Thyroid gland
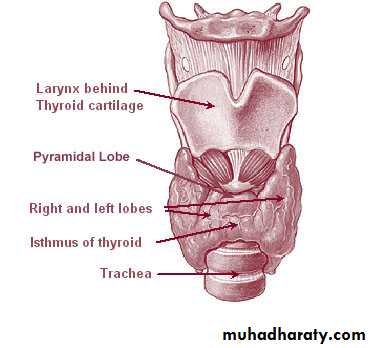
Anatomy :The thyroid gland is a butterfly-shaped organ and is composed of two cone-like lobes or wings, lobus dexter (right lobe) and lobus sinister (left lobe), connected via the isthmus. The organ is situated on the anterior side of the neck, lying against and around the larynx and trachea, reaching posteriorly the oesophagus and carotid sheath. It starts cranially at the oblique line on the thyroid cartilage (just below the laryngeal prominence, or 'Adam's Apple'), and extends inferiorly to approximately the fifth or sixth tracheal ring. It is difficult to demarcate the gland's upper and lower border with vertebral levels because it moves position in relation to these during swallowing. Between the two layers of the capsule and on the posterior side of the lobes, there are on each side two parathyroid glands.
The thyroid isthmus is variable in presence and size, can change shape and size, and can encompass a cranially extending pyramid lobe (lobus pyramidalis or processus pyramidalis), remnant of the thyroglossal duct. The thyroid is one of the larger endocrine glands, weighing 2-3 grams in neonates and 18-60 grams in adults, and is increased in pregnancy.
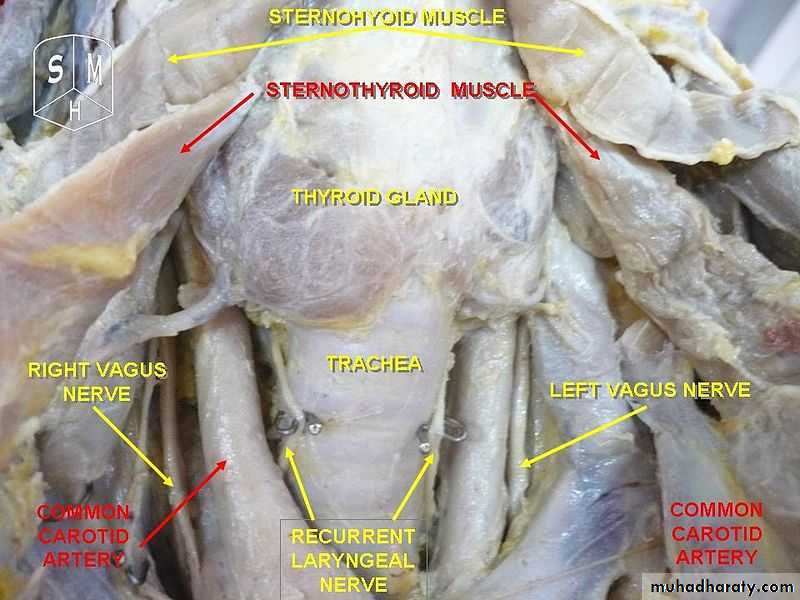
The thyroid is supplied with arterial blood from the superior thyroid artery, a branch of the external carotid artery, and the inferior thyroid artery, a branch of the thyrocervical trunk, and sometimes by the thyroid ima artery, branching directly from the brachiocephalic trunk. The venous blood is drained via superior thyroid veins, draining in the internal jugular vein, and via inferior thyroid veins, draining via the plexus thyroideus impar in the left brachiocephalic vein.
Lymphatic drainage passes frequently the lateral deep cervical lymph nodes and the pre- and parathracheal lymph nodes. The gland is supplied by parasympathetic nerve input from the superior laryngeal nerve and the recurrent laryngeal nerve.
