NEUROUROLOGY
Dr. Samir AliUrinary bladder
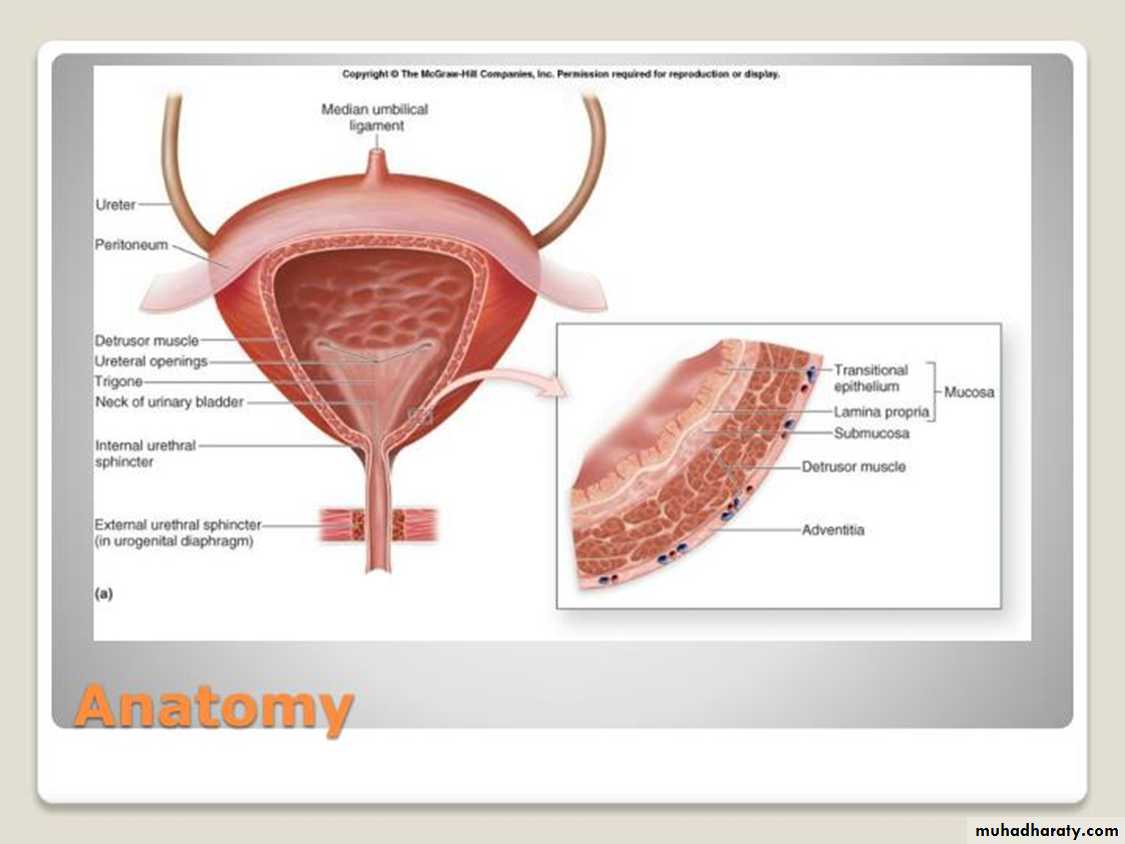
This hollow muscular organ has two main functions:Low pressure (storage) of urine
Expulsion of urine at appropriate time (voiding)
functional features
normal capacity of 400–500 ml,sensation of fullness
ability to accommodate various volumes without a change in intraluminal pressure (compliance)
ability to initiate and sustain a contraction until the bladder is empty.
voluntary initiation or inhibition of voiding despite the involuntary nature of the organ.
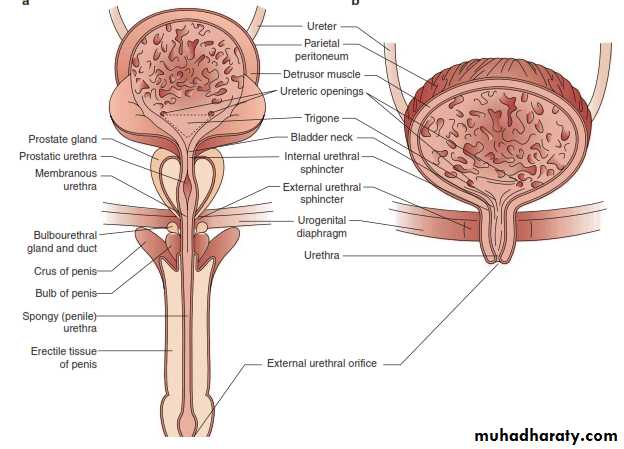
The urethra and sphincteric mechanism
Functions:To provide effective continence mechanism for majority of the time during the storage phase.
To allow adequate emptying from the bladder with minimum resistance during the voiding phase.
there are 2 sphincteric elements:
an internal involuntary smooth-muscle sphincter at the bladder neck, consists of a powerful inner layer of muscle bundles arranged in a circular orientation.(also prevents retrograde ejaculation).
an external voluntary striated-muscle sphincter from the level of verumentanum down to the distal aspect of membranous urethra in males and at the mid urethra in females.
