Coronary Artery Disease
Prof Hassan Yousif AlnajjarBaghdad Nov..2014
Introduction
Coronary Artery Disease is the most common cause of Morbidity and mortality worldwideIn Iraq it is very common
Coronary artery disease is caused by atherosclerosis in almost all cases
Atherosclerotic lesion causes Ischaemia of the myocardium hence it is called schaemic Heart Disease
Aim of lectures
1- Discuss etiology and Risk Factors of Aherosclerosis its prevention2-Discuss the pathophysiology of the ischaemic syndromes
3- Try to link the symptoms of the Ischaemic syndrome to the underlying pathology
Atherosclerosis
1- Increased atherogenic lipoproteins levels favour t their subendothelial accumulation where they undergo chemical alteration such as oxidation rendering them unclearable, and resulting In the trigger of self-perpetuating inflammatory process2- They will be taken by macrophages to form foam cells that will attracts more inflammatory cells such as fibroblasts. Myofibrils migrates from the media to the intima an multiply.
3- Eventually atheromatous plaque forms in the subendothelium starting with fatty streaks ending with large plaque that impinge on the lumen
Site of atherosclerosis
Probably affect the whole arterial tree but not uniformly ie patchy and selective
Affects the medium size arteries eg the coronaries, the femorals and the carotids
More at bifurcation.
More at jet site when the artery curve around
Can be concentric or eccentric
Etiology of Ayherosclerosis
Etiology is Unknown but there areRisk Factors. They are multiplicative
1- Age and Sex Not M
2- Smoking M
3- HTN M
4- DM ? M
5- Dyslipidaemia M
6-Family h. Not M
7-Obesity M
8-Inactivity M
New risk factors
HyperinsulinaemiaGlucose intolerance
Hyperfibrinogenaemia
Anti phospholipids' syndrome
The last two factors are associated with recurrent arterial thrombosis in total agreement with the new name of
Atherothrombosis
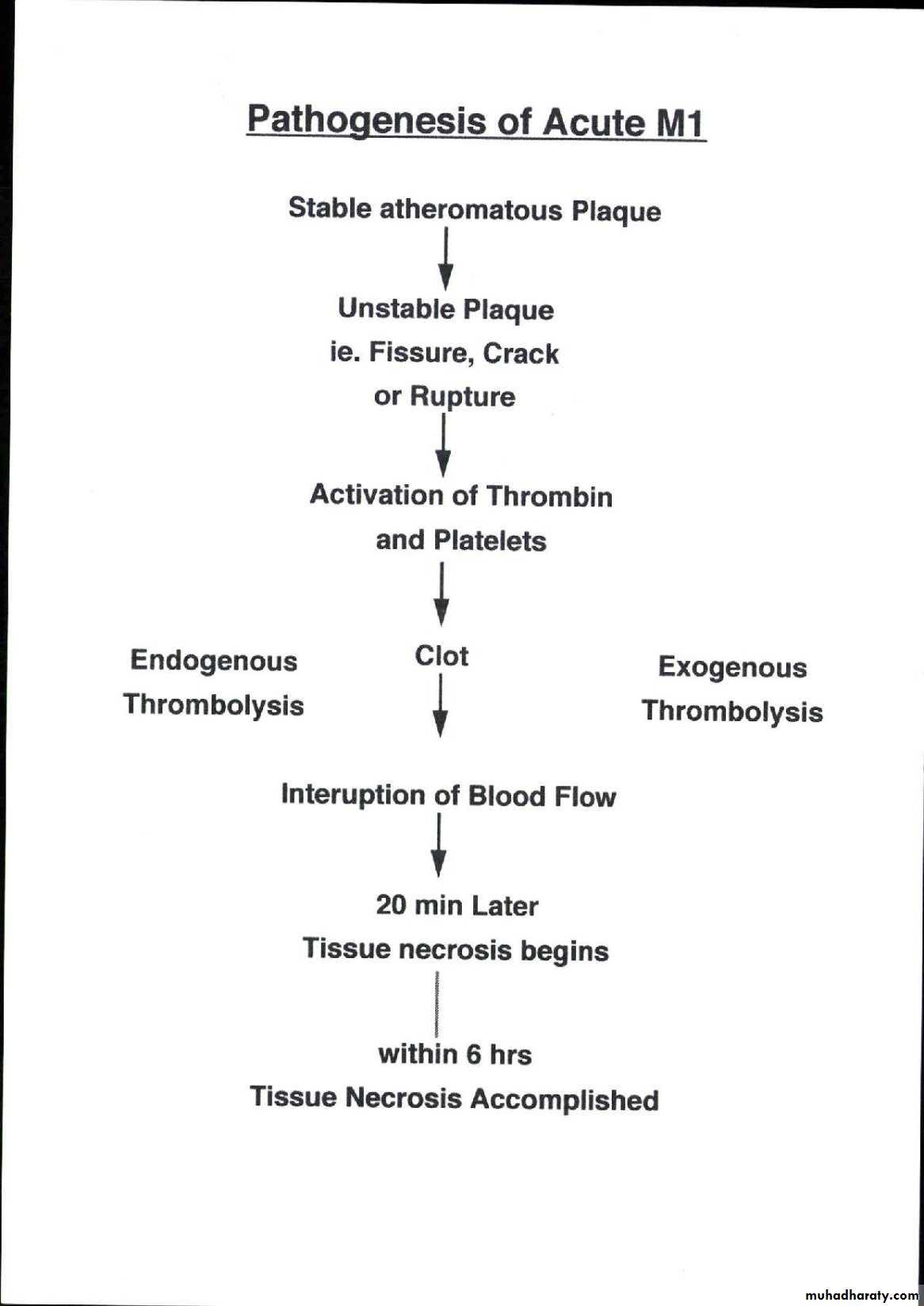
Atherosclerosis and Thrombosis
Plaque fissuring, cracking or even rupture
Exposure of subendothelium
Activation of thrombin and platelets leading toThrombosis hence the new name
Atherothrombosis
Manifestation of atherosclerosis
Atherosclerosis is a pan-arterial disease hence it affects almost all systems but the effects on the CVS and the brain is far disastrous where it causesStable and Unstable Angina and Myocardial Infarction ;
Heart Failure
Arrhythmia
Sudden death
Valvular heart disease; Acute or Ch. MR
Peripheral Vascular disease
Aneurysm of the Aorta
Dissection of the Aorta
TIA and Stroke
Determinant of Outcome of atherosclerotic plaque
Depends on
1-Stability of plaque
2- Structure and territory supplied.
3 Severity of Stenosis -
Stability of PLAQUE
The whole mark of atherosclerosis is theAtherosclerotic plaque which impinges on arterial the lumen and can impair flow
The plaques are mainly two types
1- Cellular and less fibrotic with thin cap hence unstable and susceptible to rupture
Leading to Unstable Angina or Infarction
2-Less cellular more fibrotic with thick cap ie Stable plaque ; may cause Angina Pectoris
Outcome of atheroma plaque
A -Stable plaque Outcome depends on severity1- Mild stenosis is asymptomatic
2- Moderate- total occlusion may cause
1-Silent Ischaemia
2- Ch. Stable angina.
3-Formation of Collaterals will be induced Chronic Ischaemia. Pt may remain asymptomatic
B- Unstable plaque can rupture then thrombose. Outcome depends on whether it led to
1- Partial occlusion Unstable Angina or
2-Total occlusion Acute MI
Pathophysiology of Angina :- is chest pain caused by imbalance between O2 supply and O2 demand
physics law;- Flow in a narrowed tube depends o
1- Severity of narrowing ; degree of stenosis
2- Pressure gradient across the stenosis
In coronary artery stenosis significant reduction of flow occur when the narrowing is 70%+ .
A70% Stenotic plaque causes significant reduction of O2 supply to the myocardium
This reduction is worsened by increased demands by increased heart rate ; causing pain : ie angina
Other causes of Angina :-
A Other Important factors that reduce O2 SUPPLY1- Coronary thrombus
2- -coronary spasm
3- Anaemia
B-Other Important factors that increase DEMAND
LVH due to HTN, AS, or HOCM
Chronic stable angina; Angina pectoris
Episodes of chest pain that is usually triggered by exertion. and relieved within 5 min of by rest or sublingual Nitroglycerine. The reproducibility and the predictability , and its relationship to exertion is most important features. The duration of the symptom is important. Recent onset angina is more risky than longstanding stableCriteria of ischaemic chest pain
Type
Dull Constricting
Chocking
Squeezing crushing Burning or
Heavy weight Suffocating
Aching
Location
Retrosternal
Across the
chest
In the left arm
Others
Radiation
Left arm
Left shoulder
throat
others
Other Criteria of ischaemic pain
symptomcriteria
Ischaemic sydrome
Duration
Severity
Courseshort ; few min.
few -30 min
>30 min
mild
moderate
Severe
Episodic
Fiactauting
Continous
Ch Stable Angina
Unstable Angina
Acute Myo. Inf.
CSA
UA
AMI
CSA
UA
AMI
