Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
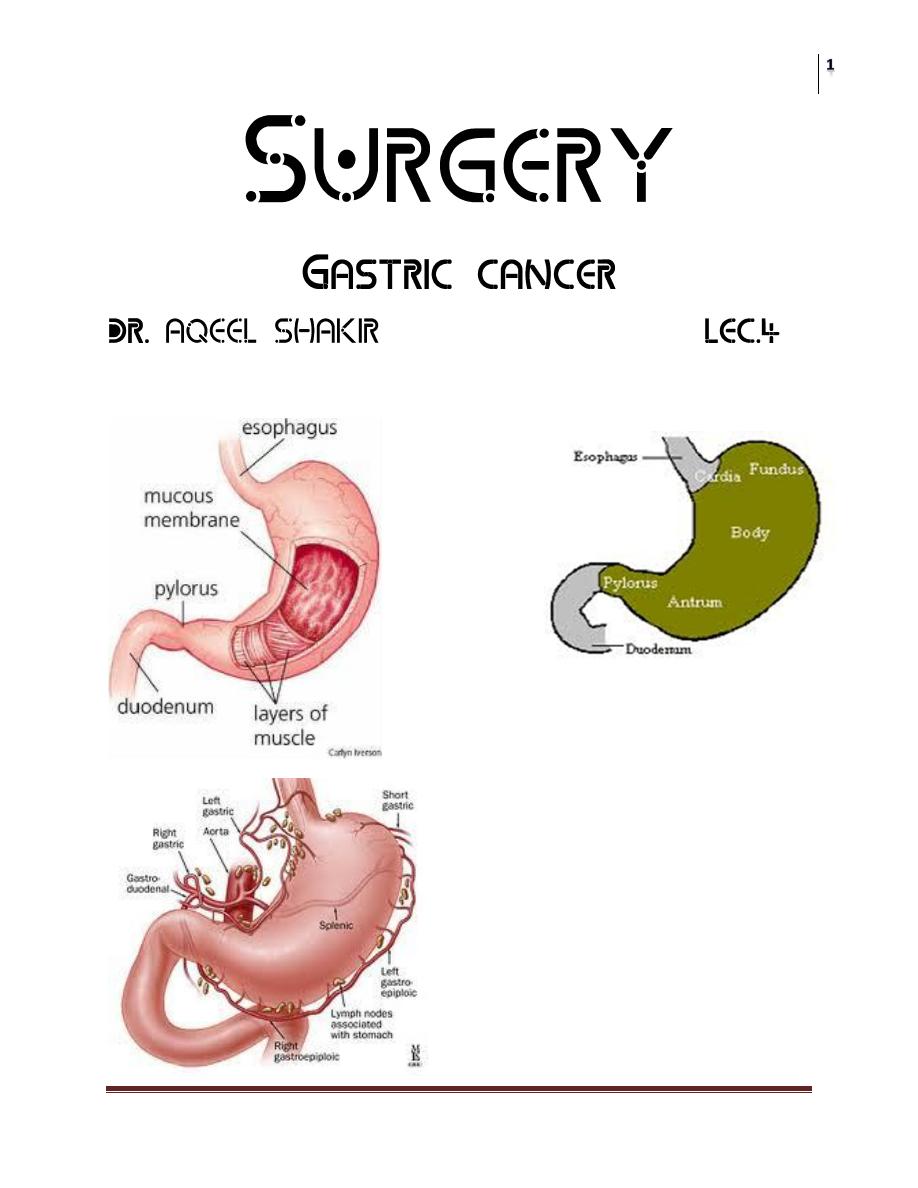
Surgical anatomy
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
Introduction
• The detection of gastric cancer in the early stage is vitally important in
ensuring an excellent prognosis.
• Early gastric cancer, whereby disease is limited to mucosa and submucosa,
confers a 5 years survival rate of greater than 90% in many centers.
• When discovered in its symptomatic phase with a 5-year survival rate of less
than 20%.
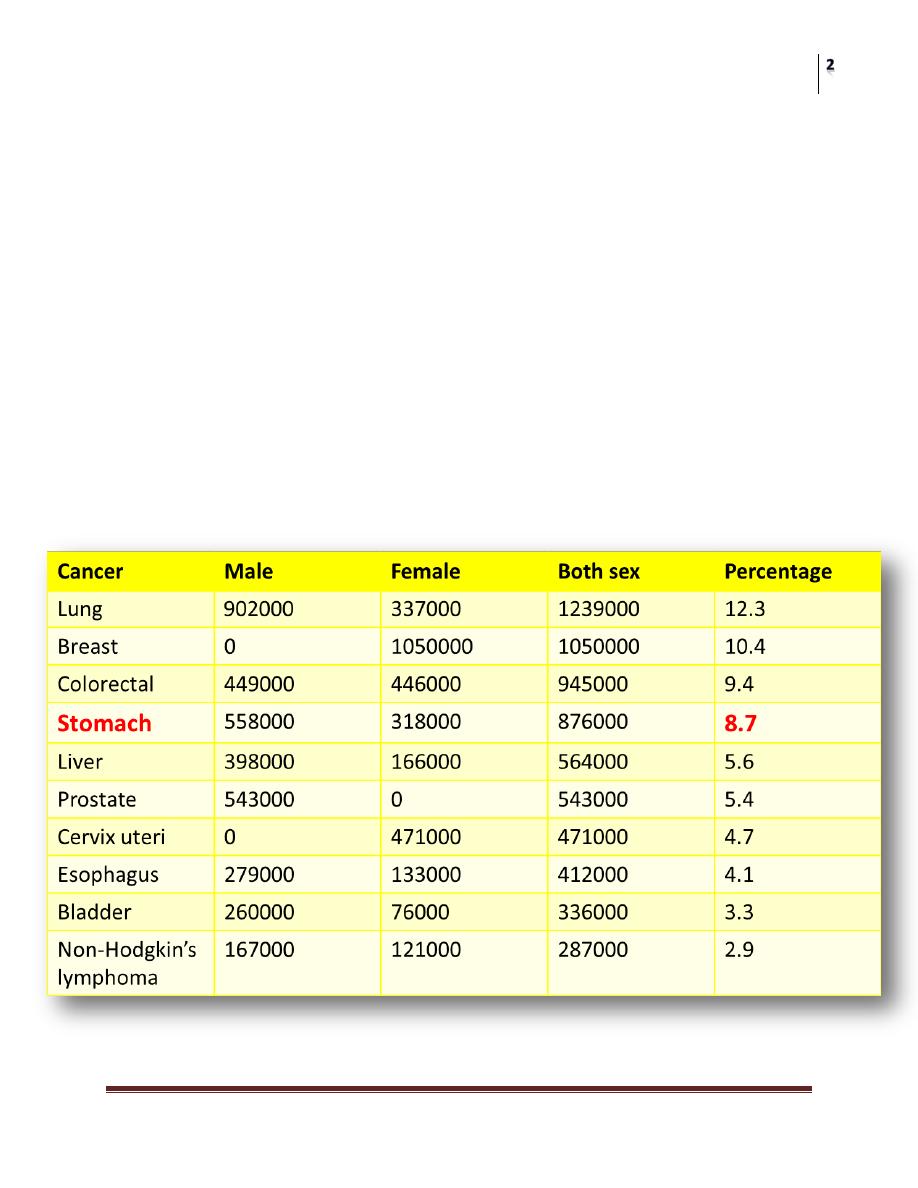
• The most recent estimation shows that gastric cancer is:
