1
Medicine
د. رﺑﺎح
Lec. 66
inflammatory bowel diseases
Ulcerative colitis and Crohn's disease
An immune-mediated chronic inflammatory bowel diseases with relapsing
and remitting course
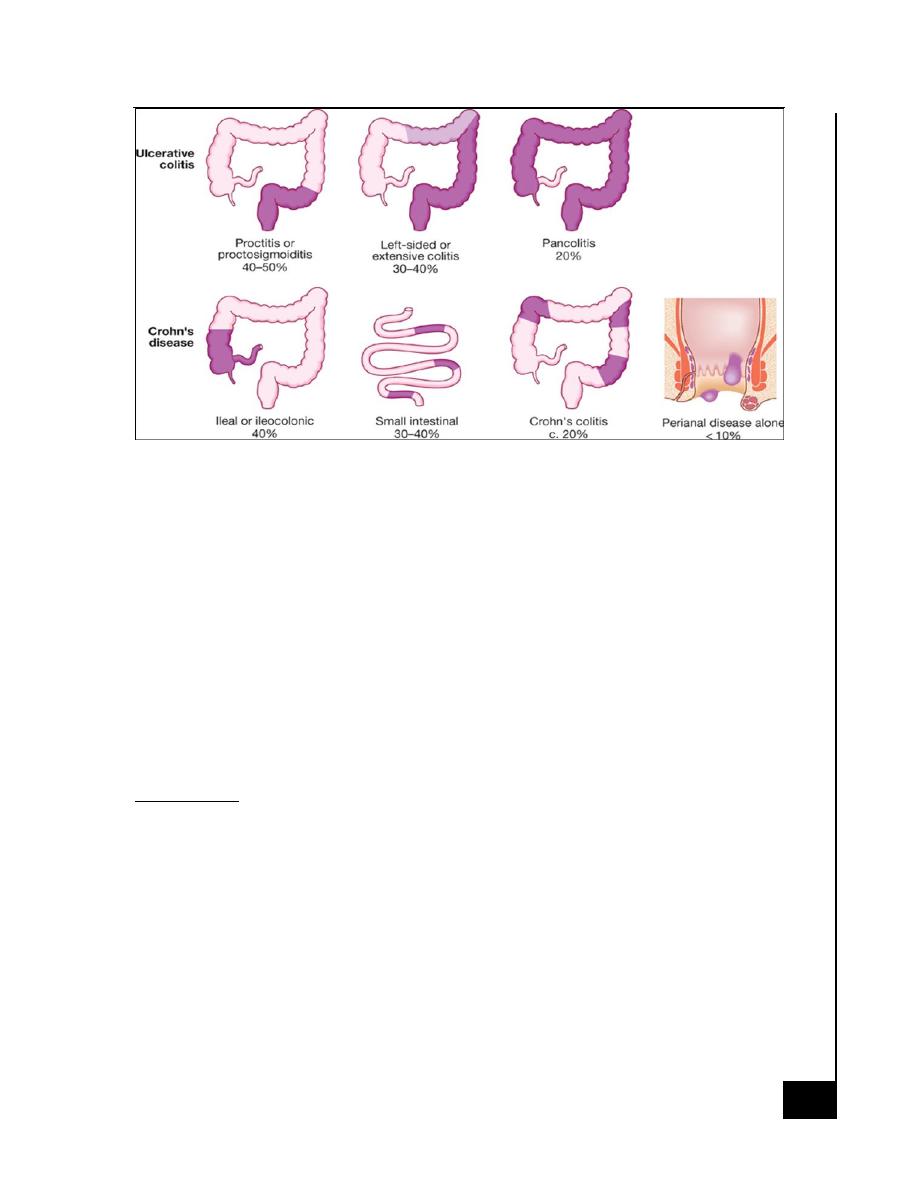
· Ulcerative colitis only involves the colon
· Crohn's disease can involve any part of the gastrointestinal tract from
mouth to anus.
Epidemiology
· In developing world
o Crohn's disease appears to be rare
o Ulcerative colitis, more common.
· In the West
o Ulcerative colitis prevalence of 100-200 per 100 000
o Crohn's disease prevalence of 50-100 per 100 000.
· Young adults (between 15 and 30 years), second smaller incidence
peak in the seventh decade (between 60 and 80 years)
· The male to female ratio for UC is 1:1 and for CD is 1.1–1.8:1.
· UC and CD have two- to fourfold increased frequency in Jewish.