Associated symptoms
NO
Mild
MODERATE
SEVERE
Nausea / vomiting
CSA or UA
AMI
AMI
AMI
Sweating
CSA
??
UA or AMI
UA or AMI
Or Cadiogenic shock
Cold periphery
CSA
??
UA
AMI
Or Cardiogenic Shock
Teacher’s story
A 50 yrs old hypertensive and diabetic teacher complained of constricting retrosternal chest pain for three months. The pain occur while walking across the bridge in the morning against the wind and is relieved by rest. He denies SOB, Palpitation, or Syncope.
He has no similar illness before His father had died suddenly at the age of 60 yrs.
His examination is unremarkable
His ECG is normal. His lipids are elevated
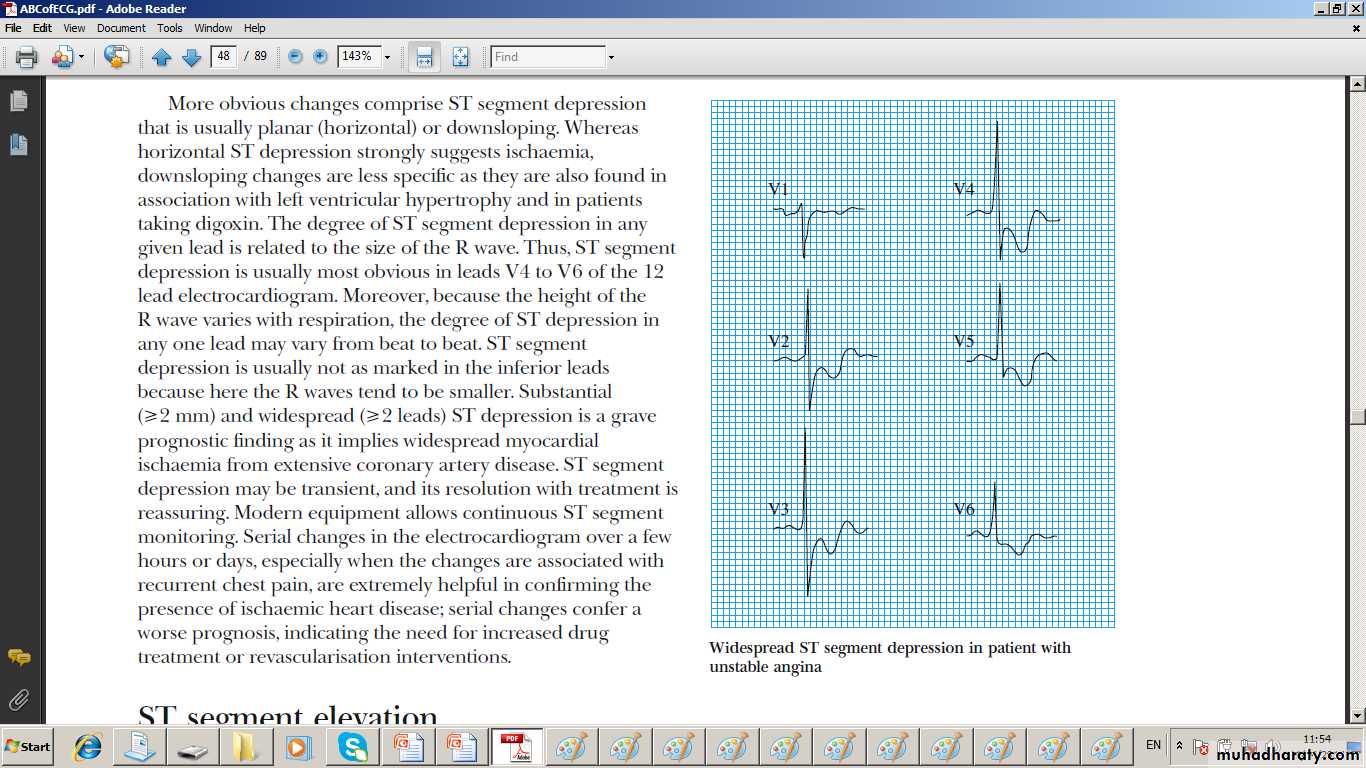
InvestigationsECG
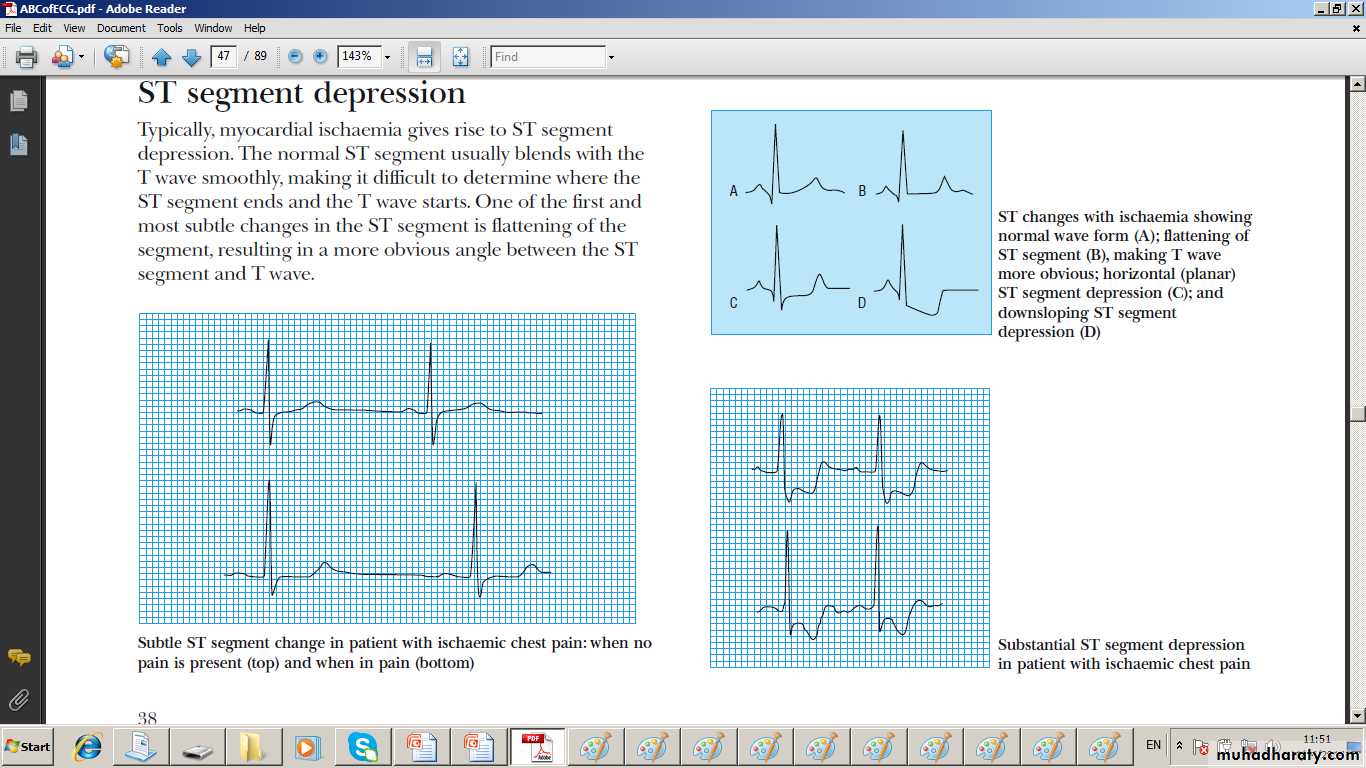
Usually normal unless done during pain wherehorizontal or down slopping ST segment depression T wave inversion on resting ECG
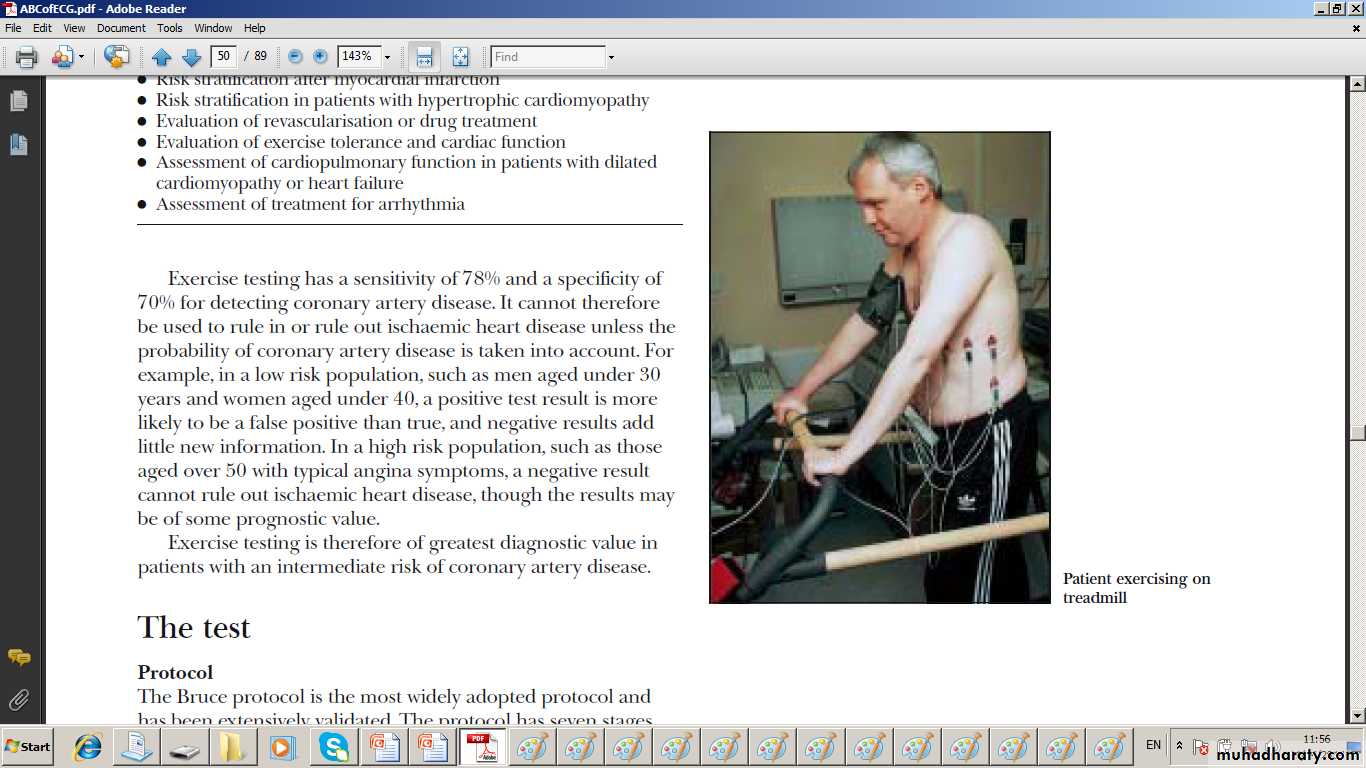
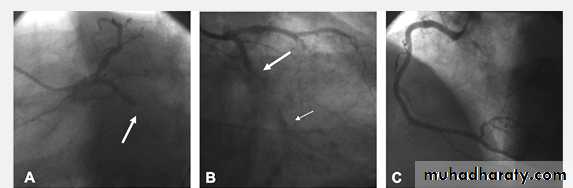
2- Stress Test
Ischaemia is revealed by stressing myocardium through inducing tachycardia . It is used to:-
a- Reveal ischaemia in atypical chest pain
b- Asses the extent of CAD
c- Identify high risk ISCHAEMIC pts pts
d- can reveal the Ischaemic cause of L.V. Dysfunction, Heart Failure arrhythmia, or syncope
Ischaemia anatomical Corelation
V2-3 septal Ischaemia LADL1-L11and AVF Inferior Ischaemia RCA or CX
V2-5 Anterior ischamia LAD
L1 and AVL= lateral Isch.= Diagonal branch of LAD
Anterior +L1+AVL and V6 AnteroLateral Isch.= LAD
nferior +L1 AVL and V5-6 Inferolateral Isch.= RCA or CX
Types of Stress test
Type depends on the way of stressing to induce Tachycardia and how to demonstrate Ischaemia
Two ways of inducing tachycardia
a- Walking on treadmill or
b- Dobutamine infusion
Three ways of of demonstrating ischaemia
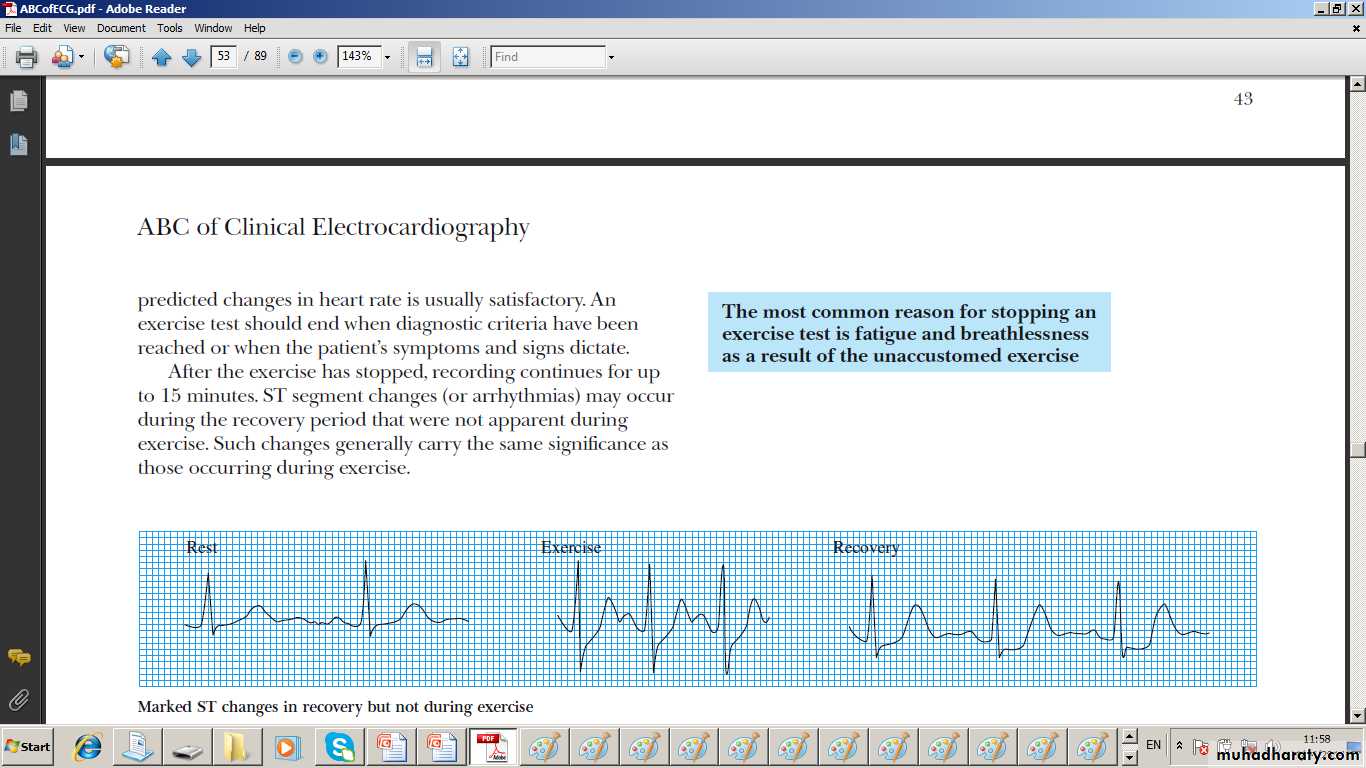
a- ST depression on ECG
b- filling defect on nuclear test
c- hypokinesia on ECHO
.
Types of Stress Tests
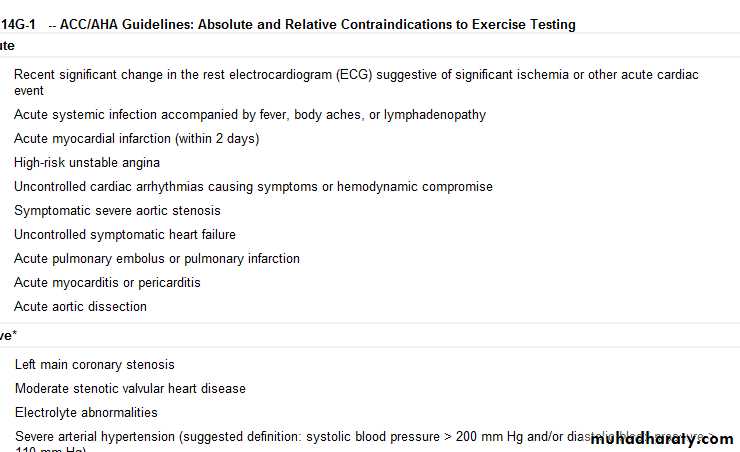
-1 1-1- Exercise test ; Exercise ECG test :-
Exercise induces tachycardia and if Ischaemia occur it manifests as ST- Depression or hypotension .
IF pt is unable to Exercise use dobutamine or e pacing
2- Dobutamine Stress Thallium test ( Myocardial perfusion scan) ;- used to demonstrate ischaemia if
a- Exercise ECG is equivocal
b- The baseline ECG shows LBBB
c- Pt. is unable exercise
Radioactive Thallium is taken by viable perfused myocardium. Transient Ischaemia causes transient filling defect while a scar causes a permanent one
3- Stress Echo:- induced Ischaemia causes transient hypokinesia while scar causes permanent akinesia
Investigations of CSA:- CT angiography and calcium score
Used to exclude ischaemia rather diagnosing it
Hence more useful for atypical chest pain and no risk factors where the test is likely to be negative and calcium score is low
New version with thinner cuts may increase the accuracy and may enable a positive diagnosis
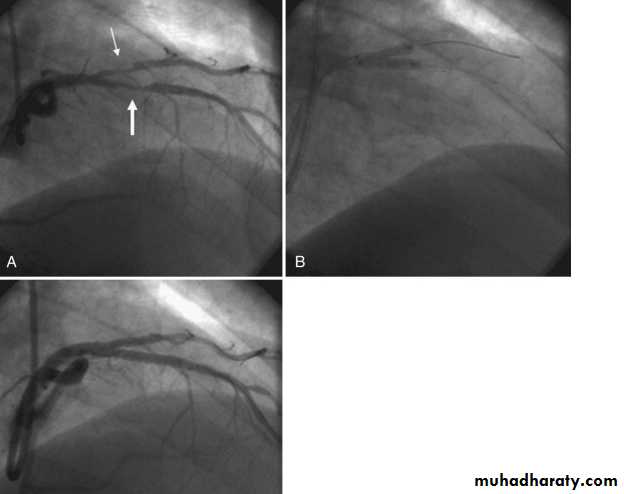
Coronary Angiography
Gold standard to diagnose I.H.D. until nowDemonstrates the anatomy of the artery. By showing
1- severity of stenosis and type of the lesion
a- non-significant stenosis (<70%)
b- Mod or severe (Critical) lesion ( >70% )
2- Extent of the disease:-
single, two ,three vessel disease, Left main
stem disease (> 50%)
3- L.V angiography if done will assess L.V. function
4- If suitable intervention can be done
Indicated for the diagnosis of atypical chest pain
and before revascularization
Cardiac Catheterization and Angiography and Intervention
Catheterization:-
Measuring the pressure of the cardiac chamber and the aorta
Angiography:-
Visualizing the cardiac chamber, the aorta, and the coronaries
Intervention
If treatment is performed as well eg Percutanous Coronary Intervention which include Angioplasty; dilating the stenosis by balloon and or Stenting for deploying stent
Diagnosis
1-Typical history is diagnostic.In young pts Risk factors are essentials for DX
2-Examination
is usually normal
Some pts may have signs related to :-
A- Risk factors e.g. nicotine stain in smokers, xanthomara in hyperlipdaemia, and Retinopathy in D.M and in HTN
B-Peripheral Vascular Dis. :- absent pulses, carotid bruits. Also abd. Bruit in Renal artery stenosis
C- Other causes of increased demand such as
Aortic Stenosis or HOCM
or reduced supply e.g. ; Anaemia
Differential diagnosis of Chest Pain
Ischaemic pain but without atheromatous coronary stenosis ; e g:-1- Microvascular angina
2– CA artery spasm
Non-ischaemic Chest pain; Atypical chest pain
Frequent causes Rare Causes
1- Musculoskeletal pain 1- Herpes zoster
2- Oesophageal spasm 2- Tietze disease
3 – Mitral valve prolapse
4- Pleuretic chest pain
5- pericarditis chest pain
Ischaemic pains without atheromatous CA stenosis
1--Micro vascular angina ( Cardiac syndrome X)
Due to defective O2 supply at the microcirculation ; No epicardial coronary stenosis
more common in women.
Pain usually occurs at night
The patient has evidence of Ischaemia on investigation such as ST depression during pain or on Exercise test
But has normal coronary angiogram.