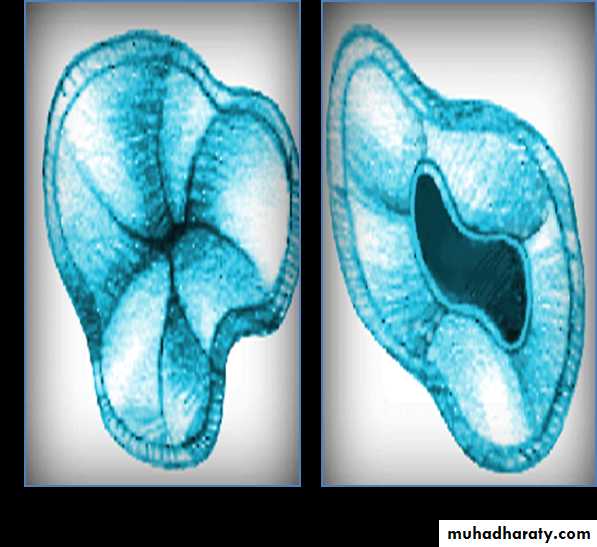
male and female sphincteric mechanisms
Comparison of male and female sphincteric mechanism
MaleFemale
Proximal bladder neck mechanism
powerful
weak
Distal urethral mechanism
powerful
Prone to effect of exogenous influences such as pelvic floor weakness and damage or denervation consequent upon childbirth
Prostate
Further increases bladder outlet resistance
Not present
Urethra
Long (20-25 cm)
Short (3-5 cm)
Pelvic floor muscles
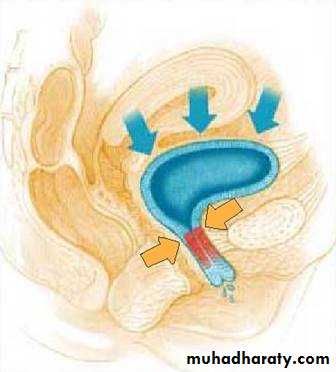
Composed mainly of levator ani muscles, endo-pelvic fascia, ad supporting ligaments.
Maintain pelvic organs in the correct position and plays a vital role in continence.
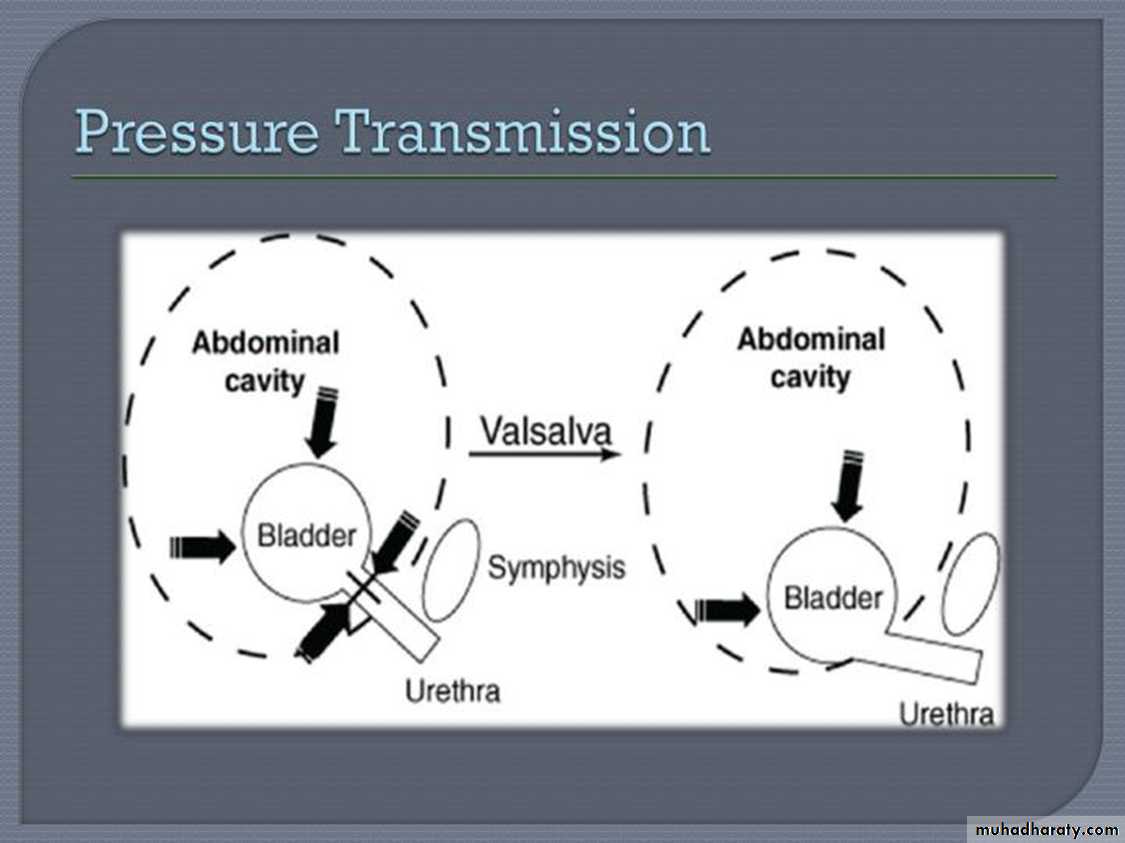
Form a supporting hammock beneath the urethra, and during increases in intra-abdominal pressure, the urethra is compressed against this hammock.