Embryology
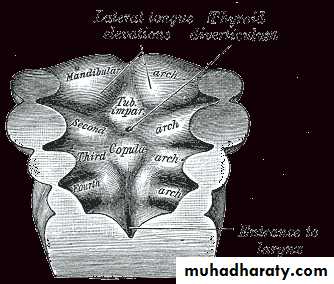
In the fetus, at 3–4 weeks of gestation, the thyroid gland appears as an epithelial proliferation in the floor of the pharynx at the base of the tongue between the tuberculum impar and the copula linguae at a point later indicated by the foramen cecum. The thyroid then descends in front of the pharyngeal gut as a bilobed diverticulum through the thyroglossal duct. Over the next few weeks, it migrates to the base of the neck, passing anterior to the hyoid bone. During migration, the thyroid remains connected to the tongue by a narrow canal, the thyroglossal duct.Thyrotropin-releasing hormone (TRH) and thyroid-stimulating hormone (TSH) start being secreted from the fetal hypothalamus and pituitary at 18-20 weeks of gestation, and fetal production of thyroxine (T4) reach a clinically significant level at 18–20 weeks. Fetal triiodothyronine (T3) remains low (less than 15 ng/dL) until 30 weeks of gestation, and increases to 50 ng/dL at term. Fetal self-sufficiency of thyroid hormones protects the fetus against e.g. brain development abnormalities caused by maternal hypothyroidism. However, preterm births can suffer neurodevelopmental disorders due to lack of maternal thyroid hormones due their own thyroid being insufficiently developed to meet their postnatal needs.
The portion of the thyroid containing the parafollicular C cells, those responsible for the production of calcitonin, are derived from the neural crest. This is first seen as the ultimobranchial body, which joins the primordial thyroid gland during its descent to its final location in the anterior neck.
Aberrations in embryological development can cause various forms of thyroid dysgenesis.
Physiology
The primary function of the thyroid is production of the hormones triiodothyronine (T3), thyroxine (T4), and calcitonin. Up to 80% of the T4 is converted to T3 by peripheral organs such as the liver, kidney and spleen. T3 is several times more powerful than T4, which is largely a prohormone, perhaps four or even ten times more active.T3 and T4 production and action
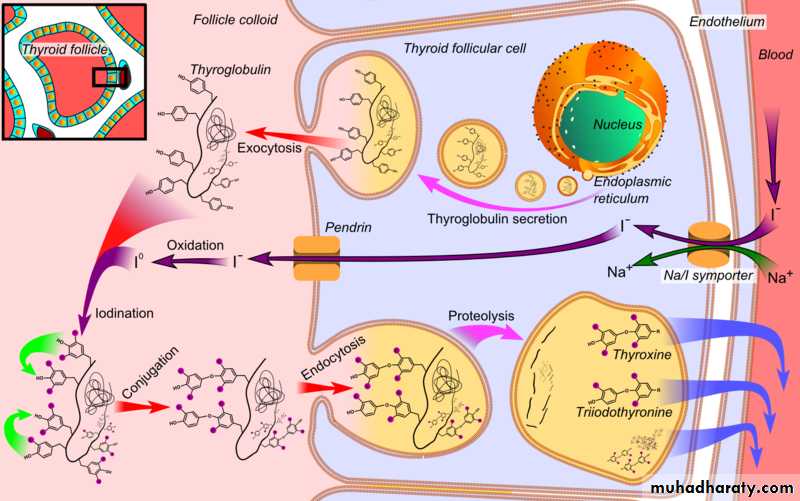
Thyroxine (T4) is synthesised by the follicular cells from free tyrosine and on the tyrosine residues of the protein called thyroglobulin (Tg). Iodine is captured with the "iodine trap" by the hydrogen peroxide generated by the enzyme thyroid peroxidase(TPO) and linked to the 3' and 5' sites of the benzene ring of the tyrosine residues on Tg, and on free tyrosine. Upon stimulation by the thyroid-stimulating hormone (TSH), the follicular cells reabsorb Tg and cleave the iodinated tyrosines from Tg in lysosomes, forming T4 and T3 (in T3, one iodine atom is absent compared to T4), and releasing them into the blood. Deiodinase enzymes convert T4 to T3. Thyroid hormone secreted from the gland is about 80-90% T4 and about 10-20% T3. T3 can activate phosphatidylinositol 3-kinase by a mechanism that may be cytoplasmic in origin or may begin at integrin alpha V beta3.