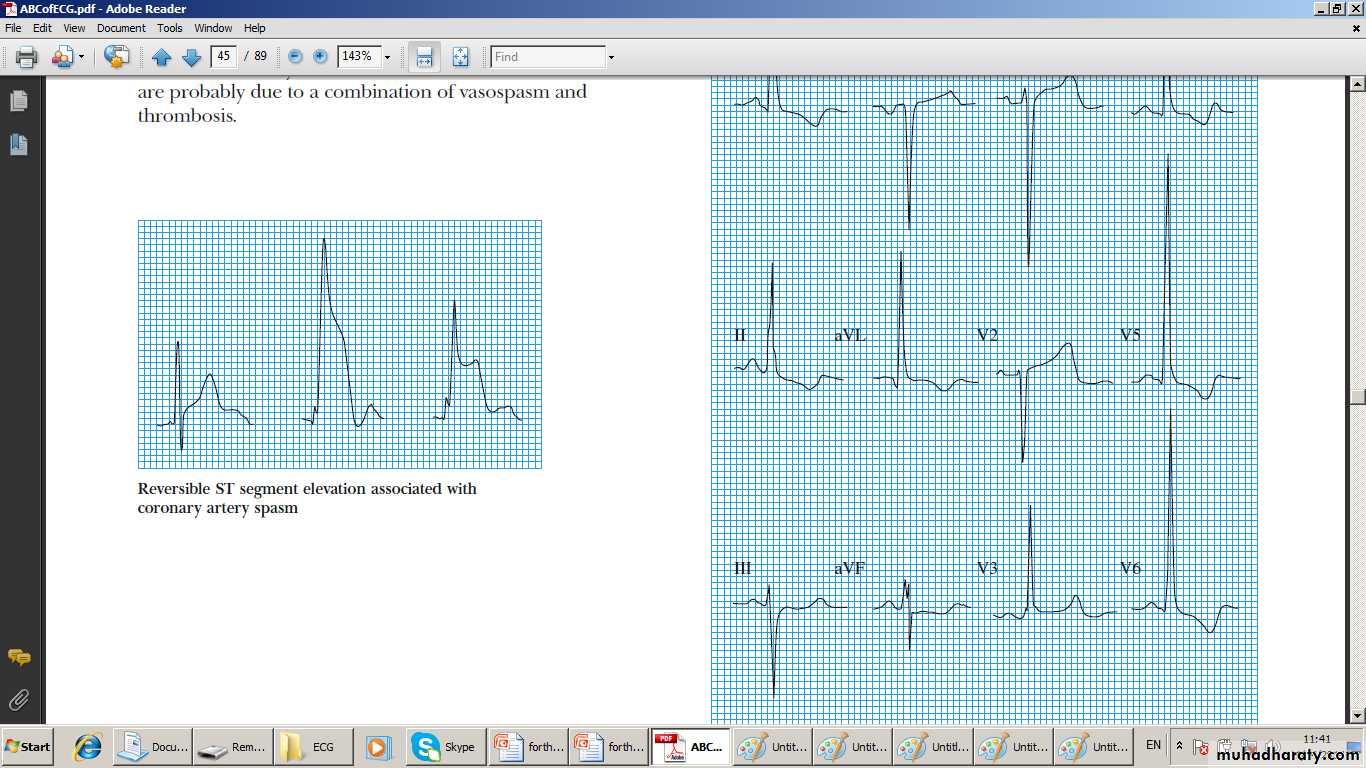
2- CA spasm
Causes transient Ischaemia which can be transmural hence the ECG reflect that ;Transient ST-elevation
usually more common in women. May occur on the top of atheromatous epicardial CA stenosis
Atypical chest pain
Not typical for Ischaemia ; Usually has some characters for ischaemia such location and some other criteria but lacks that of duration and its relation to exertion1- Musculoskeletal pain;-
Far more common than anginal pain usually nagging more in the L. arm and related to moving arm or turning over. Numbness is common as well as neck pain.
Longer duration ie hours or dayes
Atypical chest pain
2- Oesophagyeal spasm:-Ultra short ; lasts for seconds , pricking ,sharp rather than compressive in nature. It is usually associated with dyspepsia and emotional stress but not related to exersion
B-Oesophageal reflux pain causing oesophagitis which is dull pain ,felt at the xiphi sternum ,above , or below it.
Dyspepsia is common and worse in when pt. lie dow. There might be a sharp element i due spasms
ATYPICAL CHEST PAIN
3- Mitral valve prolapse;-
Commoner in young and thin girlsPricking or soffocating feeling with SOB
Unrelated to exrtion associated with palpitations and numbness of left arm Has no risk factors for IHD
Migrain or Irritable bowel syndrome are common
Examination, ECG and CXR are usually normal .
Rarely M.V prolapse is significant leading to Mitral regurgitation with Systolic click and late or pan-systolic murmur. This leads to L.V dilatation which if severe
cause SOB and EVEN LV failure
Atypical Chest Pain
3- Mitral Valve Prolapse;-Commoner in young and thin girls
Pricking or suffocating feeling with SOB
Unrelated to exertion associated with palpitations and numbness of left arm Has no risk factors for IHD
4- Migraine or Irritable bowel syndrome are common
Examination, ECG and CXR are usually normal .
Rarely M.V Prolapse is significant leading to Mitral regurgitation with Systolic click and late or pan-systolic murmur. This leads to L.V dilatation which if severe cause SOB and even LV failure
Atypical CHEST PAIN
4-- Pleuretic pain : It is due to pleurisy
Pain is sharp
More lateral and
Related to breathing and coughing.
5- Acute Pericarditis Usually due to viral infection
Pain usually dull or sharp
Worse on lying and relieved by sitting up
Pericardial rub is the diagnostic
Rare causes of Chest pain
6-Costo-Chondritis (Tietze disease)Dull or sharpe pain at those joints.
Tenderness on pressing the joint
7- Herpes Zoster of the left thoracic nerve
Severe burning pain like fire along the intercostal space
Rash with the vesicles will be diagnostic.
LATER This might cause Post herpetic neuralgia
Ischaemia
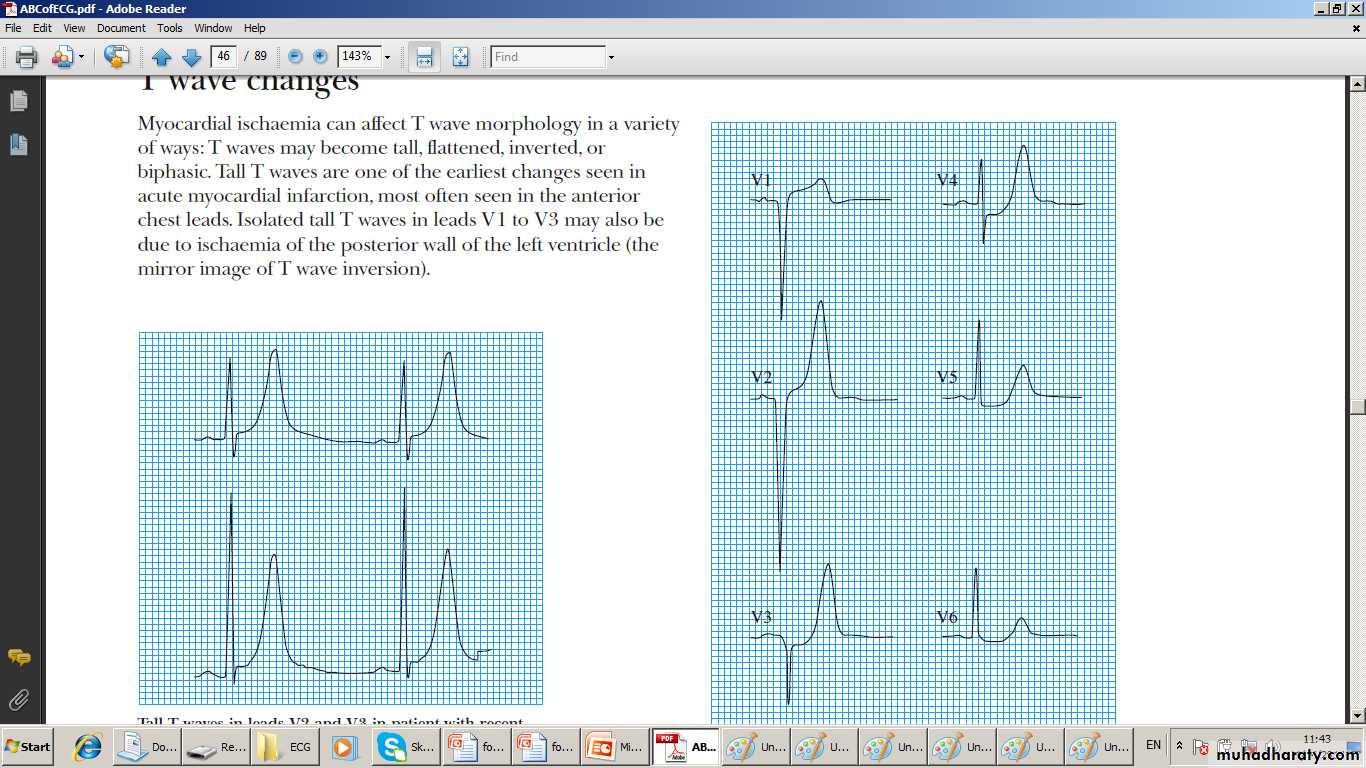
Left :Peaked T wave early ischaemiaRight :ST segment depression Ischaemia
Exercise Mechine
ST depression induced by Exercise
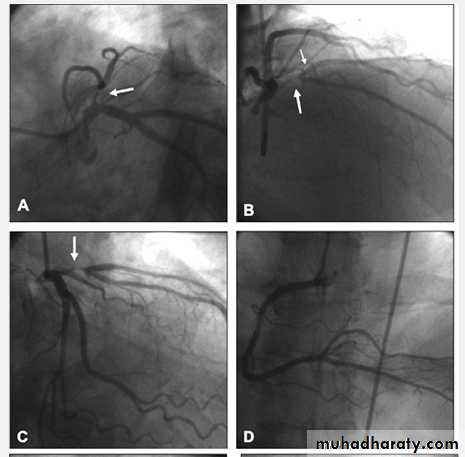
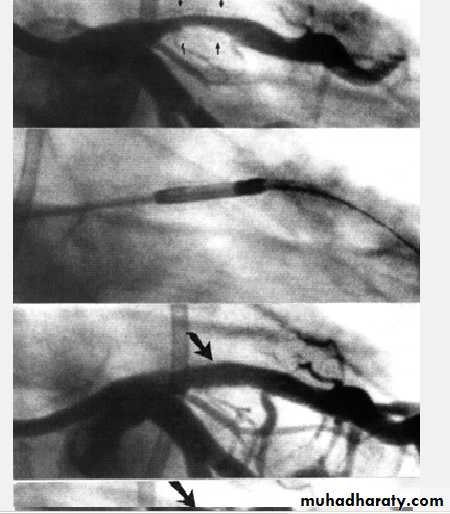
Severe proximal LAD Lesion
Very severe proximal LAD stenosis
Total CX Occlusion
Management of chronic stable angina
It involves1- Life style changes
2- Control of symptoms
3- Control of Risk Factors
4- Assessment of severity and Extent CAD
5-Identify high risk pts who may need revascularization
Life style changes
Take ExercisesAim at ideal weight
Avoid Smoking
Avoid strenuous or competitive tasks
GTN prior to angina-precipitating exertion
Control of symptoms and Lipids Quadruple therapy
1- Nitrates
2- Betablockers
3-Antilipids
4-Antiplateles
Plus
Ca antagonists
K Channel activators
I channel antagonists
Quadruple Therapy
1- Nitrates reduce demand and increase supplyGTN 0. 5 mg tab S.L. on need up to 12 tab.s daily
Isosrbide Dinitrate 10-20 mg 8 hrly
Long acting ; Mononitrates 2o-60 mg 12hrly
Nitratess free zone to reduce tolerance.
headackes needs analgesics initially
2- Betablockers Cornerstone of RX
Reduce Demands; reduce HR, BP, Contractility
Be carful in Asthma by monitoring PFR
Be careful in L.V failure start small dose
Quadruple therapy 3-- Anti lipids
A -Cholesterol Lowering Agents
Statins Act by blocking HMG CoA Reductaze in the liver hence effectively reduce LDL
Start Statin therapy ((start with Atorvastatin 20 m daily) irrespective of serum level to all pts
The new guideline use high intensity Statin therapy to cut LDL to < 50% of its baseline if it was is higher than 190mg /dl or < 30% if it was 70-190 mg/dl
Ezetimibe 10 mg BID if intolerant to statin
Quadruple therapy Antilipids and anti-platelets
Triglycerides (TG) lowering agents;Fibrates reduce synthesis and enhance catabolism 1-Gimfirozil 600mg BID is used
2-Fish oil 6.0 grams daily if needed
Side effects of Statin and Fibrates include Myopathy and arthropathy
4- Antiplatelets
1- Aspirin tab. 100m daily is effective.
2- Clopidogrel 75 mg /d is an alternative if pt. is Aspirin intolerant
OTHER Anti anginal therapy
A- Calcium antagonists Inhibits Ca influx leading to reduced BP. and Contractility. lowers O2 Demand1- Nifedipine 10-20mg TID it induces
tachycardia hence Betablocker is necesary
2- Diltaizem 60 mg TID if betablocker is not used
B- K channel Activator arterio-venous dilator such as Nicorandil 10-20 mg TID.
C- Ion channel antagonist. Inhibits the Sinus Node leading to Bradycardia; without affecting the L.V. Function. Itlowers O2 Demand
IVABRADINE 10- 30 mg BID is the only one
ACE or ARB for L.V. Dysfunction
Angiotensin Converting Enzyme (ACE) Inhibitor
OR Angiotensin Receptor blocker (ARB) in pts with L.V dysfunction
An important addition to this Quadruple therapy is An ACE inhibitor such Captopril is necessary.