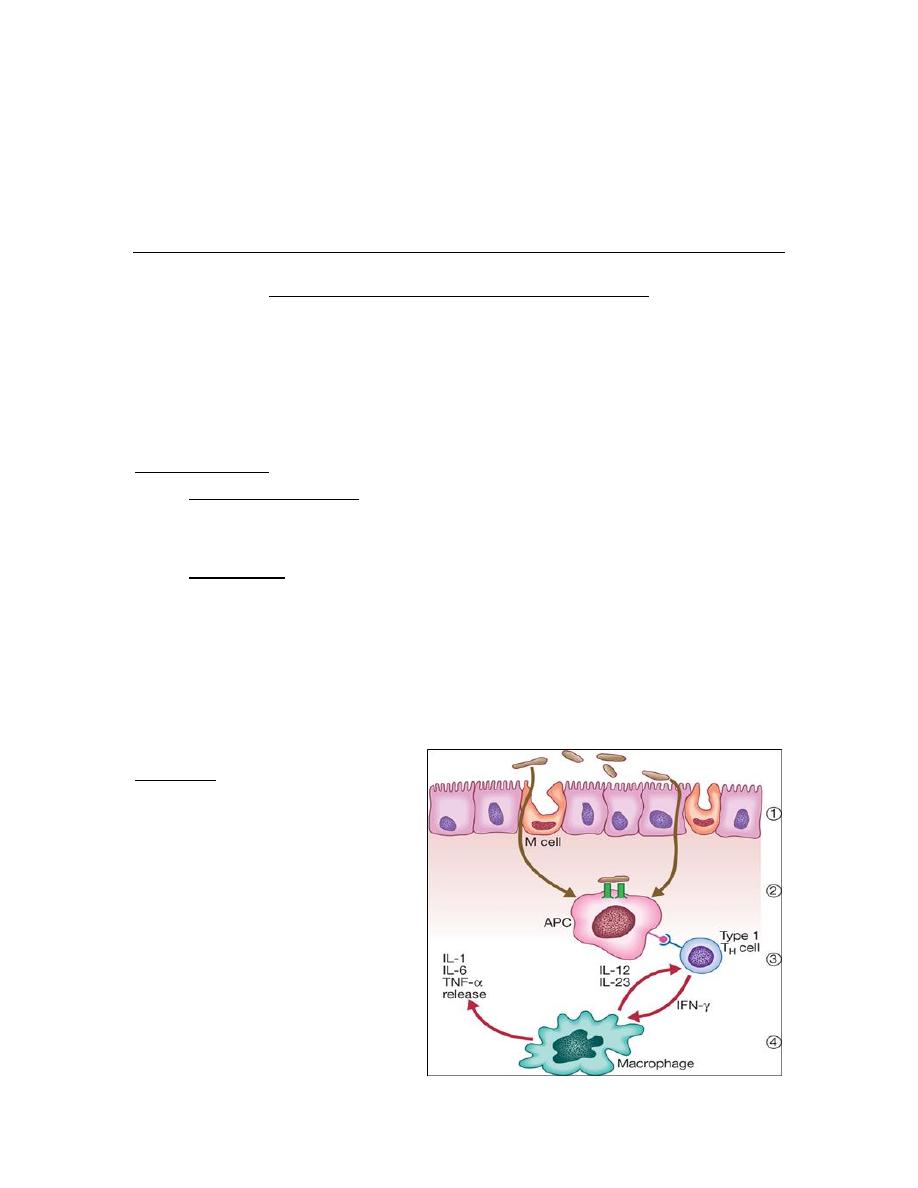
Etiology
o Abnormal host response
to an environmental
trigger in genetically
susceptible individuals
o This causes inflammation
of the intestine and
release of inflammatory
mediators, such as TNF,
IL-12 and IL-23, which
cause tissue damage.
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
2
Factors associated with the development of IBD
Genetic
o More common in Ashkenazi Jews
o 10% have a first-degree relative or at least one close relative with IBD
o High concordance between identical twins
o Crohn's disease is associated with the NOD2, ATG16L1 and IRGM
genes
o Ulcerative colitis is associated with the ECM-1 gene
o Associated with autoimmune thyroiditis and SLE
o HLA-DR103 associated with severe ulcerative colitis
o Ulcerative colitis and Crohn's patients with HLA-B27 commonly
develop ankylosing spondylitis
Environmental
o Ulcerative colitis is more common in non-smokers
o Most Crohn's patients are smokers
o Associated with low-residue, high refined sugar diet
o Appendicectomy protects against ulcerative colitis
Pathology
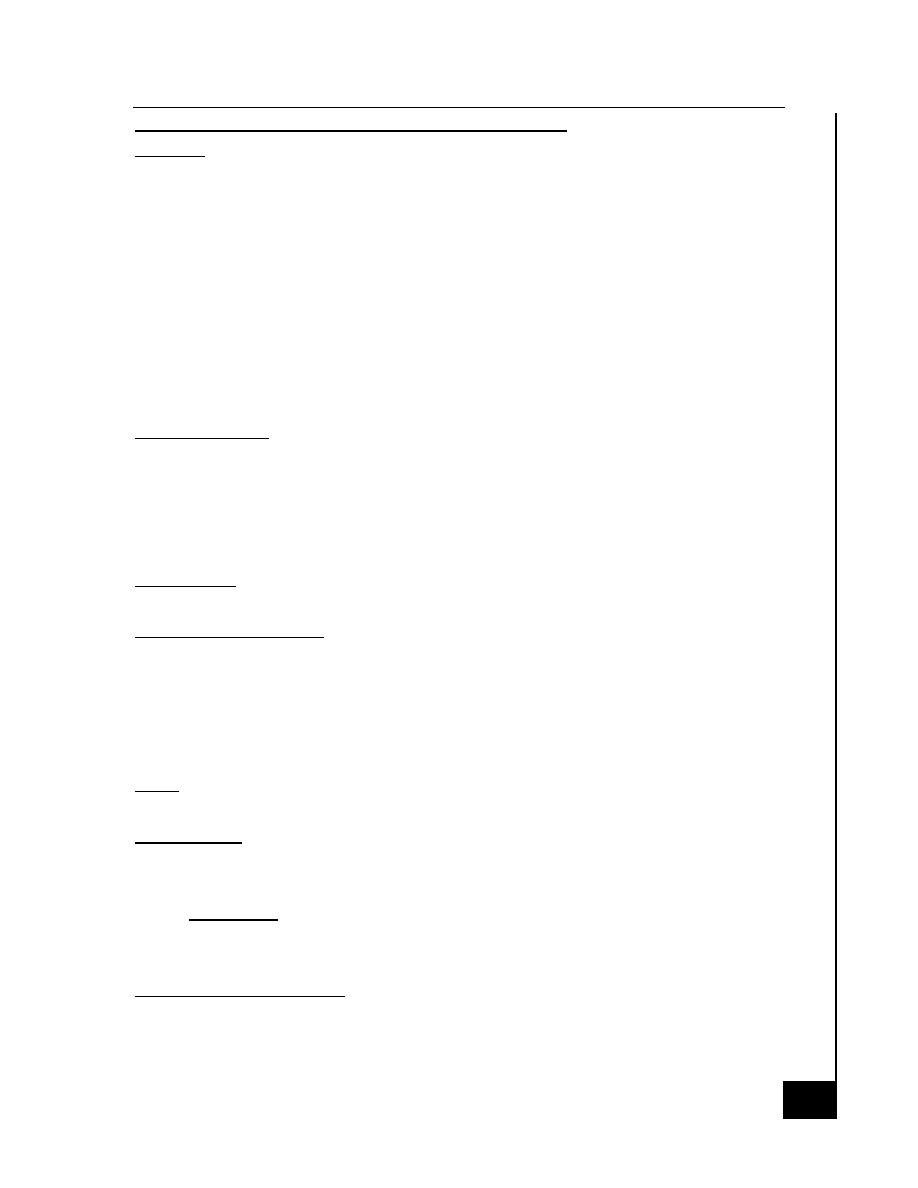
Ulcerative Colitis
Macroscopic Features
o Extends proximally to involve all or part of the colon.
o 40–50% of patients involve the rectum, rectosigmoid
o 30–40% beyond the sigmoid
o 20% have a total colitis
o Inflammation is diffused
Mild:
o The mucosa is erythematous and fine granular surface
More severe
o The mucosa is hemorrhagic, edematous, and ulcerated (superficial
diffused)
o Fulminant disease can develop a toxic megacolon where the bowel
wall thins and the mucosa is severely ulcerated; this may lead to
perforation.