1. The Fourth most common cancer.
2. The Second most common cause of cancer deaths worldwide.
Estimated new cancer cases. Ten most common sites,
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
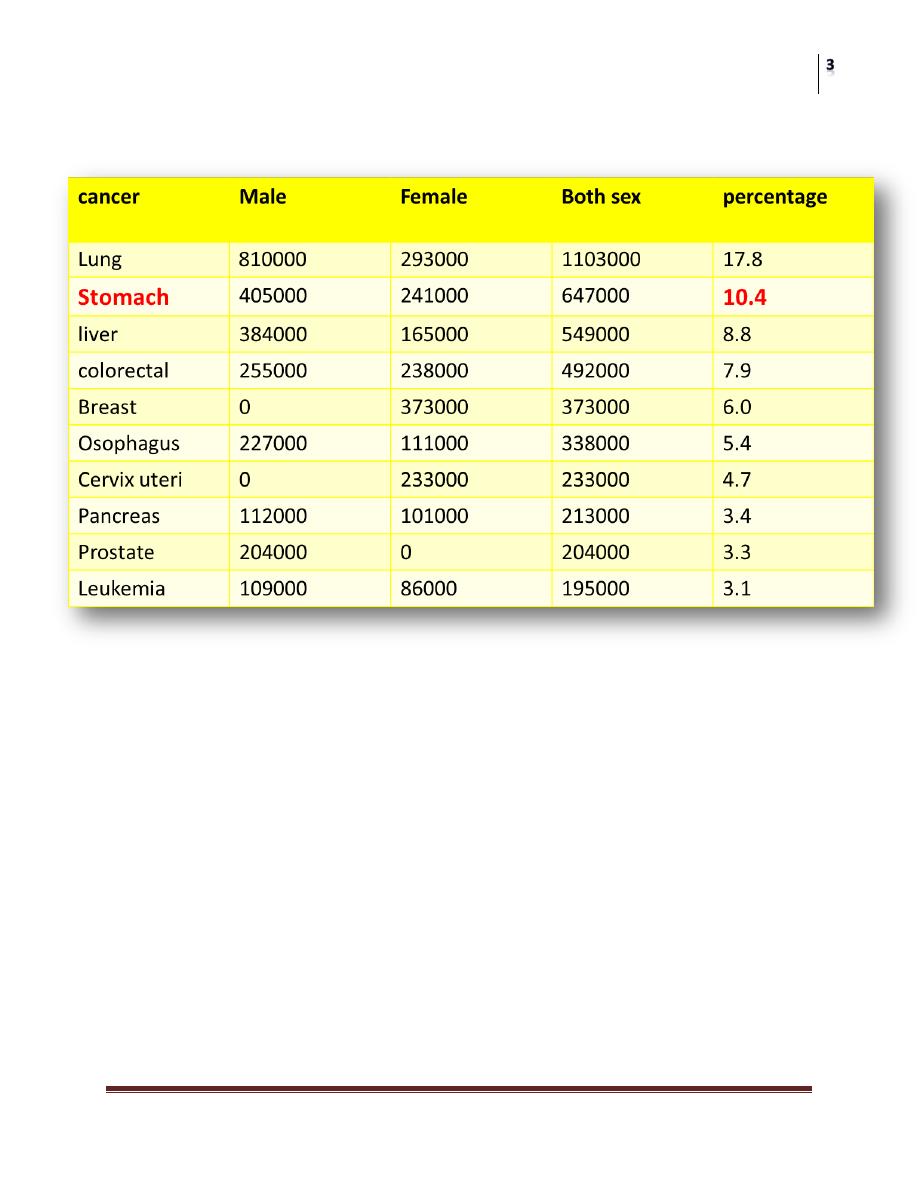
Estimated cancer deaths. Ten most common sites,
• The incidence of gastric cancer varies markedly in different areas of the
world.
• The male preponderance of 2:1 is encountered worldwide. The disease is
rarely seen before the age of 40 years and the incidence varies sharply with
age.
• The incidence and mortality is double for males in both high and low risk
countries.
• Cancer of the stomach is three times more common in social class 4 and 5 (
semiskilled, unskilled labourers ) than in social class 1 and 2 (professional ,
executive and higher manager )
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
Classification of gastric carcinoma
• several classifications of gastric carcinoma exist, like:
1. Lauren (finish) (D.I.O.) classification .
2. Japanese classification (for early gastric cancer).
3. Bormann classification (for advance gastric cancer).
Lauren classification:
• This recognizes two main groups with different histogenesis and aetiology.
• The first group is known as intestinal gastric cancer, as the gastric
carcinoma cells exhibit a striated (brush) border and generally resembles
intestinal cells, they tend to form localized expanding or ulcerating lesion
and frequently surrounded by inteseinal metaplasia.
• The second group is known as the diffuse gastric cancer as the lesion
infiltrates the gastric wall without forming large disecrete masses, this
carries worse prognosis than the intestinal type and arise from apparently
normal gastric mucosa.
• Both the intestinal and diffuse cancers account for 90% of all gastric
carcinoma, the remainder has a mixed morphology and are referred to as
others.
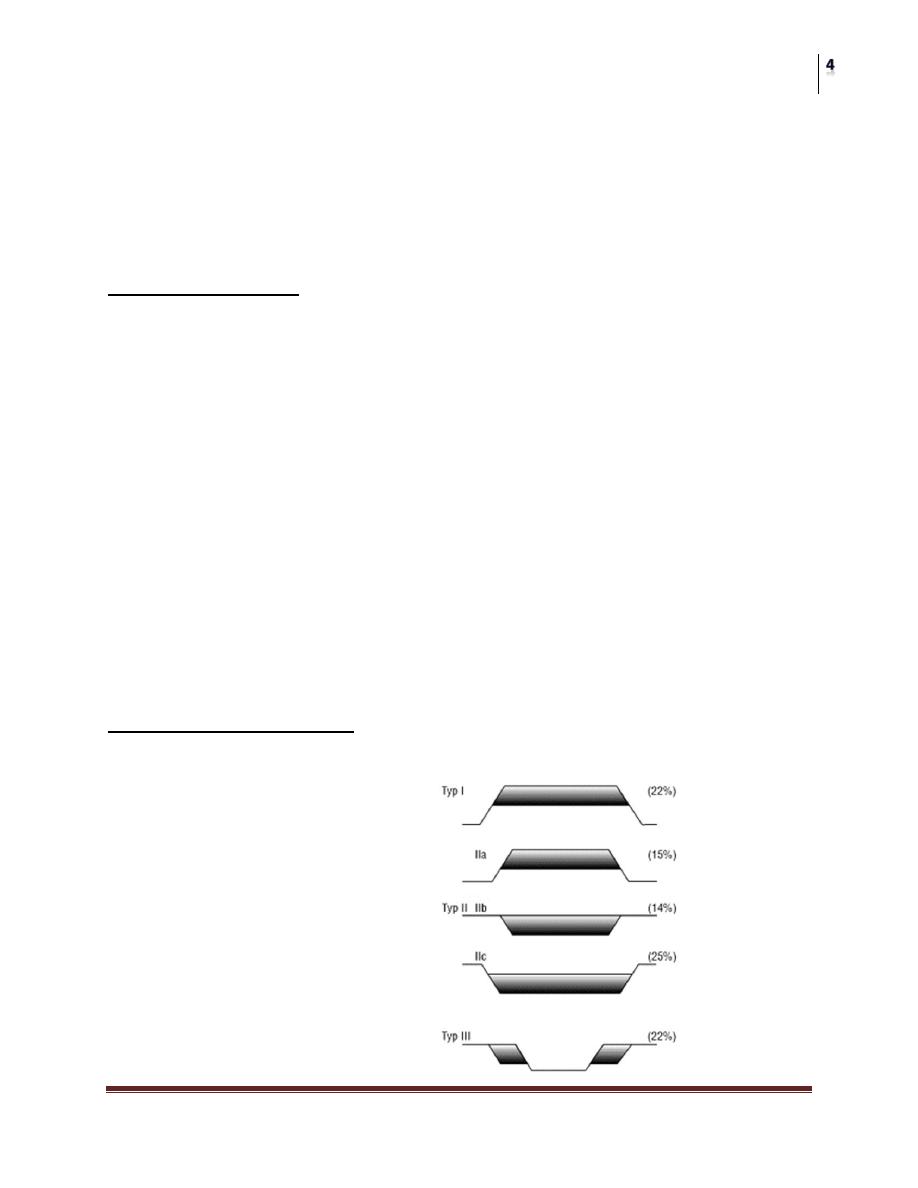
The Japanese classification:
The Japanese Endoscopic Society has classified the macroscopic appearances of
EGC into:
Type I protruded
Type II superficial
a. Elevated.
b. Flat
c. Depress.