In the blood, T4 and T3 are partially bound to thyroxine-binding globulin (TBG), transthyretin, and albumin. Only a very small fraction of the circulating hormone is free (unbound) - T4 0.03% and T3 0.3%. Only the free fraction has hormonal activity. As with the steroid hormones and retinoic acid, thyroid hormones cross the cell membrane and bind to intracellular receptors (α1, α2, β1 and β2), which act alone, in pairs or together with the retinoid X-receptor as transcription factors to modulate DNA transcription
T3 and T4 regulation
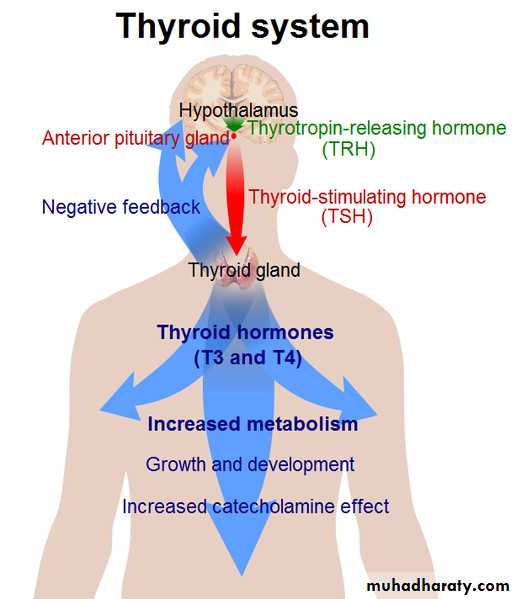
The production of thyroxine and triiodothyronine is regulated by thyroid-stimulating hormone (TSH), released by the anterior pituitary. The thyroid and thyrotropes form a negative feedback loop: TSH production is suppressed when the T4 levels are high.[21] The TSH production itself is modulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus and secreted at an increased rate in situations such as cold exposure (to stimulate thermogenesis). TSH production is blunted by somatostatin (SRIH), rising levels of glucocorticoids and sex hormones (estrogen and testosterone), and excessively high blood iodide concentration.An additional hormone produced by the thyroid contributes to the regulation of blood calcium levels. Parafollicular cells produce calcitonin in response to hypercalcemia. Calcitonin stimulates movement of calcium into bone, in opposition to the effects of parathyroid hormone (PTH). However, calcitonin seems far less essential than PTH, as calcium metabolism remains clinically normal after removal of the thyroid (thyroidectomy), but not the parathyroids.
Disorders
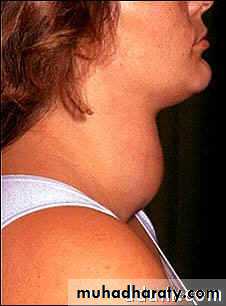
Thyroid disorders include hyperthyroidism (abnormally increased activity), hypothyroidism (abnormally decreased activity) and thyroid nodules, which are generally benign thyroid neoplasms, but may be thyroid cancers. All these disorders may give rise to goiter, that is, an enlarged thyroid. Hypothyroidism is the underproduction of the thyroid hormones T3 and T4. Hypothyroid disorders may occur as a result of congenital thyroid abnormalities (see congenital hypothyroidism), autoimmune disorders such as Hashimoto's thyroiditis, iodine deficiency (more likely in poorer countries) or the removal of the thyroid following surgery to treat severe hyperthyroidism and/or thyroid cancer. Typical symptoms are abnormal weight gain, tiredness, baldness, cold intolerance, and bradycardia. Hypothyroidism is treated with hormone replacement therapy, such as levothyroxine, which is typically required for the rest of the patient's life. Thyroid hormone treatment is given under the care of a physician and may take a few weeks to become effective.Negative feedback mechanisms result in growth of the thyroid gland when thyroid hormones are being produced in sufficiently low quantities as a means of increasing the thyroid output; however, where the hypothyroidism is caused by iodine insufficiency, the thyroid is unable to produce T3 and T4 and as a result, the thyroid may continue to grow to form a non-toxic goiter. It is termed non-toxic as it does not produce toxic quantities of thyroid hormones, despite its size.
thyroid Problems Diagnosis
The medical history and physical exam are important parts of the evaluation for thyroid problems. The health care practitioner will focus on eye, skin, cardiac (heart), and neurologic findings.1. Blood tests
Thyroid-stimulating hormone (TSH): In most cases, this is the single most useful lab test in diagnosing thyroid disease. When there is an excess of thyroid hormone in the blood, as in hyperthyroidism, the TSH is low. When there is too little thyroid hormone, as in hypothyroidism, the TSH is high.
