Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Structural and Functional Anatomy
280cm long.
Jejunum begins at LOT, no clear demarcation to ileum.
Jejunum has long vas recta, large plicae, thick walls, transparent mesentery.
Ileum has short vasa, small plicae, and thin walls, fat in the mesentery.
Mesentery attaches the small intestine to the posterior abdominal wall.
Contains nerves, blood vessels, lymphatics, lymph nodes, and fat.
Lymph tissues known as Peyer’s patches are abundant.
SMA supplies the midgut structures (duodenum distal to the ampulla,
pancreas, small intestine, ascending and transverse colon.)
Histology
Four layers.
Mucosa turns over every 3-7 days.
Submucosa contains vessels, nerves, lymph, Meissner’s plexus. This layer
provides the major strength when suturing.
Muscularis outer long layer, inner circ layer.
Adventitia is a layer of visceral peritoneum
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Physiology (CHO)
Daily CHO load is 350g of starch, lactose, sucrose.
Initial enzyme digestion is by pancreatic and salivary amylase.
CHO broken down to monosaccharides by microvilli
Physiology (Protein)
The jejunum is responsible for 80-90% of protein absorption.
Proteins are converted by acid and pepsin from stomach to polypeptides.
Acid is neutralized and pepsin is inactivated as chyme enters the duodenum.
Trypsinogen is activated from pancreas to trypsin by enterokinase in the
duodenum.
Trypsin activates chymotrypsin and elastase, further digesting polypeps.
Amino acids and dipeptides are absorbed
Physiology (Fats)
Emulsification begins in the stomach.
Fat enters the duodenum, where pancreatic and biliary secretions mix.
Lipase breaks down fats in to monoglycerides, which are absorbed by
diffusion.
In epithelial cells, triglycerides are resynthesized; chylomicrons are formed
and enter the lymphatic system thru small lacteals.
Bile salts are reabsorbed in the ileum.
Most of the excreted fat comes from desquamated cells and bacteria
Physiology (H2O, Lytes, Minerals, Vitamins)
Iron is absorbed mainly in the duodenum.
Most minerals and water soluble vitamins absorbed in jejunum.
B12 is absorbed only in terminal ileum.
Of the 5-10 liters entering the small bowel, only 500cc enter the colon.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
The Job of the Bowel
To digest food (involves a corrosive solution and potentially pathogenic
bacteria).
To absorb the food into the blood while keeping the corrosive substances
and the bacteria inside the gut.
To keep the solution moving down the bowel at the right rate for digestion
and absorption.
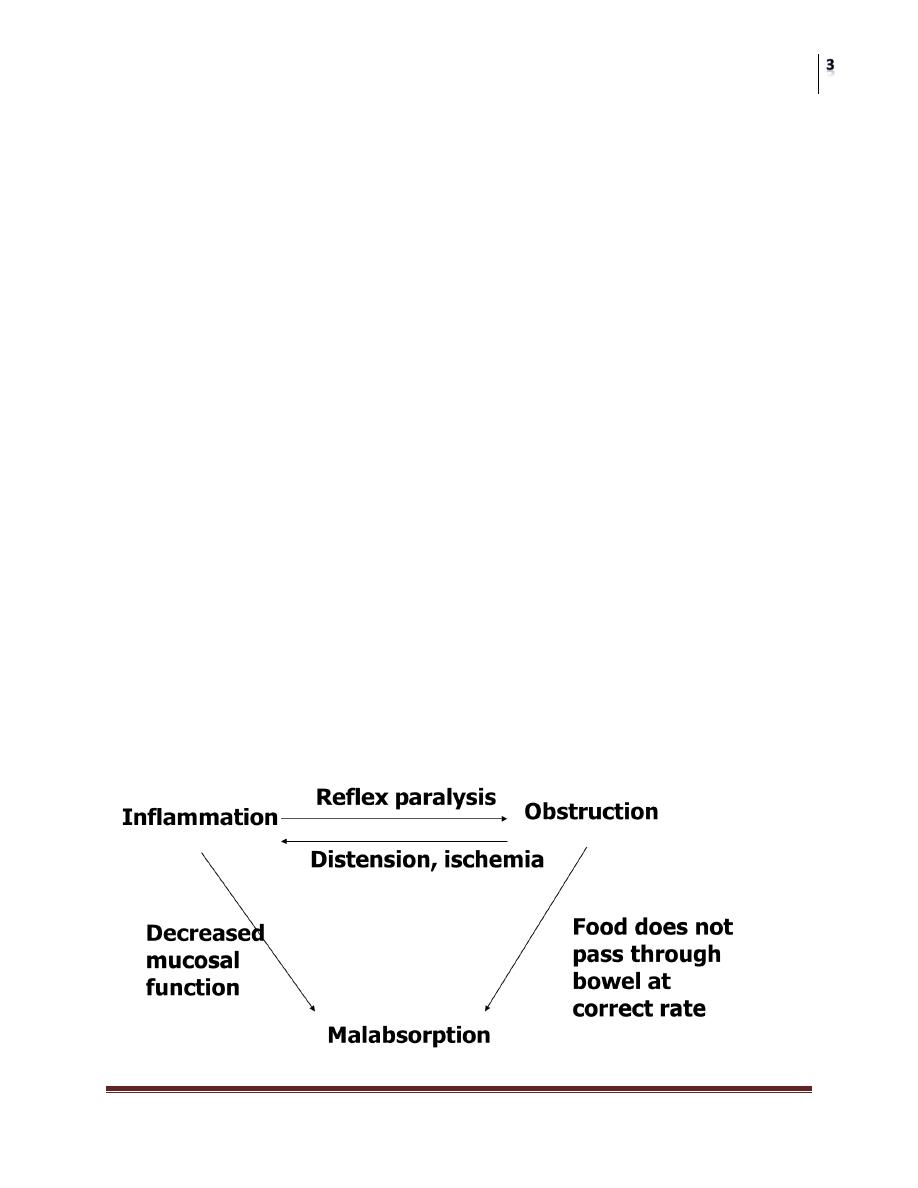
Problems that Affect Bowel Functions
Inflammation and damage to the bowel wall
Hemorrhage
anemia
Perforation
peritonitis
Decreased mucosal function
malabsorption
Decreased bacterial containment
sepsis
Malabsorption
Malnutrition, dehydration, electrolyte imbalances
Obstruction
Malabsorption
Compartment syndrome
ischemia
Bowel Problems: Interrelationships

Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Consequences of Small Bowel Resection
Frequently improve with time.
Can often be adequately treated with dietary changes and antiperistaltic
medications.
Diarrhea can result from water overload in colon.
Malabsorption (Steatorrhea).
Irritation of colonic mucosa by bile salts that haven't been reabsorbed by
terminal ileum.
Bacterial overgrowth in the small intestine may occur after resection of the
ileocecal valve (“ileal brake”) and can lead to deconjugation of bile salts in
the small intestine.
Alterations in H2O and lytes absorption lead to net secretion instead of
absorption.
Fermentation of CHO leads to gas production
These lead to bloating, diarrhea, and steatorrhea.
Nutritional deficiencies- B12 supplementation should be provided after
resection terminal ileum
Cholelithiasis may result from bile acid malabsorption after ileal resection.
Renal stones- fat malabsorption leads to calcium binding of fat in the colon.
This leaves oxalate free to form water soluble absorbable salts excreted in
the urine.