Type III excavated
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
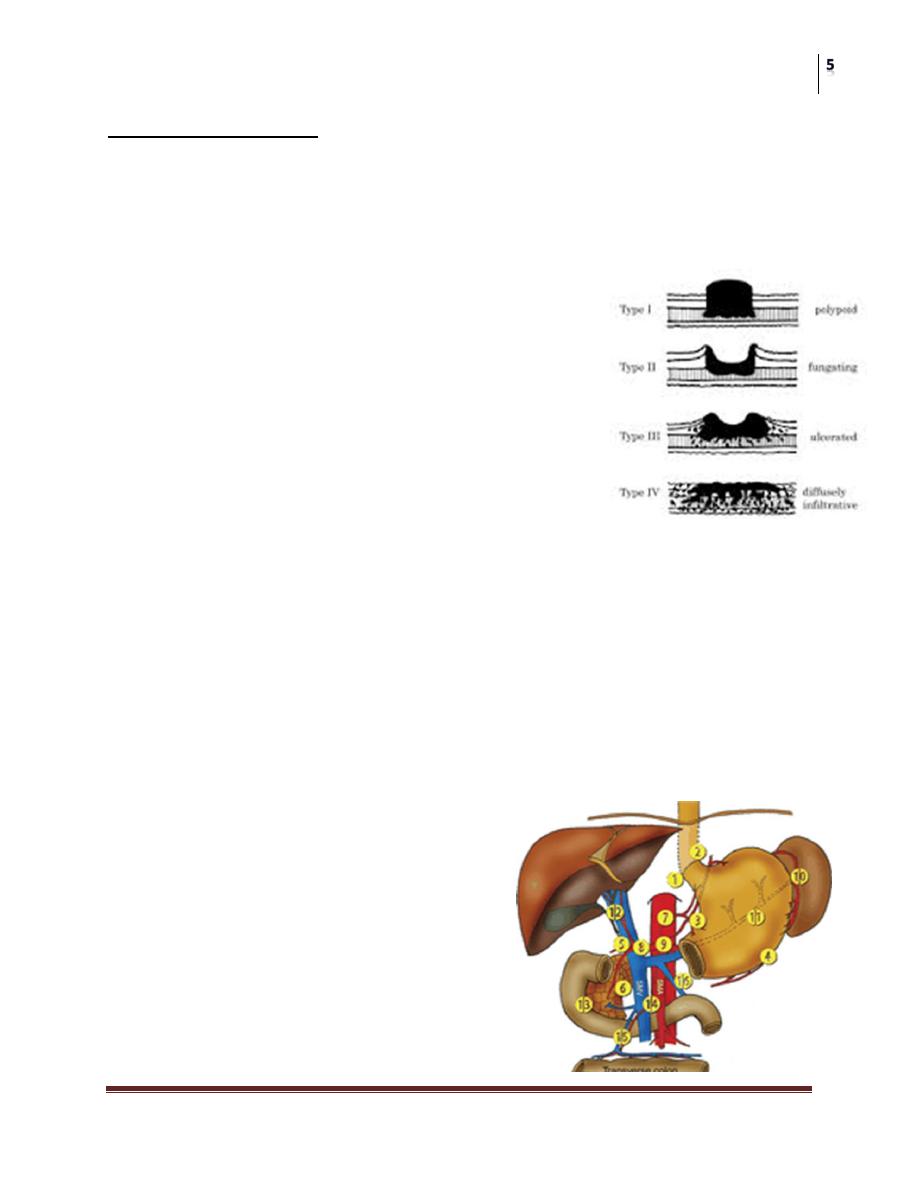
Bormann classification:
• Bormann classification of advance gastric cancer
• Type 1 polypoid.
• Type 2 carcinomatous ulcer without invasion of adjacent mucosa.
• Type 3 carcinomatous ulcer with invasion of adjacent mucosa.
• Type 4 diffusely infiltrative linitis plastic.
Staging
There were several staging for gastric cancer,
however an intermediate staging system has been
the new TNM classification
The important prognostic factors in patient
without detectable distant metastasis are:
• Depth of invasion of the gastric wall.
• LN spread.
• Other significant variables are type of cancer (intestinal or diffuse) location
of tumor (growth of cardia has poorer prognosis than middle or lower third)
and the histological type (degree of differentiation).
Staging of gastric cancer TNM:
• T—primary tumor.
• T1 –tumor invasion of mucosa or mucasa and submucasa.
• T2 - tumor invasion of muscularis propria or subserosa.
• T3- tumor penetrating of serosa.
• T4- tumor invasion of adjacent structures
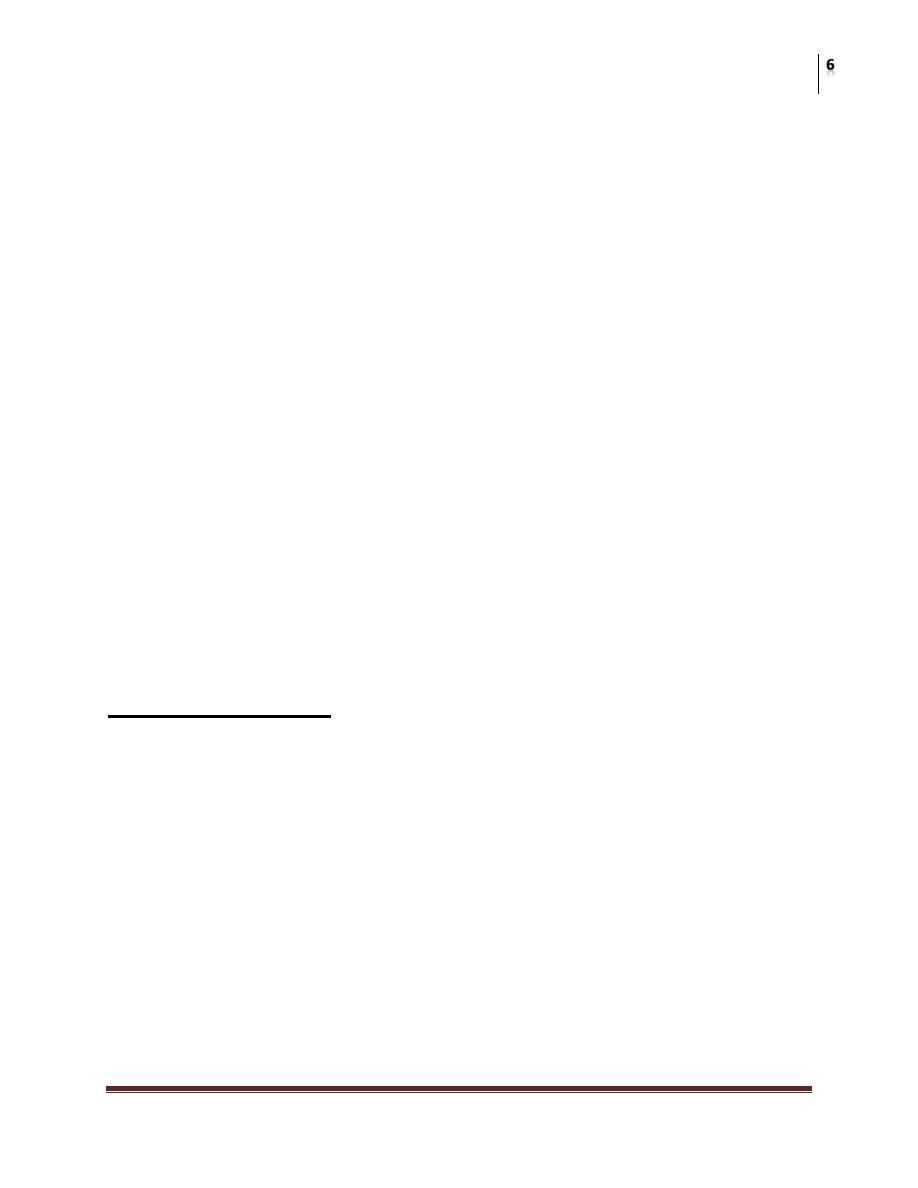
N –regional lymph nodes:
• N0- no evidence of LN metastasis.
• N1- metastasis to group 1 LN.
• Right paracardia LN.
• Left paracardial LN.
• Lesser curvature LN.
• Greater curvature LN.
• Suprapyloric LN.
• Infrapyloric LN
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
N2- metastasis to group 2 LN:
• LN along the left gastric artery.
• LN along the common hepatic artery.
• LN along the celiac artery.
• LN along the splenic hilum.
• LN along the slenic artery.