Free (T4): T4 is one of the thyroid hormones. High T4 may indicate hyperthyroidism. Low T4 may indicate hypothyroidism.
Triiodothyronine (T3): T3 is another one of the thyroid hormones. High T3 may indicate hyperthyroidism. Low T3 may indicate hypothyroidism.
TSH receptor antibody (TSI): This antibody is present in Grave's disease.
Antithyroid antibody: This antibody is present in Hashimoto's and Grave's disease.
2. Nuclear thyroid scan: During this scan a small amount of radioactive iodine is swallowed or a similar material 99m-technetium, is injected into the blood, and then an imaging study of the thyroid is taken that reveals localization of the radioactivity. Increased uptake of the radioactive material in the thyroid gland indicates hyperthyroidism, while decreased uptake is present in hypothyroidism. This test should not be performed on women who are pregnant.
3.Thyroid ultrasound: Thyroid ultrasound helps to determine the size and number as well as the different types of nodules in the thyroid gland. This exam can also detect if there are enlarged parathyroid glands or lymph nodes near the thyroid gland.
4.Fine-needle aspiration: During this procedure, a small needle is inserted into the thyroid gland in order to get a sample of thyroid tissue, usually from a nodule. This test can be done in a health care practitioner's office without special preparations. The tissue is then observed under a microscope by a pathologist to look for any signs of cancer.
5. Computerized axial tomography (CT) scan: A CT scan is occasionally used to look for the extent of a large goiter into the upper chest or to look for narrowing or displacement of the trachea (breathing tube) from the goiter.
Hypothyroidism Causes
Loss of thyroid tissue: Treatment of hyperthyroidism by radioactive destruction of thyroid tissue or surgical removal of thyroid tissue can result in hypothyroidism. Antithyroid antibodies: These may be present in people who have diabetes, lupus, rheumatoid arthritis, chronic hepatitis, or Sjogren‘s syndrome. These antibodies may cause decreased production of thyroid hormones. Congenital: Hypothyroidism can be present from birth. This is commonly discovered early with nationwide newborn screening for this disease. Defects in the production of thyroid hormone: Hashimoto's thyroiditis occurs when there are defects in the production of thyroid hormone, resulting in an increased amount of TSH. The increased TSH results in a goiter (enlargement of the thyroid gland itself that can be seen as an obvious swelling in the front of the neck). Medications: Some medications, particularly lithium may cause a drug-induced hypothyroidism.Hypothyroidism (Low Thyroid Hormone Level) Signs and Symptoms
Symptoms of hypothyroidism in infants can include:
1. Constipation 2. Poor feeding 3. Poor growth 4. Jaundice (yellow discoloration of the skin and eyes) 5. Excessive tiredness
Symptoms of hypothyroidism in children include:
1. Symptoms similar to adult symptoms 2. Excessive fatigue 3. Poor growth 4. Poor school performance
Symptoms of hypothyroidism in adults include:
a. Early symptoms
1. Easy fatigue, exhaustion 2. Poor tolerance to cold temperatures 3. Constipation 4. Carpal tunnel syndrome(pain at the wrists and numbness of the hands)
b. Later symptoms
1. Poor appetite 2. Weight gain 3. Dry skin 4. Hair loss 5. Intellectual ability worsens 6.Deeper, hoarse voice 7. Puffiness around the eyes 8. Depression 9. Irregular menstrual periods or lack of menstrual periods
Hypothyroidism in Pregnancy
Newly diagnosed hypothyroidism in pregnancy is rare because most women with untreated hypothyroidism do not ovulate or produce mature eggs in a regular manner, which makes it difficult for them to conceive.It is a difficult new diagnosis to make based on clinical observation. The signs and symptoms of hypothyroidism (fatigue, poor attention span, weight gain, numbness, and tingling of the hands or feet) are also prominent symptoms of a normal pregnancy.