Ureterovesical junction
The function of the ureterovesical junction is to prevent backflow of urine from the bladder to the upper urinary tract. Longitudinal muscle from the ureter contributes to the makeup of the trigone. Stretching of the trigone has an occlusive effect on the ureteral openings.Neuronal control of the lower urinary tract
Coordinates the activities of bladder and sphincteric mechanismsControl receptive relaxation of the bladder (compliance)
Sense bladder fullness
Maintain continence with increasing bladder fullness
Initiate voluntary voiding
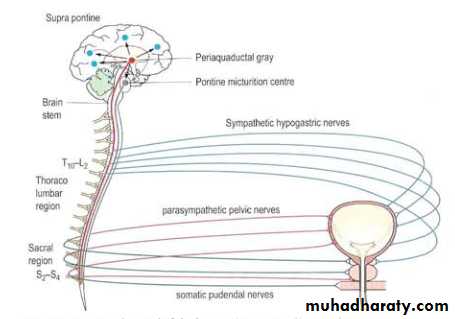
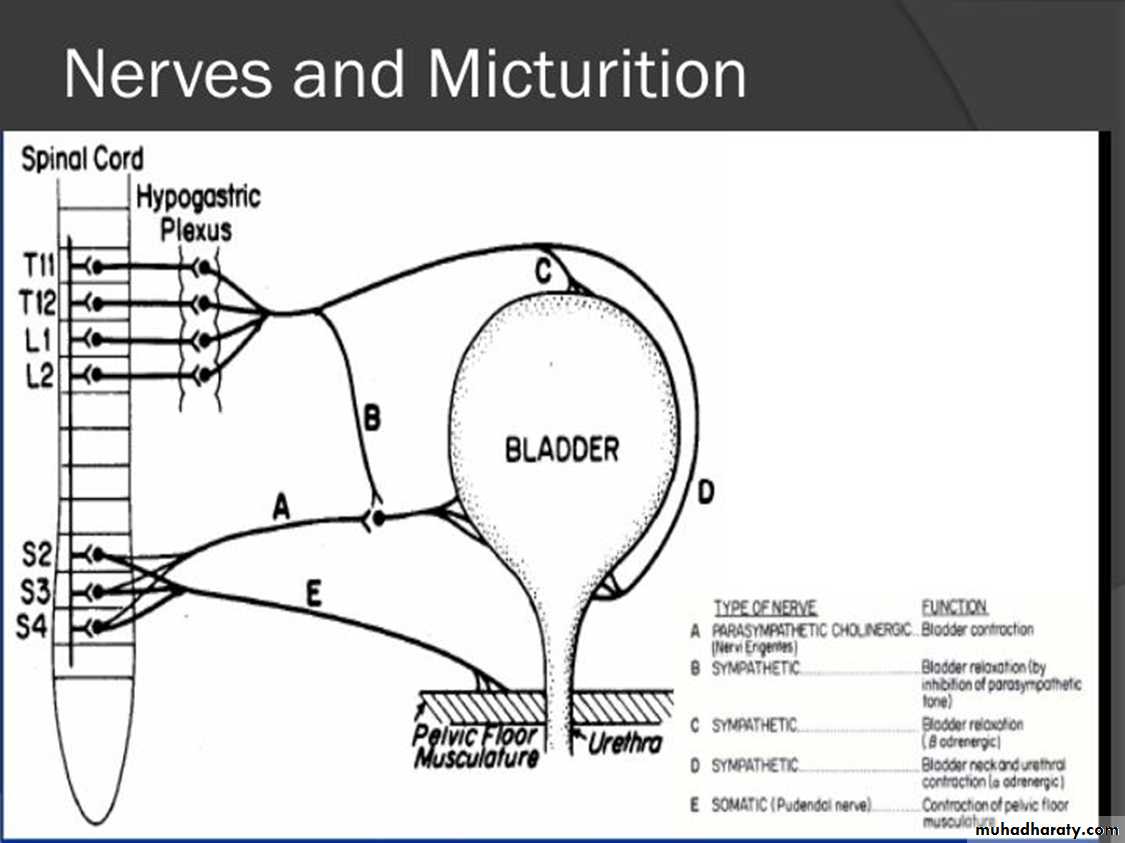
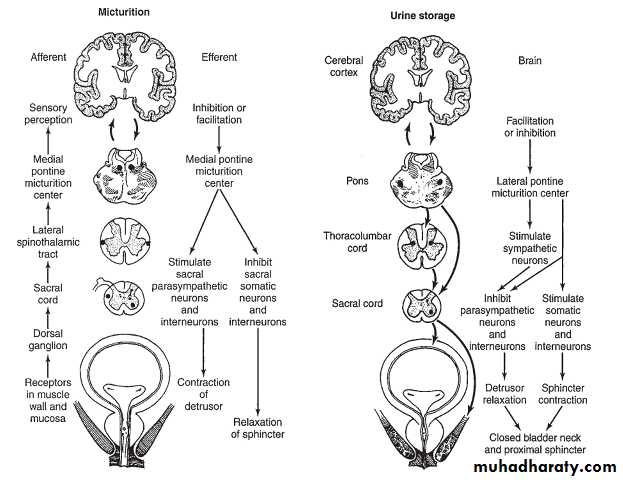
Motor (efferent) control
The storage phase in under sympathetic controlThe voiding phase is under parasympathetic control
Sensory (afferent ) control
Transmit information regarding the fullness of the bladder as well as the presence of any noxious stimuli ( cold or chemical), they are involved in both involuntary reflexes and conscious sensation of bladder fullness.