In long-standing disease
o Inflammatory polyps (pseudopolyps) may be present as a result of
epithelial regeneration.
o Many years of disease it appears atrophic and featureless and the
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
3
entire colon becomes narrowed and shortened
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
4
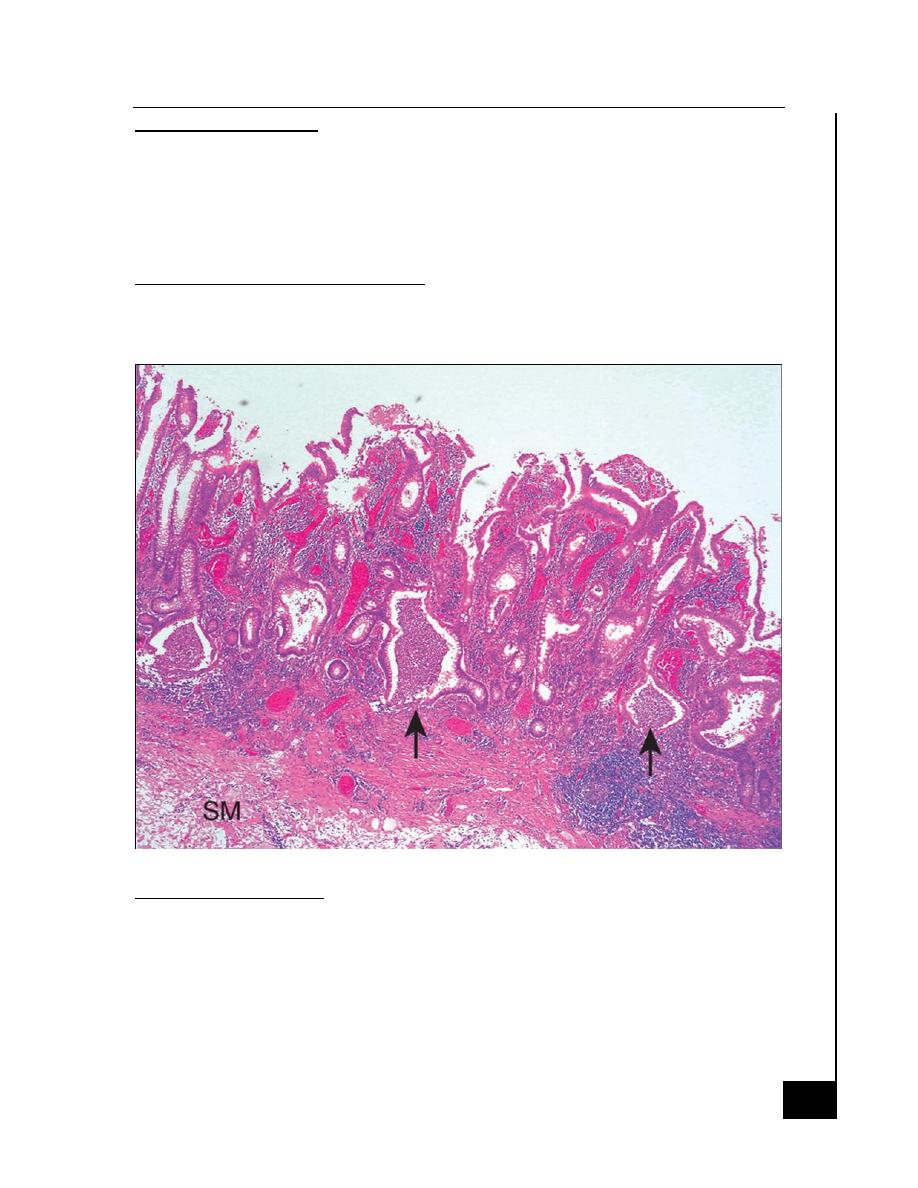
Microscopic Features
o Mucosal vascular congestion, edema and focal hemorrhage
o Inflammatory cell infiltrate of neutrophils, lymphocytes, plasma cells,
and macrophages may be present.
o The neutrophils invade the epithelium, usually in the crypts, giving
rise to cryptitis and, to crypt abscesses
Histological features of chronicity
o First, the crypt architecture of the colon is distorted
o Second, some patients have basal plasma cells and multiple basal
lymphoid aggregates
Crohn's Disease:
Macroscopic Features
o 30–40% of patients have small-bowel alone
o 40–55% have disease involving both the small and large intestines
o 15–25% have colitis alone.
o 30 % have anal involvement
o The rectum is often spared in CD.