Or an ARB such as Valsartan 80 mg / d
is a good alternative if cough ( a side effect)
is distressing Unfortunately both are contraindicated during pregnancy
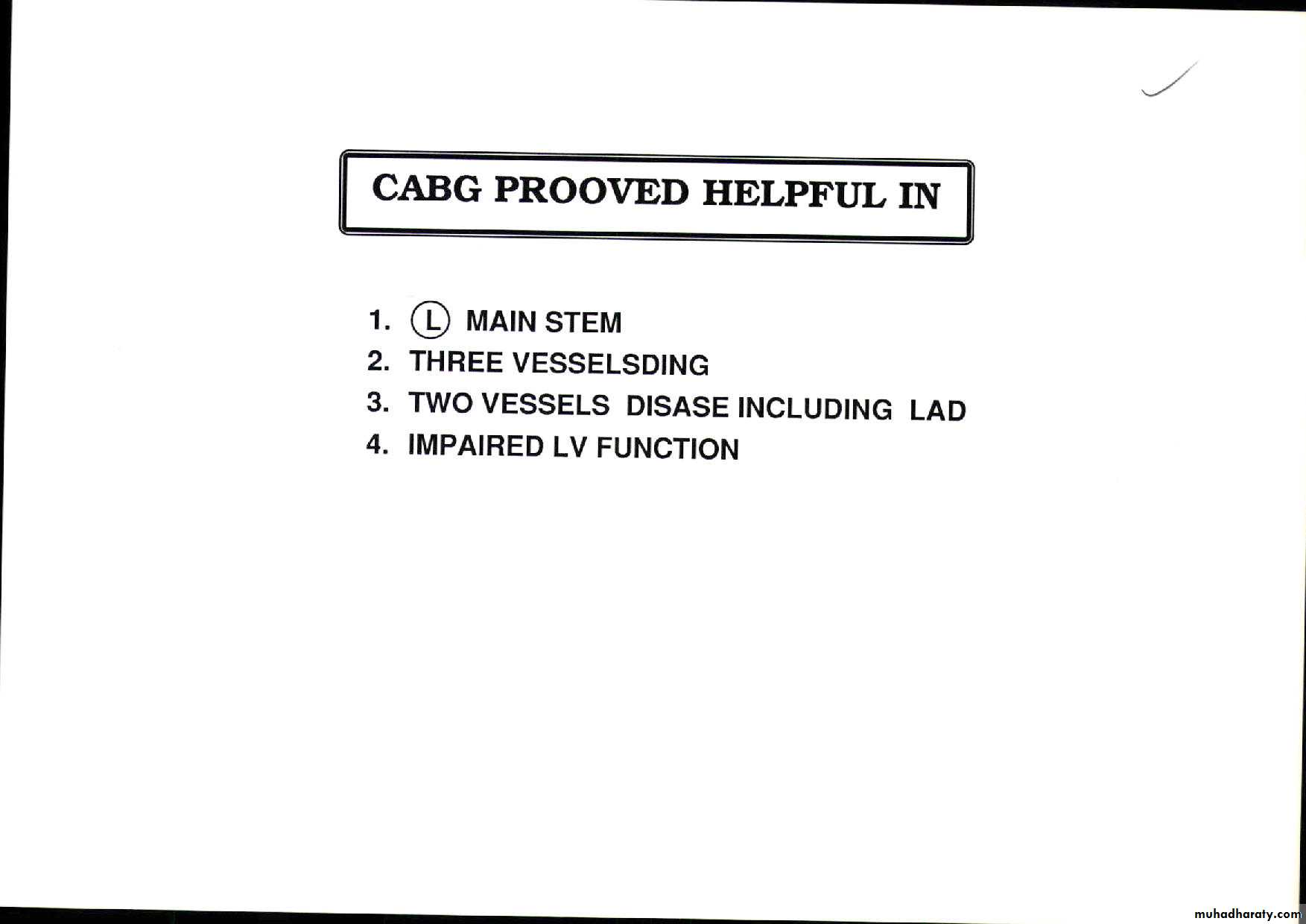
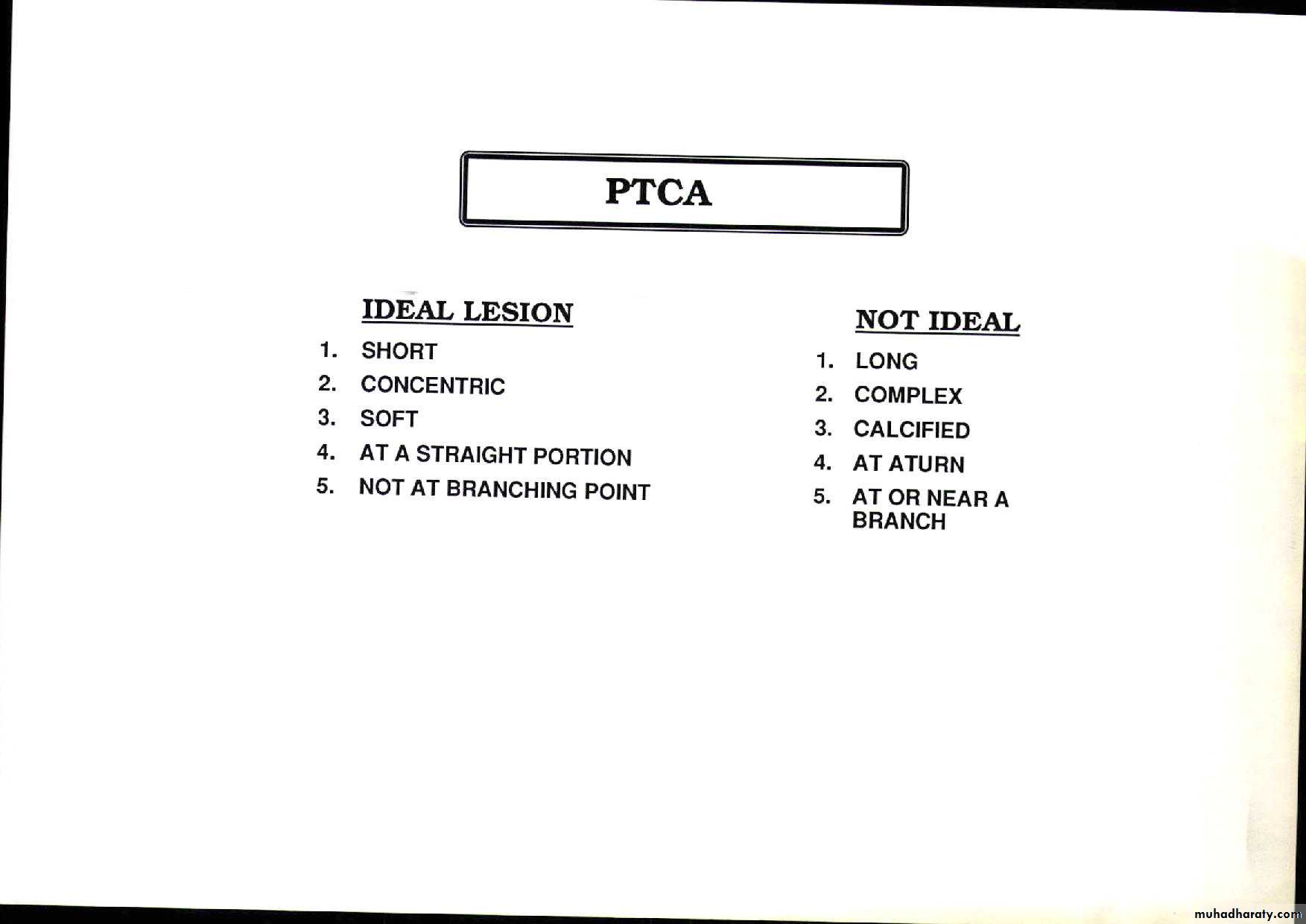
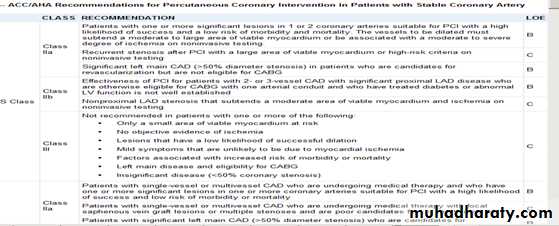
RevascularizationPercutanous C. Intervention (PCI) or C.A Bypass Grafting (CABG)
PCI which include Balloon Angioplasty + - Stenting Is indicated in discrete single vessel or two vessel lesions except that of the Proximal Left Anterior Descending artery LADCABG is for Left Main Stem lesion , Three Vessel Disease, and proximal LAD 1-2 vessels Disease
Especially diabetic pts and also those with LV dysfunction
Benefits and drawbacks of PCI
PCI benefitsImproves symptoms only (no evidence it improve survival ) and used for stenosis of native CA or graft .
PCI drawbacks ( related to lesion morphology, operator skills, and co morbidity ( page 588 Davidson)
1- Dissection and or Thrombosis ( 2-5%) Usually corrected by stenting
2- Restenosis occur in up to 33% in Angioplasty and reduced by Stenting with Bare Metal Stent ( BMS ) and reduced further by using Drug Eluting Stents (DES). Restenosis still occur in 10%. Dual antiplatelets needed
3- Late stent thrombosis occur in 0.6 % every yr.
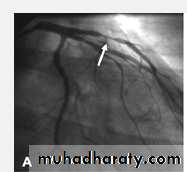
Proximal LAD PCI
Bifurcational lesion PCI
CABG benefits and drawbacks
CABG benefits1- Relives symptoms in 90% 1yr and 60% in 5 yrs
2- improve survival.
More benefits in total arterial Bypass and Off-pump
CABG drawbacks
1- Op. Mortality is 1.5% and higher in the elderly
and those with co morbidity.
2- Repeat Revascularization 2% in 2yrs
3- Stroke in 1-5%
3- Cognitive impairment (30-80%) mostly resolve at 6
months. Reports of a long term one (30% at 5 yrs)
Primary PreventionPopulation strategy and Targeted Strategy
A- Population strategy :-
Life style changes:-1- Exercise. 2- Diet to maitain ideal weight, 3- no smoking
Regular Exercise Brisk such as Brisk walking or
Cycling or Swimming for 20 min. 3 times/week
Healthy Diet Less fat ;- down to 10% of calories
Rich in fish vegetables and fruits
B- Targeted Strategy
Calculate the composite Risk Score to identify pts with risk factors ( high risk) and advise-treat them
Secondary Prevention
Life style of Primary preventionAspirin
Statin irrespective serum cholestrol and High intensity statin for high cholestrol
ACE inhibiyor even in normal L,V. Function
Control BP. Below 140/90
Good control of D.M
Acute Coronary syndrome
ACS encompasses wide spectrum of Acute Ischaemic syndromes starting with Unstable Angina through Acute Non ST-elevation MI to Acute ST-Elevation MI.It extends from Recurrent Angina at one end , to include sudden death due to extensive MI and Cardiogenic shock.
If the chest pain and the RFs are classical ACS can confidently diagnosis by history only. Investigations will confirm the diagnosis and will subclassify it and assess the severity of the case.
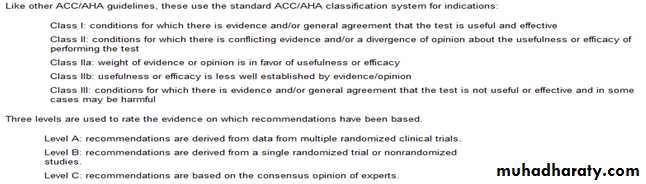
Acute Coronary Syndrome Unstable Angina Clinical Classification
UA is divided into four categories depending on the clinical Characteristics of the pain of
1- New onset Angina
2-Rapidly deteriorating Angina
3- Angina at rest
4- Long episode of angina Up to 30 min but without cardiac damage.
The pain can be recurrent or variable in intensity (wax and wane) and dictated by the coronary flow which is determined by stenosis severity, the underlying thrombus , and the possible spasm
Acute coronary Syndrome Acute MI Sub-classification
It all depends on whether the patient hasEvolutionary ST-Segment Elevation or NOT
Hence we two type
1- Acute ST Elevation MI (STEMI)
2- Acute Non-ST-Elevation (NSTEM)I
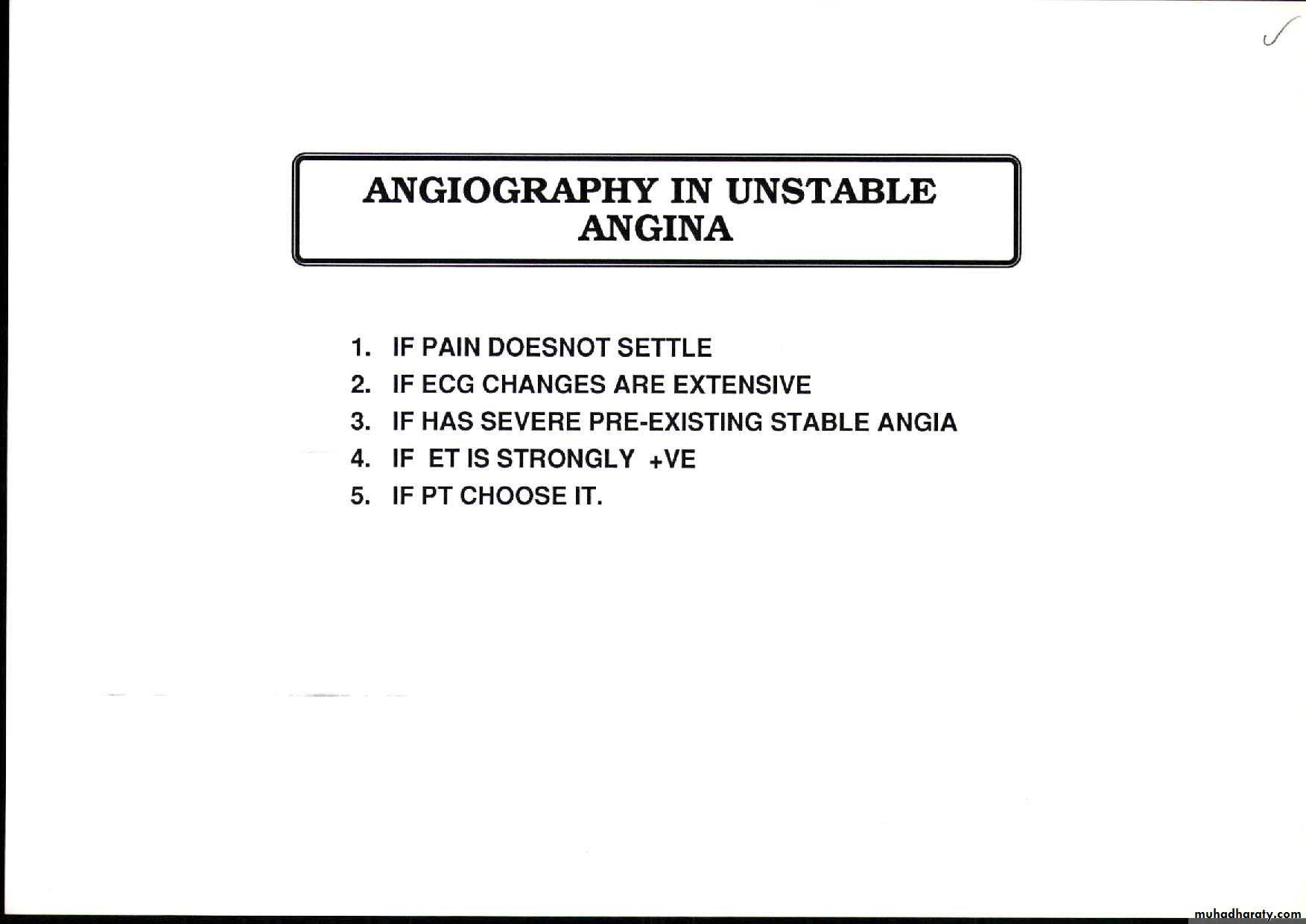
Acute coronary Syndrome Unstable Angina investigations
ECG and EchoLike CSA both ECG and Echo can show evidence of Ischaemia during pain.
Cardiac enzymes as markers of myocardial damage are normal.
Troponins
Troponins are usually negative
Nowadays with advent of highly sensitive assays small minority of pts with UA a rise of troponins can be detected and is regarded as high risk group or they are regarded as Non St Elevation MI
UA Diagnosis
1-Classical pains in a susceptible pt is diagnostic
2-Investigations may confirm or exclude the diagnosis
3-if the case is doubtful the pt must be labeled as suspected UA and managed like a certain UA case until the diagnosis is clear.
UA Assessing the Risk
1- Calculating Grace Risk scoreIt is calculated to identify high risk pts (; high risk of death or MI) . It is based of recording admission clinical findings :- Age HR, BP, RFT, CCF, STE, C arrest , Troponins. Medium score (1-9), and High score ( >9 ) scors pts need invasive approach ie Coronary angiography and Revascularization Low Risk pts ( score <1 ) go for Conservative Rx
In addition High Risk pts are those with
1- Recurrent ischaemia 3-- Diabetics.
3- Haemodynamic compromize
Common Management of UA
1- CCU admission 2- Serial ECG, 3- Biomarkers and 4- Haemodynamic moitoring 5- > 60% Oxygen6- Aspirin 100 mg or Clopidogril 75 mg
7- Nitroglycerine infusion 0.6-1.2 mg/hr or ISDN 1-2 mg/hr is given it can relive pain if maximal dose fail to relieve pain then use Narcotic analgesics
8-The Pentasaccharide Fondaparinux 2.5 mg s.c or The LMW heparin Enoxaparin 1.0 mg/kg 12 hrly i
9- I.V. Betablocker Atenolol 5-10mg or Metoprolol 5-15m every 5.0 min followed by oral Atenolol 50mg daily or Metoprolol 50mg twice a day
10 – Statin eg Atorvastatin 20 m orally
Specific Treatment for the Invasive strategy
This group will be sent for intervention. They will be given in addition to the common RX
1- High dose Clopidogril 600mg then150 mg for one week,and the 75 mg afterwards
Or Ticagrelol 180 mg then 90 mg 12 hrly
2- GP 11b/111a Receptors Blockers such Tirofiban or Abciximab a powerful antithrombotic agent will be infused before and during the Intervention .