The principal innervation of the lower urinary tract
Type
OriginDetrusor muscle
Sphincteric muscle
Principal neurotransmitter
hypogastric
sympathetic
T10-L2
Relaxation
Contracts sphincteric smooth muscle
Noradrenaline
pelvic
Para-sympathetic
S2-S4 (spinal micturition center)
Contraction
Relaxation
Acetylcholine
pudendal
Somatic
S2-S4 (Onuf’s nucleus)
N/A
Contracts sphincteric striated muscle and pelvic floor
Acetylcholine
The micturition reflex
Intact reflex pathways via the spinal cord and the pons are required for normal micturition. Afferents from the bladder are essential for the activation of the sacral center, which then causes detrusor contraction, bladder neck opening, and sphincteric relaxation.The pontine center, through its connection with the sacral center, may send either excitatory or inhibitory impulses to regulate the micturition reflex.
Cerebral (suprapontine) control
Although micturition and urine storage are primarily functions of the autonomic nervous system, these are under voluntary control from suprapontine cerebral centers, so that other groups of muscles (arm, leg, hand, bulbocavernosus) can be integrated to assist in urination at the appropriate time and place.Cerebral lesions (eg, from tumor,Parkinson’s disease, vascular accident) are known to affect the perception of bladder sensation and result in voiding dysfunction.