N3 - metastasis to group 3 LN:
• LN in the hepatoduedenal ligament.
• LN in the retro pancreatic head.
• LN along the superior mesenteric vessels.
• LN along the middle colic vessels.
• Paraoartic LN.
• LN in the anterior pancreatic head.
• LN in the inferior pancreas.
• Infradiaphragmatic LN.
• LN in the osophageal hiatus of the diaphragm.
M - Distant metastasis:
• Mo - no evidence of distant metastasis.
• M1- evidence of distant metastasis.
Etiological Factors:
Gastric carcinogenesis is a multifactorial process. Following the classical
epidemiological model, it represents the interaction of three major sets of factors:
• The agent (Helicobacter pylori).
• The host.
• The external environment.
The target tissue for this interaction is the gastric mucosa.
Screening:
• In high-incidence areas: asymptomatic groups.
• In low-incidence areas: symptomatic groups
1. Dyspeptic patients.
2. Patients on Acid suppression therapy.
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
3. Patients with Helicobacter pylori infection.
4. Premalignant lesions/conditions.
Screening in low-incidence areas:
symptomatic groups
1. Dyspeptic patients:
• Dyspeptic symptoms are common in patients with EGC. It has been
suggested that 60–90% of patients with EGC have dyspeptic symptoms, as
defined by the presence of heartburn or abdominal pain or discomfort
centered in the upper abdomen.
• These symptoms are generally identical to those with benign gastric disease.
• Gastroscopy is seen as an approach to influence the stage of cancer at
diagnosis.
2. Patients on Acid suppression therapy:
• The symptoms of EGC are often cannot be differentiated from those of
benign disease.
• This group of patients may be started on treatment with acid suppression
drugs, including proton pump inhibitors and H2 blockers before referral to a
specialist or before gastroscopy.
• The diagnosis of EGC can potentially be delayed as a result of an
improvement in dyspeptic symptoms.
Patients on Acid suppression therapy:
EGC may also ‘heal’ by acid suppression, and make endoscopic identification of
the EGC impossible, even by experienced endoscopists.
‘Healing’ of a malignant ulcer has been observed within 4 weeks with proton pump
inhibitors.
However, 37% of patients with gastric cancer, who were previously taking acid
suppression therapy, were missed at index gastroscopy. This led to a mean delay in
diagnosis.
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
Primary care physicians should therefore refrain from prescribing acid suppression
drugs in patients over the age of 45 years with dyspepsia before endoscopy in order
to minimize the risk of missing EGC.
Primary care physicians should be educated on the fact that the majority of patients
with EGC have dyspeptic symptoms.
3. Patients with Helicobacter pylori infection:
• There is compelling evidence for the role of H. pylori in the initiation of
Correa’s cascade
• (Stepwise progression from Chronic Active Gastritis Atrophic Gastritis
Intestinal Metaplasia Dysplasia and finally Adenocarcinoma).
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
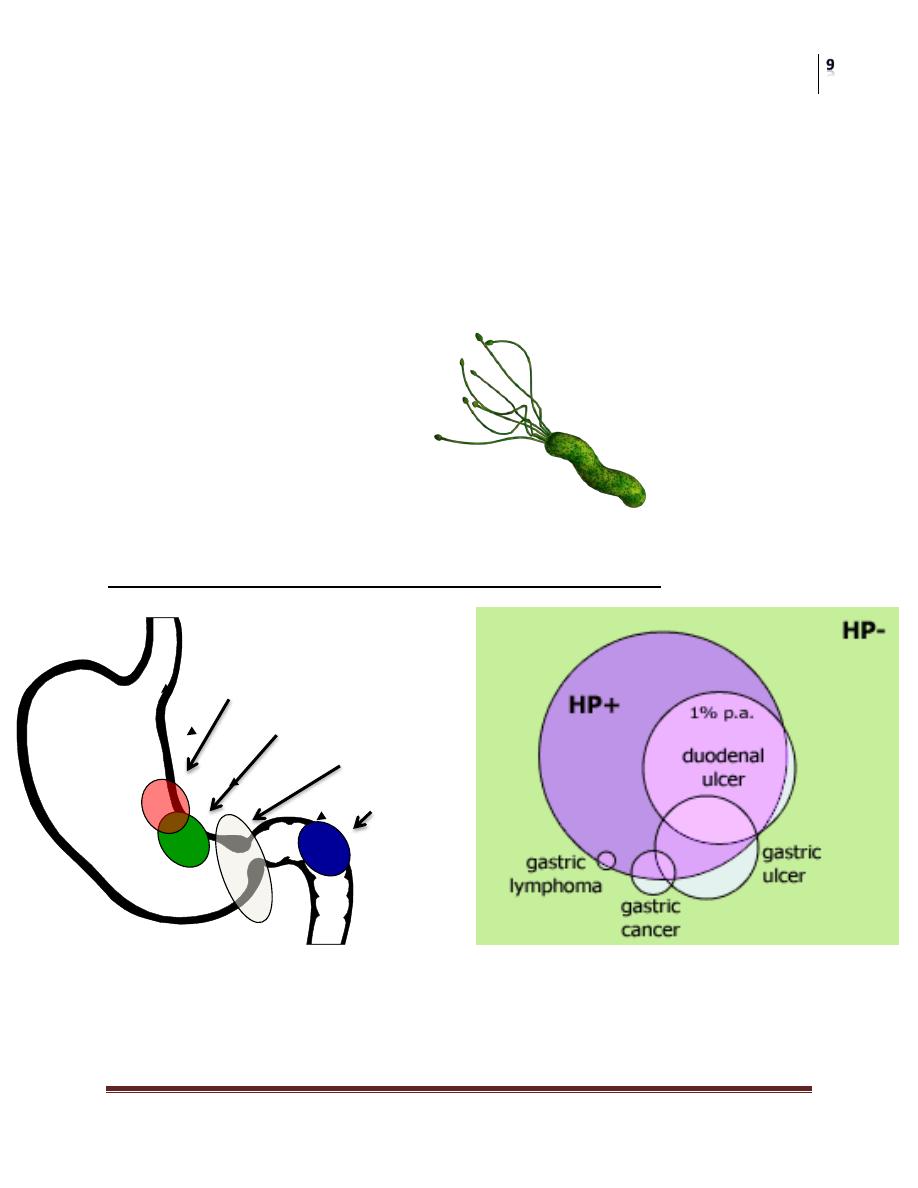
Helicobacter pylori
• Gram-negative
• Microaerophilic
• Inhabits various areas of the stomach and duodenum.
• First discovered in 1983 by Dr Barry J. Marshall and Dr J. Robin Warren.
• Marshall and Warren were awarded the 2005 Nobel Prize for Medicine &
Physiology.
Helicobacter pylori infection and gastrointestinal diseases
There is significant correlation between Helicobacter pylori infection and
duodenal/gastric ulcer and gastric malignancy
Gastric ulcers
ca 70 – 90 %
Gastric cancers
ca 60 – 90 %
H. pylori colonies
Duodenal ulcers
ca 95 %
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
• Several epidemiological studies have also indicated that populations with H.
pylori infection are at increased risk of developing gastric cancer of both
Lauren’s, intestinal and diffuse types.
• The European H pylori Study Group strongly recommended H. pylori
eradication for patients with atrophic gastritis, after gastric cancer resection,
and first-degree relatives of patients with gastric cancer.
• There are emerging data that intestinal metaplasia and atrophic gastritis
regress after H. pylori eradication.
