PERIPHERAL ARTERIAL DISEASE
Almost all peripheral arterial disease (PAD) is due to atherosclerosis. The pathology of PAD is similar to coronary artery disease and the most important risk factors are smoking, diabetes, hyperlipidaemia and hypertension.Plaque rupture is responsible for the most serious manifestations of the disease, and often occurs in a plaque that hitherto has been asymptomatic. Only one-quarter of affected patients have symptoms. The clinical manifestations depend upon: The anatomical site The presence or absence of a collateral supply The speed of onset The mechanism of injury
CHRONIC LOWER LIMB ARTERIAL DISEASEPAD affects the leg eight times more often than the arm.The lower limb arterial tree comprises: The aorto-iliac ('inflow‘) Femoro-popliteal and Infra-popliteal ('outflow') segments One or more segments may be affected in a variable and asymmetric manner. Chronic lower limb ischaemia presents as two distinct clinical entities: Intermittent claudication Critical limb ischaemia
The presence and severity of ischaemia can be determined by clinical examination and measurement of the ankle:brachial pressure index (ABPI), the ratio between the (highest systolic) ankle and brachial blood pressures.In health the ABPI is > 1.0In intermittent claudication typically 0.5-0.9In critical limb ischaemia usually < 0.5.
FEATURES OF CHRONIC LOWER LIMB ISCHAEMIA-Pulses-diminished or absent -Bruits-denote turbulent flow but bear no relationship to the severity of the underlying disease -Reduced skin temperature -Pallor on elevation and rubor on dependency (Buerger's sign) -Superficial veins that fill sluggishly and empty ('gutter') upon minimal elevation -Muscle-wasting -Skin and nails-dry, thin and brittle -Loss of hair
Intermittent claudicationIschaemic pain of the leg muscles precipitated by walking and relieved by rest is known as intermittent claudication (IC). The pain is usually felt in the calf muscles because the disease tends to affect the superficial femoral artery. However, the pain may be felt in the thigh or buttock if the iliac arteries are involved. Typically, the pain comes on after a reasonably constant 'claudication' distance, and rapidly and completely subsides on stopping walking.
Intermittent claudicationResumption of walking leads to a return of the pain. Most patients describe a cyclical pattern of exacerbation and resolution due to the progression of disease and the subsequent development of collaterals. The annual mortality rate exceeds 5%, which is 2-3 times higher than an equivalent non-claudicant population due to the fact that IC is nearly always found in association with widespread atherosclerosis. Most claudicants succumb to MI or stroke.
General measures to reduce cardiovascular mortality, many of which may also improve the functional status of the limb, are central to patient management. Peripheral vasodilators such as cilostazol can improve symptoms in patients with intermittent claudication. Intervention (angioplasty, stenting, endarterectomy or bypass) is usually only considered once best medical therapy has been instituted and given at least 6 months to effect symptomatic improvement, and then only in those patients who are severely disabled or whose livelihood is threatened by their disability.
BEST MEDICAL THERAPY FOR PERIPHERAL ARTERIAL DISEASE -Cessation of smoking -Regular exercise (in a typical claudicant this would entail 30 minutes of walking three times per week) -Antiplatelet agent (aspirin 75 mg daily or clopidogrel 75 mg daily) -Reduction of cholesterol (diet + statin therapy) -Diagnosis and treatment of diabetes mellitus (all should have fasting glucose measured) -Diagnosis and treatment of frequently associated conditions (e.g. hypertension, anaemia, heart failure)
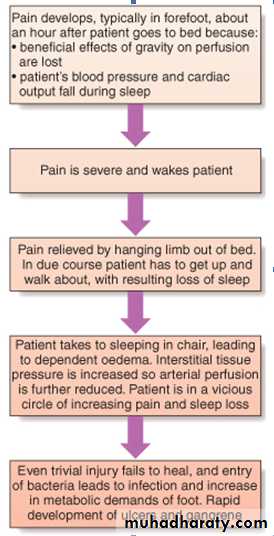
Critical limb ischaemia-Critical limb ischaemia (CLI) is defined as rest (night) pain, requiring opiate analgesia, and/or tissue loss (ulceration or gangrene), present for more than 2 weeks, in the presence of an ankle blood pressure of less than 50 mmHg. -Rest pain and no tissue loss with ankle pressures above 50 mmHg is sometimes known as subcritical limb ischaemia (SCLI). -The term severe limb ischaemia (SLI) is often used to describe both entities. -Whereas IC is usually due to single-segment plaque, CLI is always due to multi-level disease.
Patients with CLI are at risk of losing their limb, sometimes their life, in a matter of weeks or months without surgical bypass or endovascular revascularisation. However, treatment is difficult because such patients represent end-stage disease, have severe multi-level disease, are usually elderly and nearly always have significant multi-system comorbidity.
Imaging is performed using duplex ultrasonography, and additional more detailed non-invasive imaging can be provided by MRI or CT with intravenous injection of contrast agents. Intra-arterial digital subtraction angiography is mainly used for those patients who are thought suitable for endovascular revascularisation.
Buerger's disease (thromboangiitis obliterans)This is an inflammatory obliterative arterial disease that is distinct from atherosclerosis. It is more common in people from the Mediterranean and North Africa. It is likely that there is a strong genetic element. Buerger's disease usually presents in young (20-30 years) male smokers and characteristically affects the peripheral arteries, giving rise to claudication in the feet or rest pain in the fingers or toes.
