currently, intracavernous injection therapy
Priapism may be classified into high- and low-flow types.
High-flow priapism (nonischemic) usually occurs
Secondary to perineal trauma, results in loss of penile blood-flow regulation.
Aspiration of penile blood for blood-gas determination demonstrates high
oxygen and normal carbon dioxide levels.
Arteriography is useful to demonstrate aneurysms that will respond to
embolization;
Erectile function is usually preserved.
low-flow priapism (ischemic)
Painful erection.
The glans penis and corpus spongiosum are soft and uninvolved in the
process.
Most authorities believe the major abnormality to be physiologic obstruction
of the venous drainage.
Poorly oxygenated blood (low O2, high CO2) within the corpora cavernosa.
Ischemic priapism must be considered a urologic emergency.
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
The sludged blood can then be evacuated from the corpora cavernosa
through a large needle placed through the glans.
Multiple wedges of tissue can be removed with a biopsy needle to create a
shunting fistula between the glans penis and corpora cavernosa.
Another shunting technique may be used by anastomosing the superficial
dorsal vein to the corpora cavernosa.
Impotence is the worst sequel of priapism.
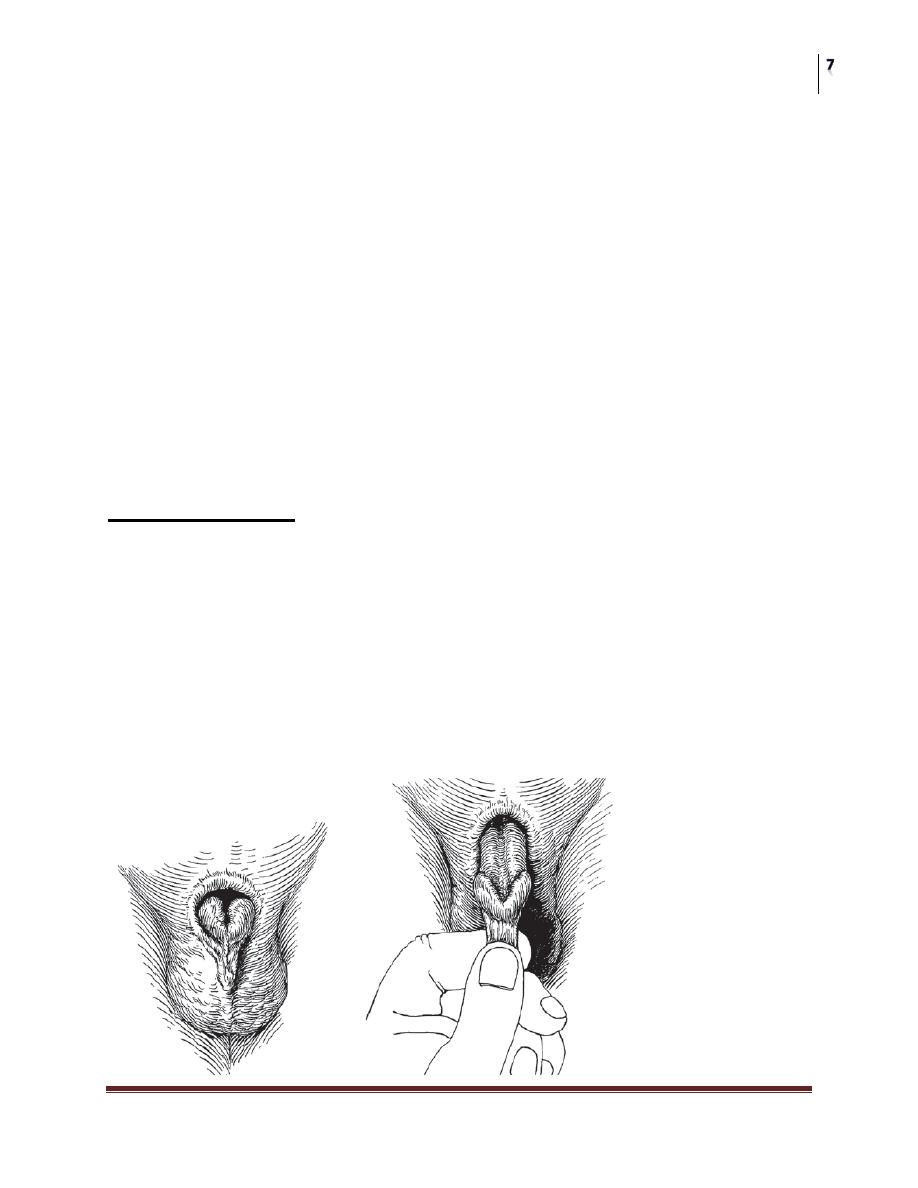
PHIMOSIS
Phimosis is a condition in which the contracted foreskin cannot be retracted
over the glans.