The teacher’s story
He was put on ISMN 20 mg/d, Atenolol 50 mg /d Atorvastatin 20 mg /d, and Aspirin 100mg /dHe stopped smoking He became asymptomatic.
Then he was lost to follow up
Two years later He appeared in the casualty when he developed prolonged chest pain (for 20 min) with sweating. He admitted that his pains has recently become more frequent and occurring even at rest but with no nausea or vomiting. His wife said he was not complaint with medications and he was still smoking
His Examinationn and his ECG were normal. His Trop- onins were negative He was admitted to the CCU as a case of Unstable Angina ie Acute coronary syndrome
Teacher’s chest pains
He was treated as a case of Unstable Angina He was labeled as high risk pt. because he is diabetic and his LV function were moderately impaired on Echo. Hence he was scheduled for Invasive strategy. His pains settled . He felt better. He refused catheterization and went home . eACS other symptoms
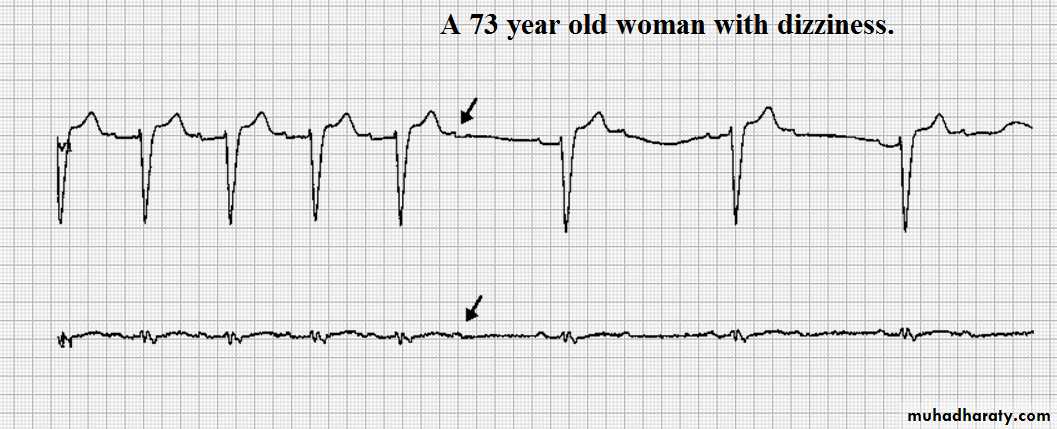
SOB depends on the amount of the LV dysfunction which becomes worse with pain reaching the feelong of suffocation. If the amount of Ischaemia is large it may lead to transient acute LV failure.Palpitation and syncope can occur and are more frequent in extensive underlying disease.
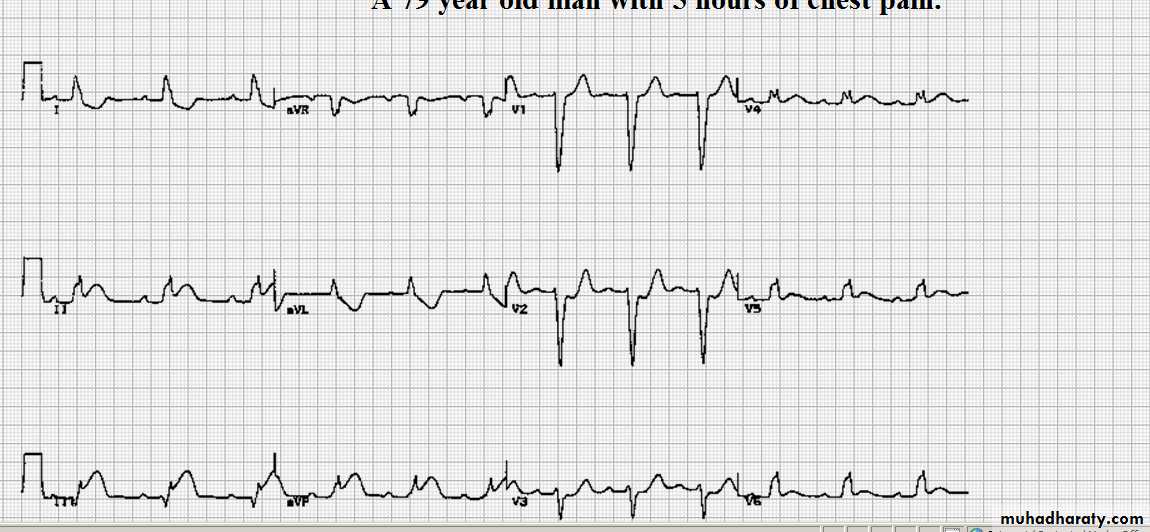
The Teacher’s story
Few weeks later he presented with severe retrosternal pain increasing in severity for an hr. The pain was constrictive associated with sweating and nausea but no vomiting .His ECG showed 2 mm ST depression and Symmetrical T wave inversion on V2-5
BIOMARKERS were more than twice normal
He was Treated as NSEMI in the causality and
improved he refused admission and decided to go home against advice.
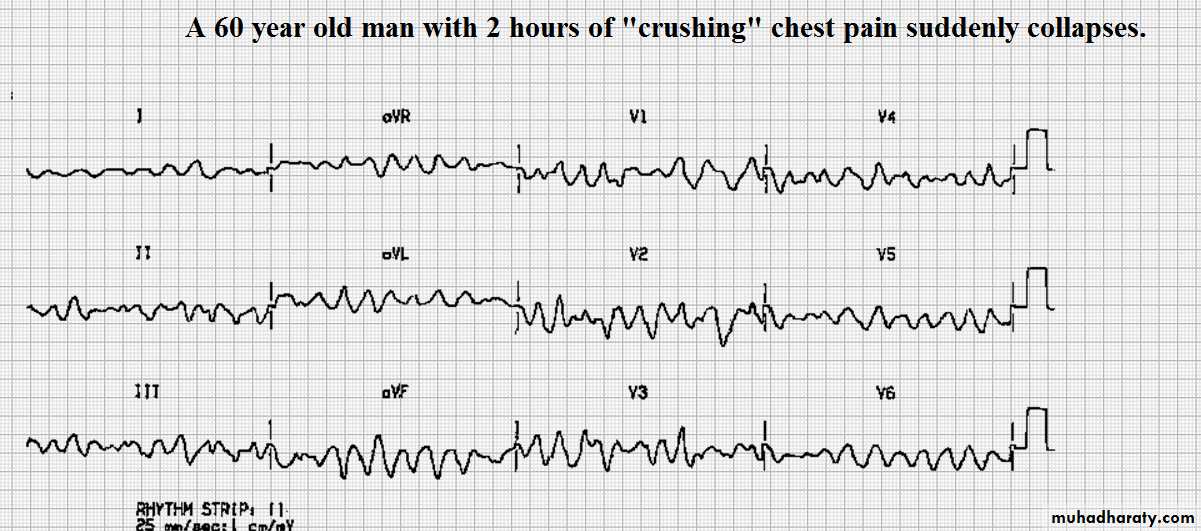
The Teacher’s Story continued
Few days later he developed severe continuous burning pain across his chest with profuse sweating , nausea and vomiting and arrested with VF on arrival there.
He was promptly resuscitated and converted to sinus rhythm by DC cardio version
his subsequent ECG showed ST segment Elevation by 5 mm on V3- V6 he was shifted to the CCU .
Acute Myocardial Infarction
Acute Ischaemic Myocardial necrosis due to sudden interuption of blood supply by an occlusive thrombus at the site of rupture or erosion of atheromatous plaque.Complete occlusion causesAcute Transmuural infarction ;- Acute ST-Elevation MI
If the ensuing ischaemia is not involving the whole thickness off the wall then it causes Nontransmuural MI usually the subendocardial layer ie Non ST-Elevation MI
Thrombosis in ACUTE MI
Occur on the background of a plaque of any sizes but more frequent on a small plaque ; mild stenosisPlaque is usually cellular, soft, and sealed by a thin cap that will crack or ulcerate
Thrombus formation is a dynamic process. It can dissolve and reform depending on the balance between endogenous thrombolysis and platelets disaggregation
Usually spontaneous lysis will prevail . HENCE only
20-30% of patients are left with total occlusion
Obviously The underlying stenosis remains
Symptoms of Acute MI
1- Pain is the cardinal symptom.similar in characters CSA pain but it is usually
A- Severe
B – lasts longer >30 min
C- Constricting ,Suffocating Chocking or Weight-like
D- Retrosternal or across the chest and may be felt
in the throat, epigastrium, arm, or in the back
2- SOB is common. This can be the only symptom
3- Palpitations , Syncope and Collapse may occur .
They are due to Arrhythmia and Hypotension
4 -Can be Silent in the elderly or the diabetic
Signs of ACUTE MI
1- Signs of Sympathetic stimulation :- Tachycardia ,Pallor, and Sweating2- Signs of Parasympathetic stimulation :-Vomiting and bradycardia.
