1
Medicine
ARDS + PTE
Lecture 36
د. ﺪ ن اﳉﺒﻮري
Acute Respiratory Distress Syndrome)
It is also called "Shock Lung“
Definition
: It is a syndrome in which there is pulmonary oedema without
increment in the pulmonary capillary venous pressure.
Unlike the Lt. sided heart failure, in which there is pulmonary oedema
due to increase pressure in the Lt. atrium which causes increase in the
pulmonary venous pressure → oozing of fluids to the lung tissue →
pulmonary oedema; but here, the pulmonary oedema is due to oozing
of fluids through the capillaries without increase in venous pressure
which means that the defect is related to the capillaries themselves
This syndrome is caused by variety of causes that are either directly or
indirectly cause damage to the lung tissue, directly: bullet injury, blast,
embolus, infections…etc., indirectly: haemolytic anaemia, fractures
(e.g. in the lower limb.)…etc.
· There are many processes that precipitate ARDS:
1) Pulmonary infection: whether viral, for e.g. *SARS because
one of it is complication is ARDS, *Influenza virus which
causes a wide spread lung infection or mycoplasma infections
or bacterial infection like Tuberculosis
2) Injuries: either directly by bullet or blast…etc. or
indirectly by fractures or haemolytic anaemia…etc.
3) Fractures
4) Head injury
5) Surgery – if prolonged- cause ARDS
6) Septicemia & septic shock, in fact all shock states
can cause ARDS, that is why ARDS is called "Shock
lung"
7) Acute pancreatitis

Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 2
8) Burn
9) Embolization:
either
fatty
embolus,
pulmonary
thrombo-embolus, air embolus, & amniotic fluid embolus...
** usually, embolization is due to small embolus that blocks
small tributary of pulmonary artery; but the patient may
develop ARDS (unknown cause) or by large embolus →
massive pulmonary embolization → ARDS
10) Direct damage to the lung by acids (due to vomiting or
regurgitation) → ARDS
11) Drowning: water is detrimental to the lung & can initiates
ARDS
12) Hanging: either suicidal or execution, if the patient –for
example- survive after hanging himself → develop ARDS
13) Inhalation of chemicals & toxic materials: as in the wars, which
cause ARDS & serious respiratory problems to the soldiers, or
it can happen to the workers (who works in water refinery