Chronic infection from poor local hygiene is its most common cause.
Phimosis can occur at any age.
In diabetic older men, chronic balanoposthitis may lead to phimosis and may
be the initial presenting complaint.
Edema, erythema, and tenderness of the prepuce and the presence of
purulent discharge usually cause the patient to seek medical attention.
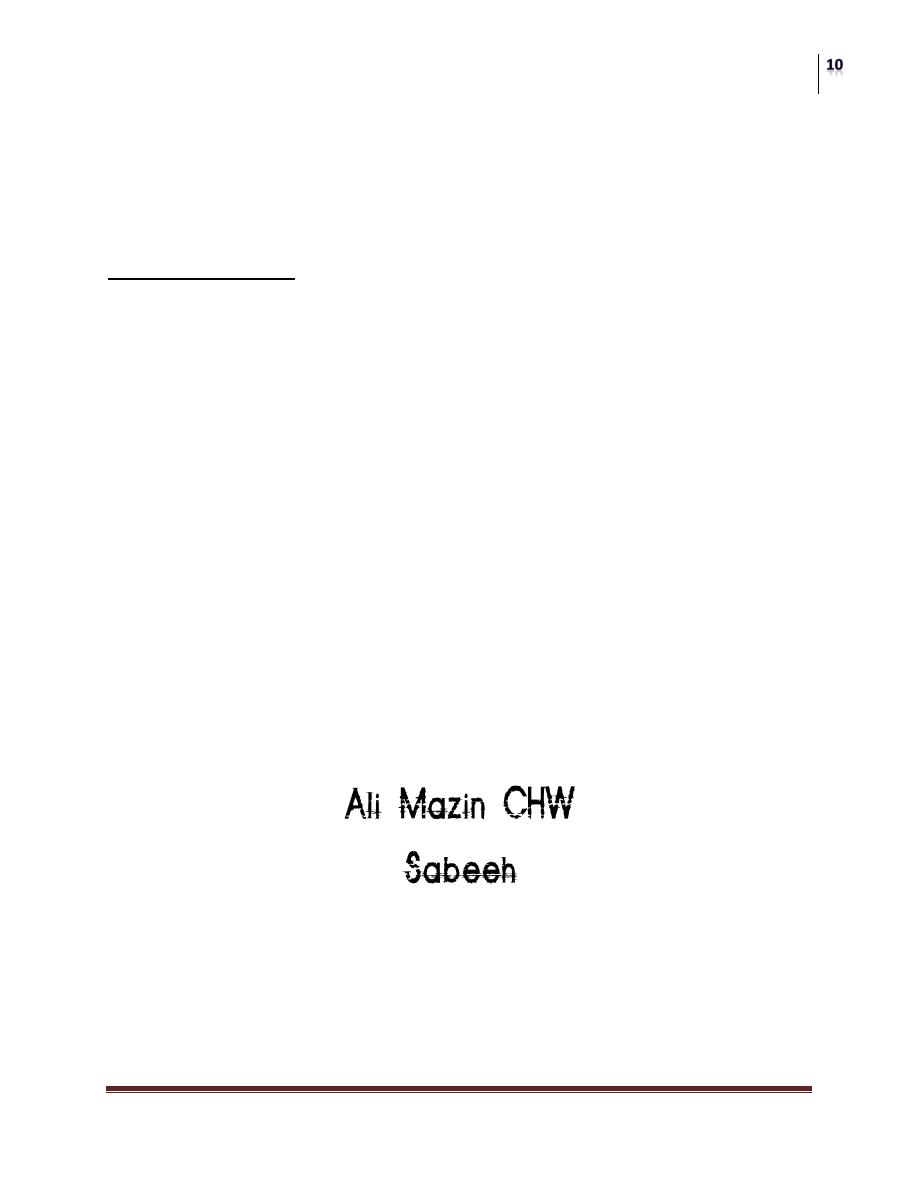
Classification of prepuce types.
Type I: preputium cannot be retracted.
Type II: only the urethral meatus can be exposed.
Type III: preputium can be retracted to expose half of the glans.
Type IV: the corona cannot be exposed because of preputial adhesions to the
corona.
Type V: no adhesions. The entire glans can be exposed
Surgery
Disorders of the Penis & Male Urethra
Dr. Montadhar AL-Madani
Lec. 45
The initial infection should be treated with broad-spectrum antimicrobial
drugs.