Short Bowel Syndrome
Inadequate length of intestine.
Generally occurs when more than 50% of the small intestine is resected or if
less than 100cm remains.
Leads to diarrhea, steatorrhea, weight loss, nutritional deficiencies,
hypergastrinemia.
If the terminal ileum and valve are retained, 70% can be resected.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Motility
The order of recovery of bowel function after surgery is:
1. Small bowel
2. Colon
3. Stomach
DIVERTICULAR DISEASE
Types
Diverticula can occur in a wide number of positions in the gut, from the
oesophagus to the rectosigmoid. There are two varieties:
1. Congenital. All three coats of the bowel are present in the wall of the
diverticulum, e.g. Meckel’s diverticulum.
2. Acquired. The wall of the diverticulum lacks a proper muscular coat. Most
alimentary diverticula are thought to be acquired.
Duodenal diverticula
There are two types:
1. Primary.
Mostly occurring in older patients on the inner wall of the second and third parts,
these diverticula are found incidentally on barium meal and are usually
asymptomatic.
They can cause problems locating the ampulla during endoscopic retrograde
cholangiopancreatography (ERCP).
2. Secondary.
Diverticula of the duodenal cap result from longstanding duodenal ulceration.
Jejunal diverticula
These are usually of variable size and multiple. Clinically, they may be:
1. Symptomless,
2. Give rise to abdominal pain,
3. Produce a malabsorption syndrome or present as an acute abdomen with
acute inflammation and occasionally perforation.

Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
4. They are more common in patients with connective tissue disorders. In
patients with major malabsorption problems giving rise to anemia,
steatorrhoea, hypoproteinaemia or vitamin B12 deficiency, resection of the
affected segment with end-to-end anastomosis can be effective.
Meckel’s diverticulum
Is present in 2% of the population; it is situated on the anti-mesenteric
border of the small intestine,
Commonly 60 cm from the ileocaecal valve, and is usually 3–5 cm long.
Many variations occur (2% – 2 feet – 2 inches is a useful aide-mémoire).
Possesses all three coats of the intestinal wall and has its own blood supply.
It is therefore vulnerable to infection and obstruction in the same way as the
appendix. It should be sought when a normal appendix is found at surgery
for suspected appendicitis
If a silent Meckel’s is found incidentally during the course of an operation, it
can be left alone provided it is wide mouthed and not thickened.
In 20% of cases, the mucosa contains heterotopic epithelium, namely gastric,
colonic or sometimes pancreatic tissue, If ectopic gastric epithelium is
present within the diverticulum, it may be the source of gastrointestinal
bleeding.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Signs and Symptoms
In order of frequency, these symptoms are as follows:
1. Severe hemorrhage, caused by peptic ulceration. Painless bleeding occurs
per rectum and is maroon in color.
2. Intussusception. In most cases, the apex of the intussusception is the
swollen, inflamed, heterotopic epithelium at the mouth of the diverticulum.
3. Meckel’s diverticulitis. May be difficult to distinguish from the symptoms
of acute appendicitis. When a diverticulum perforates, the symptoms may
simulate those of a perforated duodenal ulcer.
4. Chronic peptic ulceration. As the diverticulum is part of the mid-gut, the
pain, although related to meals, is felt around the umbilicus.
5. Intestinal obstruction. The presence of a band between the apex of the
diverticulum and the umbilicus may cause obstruction either by the band
itself or by a volvulus around it.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
‘Silent’ Meckel’s diverticulum
An aphorism attributed to Dr Charles Mayo is:
‘a Meckel’s diverticulum is frequently suspected, often sought and seldom
found’.
A Meckel’s diverticulum usually remains symptomless throughou life and is
found only at necropsy.
When a silent Meckel’s diverticulum is encountered in the course of an
abdominal operation, it can be left provided it is wide mouthed and the wall
of the diverticulum does not feel thickened. Where there is doubt and it can
be removed without appreciable additional risk, it should be resected.
Exceptionally, a Meckel’s diverticulum is found in an inguinal or a femoral
hernia sac – Littre’s hernia.
Meckel’s diverticulum can be very difficult to demonstrate by contrast
radiology; small bowel enema would be the most accurate investigation.
Technetium-99m scanning may be useful in identifying Meckel’s
diverticulum as a source of gastrointestinal bleeding.
Meckel’s diverticulectomy
A Meckel’s diverticulum that is broad based should not be amputated at its
base and invaginated in the same way as a vermiform appendix, because of
the risk of stricture.
Furthermore, this does not remove heterotrophic epithelium when it is
present. Alternatively, a linear stapler device may be used.
Where there are indurations of the base of the diverticulum extending into
the adjacent ileum, it is advisable to resect a short segment of ileum
containing the diverticulum, restoring continuity with an end-to-end
anastomosis.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Crohn’s Disease
Chronic, transmural, inflammatory process primarily affecting young
individuals.
Also known as regional enteritis, terminal ileitis, and granulomatous
ileocolitis.
Incurable condition requiring ongoing medical management and frequent
surgical interventions.
Long term pain and disability
Frequency
cases per 100,000, incidence increasing in adults and children
Males and females equally affected
Peak age of onset is between 2
nd
and fourth decades, but 5% of cases under
5y
More common in Ashkenazi Jews, white populations
Positive family history in 10-15%, suggesting a genetic predisposition
Relative risk of first degree relatives of these patients developing the disease
is 10-21 times greater than general population
Etiology
Unknown, but many hypotheses
Likely multifactorial, involving an infectious agent, environmental
exposure activating an immune response in a genetically susceptible host
The first gene locus linked to Crohn’s was the IBD1 gene on Chr 16
Bacterial agents have long been thought to be involved in the pathogenesis
of the disease although none identified as of yet.
Environmental factors such as smoking, second hand smoke have been
linked to the development of Crohn’s
HLA-DR2 and DRB1 associated with UC not Crohn’s
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Pathology
Characteristically progresses in a discontinuous manner with affected bowel
interspersed with normal bowel
Mouth to anus
Most common site terminal ileum (40%), colon only (35%), small bowel
only (20%), perianal (5%). Appendix often involved. Rectum frequently
spared
Anal involvement may be characterized by fissures (most common),
abscesses,or fistulae. Most are off midline, not the usual posterior midline.