system) where chlorine is used for water cleaning, but chlorine
is very irritant to the lung & cause damage to the lung tissue →
ARDS also happen in housewives who use detergent in large
conc.
14) In cardio pulmonary bypass in cardiac surgery
15) Multiple blood transfusion
16) Gastric aspiration
17) Toxic gases that cause this syndrome, one of which is O
2.
Though O
2
is used in the treatment of this syndrome, it is an
irritant gas if given in high conc. So it is mandated not to give
high conc. for more than 24 hours, & this could happen in
mechanical ventilators, if you breath into close circuit &
getting pure O
2
(100% conc.), so if you need O
2
, you should not
use pure O
2
over 24hs because it may lead to this syndrome.
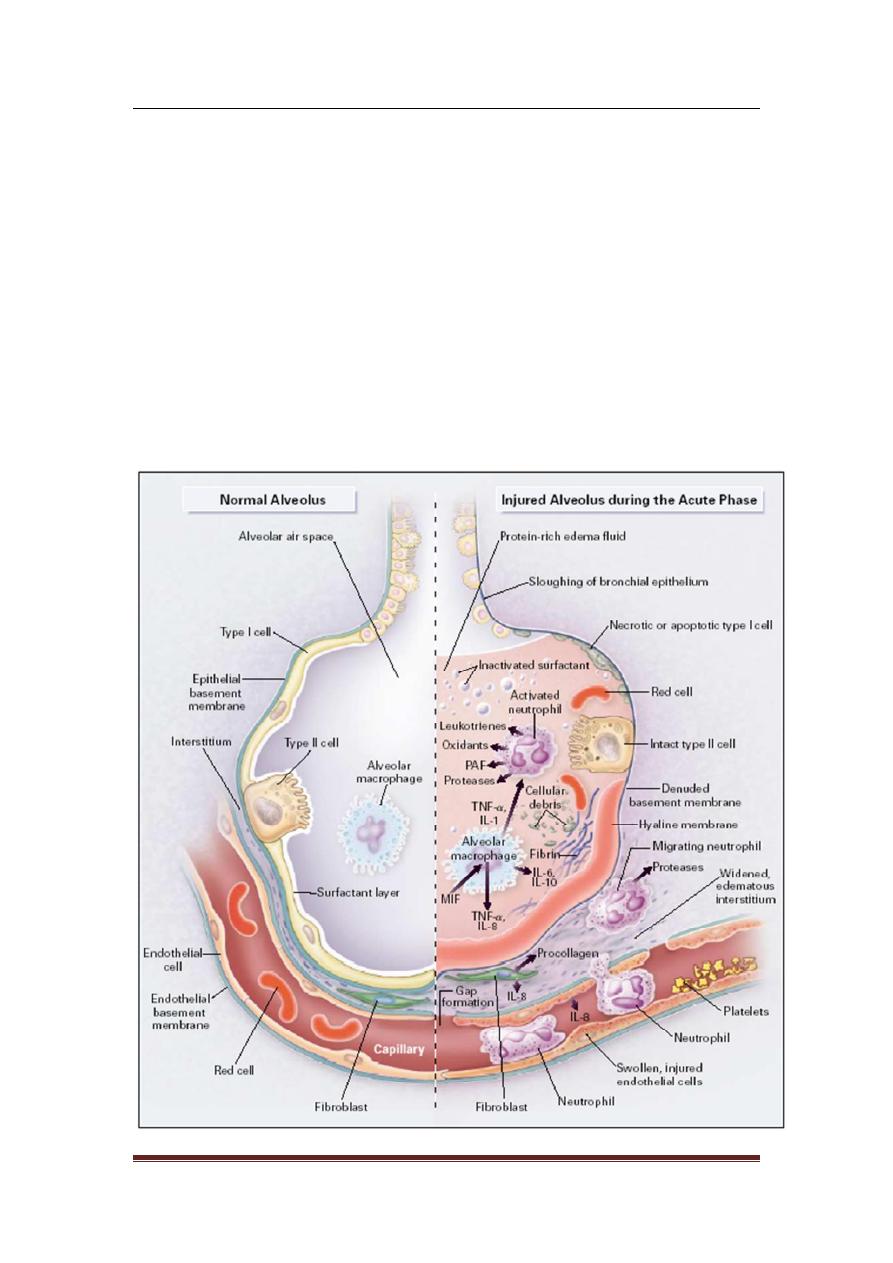
Pathophysiology
Regardless of the cause of ARDS, it will lead to destruction of the lung
tissue & this tissue contains endothelium of the blood vessels & the
epithelium in the alveoli which constitute the respiratory membrane.
Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 3
Hence, the process will lead to damage to both epithelium & the
endothelium or to any one of them, & once the capillaries get damaged
it will lead to oozing of oedema fluid to the alveolar spaces, this is
actually a pulmonary oedema, (such thing can occur in left sided heart
failure) & there will be oozing of fluid from the capillaries to the
air-spaces of the lung tissue.
Hence, damage to the epithelial & endothelial layers due to
inflammatory process of ARDS will lead to stiffness of the lung.
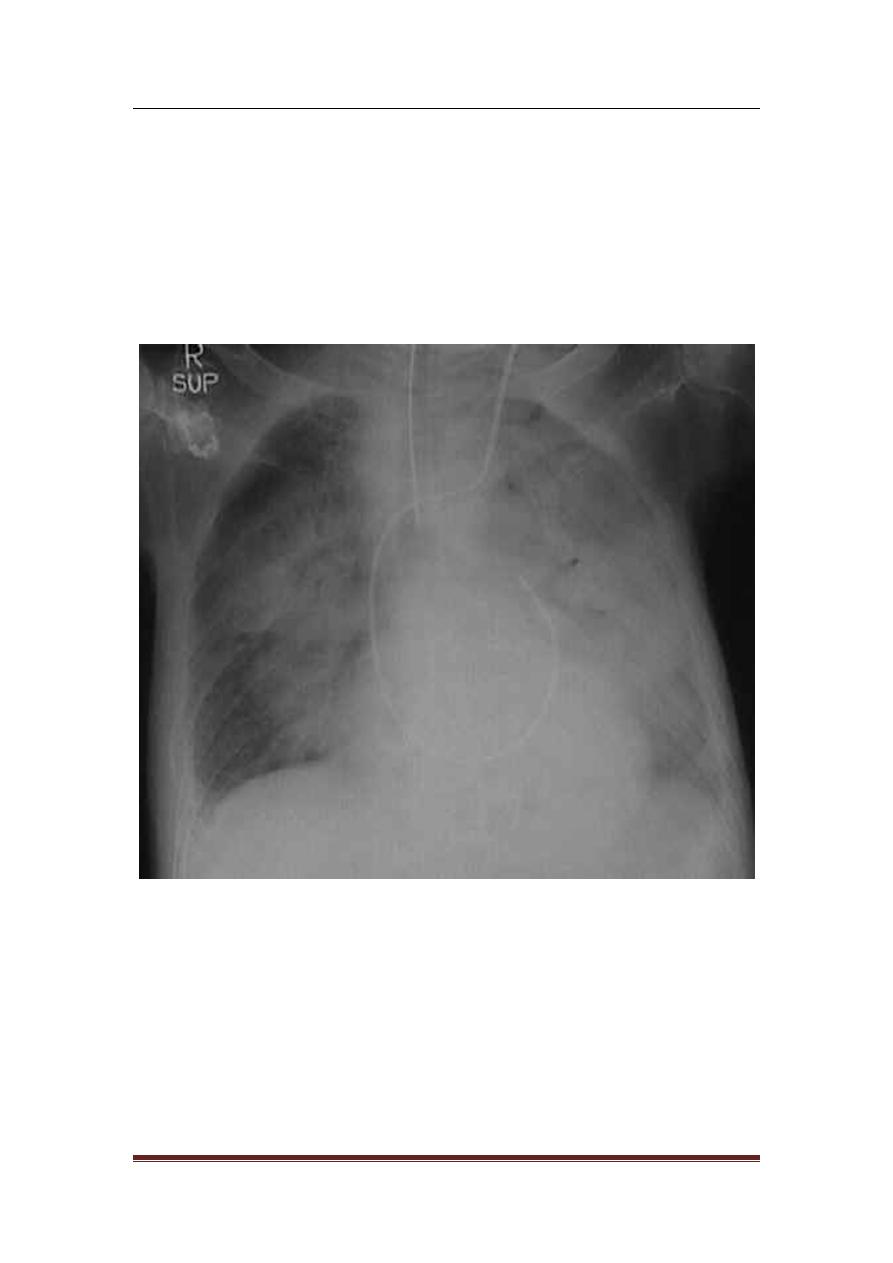
Severe ALI
B/L radiographic infiltrates
PaO2/FiO2 <200mmHg (ALI 201-300mmHg)
No e/o L Atrial P; PCWP<18
Acute Phase
:
· Pulmonary oedema with normal vascular pedicle Associated with
no cardiomegaly or upper lobe blood diversion
When pulmonary vessels can be distinguished they are often
constricted
Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 4
· Septal lines usually absent because capillary leak occurs directly
into alveolar spaces (cardiogenic pulmonary oedema)
· Progressive lung destruction and transition from alveolar to
interstitial opacities
Chronic phase
· Fibrosis
· Focal emphysema
Activation of inflammatory mediators and cellular components resulting
in damage to capillary endothelial and alveolar epithelial cells