Undiagnosed hypothyroidism during pregnancy increases the chance of stillbirth or growth retardation of the fetus. It also increases the chance that the mother may experience complications of pregnancy such as anemia, eclampsia, and placental abruption.
Probably the largest group of women who will have hypothyroidism during pregnancy are those who are currently on thyroid hormone replacement. The ideal thyroxine replacement dose (for example, levothyroxine [Synthroid, Levoxyl, Levothroid, Unithroid]) during pregnancy may rise by 25% to 50% during pregnancy. It is important to have regular checks of T4 and TSH blood levels as soon as pregnancy is confirmed; and frequently through the first 20 weeks of pregnancy to make sure the woman is taking the correct medication dose.
Treatment of Hypothyroidism
L-thyroxine (Synthroid, Levoxyl, Levothroid, Unithroid): This medication is the mainstay of thyroid hormone replacement therapy in hypothyroidism. This is a synthetic form of thyroxine. This is exactly the same hormone that the thyroid makes. The body tissues convert it to the active product L-triiodothyronine. Side effects are rare, and it has an excellent safety record.L-triiodothyronine: This is rarely used alone as thyroid hormone replacement, because it has a much shorter persistence in the blood than L-thyroxine. Its use can cause rapid increases in L-triiodothyronine concentration, which can be dangerous in the elderly and in people with cardiac disease. It may be used in combination with L-thyroxine for people who have poor symptomatic relief with L-thyroxine alone.Thyroid extract or "natural" thyroid hormone: This is dried and powdered pig thyroid gland. The hormone is not purified and the exact amount of T4 and T3 can be variable. This is not recommended as a thyroid hormone replacement. There is an excess of T3 in this preparation.
treatment
Myxedema coma
Myxedema coma is a loss of brain function as a result of severe, longstanding low level of thyroid hormone in the blood (hypothyroidism). Myxedema coma is considered a life-threatening complication of hypothyroidism and represents the far more serious side of the spectrum of thyroid disease.
Myxedema coma is not common, but tends to be seen more frequently in elderly patients and in women. There is an increased incidence in the winter months, which is likely secondary to the extremes in temperature. Myxedema coma can actually result in death. Fortunately, the condition is rare.
the symptoms of hypothyroidism
Before a patient develops myxedema coma, features of hypothyroidism are usually present and may have gone unsuspected for a long period of time.These symptoms include:
fatigue,
lethargy,
mental impairment,
depression
cold intolerance
hoarseness
dry skin
weight gain
change in menstrual cycles
Constipation and
headaches.
The causes myxedema coma
Most patients with myxedema coma have a history of hypothyroidism, thyroid surgery, or radioactive iodine treatment for thyroid disease. Very rarely, the problem is not caused by the inability of the thyroid gland to make thyroid hormone; but rather is caused by the failure of the pituitary gland or the hypothalamus to correctly signal the thyroid gland to perform its normal functions. In this situation, the thyroid gland is normal, but it is not receiving the signals from the pituitary gland or hypothalamus to make the thyroid hormone it is capable of producing.The triggers of myxedema coma
Certain factors may suddenly trigger myxedema coma in a person with poorly controlled hypothyroidism. These include:
1. Drugs particularly sedatives, narcotics, anesthesia, lithium and amiodarone
2. infections
3. stroke
4. trauma
5. heart failure
6. gastrointestinal bleeding
7. hypothermia (abnormally low body temperature) and
failing to take thyroid medications as prescribed.
The symptoms of myxedema coma
When a patient presents with myxedema coma the following may be present:
1.the body temperature is usually abnormally low (hypothermia), the core
temperature may be as low as 80 F (26.6 C);
2.severe mental changes including hallucinations, disorientation, seizures, and
ultimately, deep coma;
3.significant swelling (edema) all over the body with swollen eyes and
thickening of the tongue,
4.sparse, dry hair, and loss of the outer thirds of the eyebrows;
5.difficulty breathing;
6.collections of fluid around the lungs and heart (pleural effusion and
pericardial effusions);
7.the heart may slow down and its ability to pump blood forward can be
impaired;
8.the gastrointestinal tract does not function well and sometimes it becomes
paralyzed, thereby necessitating surgery; and
9.blood test abnormalities are a result of the increased fluid in the body. For
example, sodium levels drop because of dilution, which is caused by the body
retaining extra water.
myxedema coma diagnosed: Initial laboratory evaluation usually includes a test for thyroid function(TSH, T3 and T4 levels). Other blood tests, as well as heart and lung function testing, may also be needed.
the treatment for myxedema coma: Treatment may include assisting the patient to breathe and warming them to raise the body temperature to normal. Often, antibiotics are started until it is certain that an infection is not present.