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
5
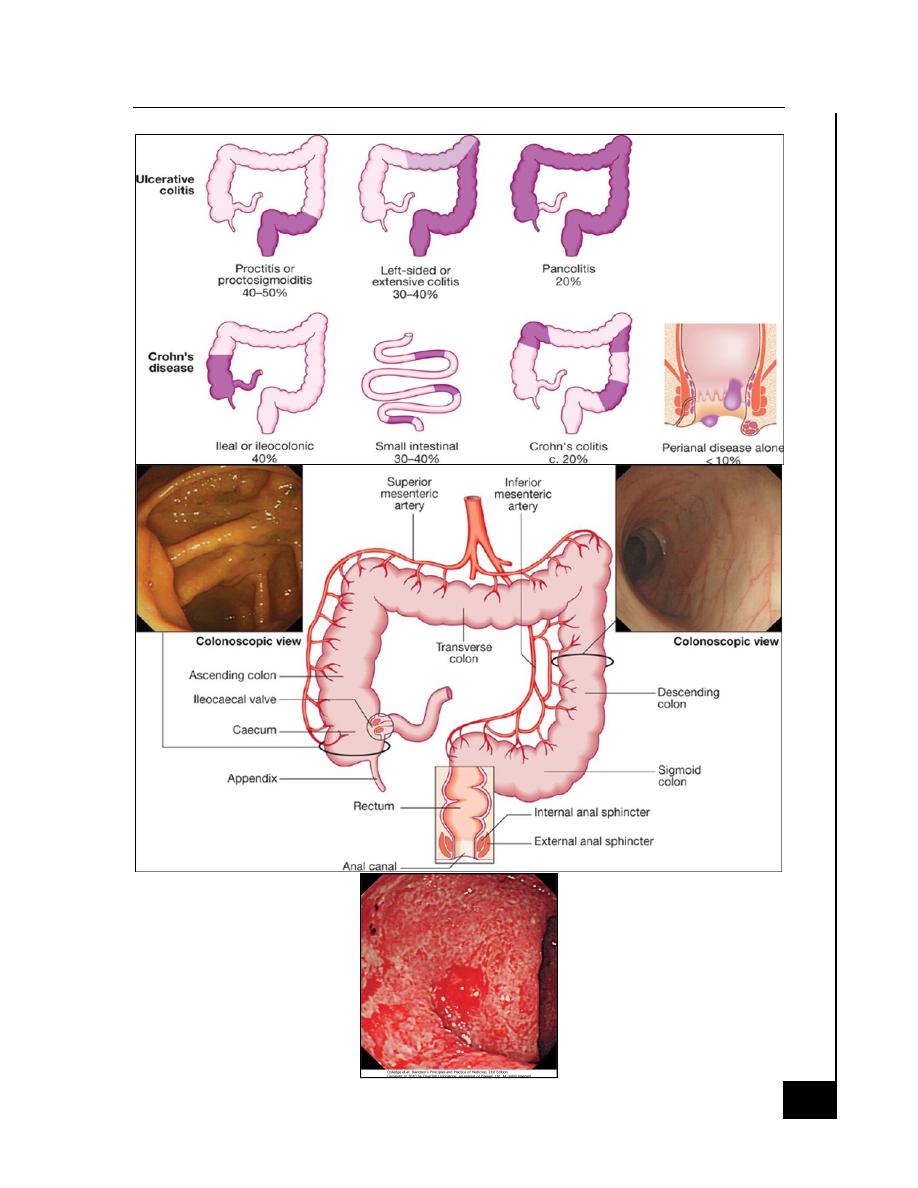
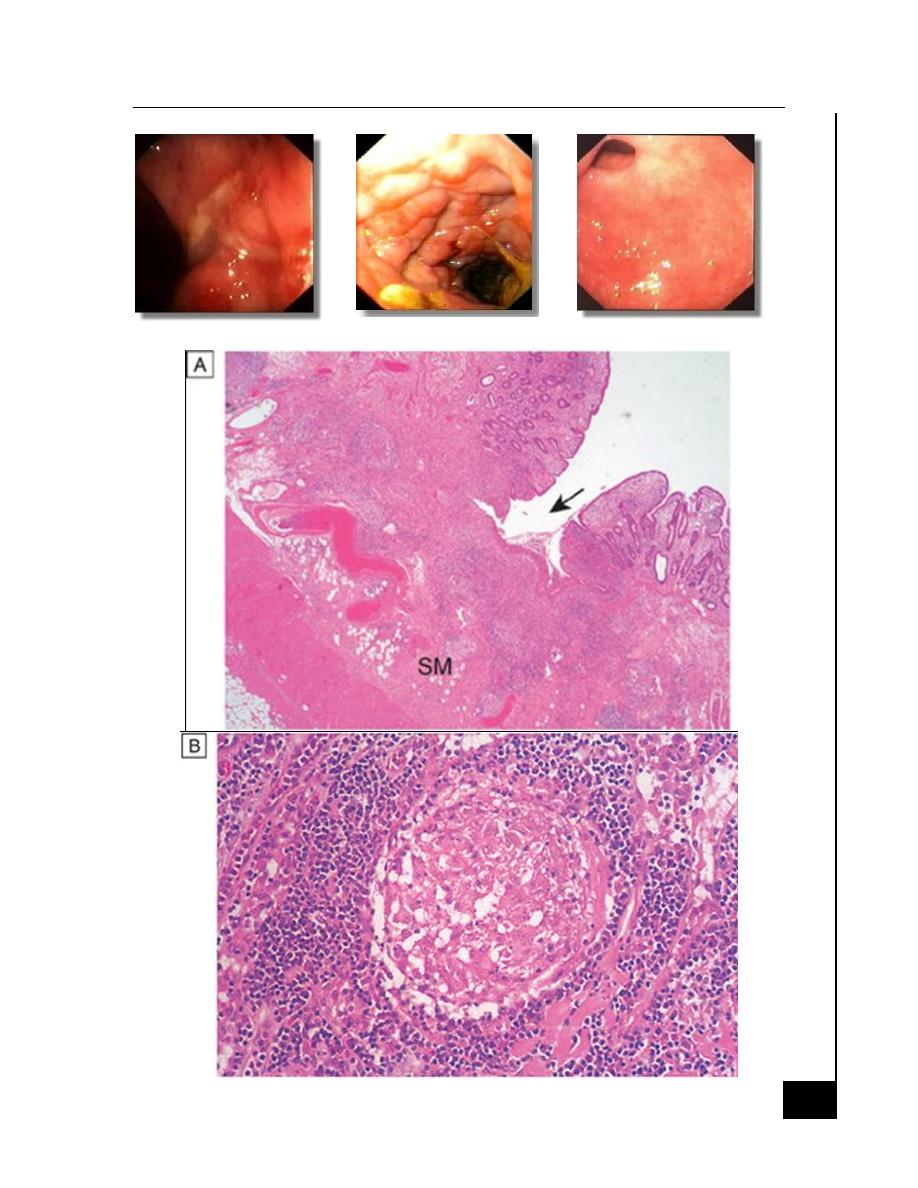
Segmental inflammation (skip areas of inflammation)
Aphthous ulcerations
Stellate ulcerations fuse longitudinally and transversely to demarcate
islands of mucosa that frequently are histologically normal.
"Cobblestone" appearance
Ulcers may penetrate bowel wall to initiate abscesses or fistulas
o The bowel
o Bladder
o Uterus
o Vagina
o Skin of the perineum
Bowel narrowed and fibrotic, with chronic, recurrent bowel
obstructions
Mesenteric lymph nodes are enlarged and the mesentery is
thickened.