Urodynamic studies
techniques used to obtain graphic recordings of activity in the urinary bladder, Urethral sphincter, and pelvic musculature.
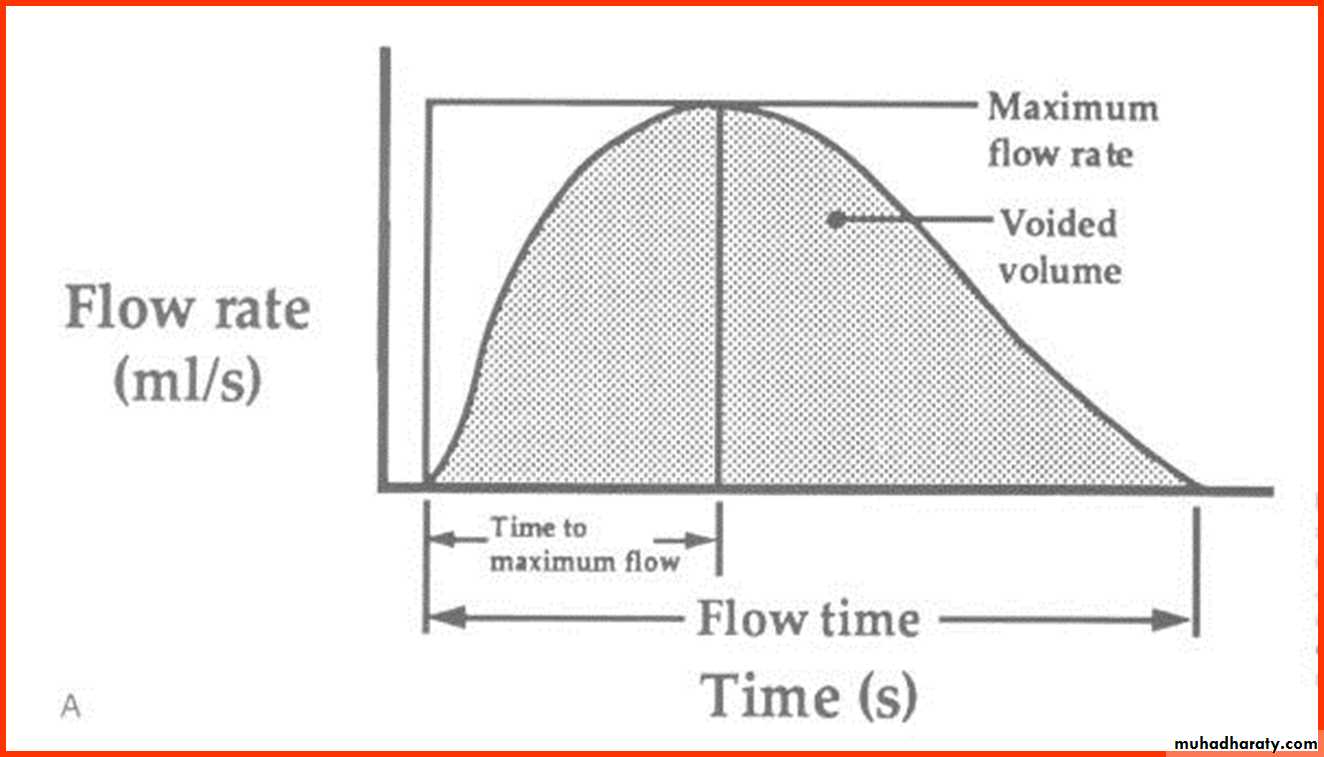
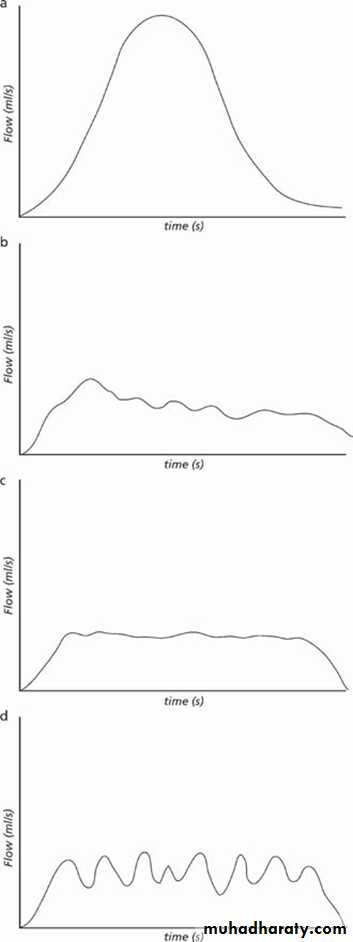
uroflowmetry: is the study of the flow of urine from the urethra
FLOW RATE IS THE PRODUCT OF DETROSAL ACTION AGAINST OUTLET RESISTANCE, so variation from normal might reflect dysfunction .
The normal peak flow rate (Qmax) for males is 20–25 mL/s and for females 20–30 mL/s.
A flow rate less than 10 ml / sec is definitive evidence of obstruction.
THE NORMAL UROGRAPH IS BELL SHAPED
average flow, max flow, and flow time.
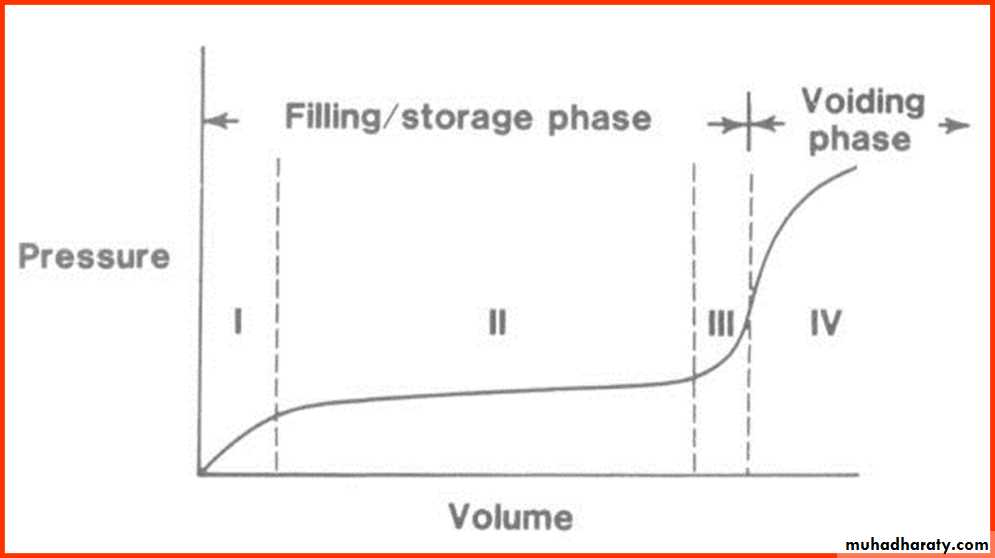
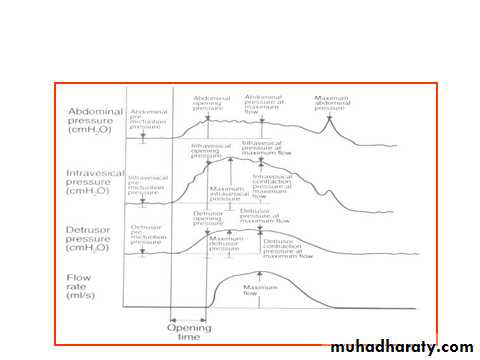
Cystometry
Cystometry simply is a plot of intravesical volume vs. pressureCompliance= volume/pressure
Intravesical pressure is the summation of both detrusor pressure and intra-abdominal Pressure
• Normal voiding pressure are below 40 cm H2O
Sphincteric function
Urinary sphincteric function can be evaluated either by recording the electromyographic activity of the voluntary component of the sphincteric mechanismor by recording the activity of both smooth and voluntary components by measuring the intraurethral pressure of the sphincteric unit. The latter method is called pressure profile measurement (profilometry).