3- Signs of impaired function :- Hypotension Oliguria, cold peripheries Thredy pulse, queit 1st Ht sound, 3rd heart sound, diffuse apex, and basal crepitations.
4- Signs of tissue damage :- Fever
5- Signs of complications:- Mitral regurgitation, ETC
6- Sudden death VF can the first sign. The risk decrease as hours pass. LV .Failure comes after
&- No SIGNS ie Silent
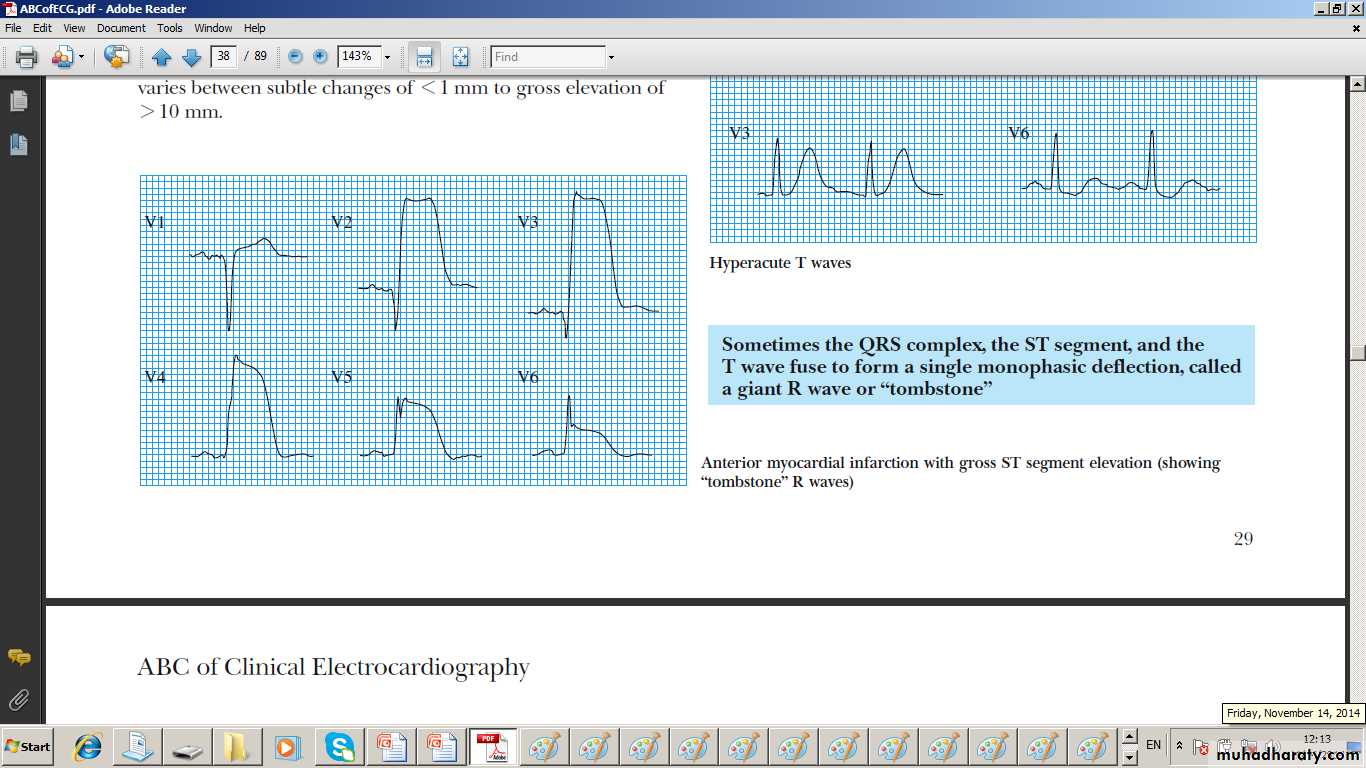
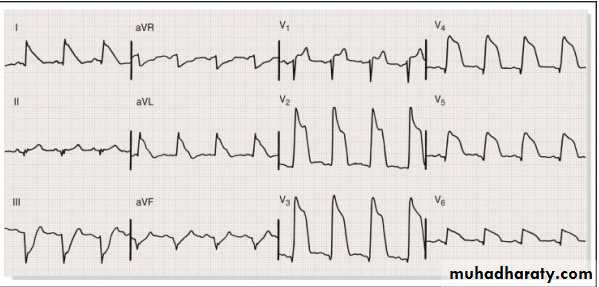
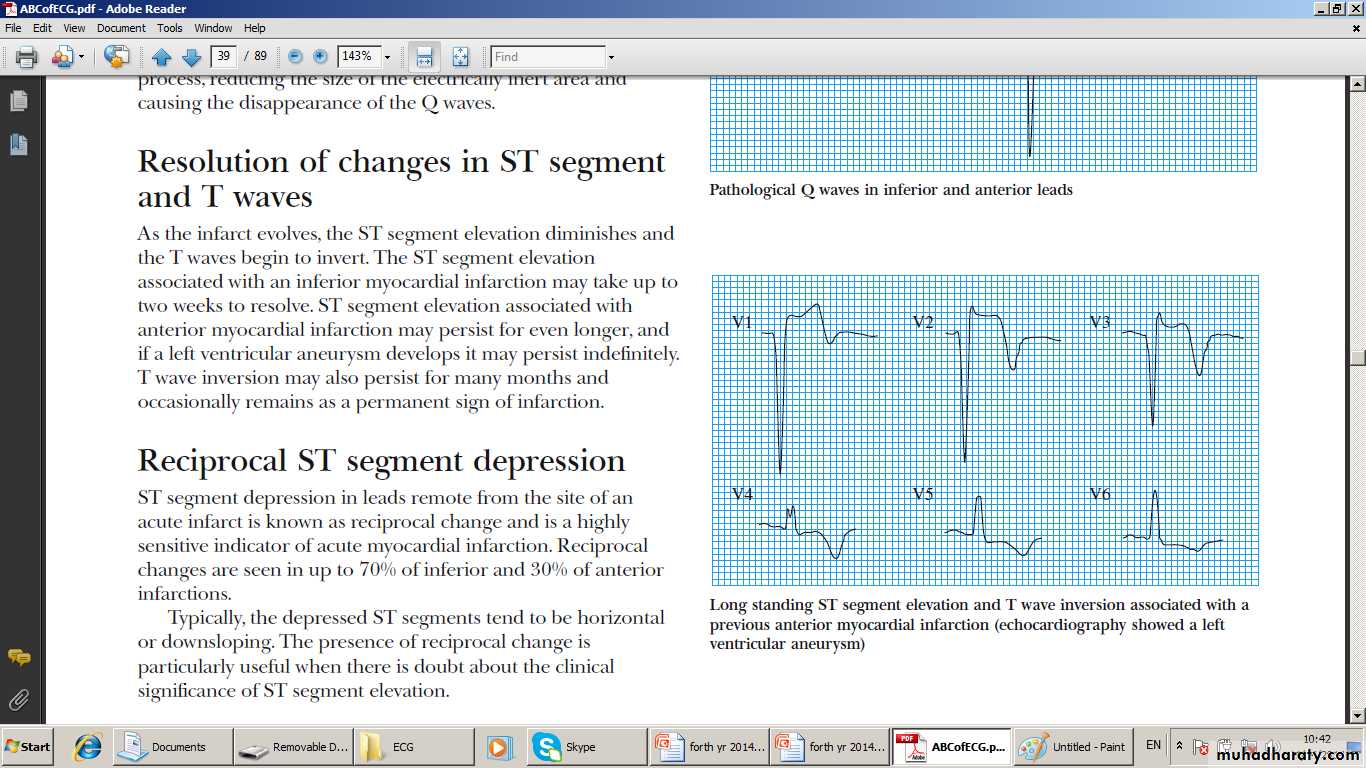
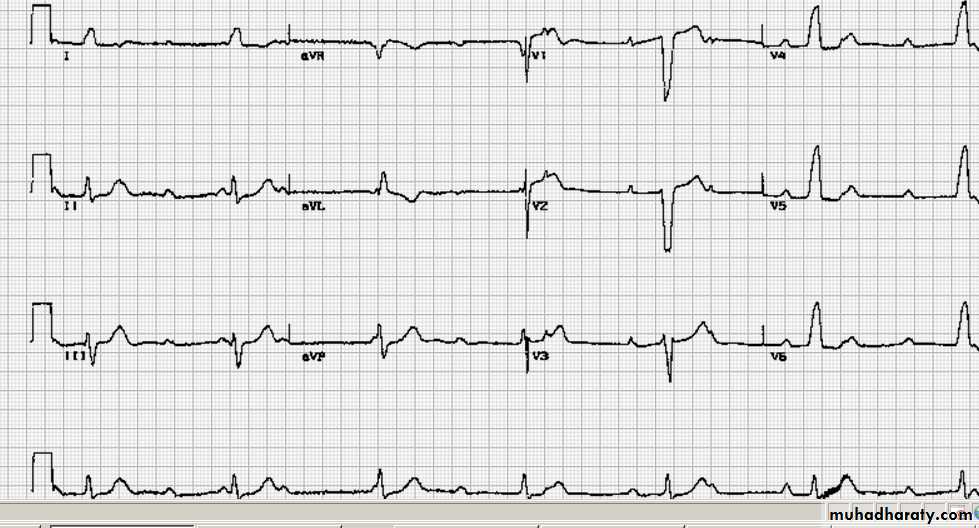
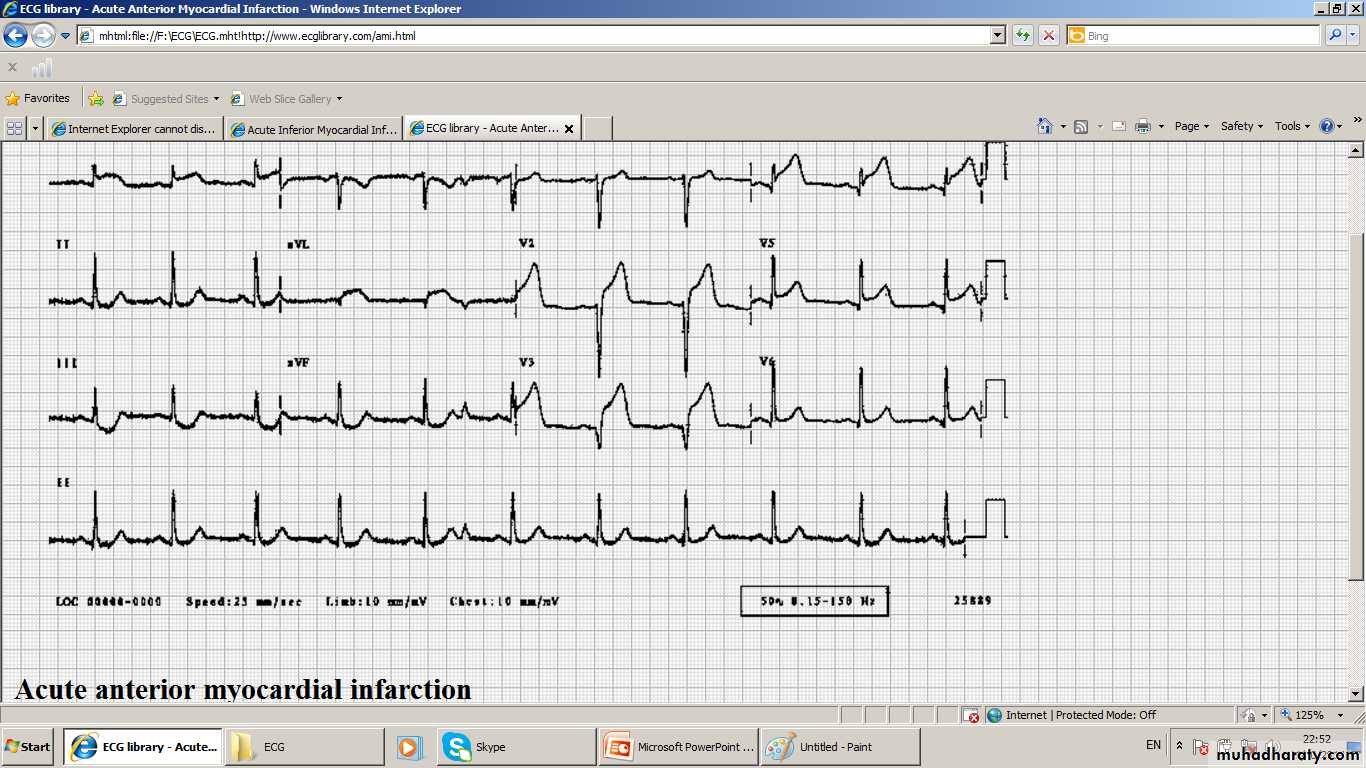
Evolution (Sequence) of MI ECG changes
1- STEMI (ST-Elevation MI)
Total occlusion of a major CA proximally causes
ST Elevation
R diminution
Q appearance
T- inversion that may persists .
2- NSTEMI ( Non ST elevation MI)
Partial occlusion of major CA or total occlusion of a minor vessel
1- ST depression
2- R- diminution.
3- T- inversion, may be deep and symmetrical
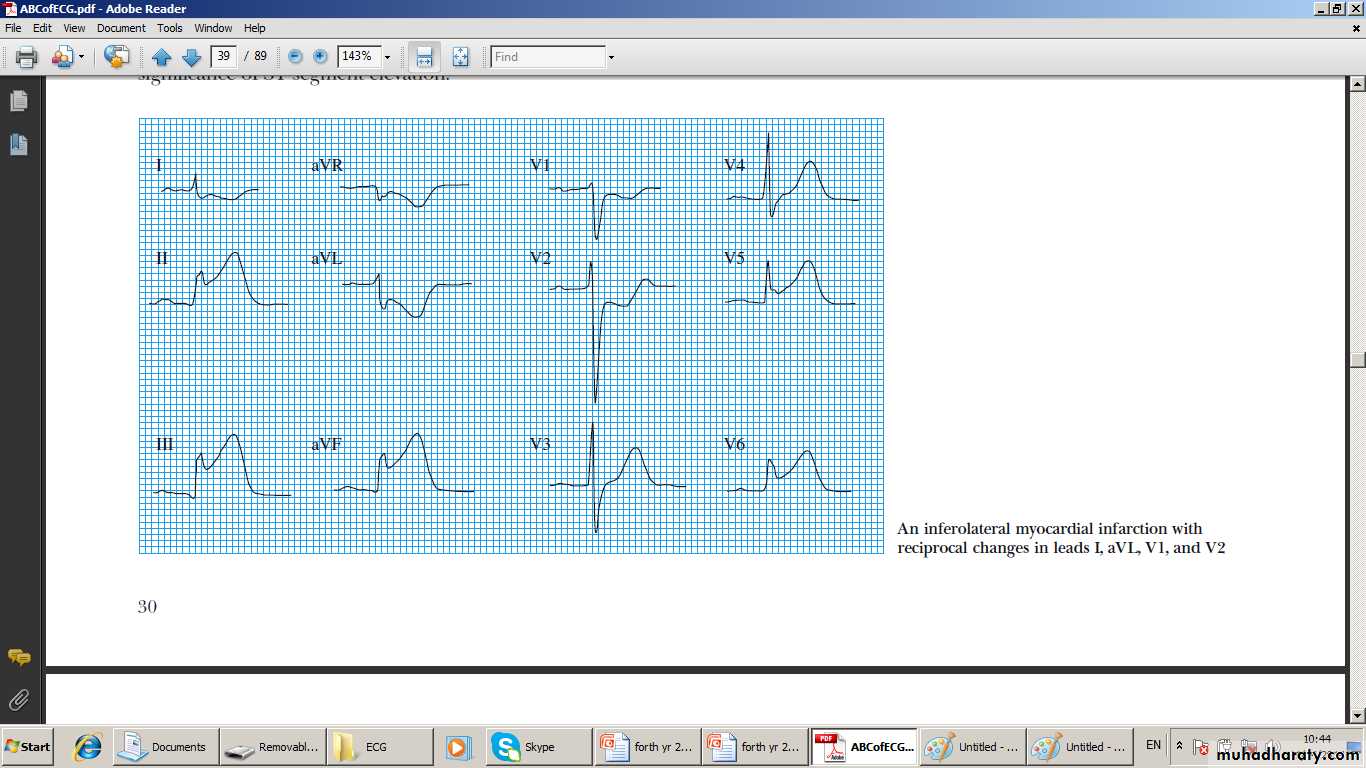
Localization of MI by ECG changes (needs two adjacent leads)
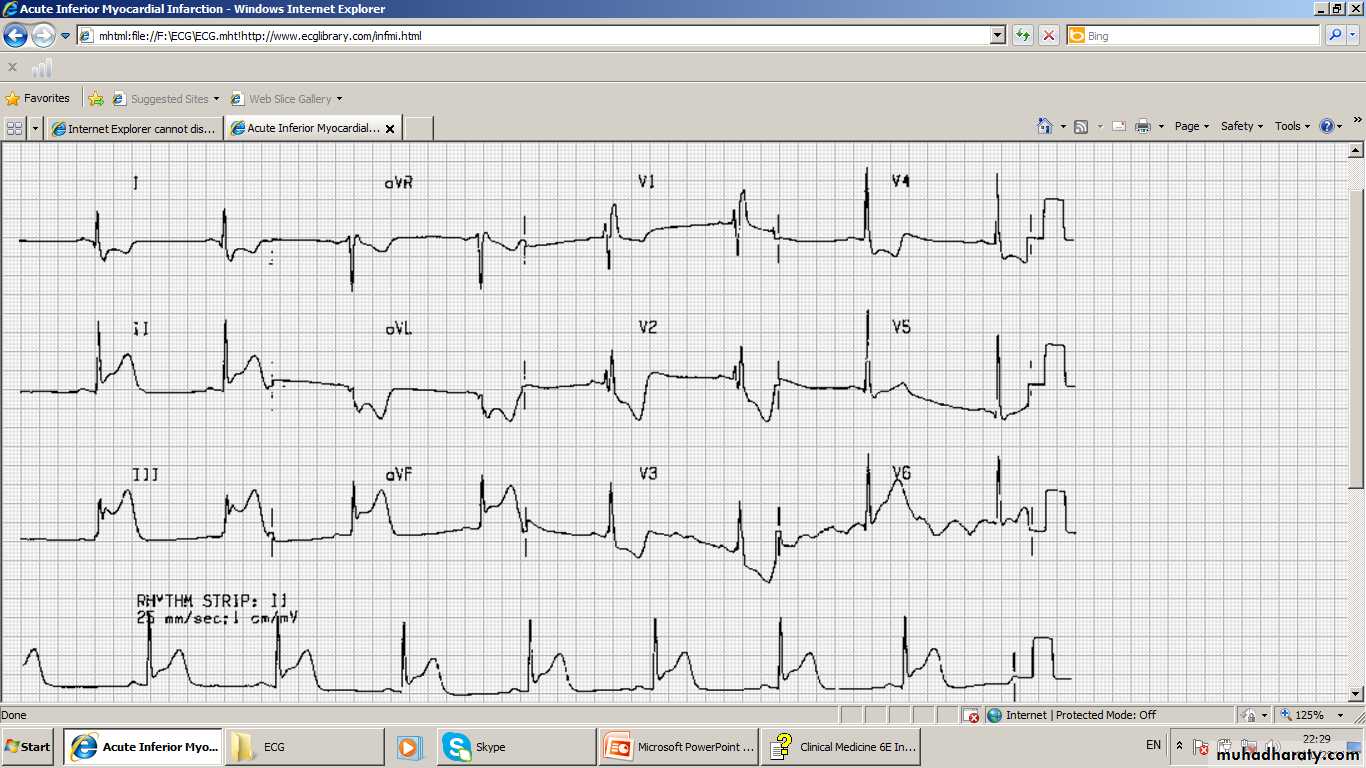
Anterior MI V2 –V6Inferior MI LII and / or LIII + AVF
Lateral MI LI and AVL +- V5-6
Antero-lateral V2 – V6 + LI and AVL
Infero-lateral LII -LIII + AVF and L1 + AVL
Antero-Septal V2 –V4
True Posterior V1 – V4 ( Tall R + ST↓)
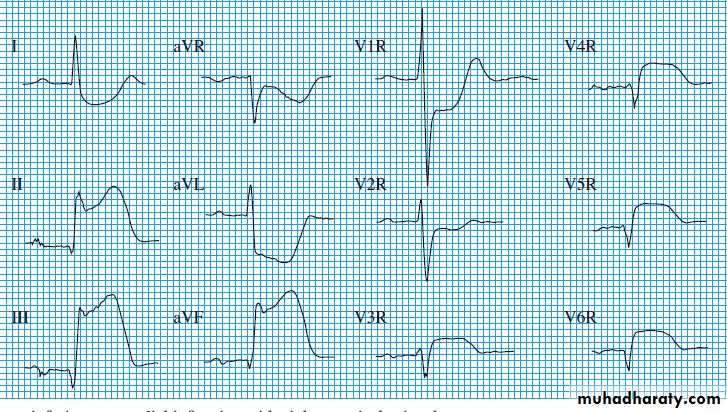
RV Infarction Inf. MI+ VR3-4
Acute Anterior MI
Acute Infero- lateral MI
Acute inferior MI and RV infarction
True Posterior MI
Persistent Q Wave indicates Old MI Persistent ST elevation May indicate Aneurysm
Acute Inferior MI and Partial RBBB
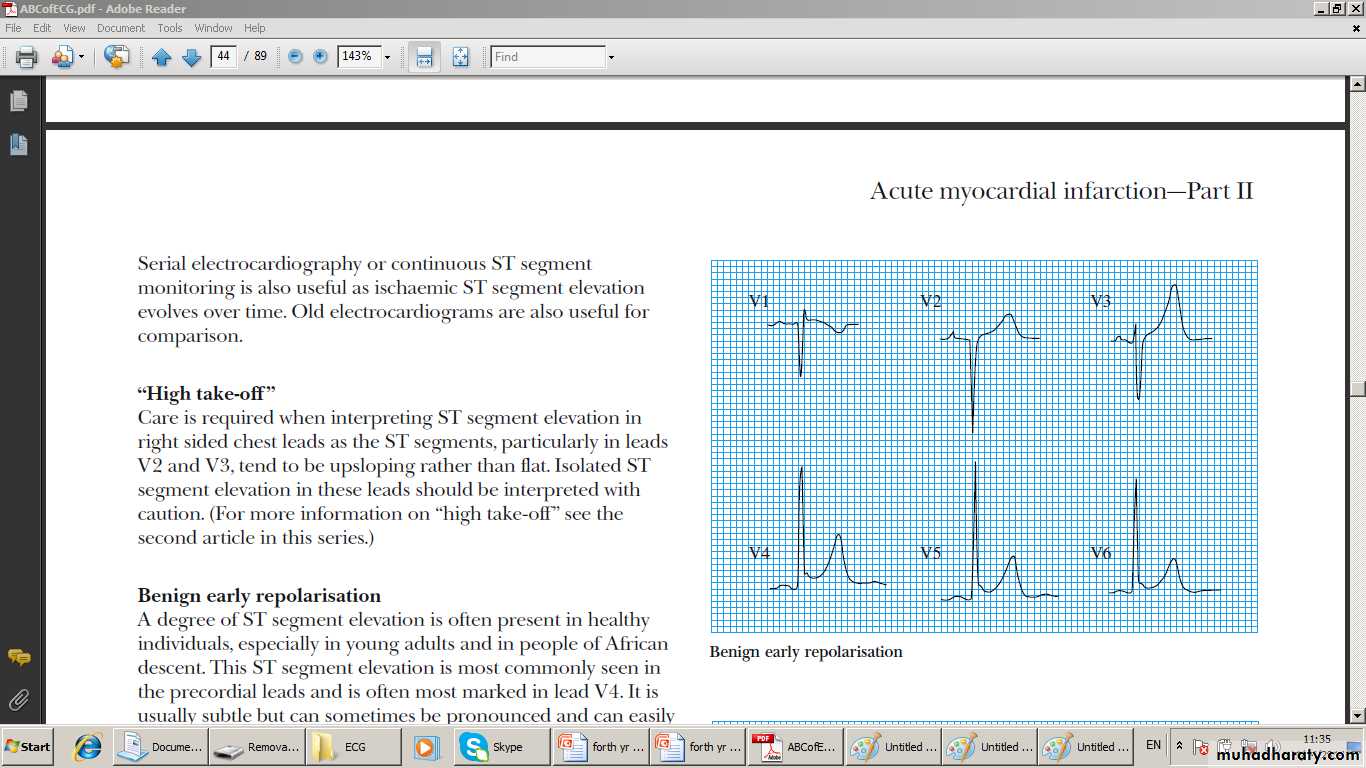
Normal Variance ST elevation
CA spasm and LVH
Biomarkers and Cardiac Enzymes
Troponins I an T are very sensitive They rise early (in 4-6) and stay elevated up to 2 weeks days . Can rise in Pul embolism .and Acute Pul oedema but not in cardioversionCKMB Rises Early in( 4-6 ) and drops in 48-72 hrs (not released from cardioversion)
Myoglobin rises very early (2-3 hrs) and drops quickly. It can also be released from skeletal muscles
Diagnosis of Acute MI
One of the following meet the diagnosis of MI :-
1- > Twice normal rise and fall of Biomarkers or
Cardiac Enzymes with one of the followings
a- Symptoms of Myocardial Ischaemia ie Chest Pain
b- ischaemic ST-T changes or new LBBB or new
pathological Q-waves
c - Immaging evidence of loss of viable
myocardium or new regional wall motion
abnormality
2- Cardiac arrest or sudden death with one of the above
and / or evidence of fresh thrombus on angiography
3-Pathological finding of Acute MI
Diagnosis of A MI
1- Troponins or Enzymes(T or I) (rise and fall)
PLUS either
2- Pain OR ECG
(Ischaemic) ( Evolutionary)
Other investigations
↑ WBC Peak CXR Echo + Doppler
1st day Early: Normal Size heart 1. Hypokinesia /
↑ ESR Peak in ± LVF Akinesia
few days LV or
Later: cardiomegaly RV dilatation
in most cases 2. Detects
complication
a. P. effusion
b. MR
c. VCD
d. Cardiac
rupture
Adverse outcome of Acute MI
1- Recurrent Ischaemia2- Extensive ECG changes at rest
3- release of Biomarkers ; Troponins or Enzymes
4-Arrhythmias
5- Haemdynamic compromize
Estimated mortality of Acute MI which occur mainly in high risk patients.
__ 20% die during the fist six months. More than half of them (12%) die during the first month
--- 20% or more die at home
TOTAL MORTALITY Up to 50%
Management of ACS especially Acute MI
• 1-Ambulance + defibrillator +-A doctor (G.P)
• 2- Hospitalization CCU
3- Bed rest + Canula + Oxygen > 60%
4- Serial ECG, Biomarkers. and close haemodynamic monitoring.
5- Antiplatelets :-
a- ASPIRIN 300mg initally then 100 mg after
b-Clopidogrel 600mg , 150mg for aweek, then75 mg