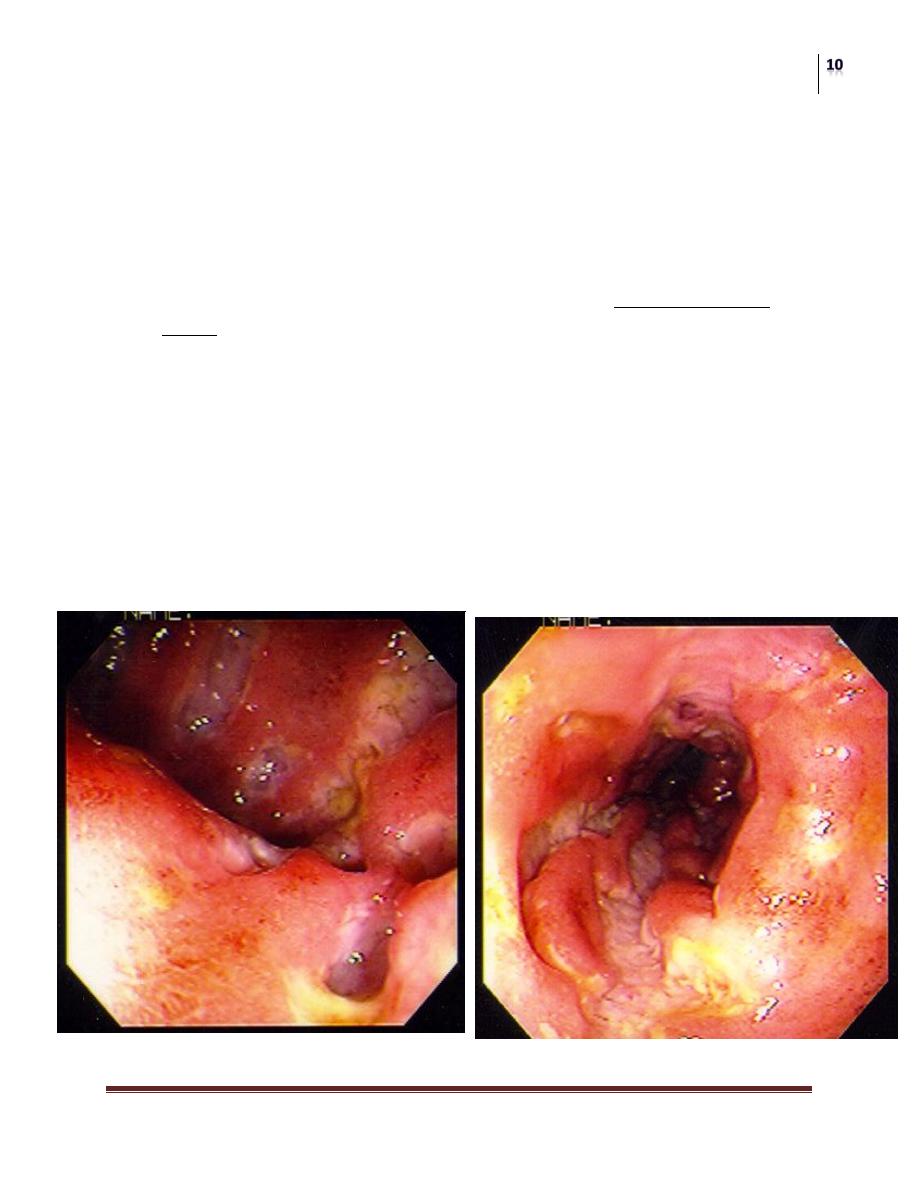
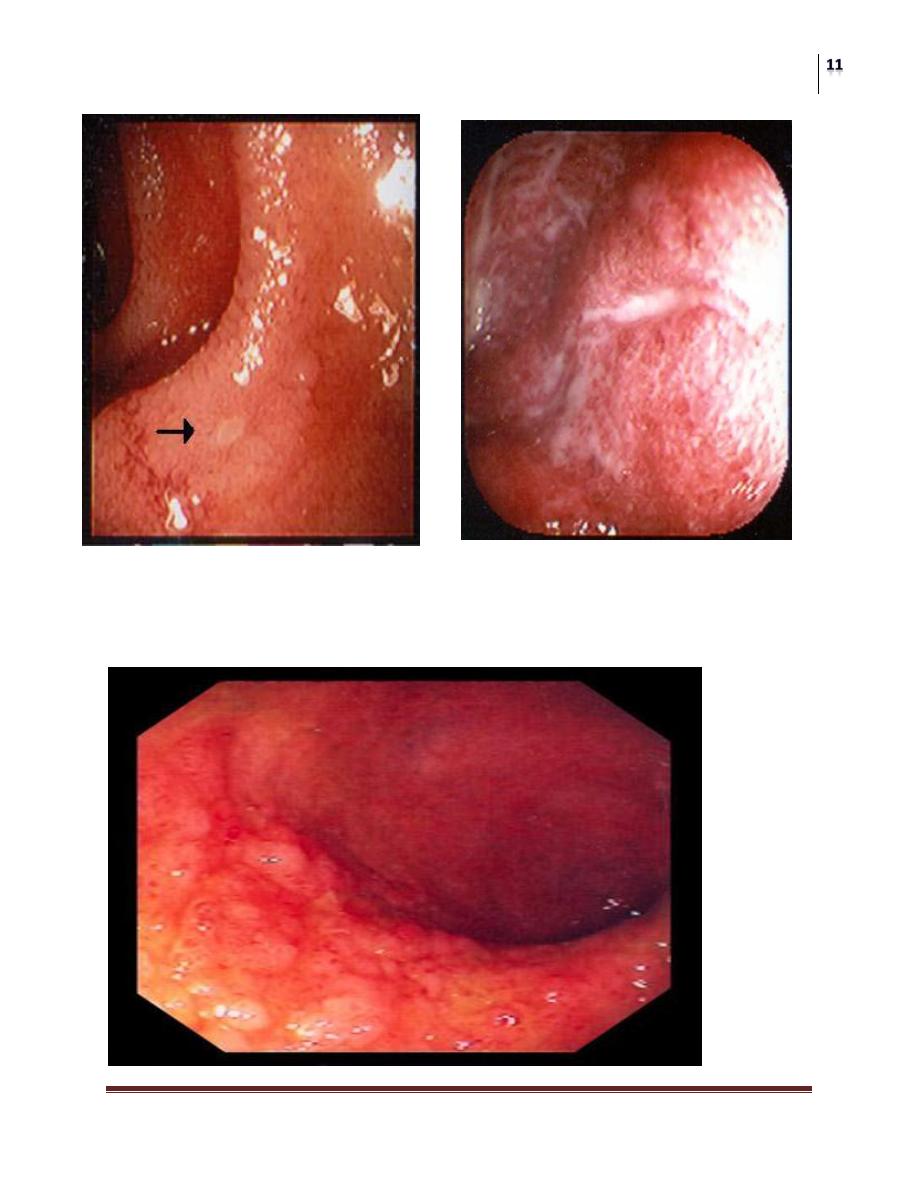
Endoscopically appears as patchy areas of inflammation separated by
uninvolved bowel “Skip”. The earliest lesions are apthous ulcers, tiny
erosions that typically occur over lymphoid follicles
Progress to lineal ulcers, which cross over transverse folds causing the
“cobblestone appearance”