Closure pressure: urethral pressure – intravesical pressure i.e the net closure pressure
Functional length: the length of the segment with positive closure pressure
Neuropathic bladder disorder
Upper motor neuron lesions or spastic bladderDue to lesions above sacral micturition center, above the conus medullaris T12 vertebral level
Due to less of inhibition from higher centers
Common lesions include vascular accidents, tumors, multiple sclerosis, and inflammatory conditions like encephalitis.
Contracted detrusor results in one of the followings :
Frequency and urgency when the sphincteric pressure is normal
Retention when the sphincteric pressure is high
Incontinence when the sphincteric pressure is low
Lower motor neuron lesionsflaccid or atonic bladder
Direct damage to peripheral innervation of the bladder or sacral cord segments S2-4
Causes include trauma, tumors,tabes dorsalis, and congenital anomalies (spinal bifida and meningomyelocele)
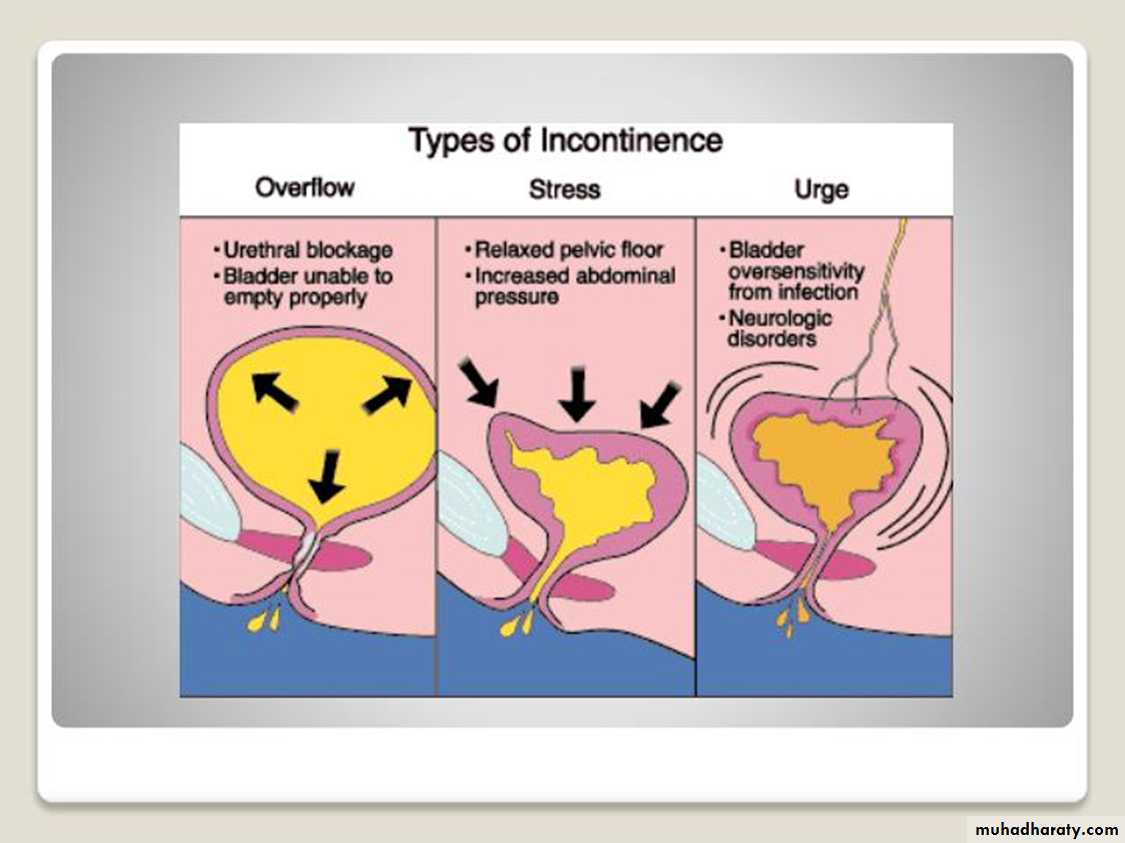
Patients experience principally retention and overflow incontinence, male patients lose their erections.
Patient evaluation should include:
Full neurological examination to establish the sensory level, the anal, bulbocavernosal, knee, ankle, and toe reflexes.Urine analysis, renal function tests.
Periodic cystourethrograms looking specifically for VUR.
Cystoscopy to evaluate the bladder and urethra
Urodynamic studies to record bladder and sphincteric pressure profiles.