c- OR Ticagrelol 180 mg the 90 mg afterwards
d- GP 11b/111a receptor antagonist Abciximabe or
Tirofiban if PCI is needed
Mangement of ACS especially Aute MI
6- Narcotic Analgesics ;_a- Morphine 5-10. mg or Diamorphine 2.5-5 mg.IV
b -Antiemetic :- Metoclopramide 10.0mg (I.V)
7-Anticagolants:-
a- The Pentasaccharide Fondaparinux 2.5 mg s.c
b- Or LMW heparin Enoxaparin 1.0 mg/kg 12 hrly
8 – Antianginal therapy
A- Nitrates
a- GTN 500ug is suitable first-aid measure in
Unstable Angina and threatened infarction.
b- Nitroglycerine infusion 0.6-1.2 mg/hr or ISDN 1-2 mg/hr is given it can sometimes relive pain ,
Mangement of ACS especially Acute Mi
9- – Beta-blockers
a- I.V. Betablocker Atenolol 5-10mg or
b- Metoprolol 5-15m every 5.0 min followed by oral Atenolol 50mg daily or Metoprolol 50mg twice a day. Try to give smaller doses in LV Failure, hypotension and Bradycardia otherwise avoid it th
C- Calcium Antagonists
a- Nifedipine 19 mg 8 hrly or amlodipine 5-10 mg forpersistant pain
b- use Verapamil or ditaizem if Beta blocker are conraindiated eg Pul Oedema. And asthma
10 – Statin eg Atorvastatin 20 m orally
11- Reperfusion Therapy
1 -NSTEMI –Emergency Reperfusion may be harmful however sellected Medium and High risk NSTEMI pts may benefit from emergency Reperfusion Therapy
2- STEMI
Immediate reperfusion if successful will
A- Restore coronary flow
B- Preserve left ventricular function
C- Improve Survival
D- Relieve pain
E- Resolve ST elevation
E- May induce transient idioventricular rhythm
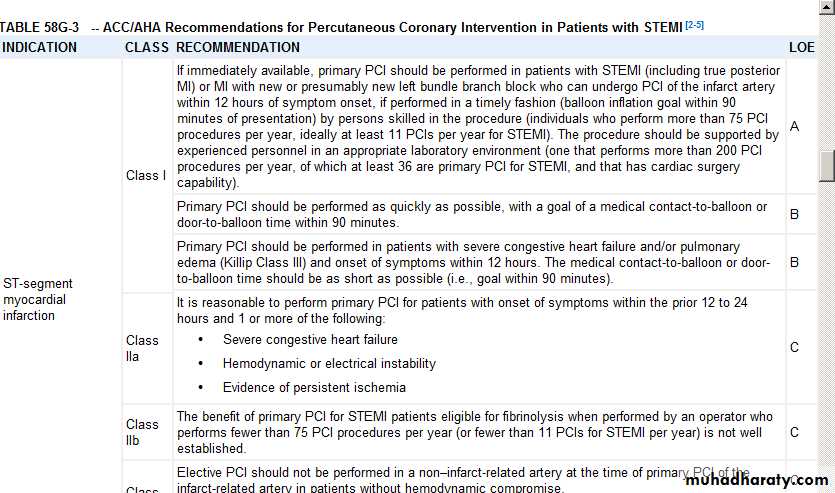
Primary Percutanous Coronary Intervention Primary PCI
1- Primary PCI is the best treatment of acute STEMI.
2- Best with GP11b/111 a antagonist and stent
3-Better than Thrombolysis in reducing MACE ie
Major Adverse Cardiac Events ; death MI, stroke
4- Limited by a- It is not widely available
b-Must be done in 2 hrs from onset
5- Indicated within 12 hrs from onset of pain and within 24 hrs in high risk cases.
6 has to organized and performed quickly in a timely fashion ; the goal of Door to Balloon time of 90 min from presentation
Rescue PCI or delayed PCI
Rescue or delayed PCI is indicated1- if Thrombolysis had failed in achieving reperfusion as evidenced by ST Elevation fail to drop significantly
2-Or symptoms continue
3-Or pt has haemodynamic compromise
4- 0r uncontrolled malignant arrhythmias
Thrombolysis
1- Can reduce mortality by 25-30%
2- Survival benefits is maintained for 10 years
3- The earlier the better or minutes mean muscle.
If given to pts with
a- ST elevation . 1 mm in limb leads
b- OR ST elevation 2 mm in chest leads
c- OR LBBB
Then Short term ( 6 M) Survival will be ;
a- 1- 6 hrs from ONSET 50 more lives per 1000
b- 7- 12 hrs from onset 40 more lives per 100
c- Otherwise no benefit if not harmful
Relative Contrandications to Thrombolysis
• Recent surgery within one month• Uncontrolled hypertension
• Previous subarachnoid and intracerebral bleed.
• Recent Trauma including that of cardiac resuscitation.
• Active internal bleeding.
• High probability of active ulcer
• pregnancy
tPA
4- tPA ; human tissue Plasminogen Activator;
15 mg IV bolus
< 50 mg Infusion over 30 min. (0.75 mg/kg)
<35 mg infusion over 60 min. (0.5 mg/kg)
Better Survival than Streptokinase
But slightly more Intracerebral bleed;
10 per 1000 more survivals BUT;
1 per 1000 more nonfatal intracerebral bleeds
Hazzards
Five extra non fatal stroks per 1000
0.5-1% other major bleeds . Hence witheld if there is risk of significant bleed
Thrombolysis ; tPA Analogues
5- tPA analogues1- TNK Teneteplase and Alteplase
a- Same survival and cerebral bleeds
b- bolus IV ; hence easier and quicker
c- Can be given before hospitalization.