• So H. pylori screening and treatment is an effective strategy in cancer
prevention
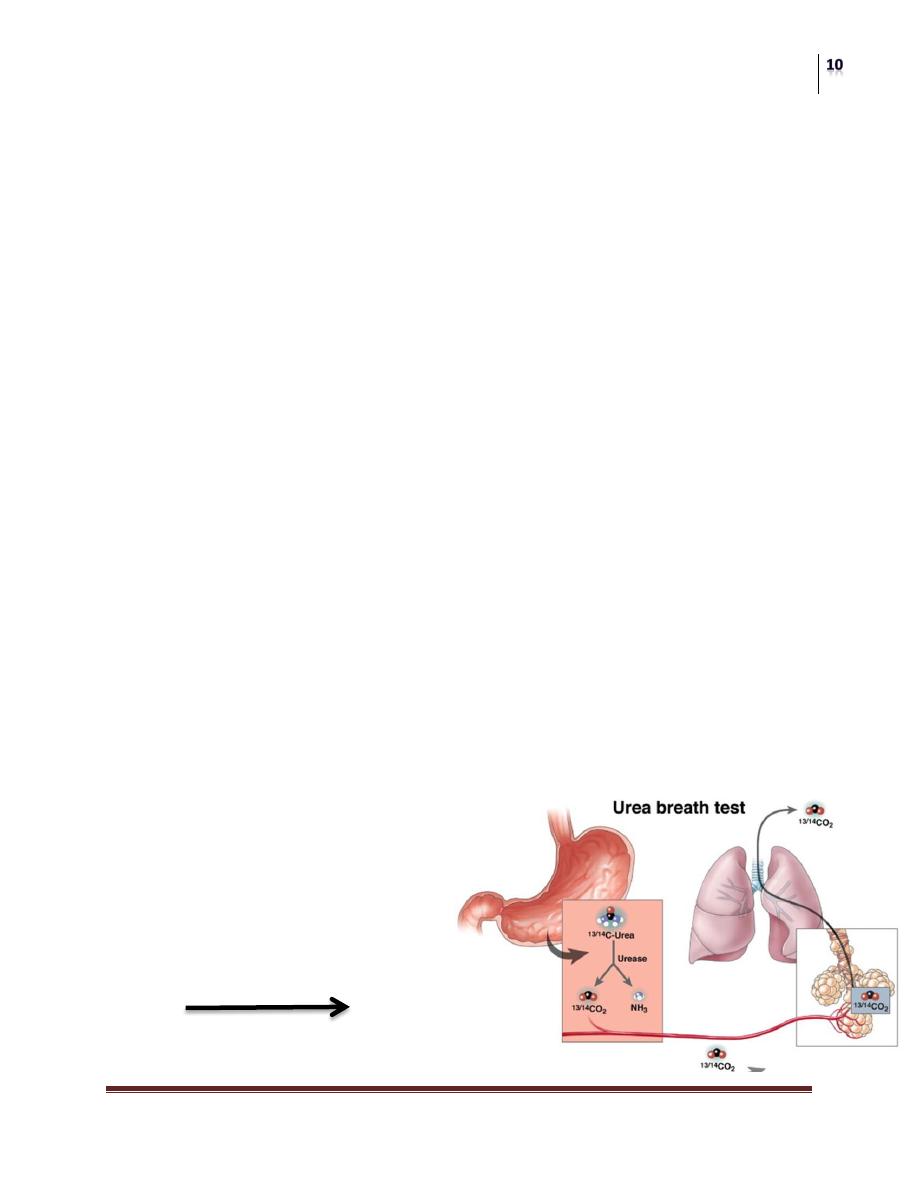
Diagnosis of H. Pylori:
Urea Breath Test
• Gold Standard for non-invasive tests for H. Pylori.
• Specificity 100%
• Sensitivity > 95%
Invasive Tests
• Gastroscopy
1. Rapid Urease Test (RUT)
2. Histology
3. Culture
• Serology
1. Antibody Test
2. PCR
Non-invasive Tests
• Urea Breath Test (UBT)
– 13C & 14C
• Antigen Test (Stool)
• Urine Test
H
2
N(
13/14
CO)NH
2
+ H
2
0
Urease Enzyme
2NH3 + 13/14CO2

Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
Urea Breath Test
The Heliprobe
®
System
Performance of Urea Breath Test
1. Swallow HeliCap™ with water.
2. After 10 min exhale into BreathCard™ until indicator changes colour.
3. Insert BreathCard™ in the Heliprobe
®
Analyzer and press Start (green
button).
4. Result will be displayed after some minutes.
Heliprobe 0 = patient not infected
Heliprobe 1 = borderline
Heliprobe 2 = patient infected
Heliprobe
®
Analyzer
HeliCap
TM
BreathCard
TM
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
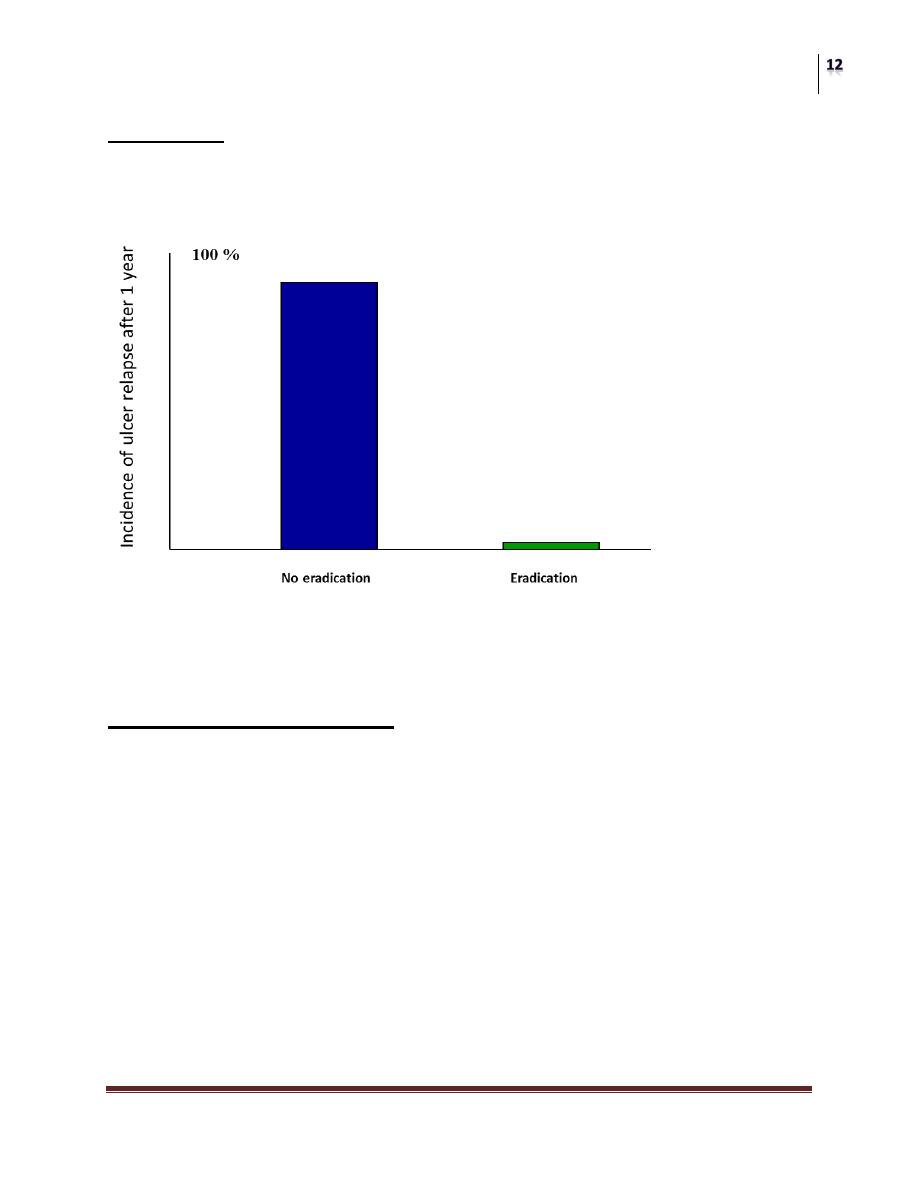
Treatment
Eradication of Helicobacter pylori significantly reduces the recurrence of gastric
ulcers
Treatment of gastric ulcer in H. pylori positive patients
Treatment and Eradication
• Triple Regimen
1. Bismuth + Tetracycline + Metronidazole
2. Clarithromycin + Amoxicillin + PPI
• Quadruple Regimen
1. Bismuth + Tetracycline + Metronidazole + PPI
2. LOAD (Levofloxaxin + Omeprazole + Nitazoxanide + Doxycycline)
• Sequential Therapy
PPI + Amoxicillin (days 1-5) followed by PPI + Clarithromycin + Tinidazole
(days 6 – 10)
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
4.
Premalignant lesions/conditions
• Chronic gastritis and chronic atrophic gastritis.
• Intestinal metaplasia.
• Non-invasive neoplasia.
• Gastric polyps.