Differential diagnosis
CystitisChronic urethritis
Vesical irritation secondary to psychic disorders
Myogenic damage
Interstitial cystitis
Cystocele
Infravesical obstruction
Treatment
We need to restore the low pressure activity to the bladder to
protects upper tracts and preserve renal function
Restore continence
Control infection
In spinal shock
Intermittent sterile catheterizationWhen indwelling catheterization is needed consider small size foley catheter (16Fr) or SPC
VCUG to rule out reflux
Cystogram is needed 3 monthly at first then annually looking for complications
Encourage plenty of fluid intake, early wheelchair ambulation, and measure to avoid calculus formation.
Spastic bladder:
reasonable bladder capacity: trigger techniques to initiate voiding, plus anticholinergic medications.Markedly diminshed capacity:
Indwelling catheter or condom (no VUR)
Parasympatholytic drugs like oxybutanin and delterodine.
Intravesical botulinum toxin injection
Neurostimulation or bladder pacemaker
Bladder augmentation and urinary diversion
Flaccid bladder:
Bladder training: timed voiding every 2 hours, by suprapubic pressure (Crede maneuver) and abdominal wall straining.
Clean intermittent catheterization every 3-4 hours.
Surgery in the form of bladder neck incision or excision or big prostate to reduce bladder outflow resistance.
Parasympathomimetic drugs: bethanicol bromide 50 mg every 6-8 hours.
Urinary incontinence
the involuntary loss of urine to the degree that is socially and hygienically unacceptable to the patient.It affects about 30% of women above 65yrs.
Some elderly patients accept it as a sign of aging
Some times its transient and resolves spontaneously as that which follows child birth or associated with bladder infection
But it is usually chronic and progressive and requires treatment
Types:
Anatomic or genuine urinary stress incontinenceUrge incontinence
Neuropathic incontinence
Congenital incontinence
False (overflow) incontinence
Iatrogenic incontinence
Fistulous incontinence
Stress urinary incontinence
Is leakage resulting from any type of straining (coughing, laughing, sneezing, or lifting), that puts pressure on the bladder.Common causes are aging , lack of estrogen , neurological disorders and obstetrical / surgical trauma
Defect is demonstrable radiologicaly
Restoration of normal anatomy restores continence
Mechanism of leak
1. Insufficient urethral support from the endopelvic fascia and muscles is the most important etiology .this results in hypermobility of the vesicourethral segment, here the sphincter itself is intact.2. Intrinsic Sphincter Deficiency ( ISD ) occurs when there is failure of the urethral sphincter due to mucosal and muscular atrophy and denervation.
Anatomy:
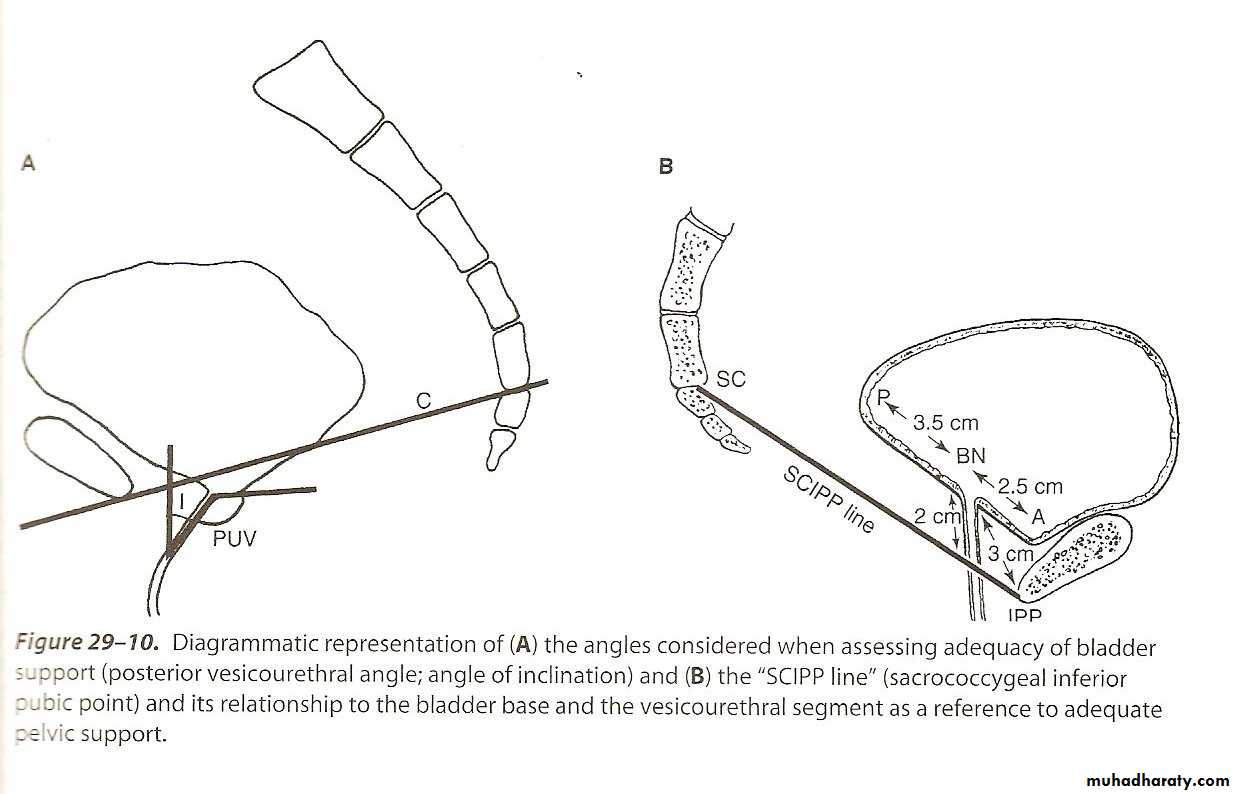