d -Less peripheral bleeds
11- rPA Retaplase
a- Same survival and cerebral bleeds
b - slightly more peripheral bleeds
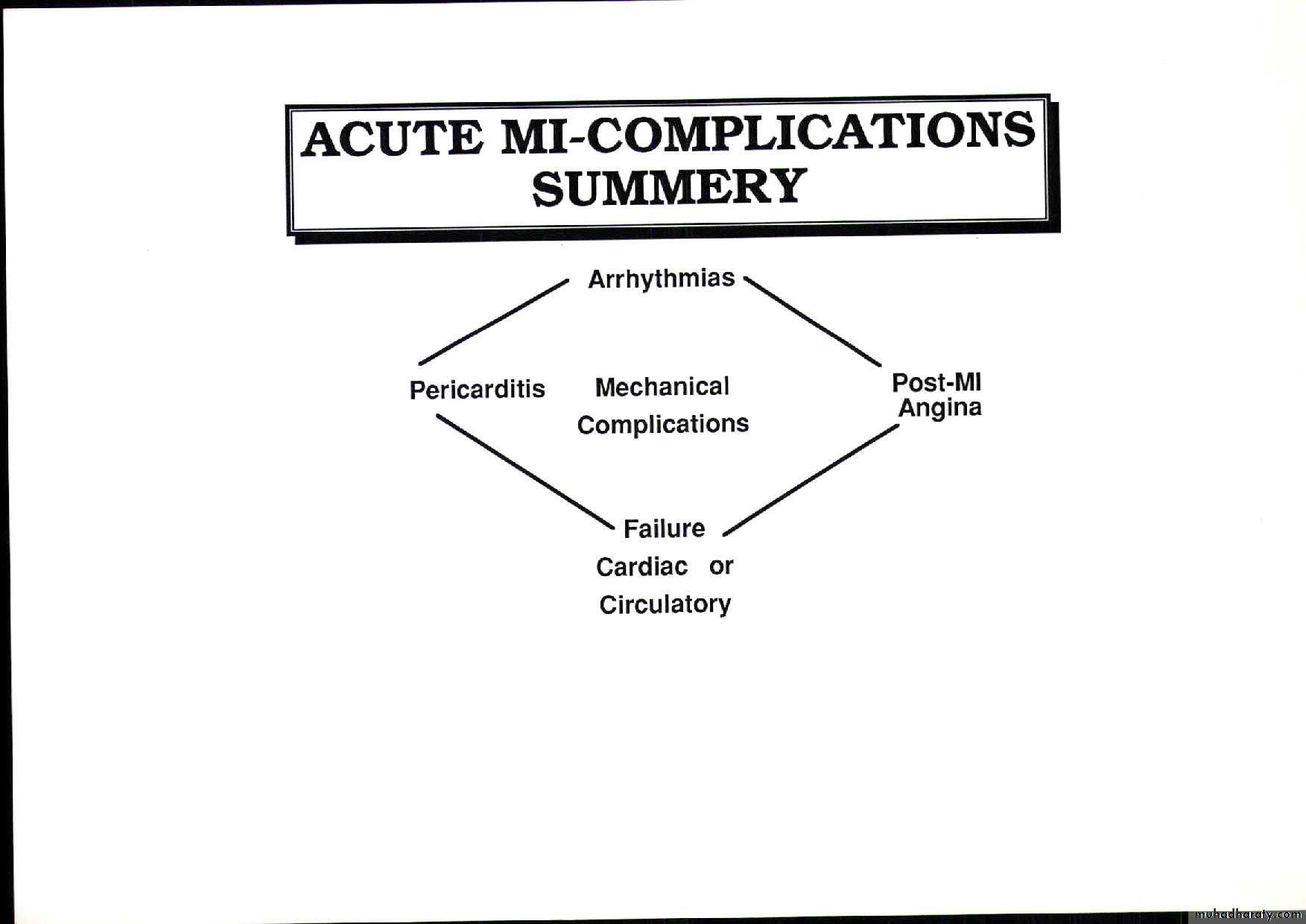
Complications Of ACSArrhthymias
CommonUsually transient
Needs no action apart from close observation
Unless they are causing
1- haemodynamic compromise ie Hypotension
2- Or carry a bad prognostic implication such late onset Ventricular Tachycardia (VT)
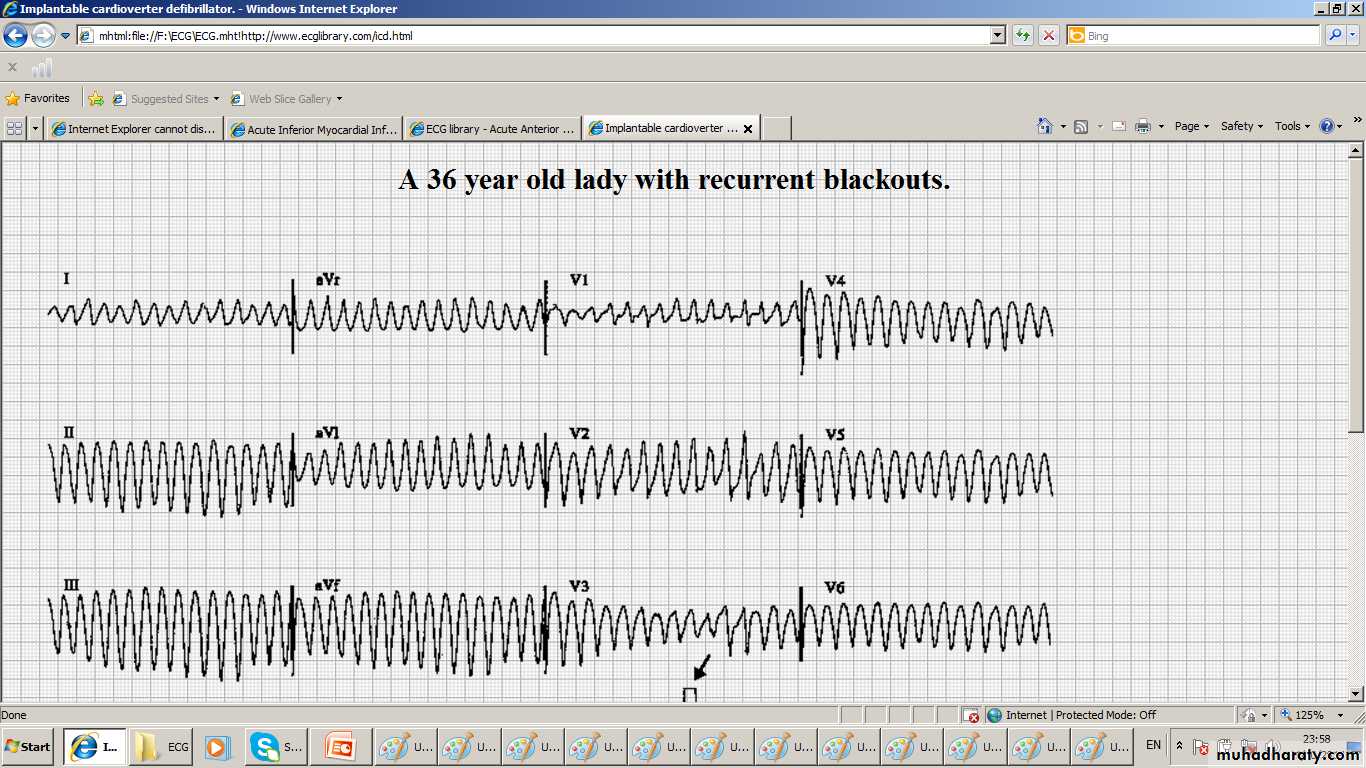
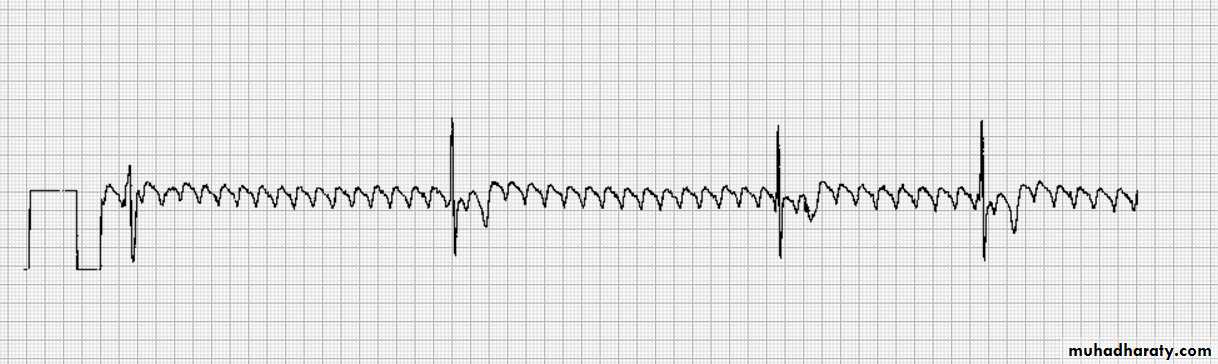
Arrhythmias in ACS VT and VF
Ventricular Fibrillation (VF)Can occurs spontaneously
or complicates Ventricular Tachycardia ( VT)
The major mode of death before hospitalization
Early VF has no bad prognosis
Treatment ;- Defibrillate promptly
Ventriculat Tachycardia VT
1- Slow VT is frequent good sign of reperfusion; called
Idioventricular rhythm. It is self limiting. No RX
2- Other VT must Defibrillate promptly
3- if not give IV Amiodarone 5 mg /kg 20 min.- 2hrs bolus followed by 15mg/kg 24hrs infusion
4- Beta blockers can prevent VT
VF ; Ventricular Fibrilation
Ventricular Tachycardia
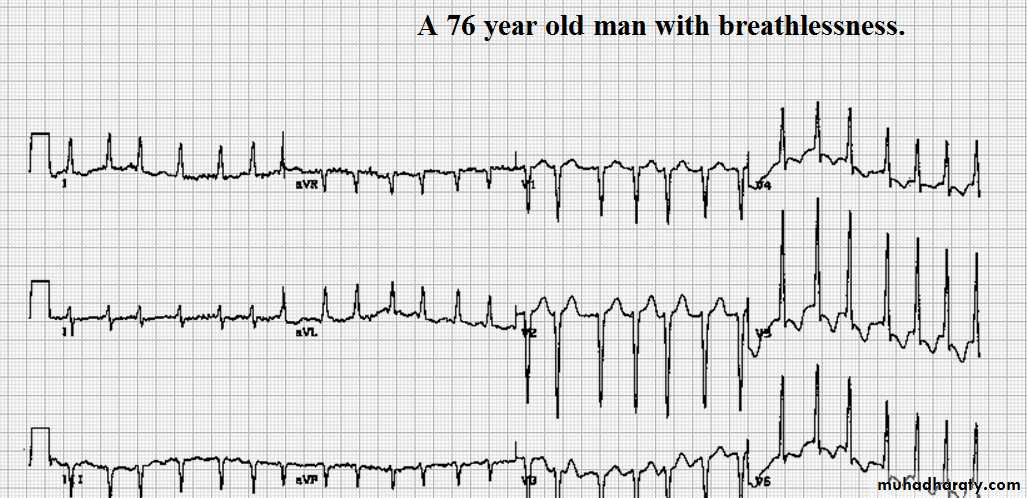
Atrial Fibrillation AF
1- common2- frequently transient
3- require no emergency treatment
4- Rapid AF with Haemodynamic compromise
require urgent synchronized DC shock
5- AF due to stretch of atrial wall is often a feature of impending or overt LV failure and therapy are ineffective unless HF is treated appropriately eg IV diuretics
6- Otherwise Digoxin 0. 25 m TID then 0.25 daily after or a betablocker
Fast AF
?? Af and complete Heat Block
ACS complications; Arrhythmia
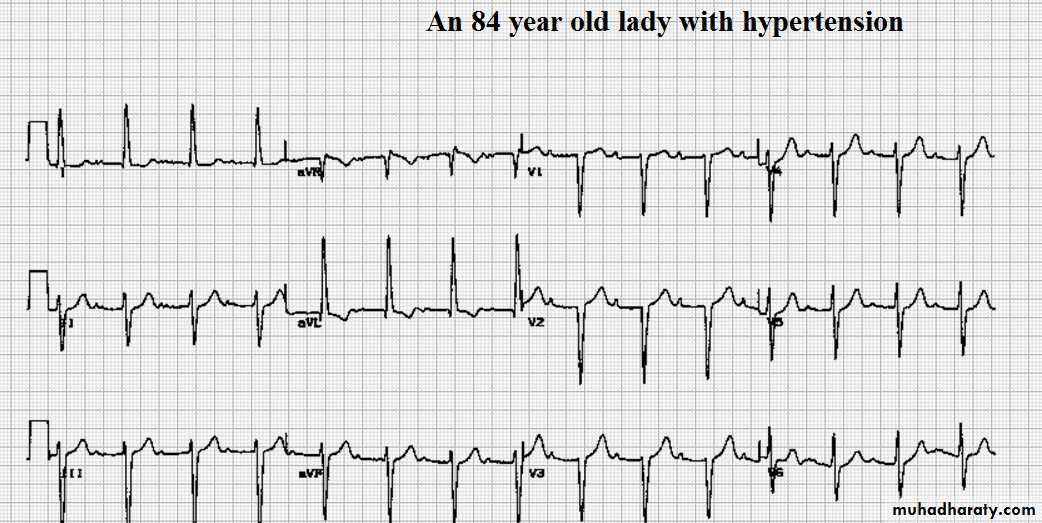
1- Sinus Bradycaridia and Atrio- ventricular block (2nd degree or complete AV Block) occur more frequently in pts with Inf. MI and both of them usually require no treatment unless ;They have led to haemodynamic deterioration then ;a- Sinus Bradycardia ;- IV atropine 0.6- 1.2 mg
b-Complete AV block require temporary Pacemaker
3- A temporary Pacemaker is certainly indicated for complete heart block complicating Anterior MI because asystole may suddenly supervene
First degree heart block
2-1 Block
Complete AVblock
Two types t
• A- Early pericarditis• 1- occur on the 2nd -3rd days after STEMI
• 2- Different pain ; little sharp, may be worse on lying down and inspiration
• 3- + Rub.
• 4- Use opiates. NoNonsteroidal Antiflamatory agents .
• Late: Dressler’ s syndrome
In few weeks.- months
Autoimmune.
Fever, pericarditis and pleurisy.
Aspirin, NSAID,…Steroid
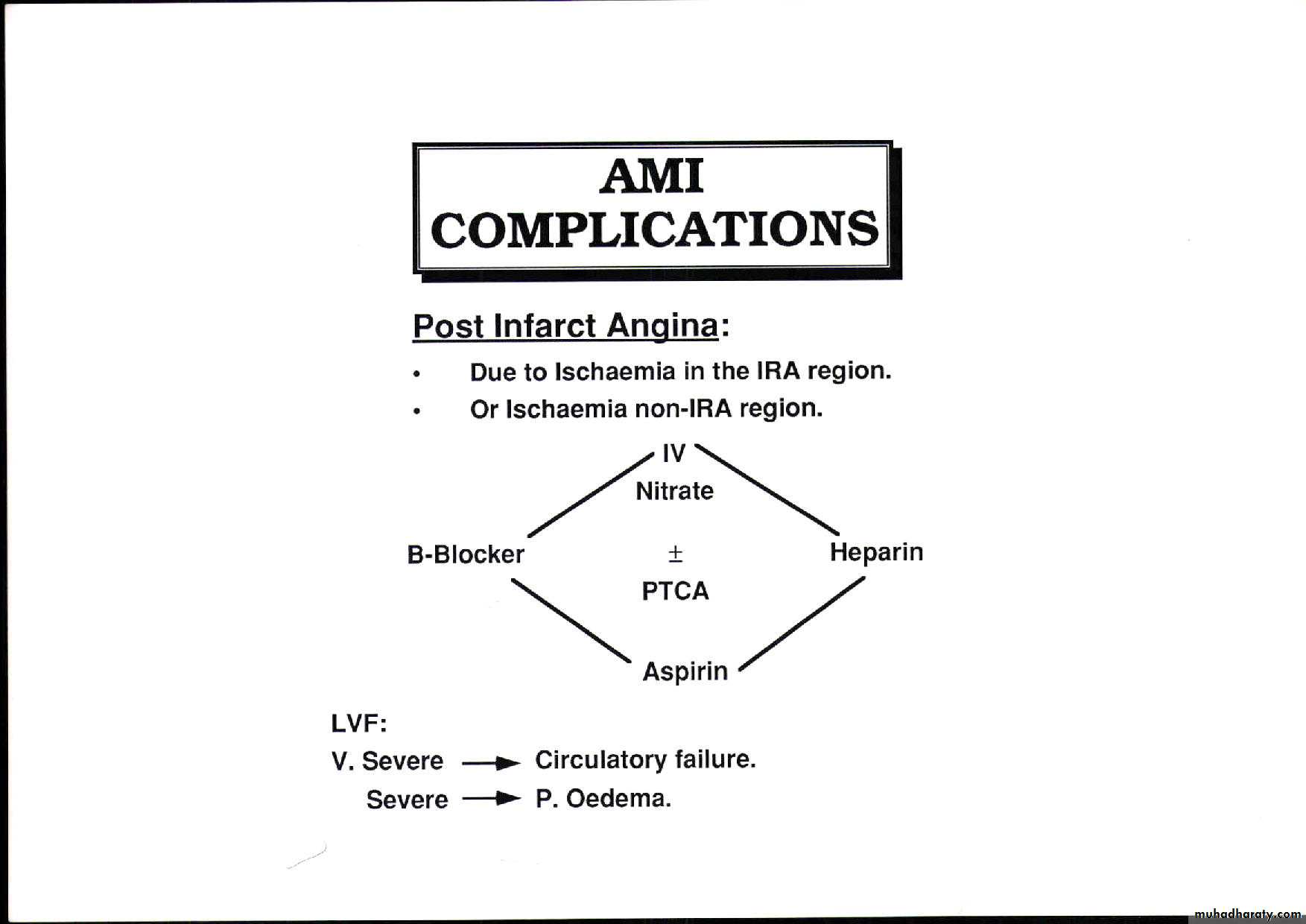
Post infarction Angina
1-Occur in 50% of pts following thrombolysis due to residual stenosis2-Pts must be on full scale RX ; nitroglycerine infusion , Betablockers . Heparin, aspirin and referred for urgent Angiography in the view of revascularization by PCI
3- Pts with dynamic ECG changes should receive IV GP 11b /11a receptors antagonist
4-Pts wih resistant pain or those who are haemodynamically unstable would needs Intraa-ortic Balloon counterpulsation
Cardiogenic Shock
Caused by
L.V dysfunction in 70 %o f cases
RV MI
Mechanical complications inclding
Cardiac Tamponade due to free wall Rupture
Acquired VSD due to IVS rupture
Acute MR due papilary musle rupture
Downward spiral of cardiogenic shock
LV systolic dysfunction causes low CO, Low BP, Low CA perfusionLV –Diastolic dysfunction causes rise of LVEDP, pul congestion , and oedema . Hypxaemia ,more ishaemi, peripheral vasoconstriction that limits cardiac output further that worsens the caes further in a spiral fashion
Low cardiac output causes hpotension , oliguria , confusion, cold extremities
While pul oedma causes :- breathlessness cyanosis,and inspiratory basl crackles
CXR may reveal pul congestion when the physical examination is normal.
Acute MI Haemodynamic subsets
Four groups of pts with cadiogenic shockG1 Normal CO and No P Oedema no rX
G2 Normal CO and P Oed Due Mod LV dysfunction Treat with Vasodilators and diuretics
G3 Low CO and No P OED due to RV MI odr Dehydration Give IV fluids use Swanz Gans to monitor therpy Considr PCI
G$ Low CO and P. OED due to Exensive MI and poor prognosiscosider IAB, Vasodilators,diuretics andinotrops and refer for PCI
LV aneurysm
Anterolateral MI
Atrial flutter