Microscopic
· Transmural inflammation
· Fissures penetrate deeply into the bowel wall
· Bowel wall thickened
· Chronic inflammatory infiltrate all layers.
· Focal crypt abscesses
· Noncaseating granulomas
· Microscopic skip areas
· Other histological features submucosal or subserosal lymphoid
aggregates.
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
6
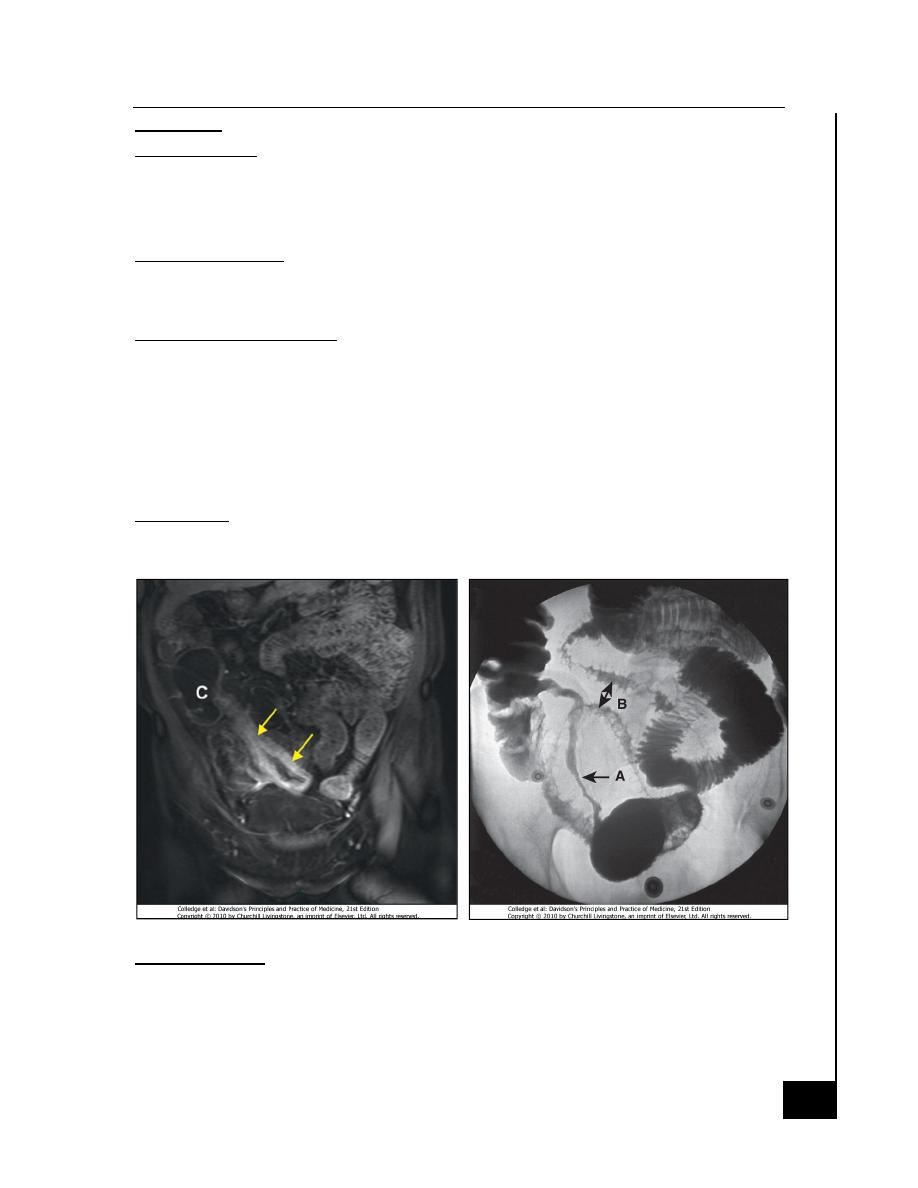
Crohn’s ulcer
Crohn’s cobblestone
Crohn’s stricture
Crohn’s disease
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
7
Clinical features
Ulcerative colitis
Bloody diarrhea relapses and remissions
· Emotional stress
· Intercurrent infection
· Gastroenteritis
· Antibiotics
· NSAID therapy may all
provoke a relapse
Proctitis
· Rectal bleeding
· Mucus discharge
· Tenesmus.
· Frequent, small-volume fluid stools
Proctosigmoiditis
· Bloody diarrhoea with mucus.
Extensive colitis
· Bloody diarrhea
· Passage of mucus.
· Severe cramping
· Abdominal pain can occur with severe attacks of the disease.
· Constitutional symptoms do not occur only in moderate to severe
disease
Severe colitis
· Bleeding
· Severe diarrhea
· Severe pain
· Fever
· Tachycardia
· Abdominal tenderness
Mild
· <4 stool/day no or small
blood amount
· No fever
· No tachycardia
· Mild anemia
· ESR<30
Moderate
· Intermediate between mild and moderate
Severe
· 6 stool /day with blood
· Fever > 37.5c
· Heart rate > 90
· Anemia < 75% of the normal
· ESR > 30
Crohn's Disease
· The major symptoms are:
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
8
o Pain is often associated with diarrhea
o Diarrhea usually watery not contain blood or mucus.
o Weight loss
o Intestinal obstruction sub-acute or even acute
o Malabsorption
Mechanism of the diarrhea
(1) Bacterial overgrowth in obstructive stasis or fistulization,
(2) Bile-acid malabsorption due to a diseased or resected terminal ileum
(3) Intestinal inflammation with decreased water absorption and
increased secretion of electrolytes
Crohn's colitis
· As ulcerative colitis
· Rectal sparing
· Stricturing can occur in the colon in 4–16% of patients
Perianal disease
· Affects about one-third of
· Large hemorrhoidal tags
· Anal strictures
· Anorectal fistulae
· Perirectal abscesses.
· Incontinence
Ileocolitis
· Recurrent right lower quadrant pain
· Diarrhea.
· Palpable mass
· Fever, leukocytosis.
· Weight loss is common
· Fistula formation
· Abscess cavity in the mesentery
Small intestinal Crohn’s
· Malabsorption and steatorrhea.