Increased permeability of alveolar capillary membrane
Influx of protein rich edema fluid and inflammatory cells into air spaces
Dysfunction of surfactant
Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 5
Clinical Features
Any patient having severe medical or surgical problem & he developed
severe RF. Within 1 or 2 days, you should think about ARDS. Again the
clinical features of the cause
Complications
· Bacterial super infection, because there is very good medium for
infection by many M.O.
· Multiple organ failure, because there will be septicemia which can
leads to liver, kidney, heart, or brain failure this is why mortality
rate is high even in best centers
· Mortality rate in best centers is about 50%, here in our country
the mortality rate is about 90%!! Because of lack of sophisticated
equipment, the average mortality rate is about 70%.
· If the patient survive, he will undergo "pulmonary Fibrosis"
Summary of finding
1) Progressive SOB (1-2 days) following any medical or surgical
problem.
2) Central cyanosis (resistant to treatment).
3) Hypoxia & hypocapnia.
4) Wide-spread shadowing (bilateral) on chest X-ray.
5) If there is pulmonary edema, we check the pulmonary venous
pressure by using a catheter & it will be normal (i.e. there is normal
pulmonary wedge pressure, yet there is pulmonary edema).
6) Fibrosis.
7) Fine crepitation, due to pulmonary edema
Treatment
The patient should be cared in an "Intensive Care Unit" ICU, with
facility for mechanical ventilator & Rx is directed toward:
A: cause (medical or surgical)
B: General measures
· General measures that include the following
1- O2
therapy: it is general Rx or therapy for all causes; but not
pure O
2
because it is irritant to the lung tissue

Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 6
2- Mechanical ventilation: in ARDS, there is damage to type-2
pneumatocyte → decrease amount of surfactant, so you need
always a +ve pressure to keep the lung inflated & push the
fluids away from the airspaces
B: General measures that include the following
1- O2
therapy: it is general Rx or therapy for all causes; but not
pure O
2
because it is irritant to the lung tissue
2- Ventilation: in ARDS, there is damage to type -2- pneumatocyte
→
decrease amount of surfactant, so you need always a +ve
pressure to keep the lung inflated & push the fluids away.