• Postgastrectomy.
• Family history.
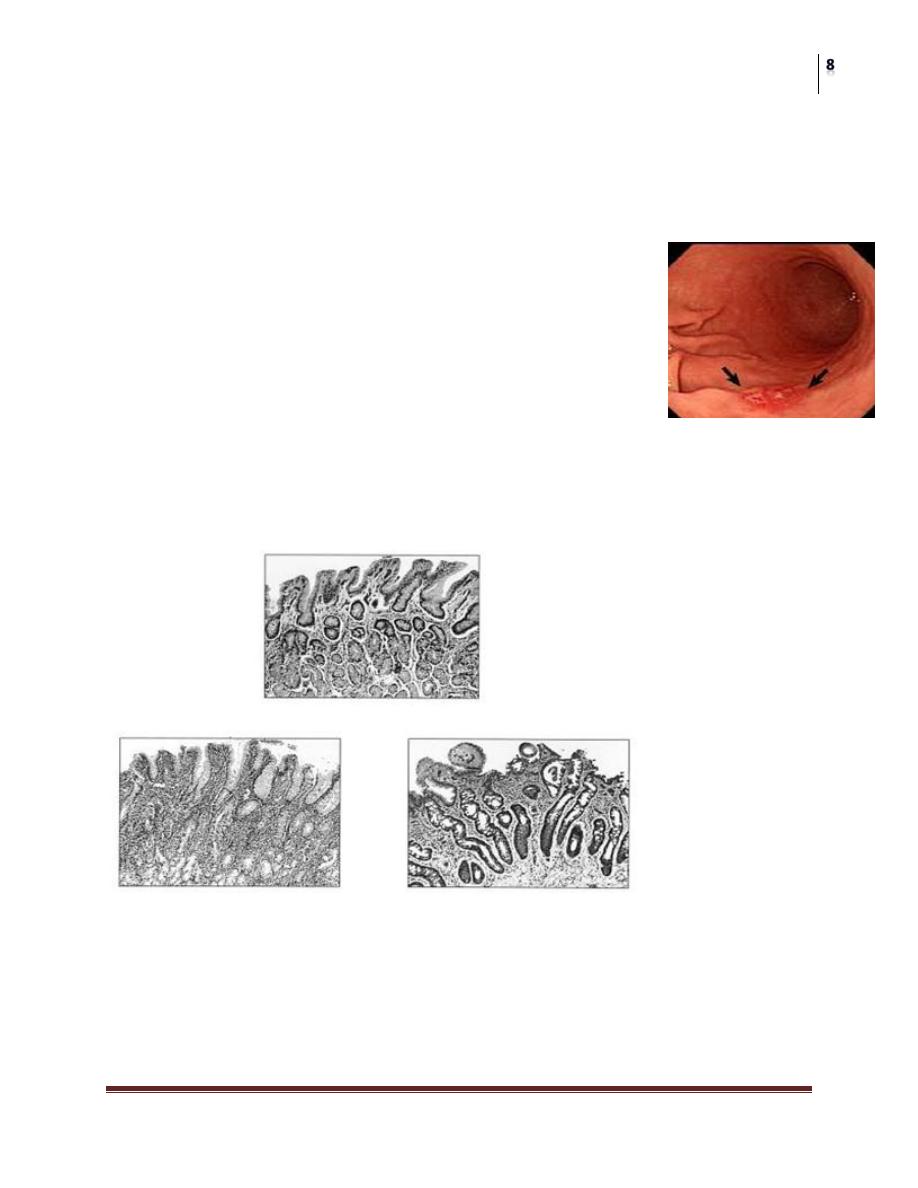
Advances in endoscopic techniques
Recent advances in endoscopic technology have improved the sensitivity of
detecting EGC.
1. Chromoendoscopy:
Using non-absorbable dye such as indigo carmine
This involves spraying the dye over the gastric mucosa to enhance tissue
irregularities and therefore facilitate the identification and biopsy of abnormal
areas.
2. Magnifying endoscopy:
(Capable of magnifying approximately 80) is useful in assessing gastric lesions at
the level of microvascular architecture and thus providing the possibility of
predicting the histological nature of the cancer.
3. Light-induced fluorescence endoscopy:
Is promising as a useful adjunct to conventional white-light endoscopy. Have
sensitivity and specificity of 94 and 86%, respectively, for this spectroscopic
technique in detecting EGC
4. The infrared video endoscope:
Is another new technique whereby infrared light gives deeper tissue penetration
and therefore the possibility of obtaining information about the submucosal aspect
of EGC.
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
Biomarkers for gastric cancer:
1. Serum Pepsinogen level.
2. Anti H pylori antibody.
3. Serum Gastrin-17.
Serum Pepsinogen level:
It has been demonstrated that serum pepsinogen levels are useful for the screening
of atrophic gastritis and a low PGI/PGII ratio is predictive of an increased risk of
gastric cancer.
Anti H pylori antibody:
• H. pylori serology is a useful screening tool for dyspeptic patients under the
age of 45 years with a sensitivity of 97% and specificity of 87%.
• Individuals with a negative test can safely be excluded from having
endoscopy.
• Combination of H. pylori antibody and pepsinogen was demonstrated to be a
valid screening biomarker in predicting the likelihood of gastric cancer
development, and who should be subjected to a close endoscopic follow-up.
Serum Gastrin-17
• Gastrin is synthesized in G cells found in the antrum.
• Over 90% of the gastrin secreted is of type G-17.
• In cases of atrophic gastritis, the loss of antral G cells will result in low
gastrin levels despite an achlorhydric stomach.
• A combination of pepsinogen and gastrin levels in connection with H. pylori
antibody status can effectively identify different types of atrophic gastritis
with a sensitivity and specificity of 90% and 93%, respectively.
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
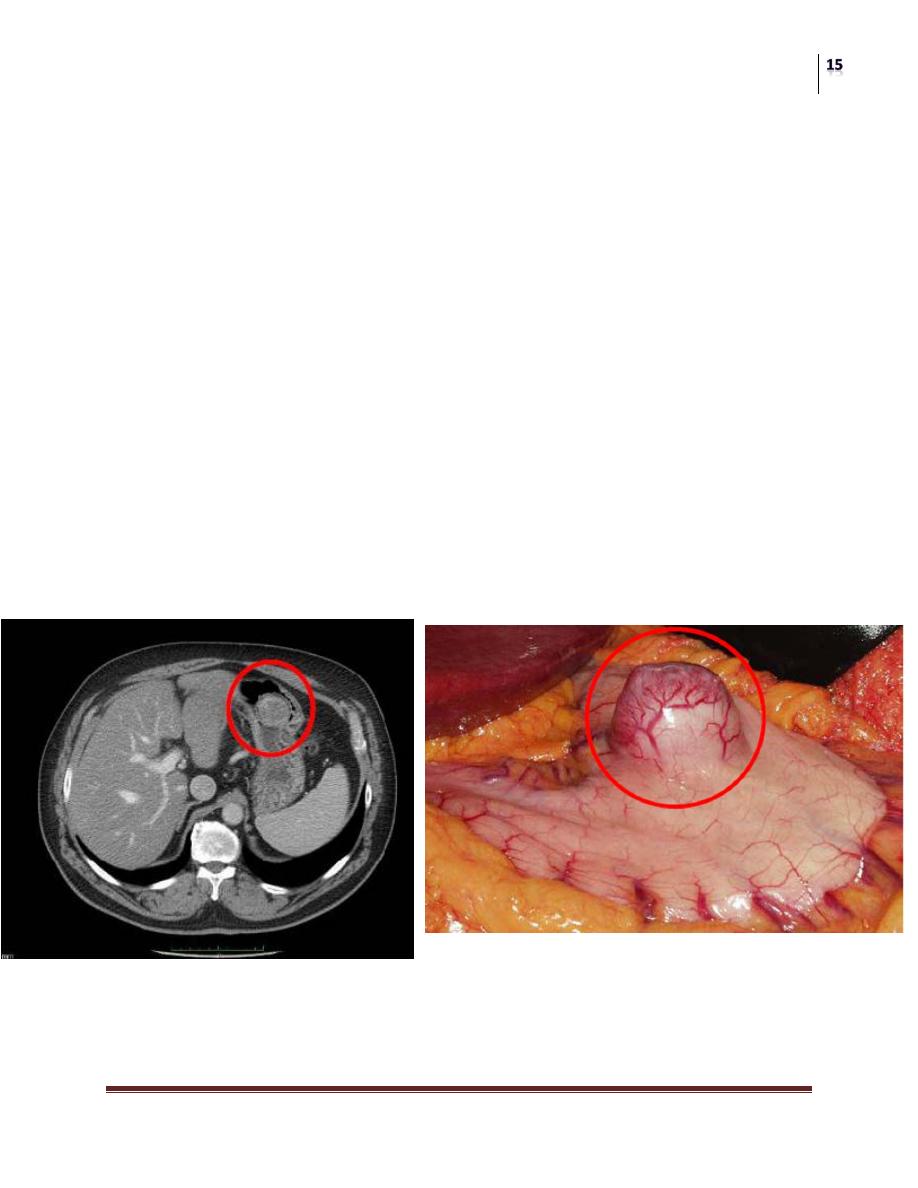
GIST
Gastro intestinal stromal tumor
Background: GIST
• Localized disease
– 5 year survival rate < 50%.