· Nutritional deficiencies.
· Vomiting from jejunal strictures or severe oral ulceration.
Differential diagnosis
· Colitis
· Infective
o Bacterial
§
Salmonella
§
Shigella
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
9
§
Campylobacter jejuni
§
E. coli
§
Gonococcal proctitis
§
Pseudomembranous colitis
§
Chlamydia proctitis
o Viral
§
Herpes simplex proctitis
§
Cytomegalovirus
o Protozoal
§
Amoebiasis
· Non-infective
o Vascular
§
Ischaemic colitis
§
Radiation proctitis
o Idiopathic
§
Collagenous colitis
§
Behçet's disease
o Drugs
§
NSAIDs
o Neoplastic
§
Colonic carcinoma
o Other
§
Diverticulitis
Small bowel Crohn's disease
· Right iliac fossa mass
Caecal carcinoma
Appendix abscess
· Infection
Tuberculosis
Yersinia
Actinomycosis
· Intestinal Lymphoma
· Mesenteric adenitis
· Pelvic inflammatory disease
Complications
Toxic megacolon
· Acute colonic dilatation due severe flare of the colitis
· More with extensive colitis
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
10
· 5% incidence
· Precipitating factors as hypokalemia, antimotility, colonoscopy
Clinical features
· Features of severe colitis with
· Diffused abdominal distension
· Diffused tenderness
· Decease bowel sound
· Lab sings of systemic
inflammation
Treatment
· Conservative
Indication for surgery
· No response within 72 hr
· Sings of peritonitis or perforation
Hemorrhage
· Hemorrhage major artery is rare
· Can occur in both conditions.
Fistulas
Enteroenteric
diarrhoea
Malabsorption.
Enterovesical
recurrent UTI
pneumaturia.
Enterovaginal
a feculent vaginal discharge.
Bowel fistulation
perianal ischiorectal
Abscesses
Fissures
Fistulas.
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
11
Cancer
· Active colitis of more than 10 years'.
· The cumulative risk 10%
· Lower for Crohn's colitis.
· Tumors develop in areas of dysplasia
· Surveillance programmes beginning 8-10 years after diagnosis by
colonoscopy 1-2-yearly.
· Mild to moderate dysplastic changes are the frequency of screening
is increased
· High-grade dysplasia panproctocolectomy
Strictures
In Crohn's disease
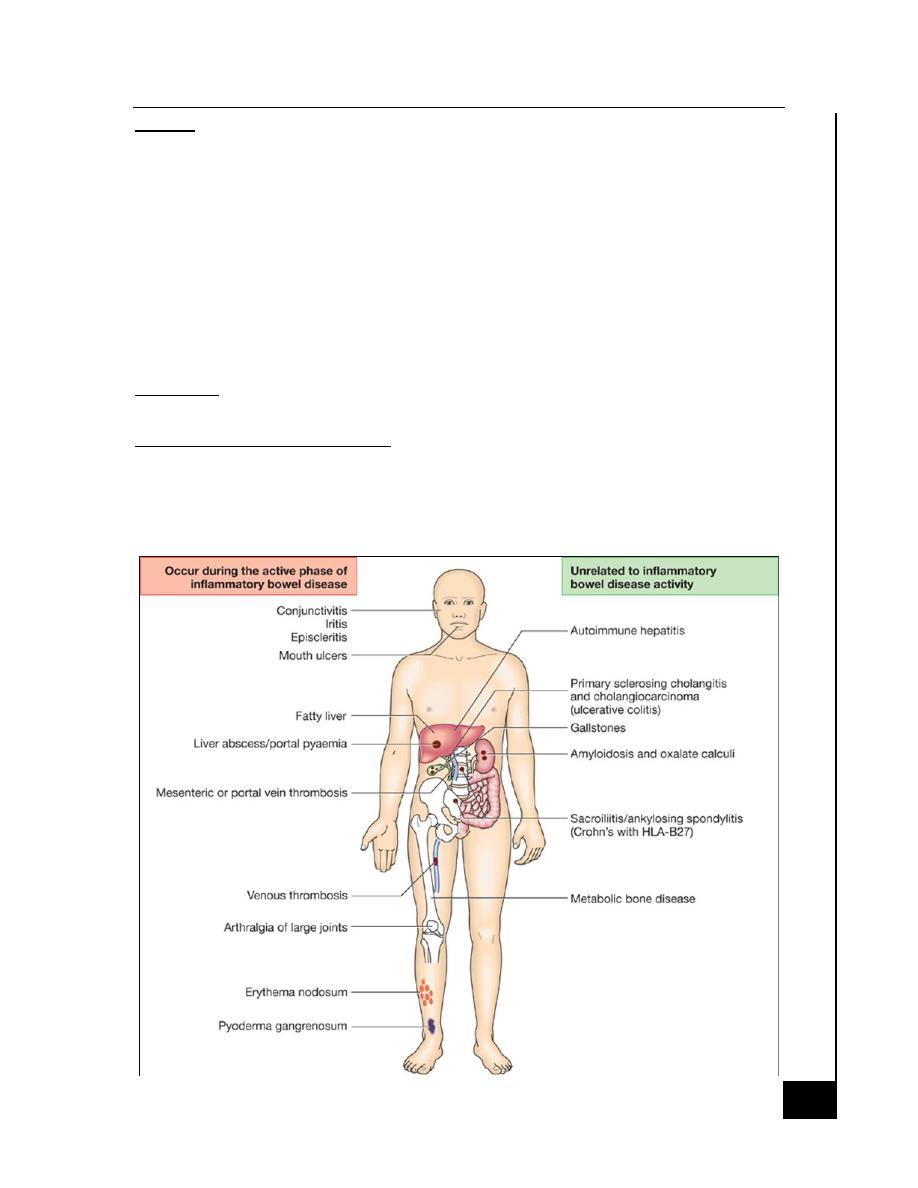
Extra intestinal complications
· Common in IBD
· May dominate the clinical picture.
· Some of these occur during relapse of intestinal disease
· Others unrelated to intestinal disease activity
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
12
Investigations
· Confirm the diagnosis
· Define disease distribution
· Define activity
· Identify complications.
· Full blood count may show anaemia
· Serum albumin.