Ulcers
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
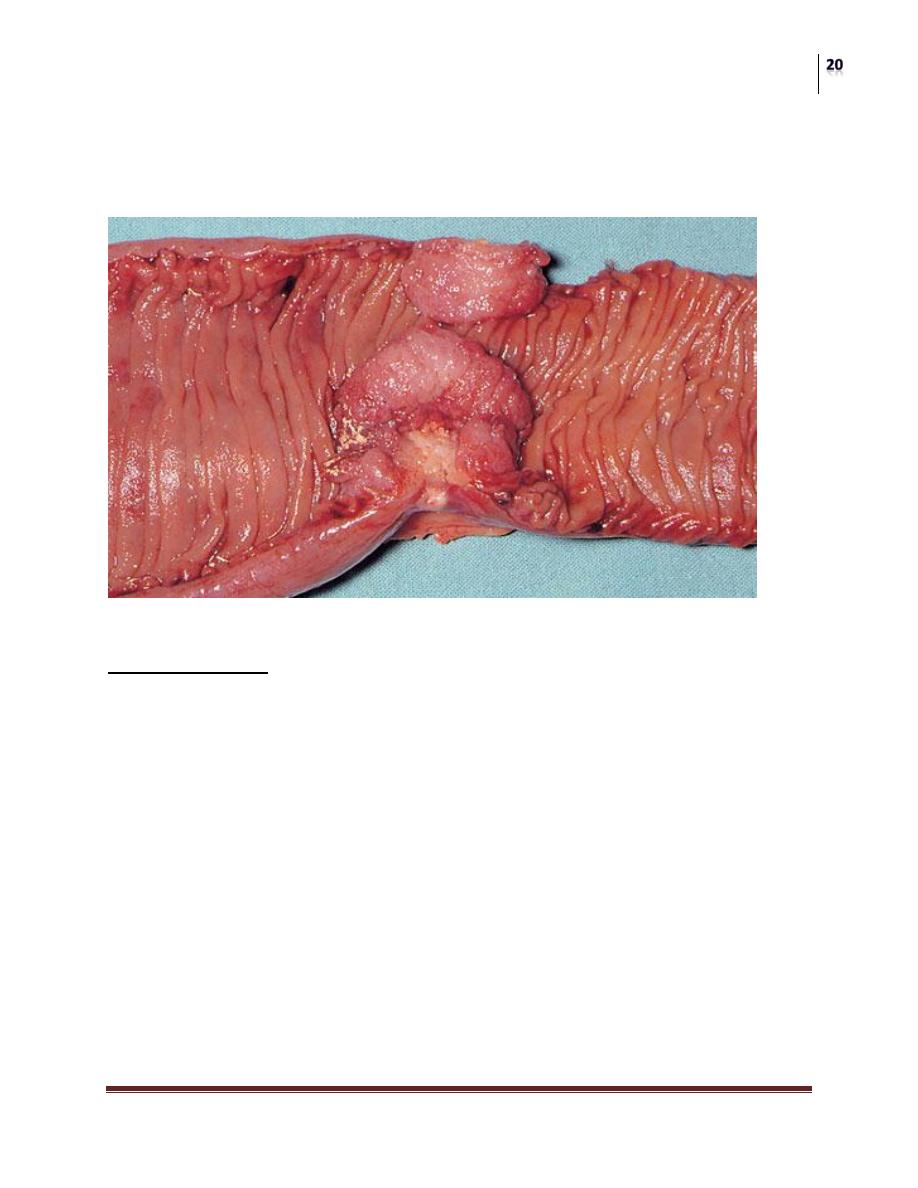
Cobblestone
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
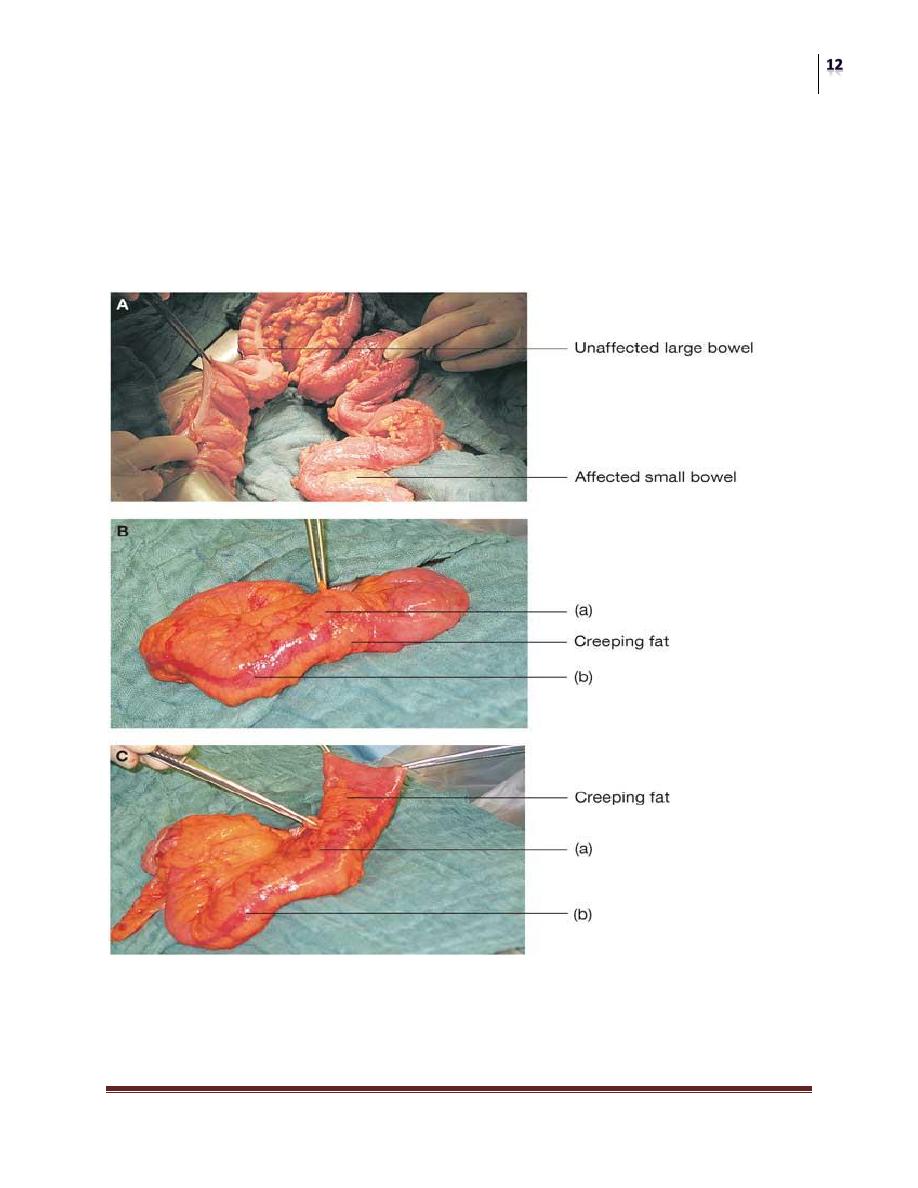
Pathology
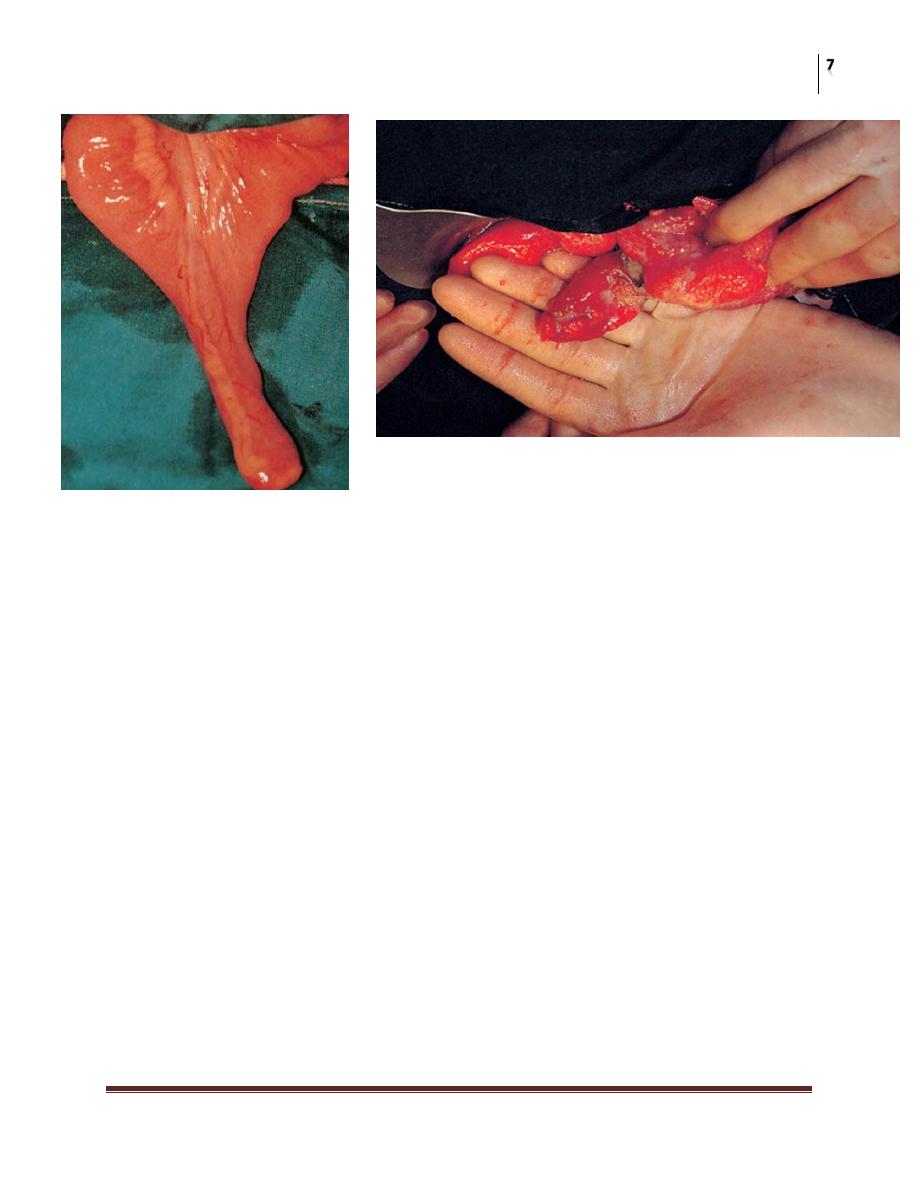
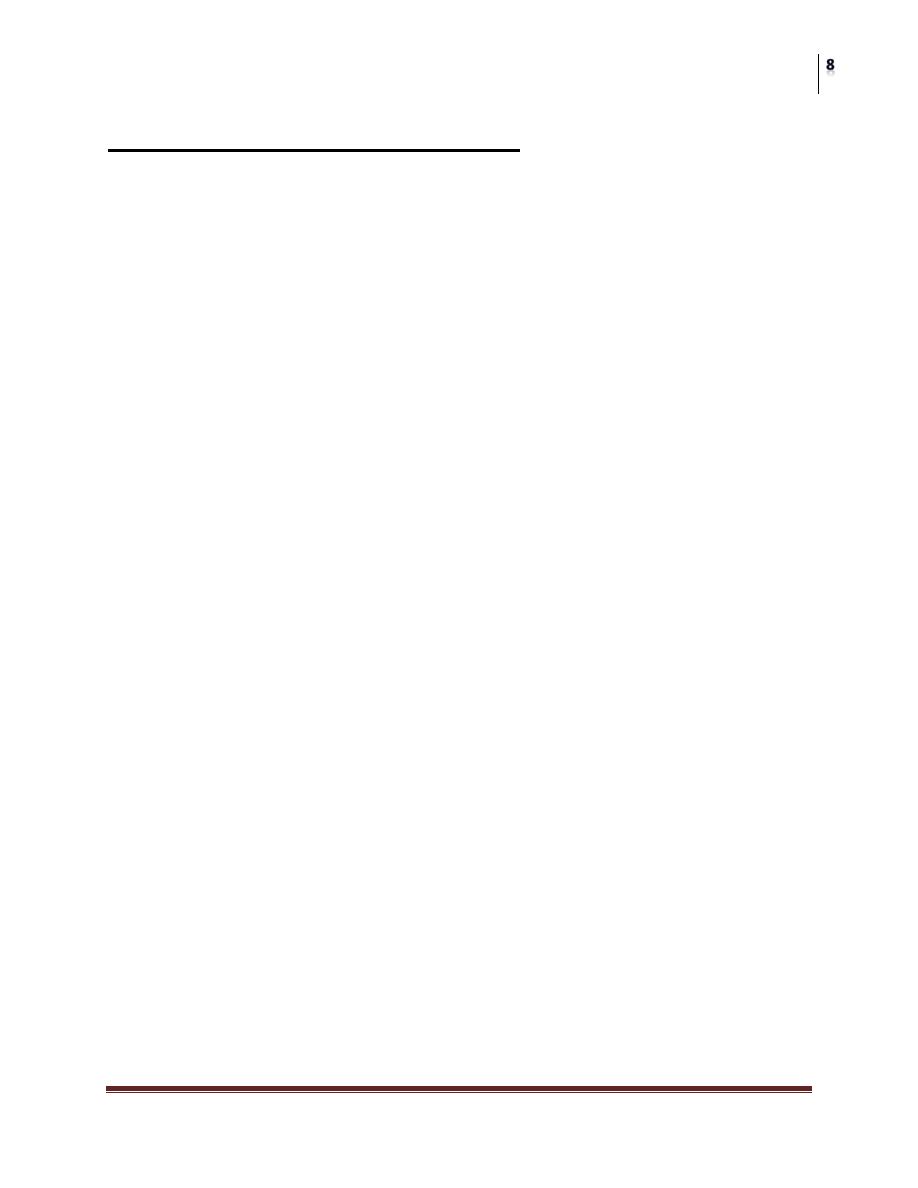
Grossly, surgical specimens are rigid, thickened as a result of chronic
inflammation and fibrosis during healing periods
Mesentery is thickened and shortened, may surround the bowel “creeping
fat”
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Because of the transmural nature of the disease, fistulous connections can
occur to other bowel or organs.
Non-caseating granulomas are found in lamina propria or submucosa in 50%
of patients.