• Metastatic GIST
– median survival prior to tyrosine kinase inhibitors (TKIs) was 12-19
months
• GISTs are chemo- resistant to conventional chemo and radiotherapy
• Introduction of TKIs has revolutionized the treatment and prognosis of
patients with GISTs
Role of Surgery in Primary Disease
• Surgery is the principal treatment and the only curative therapy for localized,
resectable primary disease
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
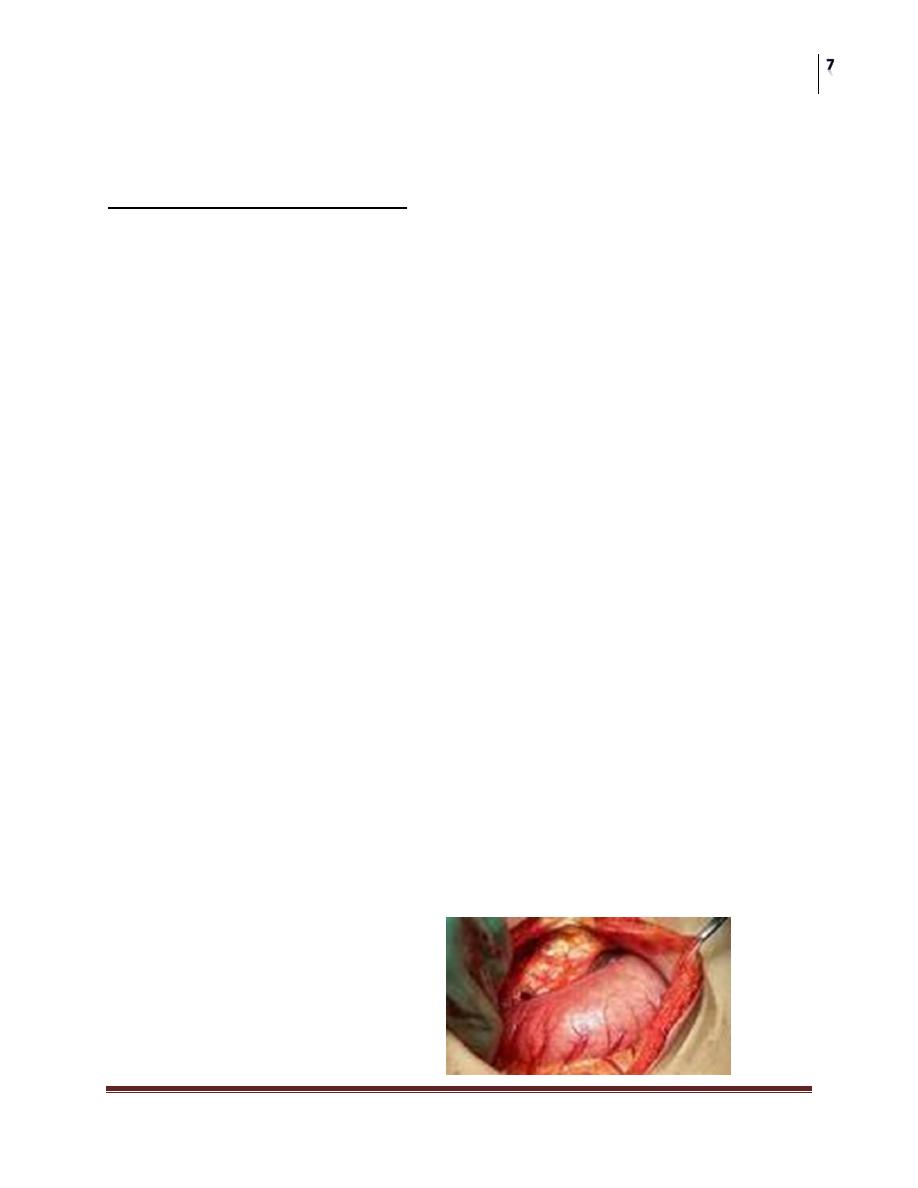
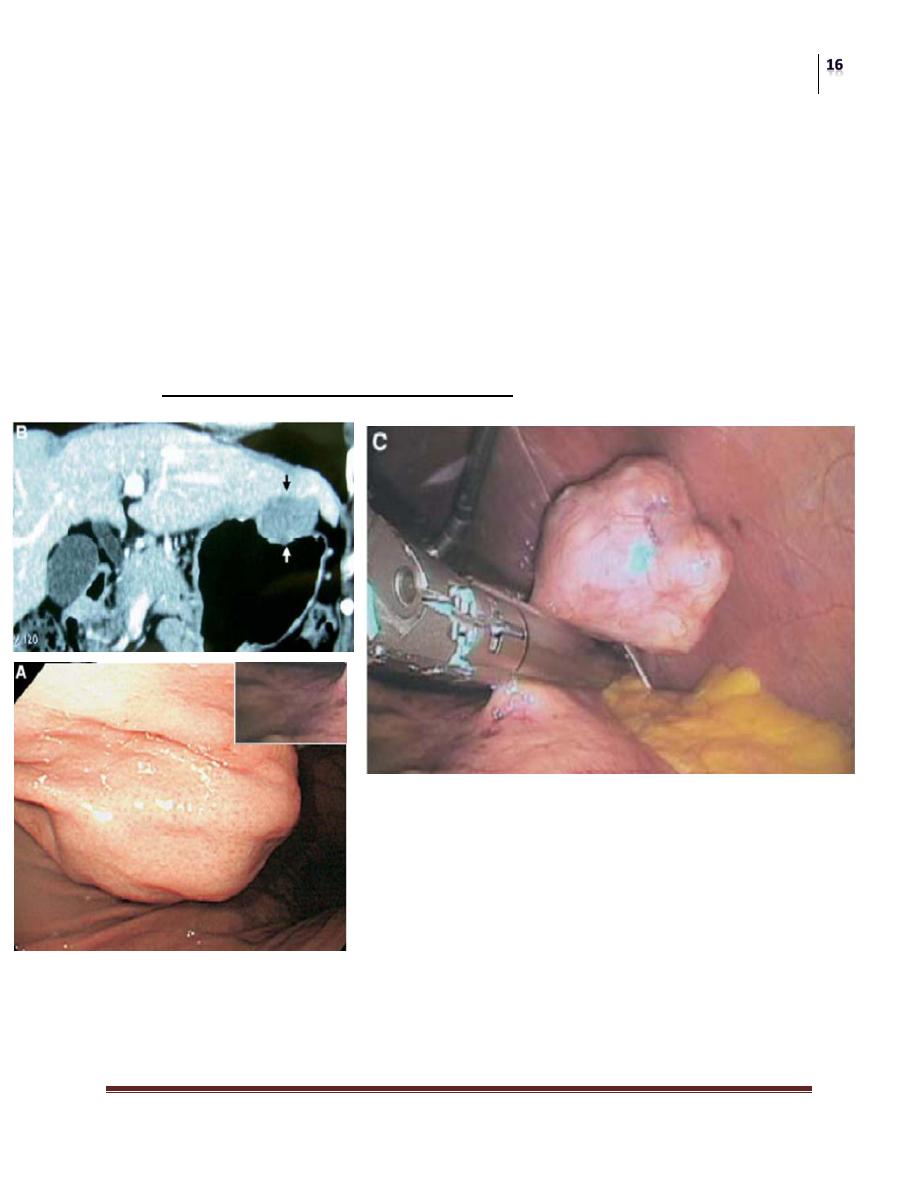
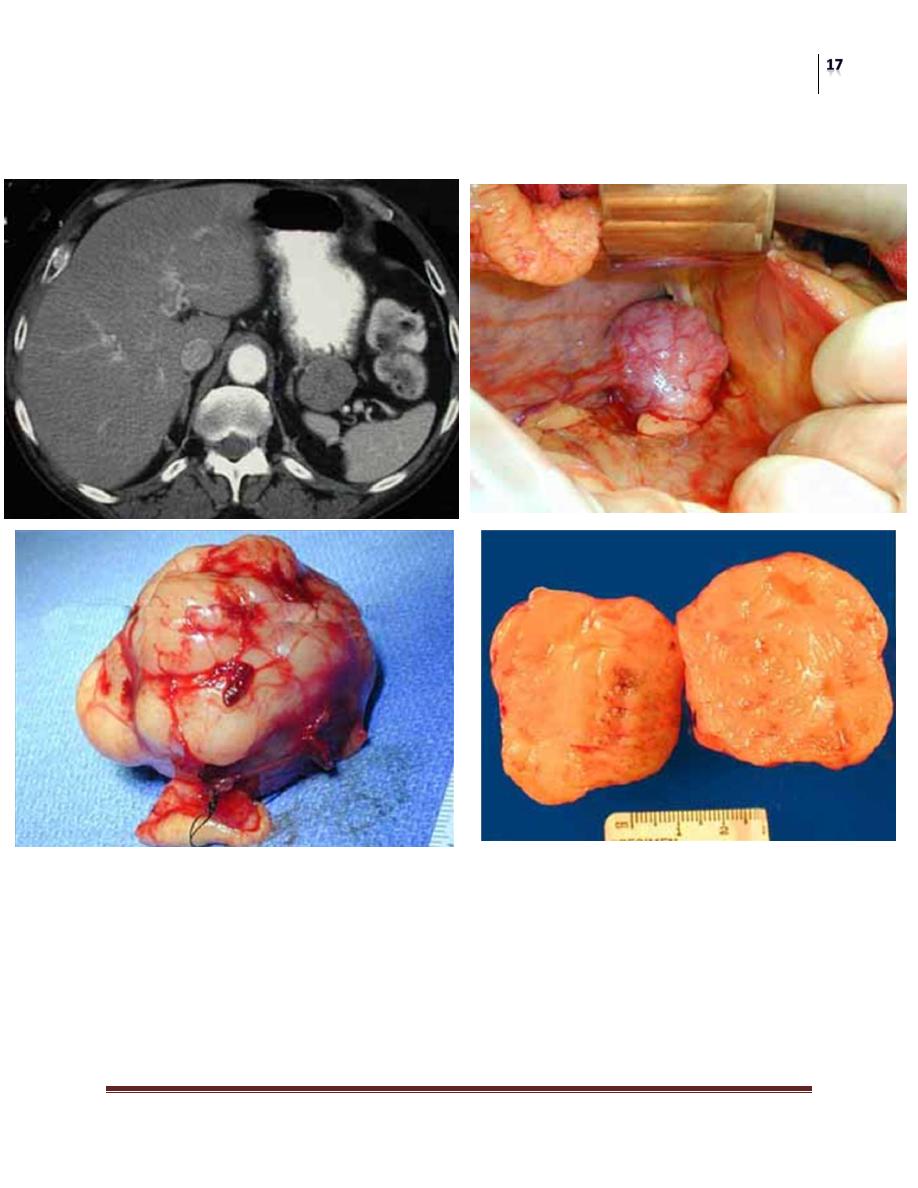
Surgical Treatment of primary GIST
Pearls for the Surgeon
• GIST lesions are highly vascularized and have a fragile pseudocapsule
– Minimize the risk of tumor rupture
• GIST rarely involve regional nodes