· The ESR and CRP
Elevated in exacerbations and in response to abscess formation
Bacteriology
· Stool microscopy
· Culture and examination
Ova
Cysts
Clostridium difficile toxin
· Blood cultures
· Serological tests p ANCA, ASCA
Endoscopy with Biopsies
· Confirm the DX
· Define disease extent
· Detect dysplasia in long-standing colitis.
In ulcerative colitis
· Loss of vascular pattern
· Granularity
· Friability
· Ulceration.
· Pseudopolyps
· Stricture formation does not occur
In Crohn's disease
· Patchy inflammation
· Discrete, deep ulcers
· Perianal disease (fissures, fistulas and skin tags)
· Rectal sparing
Capsule endoscopy
· The identification of small bowel inflammation, but should be
avoided in the presence of strictures.
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
13
Radiology
Barium enema
· Less sensitive investigation than colonoscopy
· Crohn's disease; affected areas are narrowed and ulcerated, and
multiple strictures are common
CT and MRI scans
· Bowel thickining and extrahepatic disease
· Pelvic or perineal involvement.
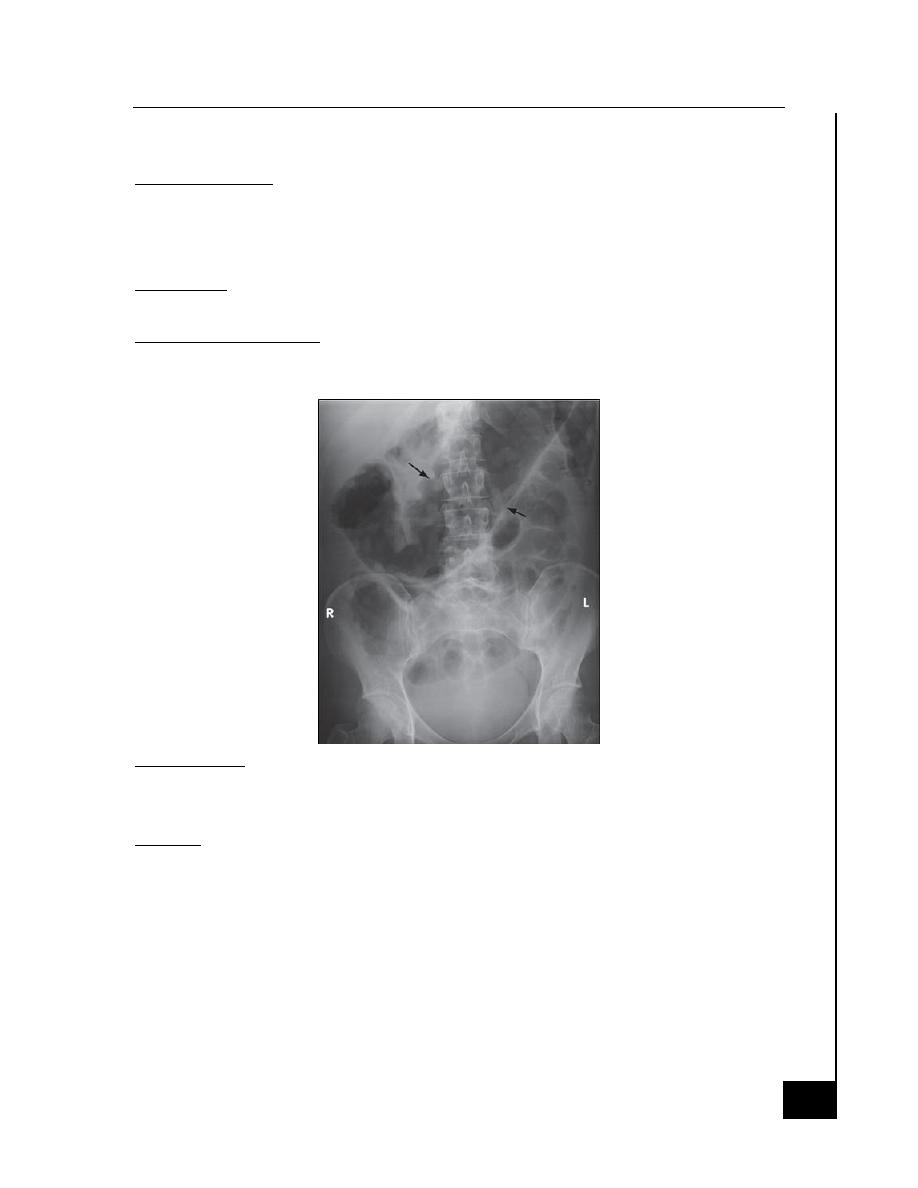
A plain abdominal X-ray
· With severe active disease.
o Dilatation of the colon
o Perforation may be found.
o In small bowel Crohn's disease there may be evidence of
intestinal obstruction or displacement of bowel loops by a
mass.
Ultrasound
· Thickened small bowel loops
· Abscess development in Crohn's disease.
Management
· Treat acute attacks
· Prevent relapses
· Select patients for surgery
· Detect carcinoma at an early stage
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
14
Treat acute attacks
Aminosalicylates
Mode of action: modulate cytokine release
Oral or topical (enema/suppository)
Mesalamine
· Pentasa (time dependent release)
· Ascol (PH dependent release)
With carrier
· Sulfasalazine, balsalazide, olsalazine
Side-effects 10-45%
· Headache
· Nausea
· Diarrhea
· Blood dyscrasia
Corticosteroids
· Anti-inflammatory
· Topical and oral and I.V
· Prednisolone
· Hydrocortisone
· Budesonide
Cyclosporine
· Suppresses T-cell expansion
· Rescue' therapy to prevent surgery in ulcerative colitis responding
poorly to corticosteroids.
· No value in Crohn's disease
· Major side-effects in 0-17% nephrotoxicity, infections, neurotoxicity
· Minor complications in up to 50%: tremor, paraesthesiae, abnormal
liver function tests, hirsutism
Anti-TNF antibodies
(Infliximab and adalimumab)
· Suppress inflammation and induce apoptosis of inflammatory cells
· Moderately to severely active Crohn's disease, especially fistulating
· Severe active ulcerative colitis
· Anaphylactic reactions after multiple infusions
· Contraindicated in the presence of infections; reactivation of
tuberculosis
Antibiotics
· Useful in perianal Crohn's disease
Antidiarrhoeal agents (codeine phosphate, loperamide, lomotil)
· Reduce gut motility and small bowel secretion
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
15
· Avoided in acute flare-ups of disease
· May precipitate colonic dilatation
Prevent relapses
Thiopurines
(Azathioprine, 6-mercaptopurine)
· Immunomodulation by inducing T-cell cytotoxic effect
· Effective after 12 weeks of starting therapy
Complications in 20%.