Fibrosis may lead to strictures
Clinical Features
Intestinal manifestations:
1. Diarrhea
2. Pain
3. Anorexia
4. Nausea, weight loss
5. Perirectal disease
6. Bleeding is uncommon in comparison to UC
Extraintestinal manifestations
1. Arthritis
2. Erythema nodosum, multiforme
3. Pyoderma gangrenosum
4. Sclerosing cholangitis, cholelithiasis
5. Renal calculi
6. Endocrine disorders (growth, amenorrhea), ocular disease
Clinical Patterns
Acute Crohn’s disease
Chronic Crohn’s disease
1. Enteroenteric fistulae
2. Enterocutaneous fistulae
Anal disease
Diagnosis
Combination of laboratory, radiological, pathologic examinations
Differential includes bacterial enteritis, viral enteritis, and ulcerative colitis,
among others.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Labs may show anemia, malnutrition, increased ESR
B12 anemia, iron deficiency, folic acid deficiency
Deficiencies in copper, selenium, zinc common
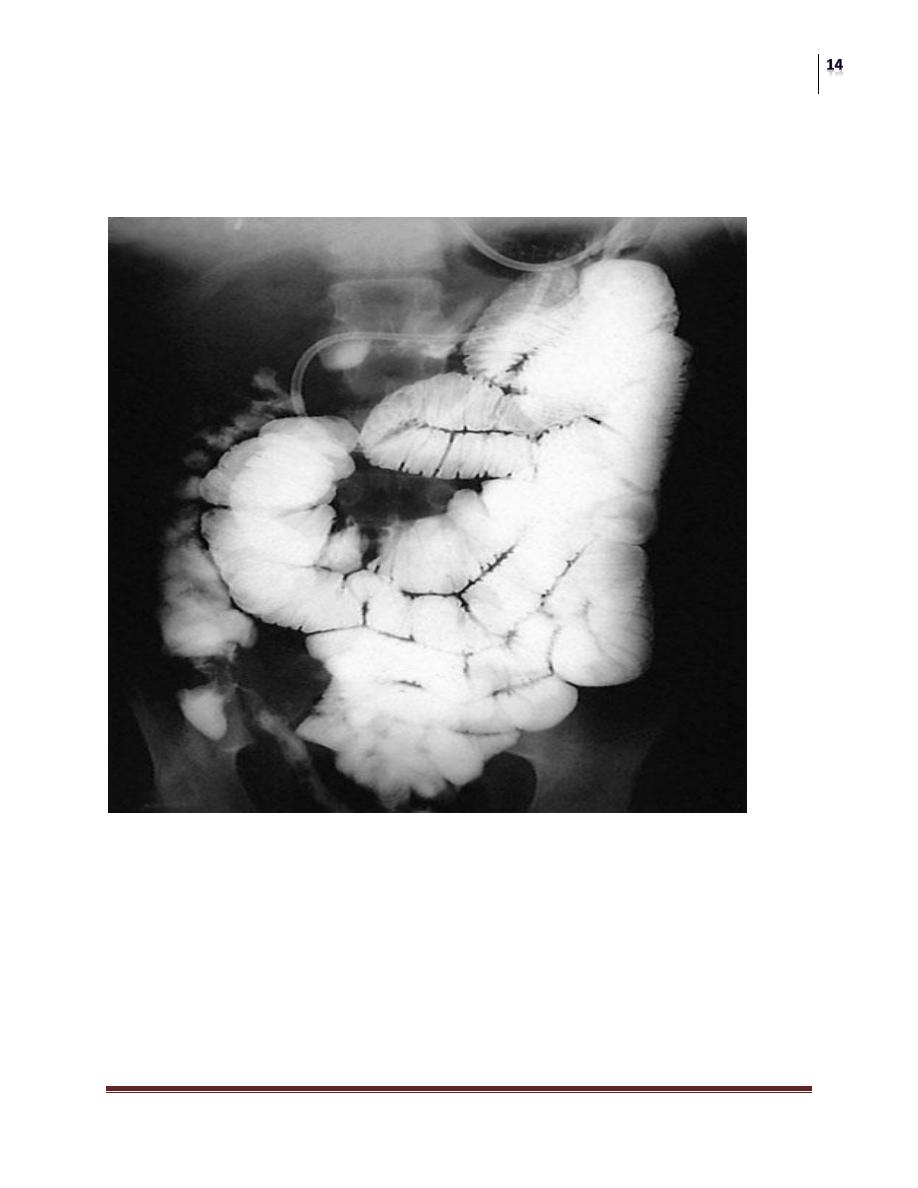
Work-up
Colonoscopy
UGI series with small bowel follow thru
CT scan
Barium enema
Fistulogram
Despite work-up, 10% will have indeterminate colitis, with features of both
Crohn’s and UC

Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Complications of Crohn’s
Fistula (29%)
Pelvic abscess (20%)
Obstruction (30-50%)
Hemorrhage (2%)
Cancer (1%)
Perforation (1%)
Ureteral obstruction (1%)
Medical Management
Aminosalicylates often 1
st
line, include sulfasalazine(old),
mesalamine(Asacol, Pentasa), olsalazine, balsalazide
The newer meds lack the sulfapyridine carrier, so better tolerated. Also
come in enema form for colon symptoms
5-ASA blocks prostaglandin release, decreases inflammation
Corticosteroids for treating acuter disease, not long term or for achieving
remission.
Topical steroids used in colitis, as enema, without the side effects of
systemic.
Flagyl most commonly used antibiotic
Can heal perianal fistulas caused by Crohn’s to completion
Cipro is the most common alternative
Immunosupressants such as Azathioprine and 6-mercaptopurine used,
especially to reduce time on steroids, effective in maintenance therapy
Cyclosporine, oral treats active disease, used as bridge therapy until the
above two start working, effects go on after stopping drugs for months
Biologic therapies against TNF-alpha (inflammatory cytokine)
FDA approved infliximab (Remicade), an antibody that targets TNF-alpha
Used for active disease, fistula
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Surgical Therapy
Reserved for complications of the disease, and failure of medical
management
Most patients will require surgery during their lifetime
Within 20y of the onset of their symptoms, 75% require surgery, many
multiple resections, so attempts to conserve bowel are a must to avoid SBS
No surgical cure
An alternative to bowel resection is stricuroplasty
In cases of long strictures (>12cm), or multiple strictures in close proximity,
resection with primary anastamosis is required.
Anastomotic leak around 9%
Recurrence is 2%
Surgical Options
1. Ileocaecal resection
2. Segmental resection.
3. Colectomy and ileorectal anastomosis.
4. Emergency colectomy.
5. Laparoscopic surgery.
6. Temporary loop ileostomy.
7. Proctocolectomy.
8. Strictureplasty.
9. Anal disease.
Tumors of the Small Bowel
Benign
Adenomas,
submucous lipomas and
Gastrointestinal stromal tumours (GISTs) occur from time to time, and
sometimes reveal themselves by causing an intussusception.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
The second most common complication is intestinal bleeding from an adenoma, in
which event the diagnosis is frequently long delayed because the tumour is
overlooked at barium radiology, endoscopy and even surgery.
Peutz–Jeghers syndrome
This is an autosomal dominant disease. The gene STK11 on chromosome 19 has
been found in a proportion of patients with condition. This consists of:
Intestinal hamartomatosis is a polyposis affecting the whole of the small
bowel and colon, where it is a cause of haemorrhage and often
intussusception;
melanosis of the oral mucous membrane and the lips.
The melanosis takes the form of melanin spots sometimes present on the digits and
the perianal skin, but pigmentation of the lips is the sine qua non.
Long-term follow-up of patients with Peutz–Jeghers syndrome has shown
reduced survival secondary to complications of recurrent bowel cancer and
the development of a wide range of cancers. These include colorectal,
gastric, breast, cervical, ovarian,pancreatic and testicular cancer.
It is therefore important to keep these patients under surveillance. This can
be done by endoscopy or contrast examinations every 3 years to detect early
gastrointestinal cancers. It is also important to make sure that female patients
attend cervical and breast screening programmes.
The polyps can be likened to trees. The trunk and branches are smooth
muscle fibres and the foliage is virtually normal mucosa.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Treatment
As malignant change rarely occurs, resection is only necessary for serious
bleeding or intussusception.
Large single polyps can be removed by enterotomy, or short lengths of
heavily involved intestine can be resected.
The incidence of further lesions developing problems in the future can be
reduced by thorough intraoperative examination at the time of the first
laparotomy.
Using on-table enteroscopy, polyps suitable for removal can be identified.
Those lesions within reach can be snared by colonoscopy.