The method of replacing thyroid hormone in patients with myxedema coma is controversial. Many different approaches are used. In general, initial replacement is done by intravenous infusion, since the intestinal system may not be absorbing properly.
While common hypothyroidism without myxedema is usually treated with T4 replacement (the hormone produced in greatest quantity by the thyroid gland), in the case of myxedema coma, management is different. The thyroid gland also produces a small amount of another hormone, T3. This is the more metabolically active of the two hormones. In patients who are well, T4 is converted into T3 in the bloodstream. However, patients with myxedema coma are often so sick that this conversion is impaired. As a result, many doctors choose to treat these patients with T3 initially and start T4 therapy as well. Since T4 therapy can take a month or so to work, there is usually an overlap of these two hormones. Care is taken to avoid heart rhythm abnormalities (arrhythmias) and stress on the heart, which can be caused by replacing thyroid hormone too quickly, particularly in elderly patients.
While mild thyroid disorders can be managed by primary care physicians, myxedema coma is generally managed by a thyroid specialist (endocrinologist) because treatment can be cmplicated and critical.
myxedema coma be prevented
The ideal way to manage this condition is to prevent it from occurring in the first place. An individual with hypothyroidism should visit their doctor regularly for follow-up and blood testing to be certain that their replacement dose is appropriate.
If an individual has symptoms that concerns them, but has not been diagnosed with hypothyroidism, they should visit their health care practitioner to discuss their concerns and explore the option of testing for thyroid imbalance.
Hyperthyroidism
Hyperthyroidism is a condition in which an overactive thyroid gland is producing an excessive amount of thyroid hormones that circulate in the blood. ("Hyper" means "over" in Greek). Thyrotoxicosis is a toxic condition that is caused by an excess of thyroid hormones from any cause. Thyrotoxicosis can be caused by an excessive intake of thyroid hormone or by overproduction of thyroid hormones by the thyroid gland. Because both physicians and patients often use these words interchangeably, we will take some liberty by using the term "hyperthyroidism" throughout this article.causes of hyperthyroidism include:
1. Graves' Disease2. Functioning adenoma ("hot nodule") and toxic multinodular goiter(TMNG)
3. Excessive intake of thyroid hormones
4. Abnormal secretion of TSH
5. Thyroiditis (inflammation of the thyroid gland)
6. Excessive iodine intake
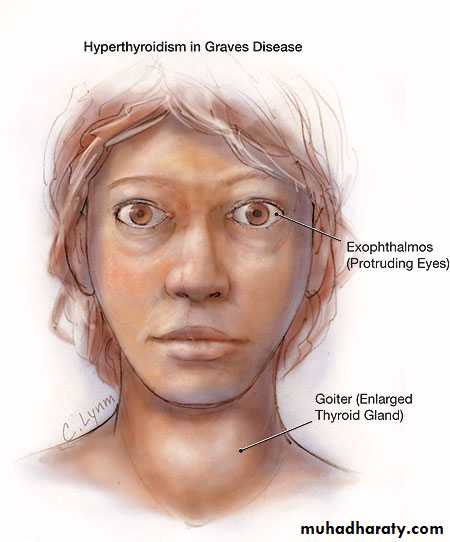
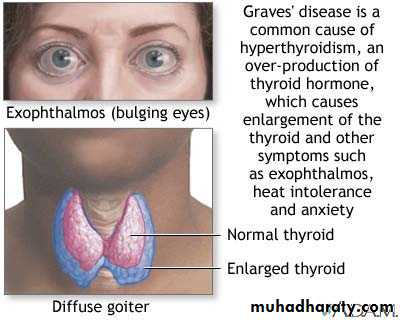
1. Graves' Disease
Graves' disease, which is caused by a generalized overactivity of the thyroid gland, is the most common cause of hyperthyroidism. In this condition, the thyroid gland usually is renegade, which means it has lost the ability to respond to the normal control by the pituitary gland via TSH. Graves' disease is hereditary and is up to five times more common among women than men. Graves' disease is thought to be an autoimmune disease, and antibodies that are characteristic of the illness may be found in the blood. These antibodies include thyroid stimulating immunoglobulin (TSI antibodies), thyroid peroxidase antibodies (TPO), and TSH receptor antibodies. The triggers for Grave's disease include:
stress, smoking, radiation to the neck, medications, and infectious organisms such as viruses.