· Flu-like syndrome with myalgia
Leucopenia in 3%
· Safe during pregnancy
Methotrexate
· Anti-inflammatory (folic acid antagonist)
· In 10-18%. Nausea, stomatitis, diarrhoea, hepatotoxicity and
pneumonitis
Ciclosporin
Anti-TNF antibodies
Ulcerative colitis
Active proctitis and proctosigmoiditis
· In mild to moderate disease mesalamine enemas or suppositories
combined with oral mesalazine are effective first-line therapy.
· Topical corticosteroids are less effective and are reserved for patients
who are intolerant of topical mesalazine.
· Patients who fail to respond are treated with oral prednisolone.
Active left-sided or extensive colitis
· In mildly active cases, high-dose aminosalicylates combined with
topical aminosalicylate
· Oral prednisolone 40 mg daily is indicated for more active disease or
when initial aminosalicylate therapy is ineffective
Severe ulcerative colitis
· Hospital admission
· Monitored clinically: for the presence of abdominal pain,
temperature, pulse rate, stool blood and frequency
· Laboratory; haemoglobin, white cell count, albumin, electrolytes,
ESR and CRP
· Radiologically: for colonic dilatation on plain abdominal X-rays.
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
16
· Intravenous fluids
· Transfusion blood if Hb < 10 g/L
· Nutritional support
§
IV corticosteroids (hydrocortisone 400 mg/day)
§
Avoidance of opiates and antidiarrhoeal agents
§
Topical and oral aminosalicylates.
§
Patients who do not promptly respond to corticosteroids are
considered for intravenous ciclosporin or infliximab
· Those who do not respond after ' maximal medical treatment usually
require urgent colectomy.
· Which, in approximately 30% of cases, 7-10 days overcomes the need
for urgent colectomy.
Maintenance of remission
· Life-long therapy recommended
· Extensive disease
· Distal disease who relapse more than once a year.
· Oral aminosalicylates first line
· Patients who frequently relapse despite aminosalicylate drugs are
treated with thiopurines.
Crohn's disease
Active colitis or ileocolitis
· Aminosalicylates
· Corticosteroids
· In severe disease intravenous steroids
Isolated ileal disease
· Corticosteroids.
· Aminosalicylates have little added value
· Poorly responding patients should, at an early stage, be considered
for surgical resection since this is associated with prolonged remission
in most cases.
Fistulas and perianal disease.
· Surgical intervention required for abscess
· For simple perianal disease metronidazole and/or ciprofloxacin are
first-line therapies.
· Treatment of underlying active disease with corticosteroids and
nutritional support usually by TPN.
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
17
· Infliximab and adalimumab heal enterocutaneous fistulas and
perianal disease in many patients.
Maintenance of remission
· Aminosalicylates have minimal efficacy.
· Thiopurines for relapse more than once a year or severe disease.
· Patients who are intolerant of or resistant to thiopurines should be
treated with once-weekly methotrexate combined with folic acid.
· Patients with aggressive disease are managed using a combination of
immunosuppressives and anti-TNF therapy.
Indications for surgery in ulcerative colitis
Impaired quality of life
· Loss of occupation or education
· Disruption of family life
Failure of medical therapy
· Dependence upon oral corticosteroids
· Complications of drug therapy
Fulminant (severe) colitis no response
Disease complications unresponsive to medical therapy
· Arthritis
· Pyoderma gangrenosum
Colon cancer or severe dysplasia
Indications for surgery in Crohn's disease
· The indications for surgery are similar to those for ulcerative colitis.
· Unresponsive fulminant disease
· Operations are often necessary to deal with abscesses
· Relieve small or large bowel obstruction.
· Chronic fistulating small bowel disease may require resection if no
reponse
The end of this lecture
Sabeeh & CHW
Inf
la
mm
at
or
y
bo
w
el
d
is
ea
ses
Lecture 66
Medicine
Dr. Rabah
18
اﻟﺳﻼم ﻋﻠﯾﻛم
ﻣﺣﺎﺿرة
60
Hyperlipidaemia
د. ﺳﺎﻟم اﻟرﺑﯾﻌﻲ ﻧزﻟت ﺑﺎرت
واﺣد و ﻻ ﯾوﺟد ﺑﺎرت آﺧر ﻷن ھذا ﻛل ﻣﺎ ﺷرﺣﮫ اﻟدﻛﺗور و ﺳﺄﻗوم
ً ﺑرﻓﻊ اﻟﺑورﺑوﯾﻧت ﻟﻣن ﯾﺣب اﻹطﻼع ﻋﻠﻰ ﺑﺎﻗﻲ اﻟﺳﻼﯾدات )ﺷﻛرا
ﺑﺔ آﻻء ﺗرةَ ﻛرﺑ و ءﻻآ و لﯾﺑﻧ ﻰﻔطﺻﻣﻟ
J
(
ﺑﮭذه اﻟﻣﺣﺎﺿرة ﻧﺧﺗﺗم ﻣﺣﺎﺿرات اﻟﺑﺎطﻧﯾﺔ ﻟﮭذا اﻟﻌﺎم
أﺣب أن أوﺟﮫ ﺷﻛري ﻟﻛل ﻣن
ﺳﺎﻋد ﻓﻲ اﻟﻣﺣﺎﺿرات ﺑﺄي ﺷﻛل
ﻟﻛم ﺟﻣﯾﻌﻛمً ارﻛﺷ اذﻟ ةرﯾﺛﻛ ءﺎﻣﺳﻷا
My last Medicine lecture ever!!
THE END OF ALL LECTURES J
ﻣﻊ
اﻟﺗﻣﻧﯾﺎت ﺑﺎﻟﻣوﻓﻘﯾﺔ و اﻟﻧﺟﺎح ﺑﺎﻟﻔﺎﯾﻧل
Yours
Sabeeh & CHW
JJJJJJJJJJ