Malignant Tumors of the Small Bowel
Rare disorder, Comprise ~2% of GI malignancies, <0.4% of all cancers
Incidence ~1 per 100,000
Slight male predominance
Median age of presentation = 57
Known disease associations: Peutz-Jeghers, Crohn’s disease, FAP,
Gardner’s syndrome, autoimmune diseases, immune deficiency states,
immune suppresion
Histology’s:
Adenocarcinoma ~45%
Carcinoid ~30%
Lymphoma ~15%
Sarcoma ~10%
Why are they so rare?
Putative factors:
Rapid transit of intestinal contents – less carcinogen exposure
Liquid bowel contents – less mucosal irritation
Lower bacterial load than colon – less conversion of bile acids into
carcinogens by organisms
Increased lymphoid tissue/IgA may be protective
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Risk factors:
Diet (i.e. red meat, salt-cured foods)
Tobacco (cigarette smoking)
Alcohol use
Impaired GI motility
Other disease states: Peutz-Jeghers, Crohn’s disease, Gardner’s syndrome,
FAP, celiac sprue, immune deficiency states (AIDS, post-transplant),
autoimmune diseases
Clinical Presentation:
Non-specific symptoms including abdominal pain (dull, cramping), weight
loss/anorexia, anemia/occult bleeding, palpable mass, small bowel
obstruction, rare bowel perforation.
Often advanced disease by the time patients present with symptoms.
Diagnosis:
H&P, CBC, CMP; urine 5-HIAA if carcinoid suspected
No clear role for CEA or other tumor markers
Imaging:
No single standard preferred method
Choices include CT, MRI, upper GI with SBFT, and
enteroclysis (double contrast study), octreotide or MIBG scan
(carcinoid sx)
Diagnostic procedures:
GI procedures include capsule endoscopy, upper endoscopy
(standard – to duodenum), upper endoscopy with push
enteroscopy (visualize most of small bowel)
Exploratory laparotomy – particularly if indicated for complete
SBO, bowel perforation, bleeding, etc.
Adenocarcinoma
Most common histology (up to ~50%)
Most common in 50s-60s, M>F
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Highest incidence in duodenum, except in Crohn’s disease (ileum)
~2/3 are resectable at time of diagnosis
Stage at presentation predicts prognosis
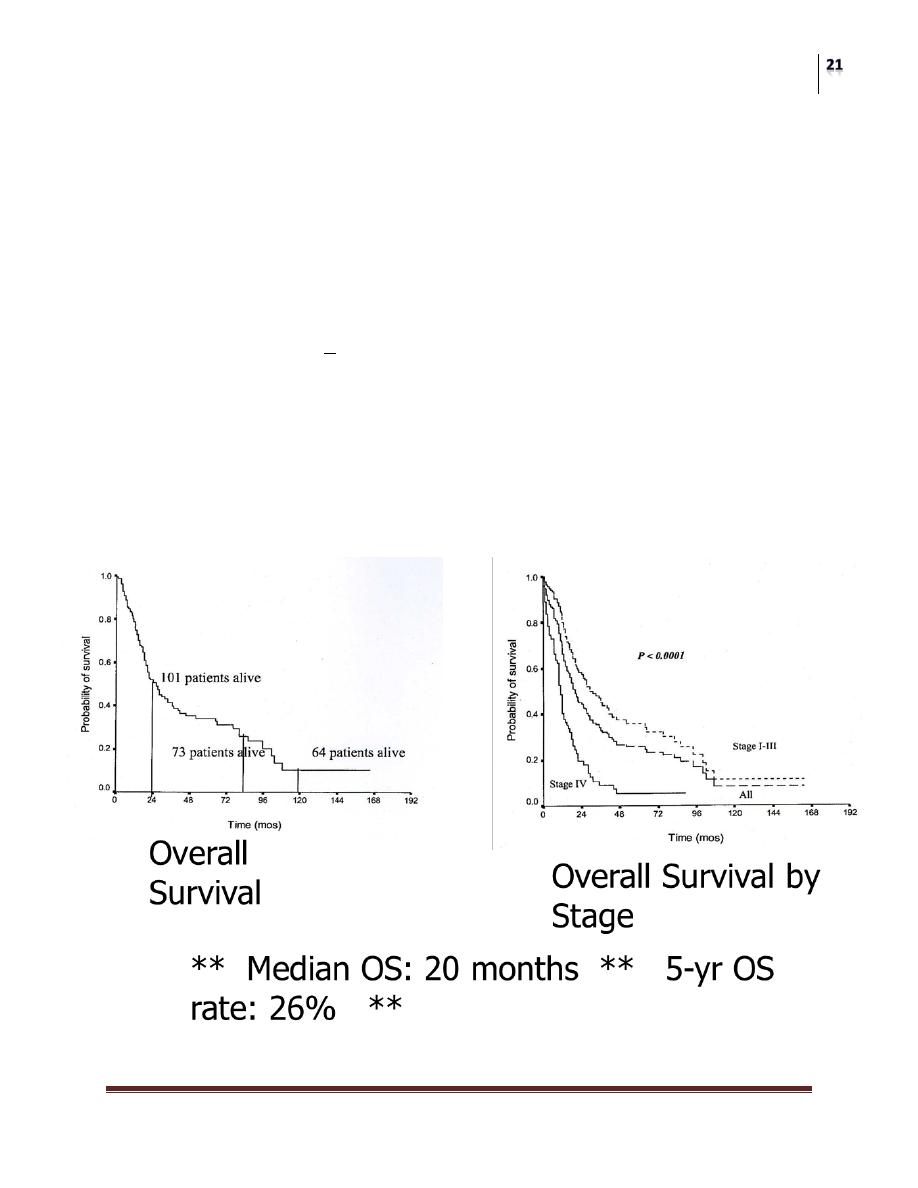
Adenocarcinoma of Small Bowel
Adenocarcinoma:
5 year survival by stage:
Stage I: 100%
Stage II: 52%
Stage III: 45%
Stage IV: 0%
5 year survival by resectability:
54% in resected, 0% in unresected
Curative-intent resection performed in 61%
(Barnes et al., Ann Surg Oncol 1994; 1:73; retrospective analysis of 67 pts, MD
Anderson)
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Retrospective review of 217 patients:
Median age 55, male predominant (61%)
Stage: I (4%), II (20%), III (39%), IV (35%)
Site of origin: Duodenum 52%, jejunum 25%, ileum 13%
Curative-intent surgery in 67% (Whipple done in 17%)
Mode of Dx:
<1998: Surgery 39%, Upper GI 36%, EGD 14%
>1998: EGD 28%, Surgery 26%, Upper GI 22%, CT
18%
Mode of Dx (by location):
Duodenum: EGD 42%, Upper GI 24%, CT 16%, Surgery
15%
Ileum: Surgery 57%, Upper GI 21%, CT 7%, Phys exam
7% (MD Anderson, Dabaja et al., Cancer 2004; 101:518)
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
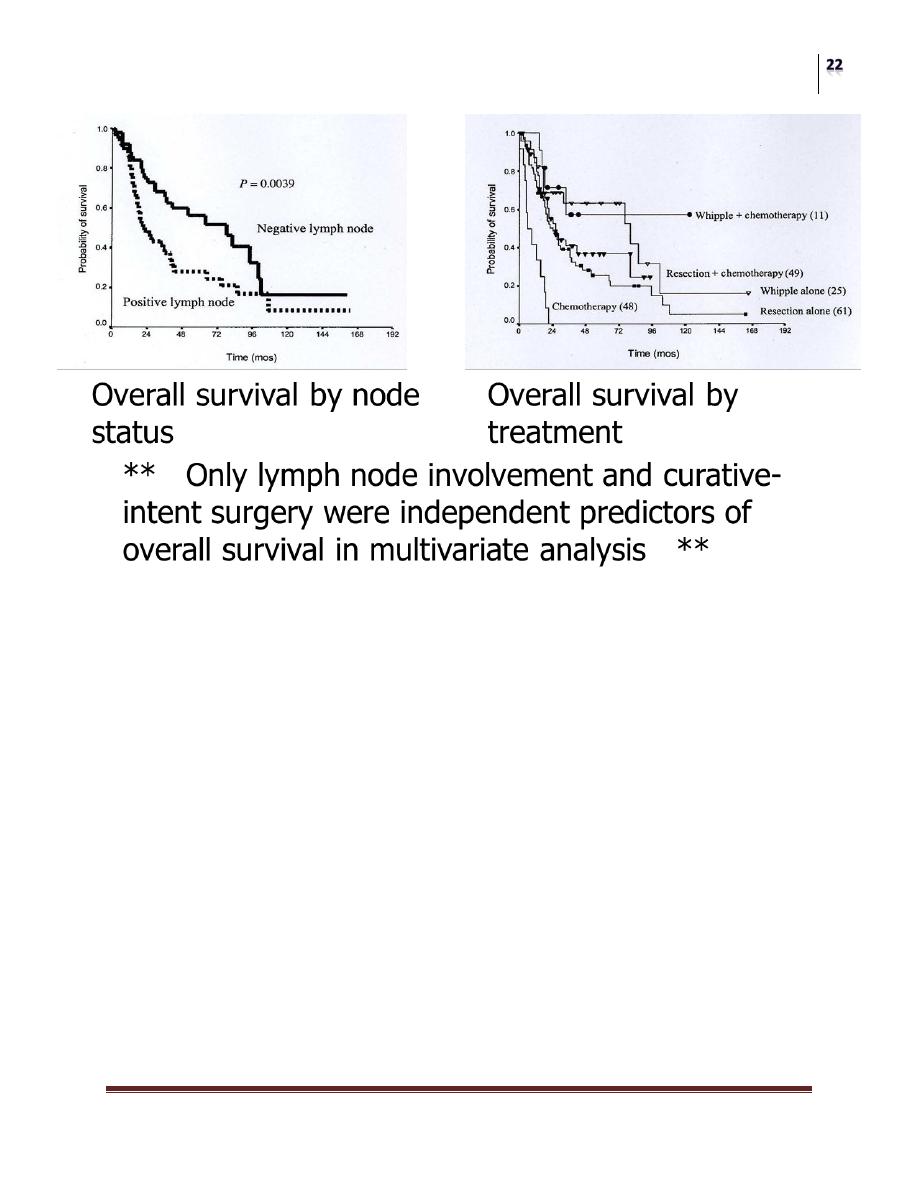
So what about adjuvant therapy?
“Adjuvant chemotherapy after a Whipple procedure or resection did not appear to
significantly affect the survival curve (P = 0.49) .
Role of adjuvant therapy?
Limited data, no prospective trials
No proven benefit in retrospective trials
Adjuvant regimens used in colon cancer are often employed in clinical
practice
Role of adjuvant therapy remains undefined, as benefits remain
unknown
Adenocarcinoma: Chemo in advanced disease
No standard chemotherapy regimen
Regimens used include:
5-FU, doxorubicin, mitomycin C (FAM)