There are 2 types of assisted ventilation to keep this +ve pressure:
1) IPPV “intermittent positive pressure ventilation”
2) PEEP “positive end expiratory pressure”
Other general measures that include
1) Dealing with infection.
2) IV nutrition may be needed in ICU
3) Cleanliness
4) Prevent bed sore
5) Electrolyte balance must be carefully controlled.
6) Use of Steroids
End of ARDS
Sabeeh & CHW

Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 7
Pulmonary Thrombo-Embolism
It is a blockage of the pulmonary artery or its tributaries by an embolus
coming from DVT in 90% of cases, while the other 10% comes from the
heart
The burden of PTE
PM finding:
5% of hospital deaths are due to PTE
While 40-50% who die in hospital were found to have DVT.
This indicates that PTE is a common problem in hospital practice
DVT
Clinical Features
Unilateral pain in the thigh & calf muscles
O / E:
They are swollen, tender, hot & pitting edema.
DVT + PTE = ????????????
ﯾرﺟﻰ ﻗراءة اﻟﻣﻼﺣظﺔ ﻓﻲ
ﻧﮭﺎﯾﺔ اﻟﻣﺣﺎﺿرة
P.T.E. (pulmonary Thrombo-Embolism)
** Diagnosis (DX): the Dx of PTE is by clinical suspicion & you should
diagnose it early, because it is a fatal condition..
≥ It occurs mainly in hospitalized patient because of prolonged bed
rest especially after surgery because of increased risk of DVT that is
usually complicated by PTE.
So, you must know the Dx of DVT: Pain in the thigh & calf muscles 7
they are Swollen, Tender & pitting oedema (Unilateral).
Or from the history of the patient if he had past PTE, so he more liable
for another attack of PTE
** The Dx of PTE depends on the clinical feature of it is types that
mentioned previously. There are many diseases affecting respiratory
system & cardiovascular system that mimic PTE:
1) Massive PTE mimic Acute MI, dissecting aortic aneurysm, &
massive pulmonary collapse
2) Pulmonary infarction (occlusion of 1 branch of pulmonary artery)
mimic T.B., pulmonary abscess, acute asthma, bronchiectasis,
bronchogenic CA.

Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 8
3) Recurrent small pulmonary emboli → primary pulmonary
hypertension → Rt. Sided heart failure mimic secondary
pulmonary hypertension (mitral stenosis or other causes of Lt.
sided heart failure) & other causes that leads to Acute respiratory
failure..
** Investigation:
A. Radiological: 90% of PTE is caused by DVT, so we do venogram to
calf veins, thigh veins or pelvic veins, so we can detect filling
defect in the veins.
B. Ultra-sound (Doppler): we can use it for the same area of above.
C. Chest X-ray: it is helpful in most cases, in which the chest x-ray is
abnormal. The effect of recurrent small emboli or pulmonary
infarction of small/medium emboli may be not seen; but later on
you may see lung collapse (at the affected site), linear opacities or
any type of opacity, wedge-shape opacity suggest collapse of one
of segments.
- Also, you can see effusion because pulmonary infarction will
affect the overlying pleura → effusion (usually haemorrhagic)
- Sometimes you see Elevated hemidiaphram only suggested
Hidden collapse segment.
- Increase in hilar shadow because of pulmonary hypertension
- The lung is oligemic at the area of infarction if the PTE is
massive → the whole lung is oligemic.
D. C.T. scan & Angiogram : they are very much confirmative of this
disease by pulmonary angiogram you can detect the pulmonary
artery & it is branches
E. Radioactive scanning procedures : Technitium scan can show PTE
but bronchogenic CA, pneumonia, & pulmonary oedema mimic
the PTE, so it will be confused … So, it is better to do ventilation
scan & ventilation-perfusion scan using radioactive xenon, then
matching them → not matched.
F. E.C.G. changes : would be specific for the Rt.side of the heart,
sinus tachycardia & evidence of Rt. Sided ventricular hypertrophy
& classical pattern ( S
1
, Q
3
,T
3 )
· Deep S in lead 1
Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 9
· T-wave is inverted in lead 3
· Q – wave in lead 3
· Rt. Bundle branch may appears
· If the embolus is small, the E.C.G. may be normal or there is
very small changes.