The dorsal foreskin can be slit if improved drainage is necessary.
Circumcision, if indicated, should be done after the infection is controlled.
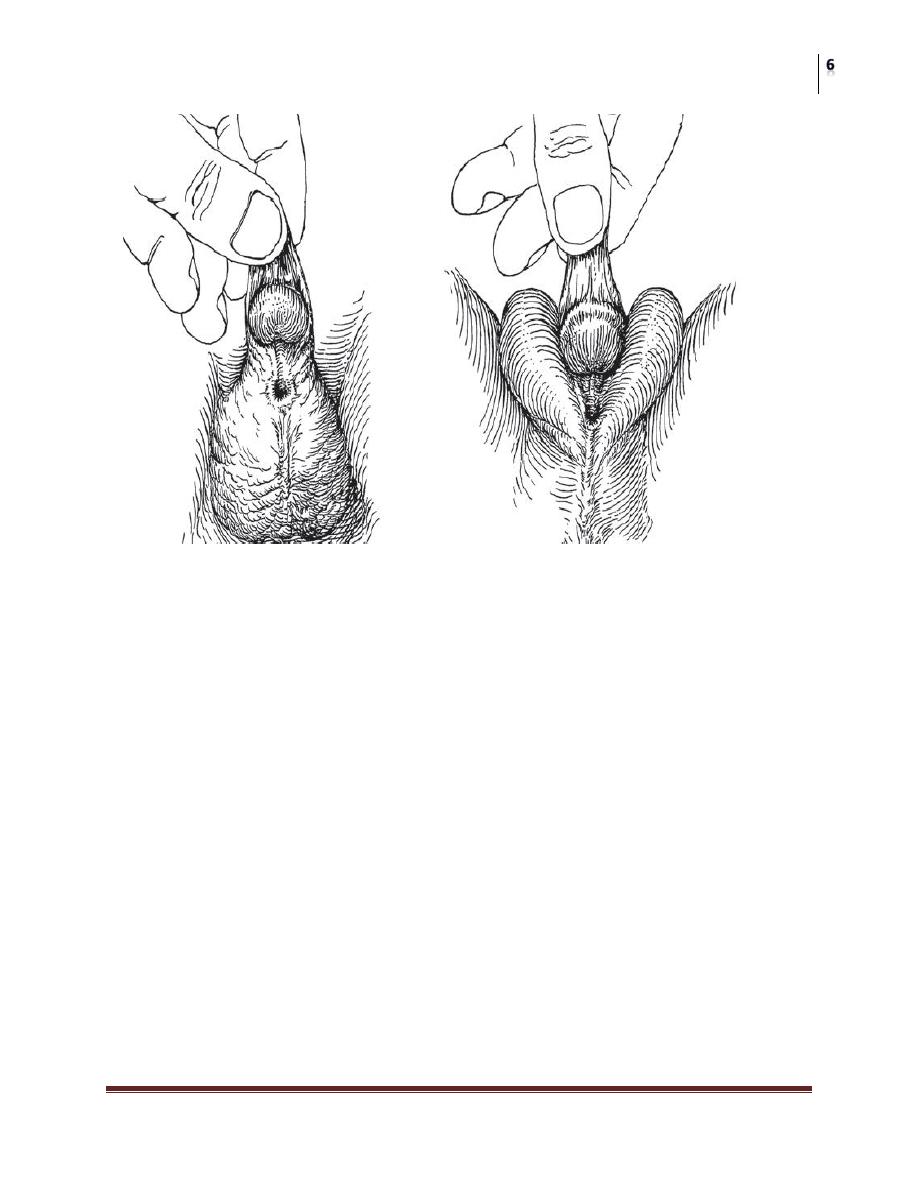
PARAPHIMOSIS
Paraphimosis is the condition in which the foreskin, once retracted over the
glans, cannot be replaced in its normal position.
This is due to chronic inflammation under the redundant foreskin, which
leads to contracture of the preputial opening (phimosis) and formation of a
tight ring of skin
The skin ring causes venous congestion leading to edema and enlargement
of the glans, which make the condition worse. As the condition progresses,
arterial occlusion and necrosis of the glans may occur.
Paraphimosis usually can be treated by firmly squeezing the glans for 5
minutes to reduce the tissue edema and decrease the size of the glans.
Occasionally, the constricting ring requires incision under local anesthesia.
Antibiotics should be administered and circumcision should be done after
inflammation has subsided.