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
5-FU + cisplatin or carboplatin or oxaliplatin
Gemcitabine and irinotecan, 5-FU based regimens
5-FU based chemotherapy
Chemo appears active; prospective trials lacking
Carcinoid of the Small Bowel
Roughly 30% of small bowel tumors
Originate from Kulchitsky cell, an enterochromaffin cell in crypts of
Lieberkuhn
Most commonly found in ileum
Often secrete serotonin and other bioactive products including histamine,
prostaglandins, polypeptides such as VIP, gastrin, glucagon, etc.
In addition to abdominal symptoms, may present with symptoms related to
secretory products (carcinoid syndrome):waterydiarrhea, flushing, sweating,
dyspnea, facial edema, tachycardia, hypotension, etc.
Metastatic disease present in 90% of symptomatic pts.
Carcinoid:
If suspected, diagnostic tests include:
24 hr urine for 5-HIAA (serotonin by-product) Also consider other
biochemical tests (urine 5-HT, serum 5-HT, serum chromogranin A, etc.)
Octreotide scan - 90% sensitivity if carcinoid sx
MIBG scan (radiolabeled iodine, taken up by tumor and stored in granules) –
50-60% sensitive
Carcinoid Tumors
Management:
Surgery is treatment of choice if localized
Appendiceal carcinoids – appendectomy
Second GI malignancies common:
Endoscopy recommended prior to surgery

Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Rx for advanced disease/carcinoid syndrome:
Octreotide (somatostatin analogue)
Hepatic regional therapy (RFA, cryotherapy, chemoembolization, etc.)
Interferon
Chemotherapy/clinical trial
Lymphoma of the small bowel
15% of small bowel tumors
Small percentage of GI lymphomas:
Stomach 75%, small bowel 9%, ileocecal 7%
Most common in ileum
Risk factors: autoimmune diseases, immune deficiency or immune
suppression, Crohn’s dz
Histology’s include:
Extranodal marginal zone B-cell lymphoma of MALT type
(MALToma)
Marginal zone lymphoma
Burkitt’s lymphoma
Immunoproliferative small intestinal disease (IPSID) –
common in Middle East
Treatment:
Surgical Resection
Locoregional Radiation Therapy
Chemotherapy for advanced disease
Treatment per histologic subtype of NHL
MALToma – follicular lymphoma-like regimens
MCL, Burkitt’s – more aggressive regimens
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Sarcoma of the Small Bowel
Account for 10% of small bowel tumors
Most in jejunum or ileum
Majority are leiomyosarcoma (75%)
Then fibrosarcoma, liposarcoma, angiosarcoma
Enlarge extraluminally – may grow extensively without causing obstruction
Similar histologically to benign counterparts:
Leiomyosarcoma: leiomyoma; liposarcoma: lipoma
Criteria for malignancy: number of mitoses, nuclear atypia, cellularity,
presence of necrosis
Treatment:
Surgical resection is mainstay of therapy
Incomplete resection may still palliate symptoms
Chemotherapy may be considered
Limited data for sarcoma regimens for SB sarcoma
Gastrointestinal stromal tumours
These tumours can be either benign or malignant.
Increased size is associated with malignant potential.
GIST is a type of sarcoma that develops from connective tissue cells.
It is found most commonly in the stomach but can be found in other sites of
the gut.
It occurs most commonly in the 50- to 70-year age group. Although its cause
is unknown, patients with neurofibromatosis have an increased risk of
developing these types of tumour.
Symptoms
Patients may be asymptomatic. Other symptoms include lethargy,pain, nausea,
haematemesis or melaena.
Surgery
Small Bowel
Dr. Imad Al-Fahad
Lec. 7 & 8
Treatment
Surgery is the most effective way of removing GISTs as they are radioresistant.
Glivec (imatinib) is a tyrosine kinase inhibitor that has been shown to be effective
in advanced cases.
T
he
E
nd