– Lymphadenectomy not necessary
– The margins of resection from the tumor specimen should be carefully
oriented and examined
Gastric GIST: Laparoscopic Approach
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
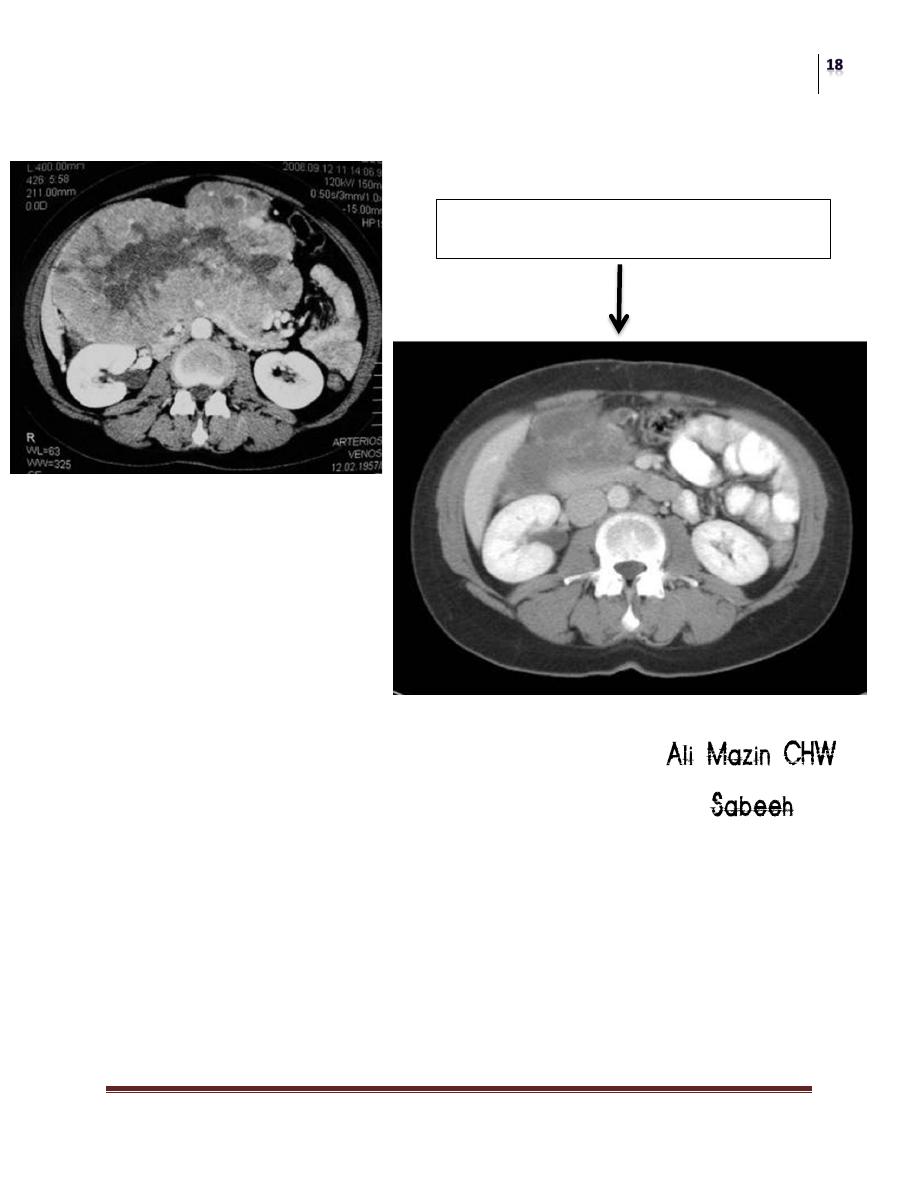
Gastric GIST
Surgery
Gastric Cancer
Dr. Aqeel Shakir
Lec. 4
Inoperable Disease
Treatment of Gastric Cancer
• Surgery
• Chemotherapy
• Radiotherapy
Conclusion:
• Although a multifactorial etiology Is acknowledged, the main factors are
infection with H. pylori
• The precancerous process is very prolonged, usually lasting several decades.
Its intermediate steps are well-characterized histopathologically and may be
reversible.
• A strategy of H. pylori screening and eradication will probably reduce
gastric cancer incidence.
6 Months after Imatinib