The anatomic feature is that of hypermobility or a lowering of the position of the VU segmentVarious relations between the urethra, bladder, and bony landmarks have been studied
Posterior vesicourethral angle
Axis of inclination (urethral line vs. vesical plane)
UV junction and the SCIPP
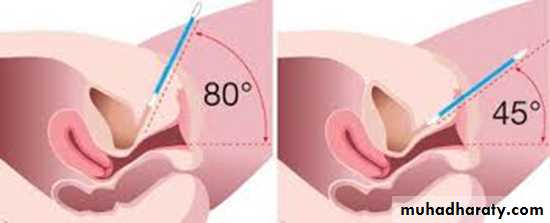
Urethral hypermobility test
Radiology
Do lateral cystogram with urethral catheter inserted at rest and stress to study the relationship of VU junction and pubic bone, normal mobility during stress should be less than 1.5 cmUrodynamic Features
Low urethral pressure profile, with reduced closure pressureShorter functional length with the loss in the proximal segment
In severe cases there is loss of voluntary increase in urethral pressure
These changes may be mild in rest , but will be very prominent during stress
Diagnosis
History:
Degree of leakage, its relation to activity, position and status of bladder filling
Time of onset, and course of progression
Previous surgical and obstetrical history
Medications taken and medical illnesses
Examination:
Pelvic exam: laxity of pelvic support, and degree of prolapse
Neurological exam should be done if neuropathy is suspected
Cystography is done to demonstrate the anatomic abnormality, not to make the diagnosis
The diagnosis is made by urodynamic study in rest and stressTreatment
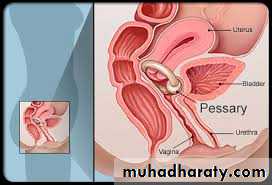
Conservative therapy may involve hormonal replacement, pelvic floor exercises, bladder retraining, and life style modification such as weight reduction or avoidance of foods that irritate the bladder.Other options include the use of a urethral plug or vaginal pessary.
• Surgical intervention may be needed to restore anatomical relationships.
Types of Surgical Procedures
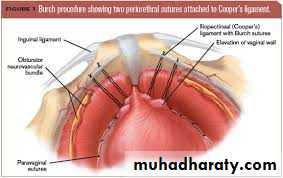
1. Retropubic suspensions as ,MMK,Burch
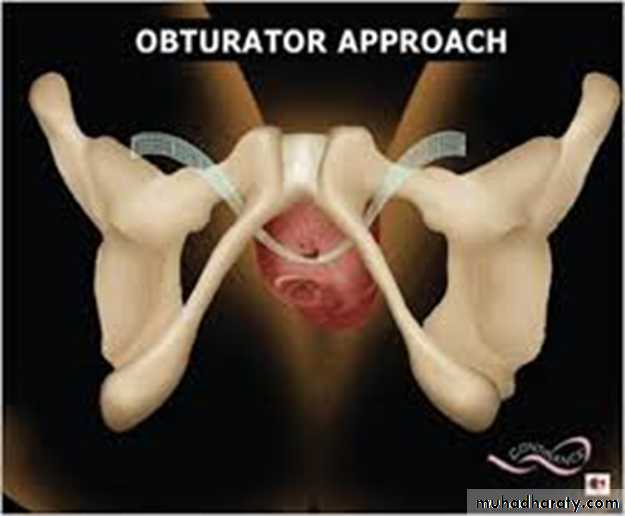
2. Transvaginal needle suspension as TVT and TOT.
3. Sling operations as anterior rectus sheath slings
4. Periurethral injection specially for Intrinsic sphincter deficiency
Urge Incontinence
The basic feature is detrusor instability and loss of urine while attempting to inhibit micturitionThe bladder is described to be overactive with clinical symptoms of urgency, frequency, and nocturia
• The bladder overactivity can result from bladder inflammation, obstruction or neurological trauma
Urodynamic Features
Normal or high closure pressureNormal response to stress and filling
Detrusor hyperirritability with contractions overcoming urethral resistance
In some cases the detrusor pressure remains normal, but there is dropping in the urethral closure pressure leading to leak (urethral instability)
Combination of the two
Treatment
Bladder trainingDecreased fluid intake
Scheduled voiding
Relaxation technique
Anticholinergic drugs
Intravesical botulinum toxin injection
Surgery rarely needed as SNS, augmentation, and diversion
THANK YOU
&GOOD LUCK