G. Arterial blood gases: the pattern is of type -1- respiratory failure
(hypoxia, normocapnia, or hypocapnia) that indicate
ventilation-perfusion problem..
** Treatment (Rx):
Preventive measures:
1) Prevention of prolonged bed rest, use stockings to prevent DVT
(usually the patient is in faulty posture due to trauma or fatigue.
So change the position frequently by the patient himself or the
companion).
2) Also treat other risk factors for DVT like dehydration & treat
congested heart failure.
3) Prophylaxis is offered to any patient have problem & needs
operation, if he has past PTE or DVT in the next surgery he will
have a high incidence of PTE, therefore we we must give the
patient prophylactic measures like : Anti-coagulants (leads to
increase bleeding time, so in this case the surgeon must block all
the bleeding vessels that are usually left to block themselves)
We give – Heparin – 5000 IU/12 hr (very low dose) helpful to
prevent DVT or we give – Dextran – I.V. during the operation
4) If the patient has DVT & recurrent pulmonary embolism &
resistant to Rx , so mechanical measures used as Inferior Vena
Cava PLICATION or other devices to allow blood to go on; but
prevent emboli to come to the heart.
** Treatment (Rx) of established cases:
IF the patient has massive PTE use thrombolytic agents which lysis
thrombus (for e.g.: Streptokinase, starting with loading dose 250,000 –
500,000 IU, then every hour 150,000 IU for 2 days with no complication
(like : brain haemorrhage or G.I.T. bleeding – contraindication-)
· Tissue Plasminogen Activator (TPA) by catheter is injected into
the thrombus, directly leading to it is lysis.
Lecture 36
Medicine
Dr. Adnan
ARDS + PTE
Page 10
· Anti-coagulant given to the patient by special device that
produce stable conc. of blood like that for Heparin 1000 IU/ hr,
so in 24 hr. there is 24000 IU. This will lead to smooth circulation
& we can follow up this by PTT (Partial Thromboplastin Time),
2-3 times than normal control.
· The Warfarin orally gradually taken before stopping heparin,
because it is effect appears after 3 days the PTT must be 2-3
times than normal control.
· The Rx must be from 6 weeks to 6 months depending on the
patient
’
s status, age (young 6 weeks, old or ill 6 months), & the
degree of embolization.
· Also supportive measures like good nutrition
ﻣﻼﺣﻈﺔ
ﲞﺼﻮص ﳏﺎﴐة:
PTE
... دﻛﺘﻮر ﺪ ن ﻋﺮض ﺑﻮرﺑﻮﯾ ﺖ ﻣﺎ
ﰷﻣﻞ و ﳊﺪ ﻋﺒﺎرة
DVT + PTE =
إ ﻜﻄﻢ اﳊﺠﻲ و ﻓ ﺢ دو ﯿﻮﻣ ﺖ وورد ﺑﯿﻪ ﳬ اﶈﺎﴐة ﺲ ﰷل ﻫﺎي اﶈﺎﴐة ﻣﻮ ﻣ ﻘ ﺔ و ﳱﺎ ا ﻼط و
ﺪ )اﻟﯿﻮم( ﻋﺴﺎس رح ﯾﻨﻄﻲ اﶈﺎﴐة ﺑﻮرﺑﻮﯾ ﺖ ﰷﻣ و ﻣ ﻘ ﺔ و ﺎﻻ ﻠﺐ ﲆ ﻣﻮﻗﻊ اﻟﳫﯿﺔ
إذا ﺣﺼﻠﺖ اﶈﺎﴐة رح ا ﺰﻟﻬﺎ ﲆ ﺮوب اﳌﺮ
و ﻫﺎي اﻟﺼﻔ ﺎت ذﺑﻮﻫﺎ و اذا ﻣﺎ ﺣﺼﻠﳤﺎ او ﻣﺎ ﺰﻟﺖ ﲆ
ﻣﻮﻗﻊ اﻟﳫﯿﺔ
...
ﻫﺎي وراق ﲤﴚ ﺷﻐﻞ ﻠﻤﻮد ﻣ ﺎن
ﻫﺎي آﺧﺮ ﳏﺎﴐة ﲠﺎﻟﻔﺼﻞ و ﰻ ﳏﺎﴐات دﻛﺘﻮر ﺪ ن دا ﳌﺪ
ًو ﺷﻜﺮا
The end of this lecture
Sabeeh & CHW