The condition also affects the veins, and superficial thrombophlebitis is common. Wrist and ankle pulses are usually absent, but brachial and popliteal pulses are characteristically palpable.Arteriography shows narrowing or occlusion of arteries below the knee but relatively healthy vessels above that level.
The condition often remits if the patient stops smoking; sympathectomy and prostaglandin infusions may be helpful. If amputation is required it can often be limited to the digits at first. However, bilateral below-knee amputation is the most frequent outcome if patients continue to smoke.
CHRONIC UPPER LIMB ARTERIAL DISEASE
The subclavian artery is the most common site of disease, which may manifest as:1-Arm claudication (rare). 2-Atheroembolism (blue finger syndrome). Small emboli lodge in digital arteries and may be confused with Raynaud's phenomenon, except that in this case the symptoms are unilateral. Failure to make the diagnosis may eventually lead to amputation. 3-Subclavian steal. When the arm is used, blood is 'stolen' from the brain via the vertebral artery. This leads to vertebro-basilar ischaemia, which is characterised by dizziness, cortical blindness and/or collapse.Most subclavian artery disease should be treated by means of angioplasty with or without stenting, as the results are good and surgery (carotid-subclavian bypass) is difficult.
RAYNAUD'S PHENOMENON AND RAYNAUD'S DISEASE
Raynaud's phenomenonCold and sometimes emotional stimuli may trigger vasospasm in the peripheral arteries.Raynaud's phenomenon describes the characteristic sequence of digital pallor due to vasospasm, followed by cyanosis due to the presence of deoxygenated blood, and then rubor due to reactive hyperaemia.Primary Raynaud's phenomenonThis is also called Raynaud's disease and affects 5-10% of young women in temperate climates. The condition is often familial and usually appears between the ages of 15 and 30 years. It does not progress to ulceration or infarction and significant pain is unusual.
No investigation is necessary and the patient should be reassured and advised to avoid exposure to cold, in the first instance. Treatment with a long-acting preparation of nifedipine may also be helpful. The underlying cause is unclear. Sympathectomy is not indicated.
Secondary Raynaud's phenomenonThis is also known as Raynaud's syndrome and tends to occur in older people in association with:-Connective tissue disease (most commonly systemic sclerosis or the CREST syndrome) -Vibration-induced injury (from the use of power tools) -Thoracic outlet obstruction (e.g. cervical rib).
In contrast to primary disease the condition is associated with fixed obstruction of the digital arteries; fingertip ulceration and necrosis are often present and pain is usual. The fingers must be protected from cold and trauma, infection requires treatment with antibiotics, and surgery should be avoided if possible. Vasoactive drugs have no clear benefit. Sympathectomy helps for a year or two. Prostacyclin infusions are sometimes beneficial.
ACUTE LIMB ISCHAEMIA
Acute limb ischaemia is most frequently caused by one of the following mechanisms:1. Acute thrombotic occlusion of a pre-existing stenotic arterial segment.2. Thromboembolism 3. Trauma, which may be iatrogenic.Apart from paralysis (inability to move toes/fingers) and paraesthesia (loss of light touch over the dorsum of the foot/hand), the so-called 'Ps of acute ischaemia' are non-specific for ischaemia and/or inconsistently related to its severity. Pain on squeezing the calf indicates muscle infarction and impending irreversible ischaemia.
Symptoms/signs
CommentPain Pallor May be absent in complete acute ischaemia, and can be present in chronic ischaemia
Pulselessness
Perishing cold :Unreliable, as the ischaemic limb takes on the ambient temperature
Paraesthesia Paralysis :-Important features of impending irreversible ischaemiaAll suspected acutely ischaemic limbs must be discussed immediately with a vascular surgeon; a few hours can make the difference between death/amputation and complete recovery of limb function. If there are no contraindications (for example, acute aortic dissection or trauma, particularly head injury), an intravenous bolus of heparin (3000-5000 U) should be administered to limit propagation of thrombus and protect the collateral circulation.
Distinguishing thrombosis from embolism is frequently difficult but it is important because treatment and prognosis are different. Acute limb ischaemia due to thrombosis can usually be treated medically in the first instance: intravenous heparin (target APTT 2.0-3.0), antiplatelet agents, high-dose statins, intravenous fluids to avoid dehydration, correction of anaemia, oxygen and sometimes prostaglandins such as iloprost. Careful monitoring is required.
Acute limb ischaemia due to embolus will normally result in extensive tissue necrosis within 6 hours unless the limb is revascularized. The indications for thrombolysis remain controversial but, in general, enthusiasm for this treatment is waning. Irreversible ischaemia mandates early amputation or palliative therapy.
Clinical features Embolism Thrombosis in situ
Severity Complete (no collaterals) Incomplete (collaterals)Onset Seconds or minutes Hours or days
Limb Leg 3:1 arm Leg 10:1 arm
Multiple sites Up to 15% Rare
Embolic source Present (usually AF) Absent
Previous claudication Absent Present
Palpation of artery Soft, tender Hard, calcified
Bruit Absent Present
Contralateral leg pulses Present Absent
Diagnosis Clinical Angiography
Treatment Embolectomy, warfarin Medical, bypass, thrombolysis
Prognosis Loss of life > loss of limb Loss of limb > loss of life