Graves' disease can be diagnosed by a standard, nuclear medicine thyroid scan which shows diffusely increased uptake of a radioactively-labeled iodine. In addition, a blood test may reveal elevated TSI levels.
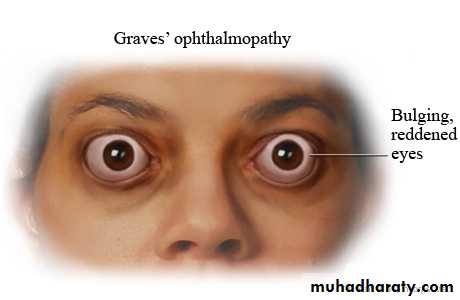
Grave's disease may be associated with eye disease (Graves' ophthalmopathy) and skin lesions (dermopathy). Ophthalmopathy can occur before, after, or at the same time as the hyperthyroidism. Early on, it may cause sensitivity to light and a feeling of "sand in the eyes." The eyes may protrude and double vision can occur. The degree of ophthalmopathy is worsened in those who smoke. The course of the eye disease is often independent of the thyroid disease, and steroid therapy may be necessary to control the inflammation that causes the ophthalmopathy. In addition, surgical intervention may be required. The skin condition (dermopathy) is rare and causes a painless, red , lumpy skin rash that appears on the front of the legs.
2. Functioning Adenoma and Toxic Multinodular Goiter
The thyroid gland (like many other areas of the body) becomes lumpier as we get older. In the majority of cases, these lumps do not produce thyroid hormones and require no treatment. Occasionally, a nodule may become "autonomous," which means that it does not respond to pituitary regulation via TSH and produces thyroid hormones independently. This becomes more likely if the nodule is larger that 3 cm. When there is a single nodule that is independently producing thyroid hormones, it is called a functioning nodule. If there is more than one functioning nodule, the term toxic, multinodular goiter is used. Functioning nodules may be readily detected with a thyroid scan.3. Excessive intake of thyroid hormones
Taking too much thyroid hormone medication is actually quite common. Excessive doses of thyroid hormones frequently go undetected due to the lack of follow-up of patients taking their thyroid medicine. Other persons may be abusing the drug in an attempt to achieve other goals such as weight loss. These patients can be identified by having a low uptake of radioactively-labelled iodine (radioiodine) on a thyroid scan.
4. Abnormal secretion of TSH
A tumor in the pituitary gland may produce an abnormally high secretion of TSH (the thyroid stimulating hormone). This leads to excessive signaling to the thyroid gland to produce thyroid hormones. This condition is very rare and can be associated with other abnormalities of the pituitary gland. To identify this disorder, an endocrinologist performs elaborate tests to assess the release of TSH.
5.Thyroiditis (inflammation of the thyroid)
Inflammation of the thyroid gland may occur after a viral illness (subacute thyroiditis). This condition is association with a fever and a sore throat that is often painful on swallowing. The thyroid gland is also tender to touch. There may be generalized neck aches and pains. Inflammation of the gland with an accumulation of white blood cells known as lymphocytes (lymphocytic thyroiditis) may also occur. In both of these conditions, the inflammation leaves the thyroid gland "leaky," so that the amount of thyroid hormone entering the blood is increased. Lymphocytic thyroiditis is most common after a pregnancy and can actually occur in up to 8% of women after delivery. In these cases, the hyperthyroid phase can last from 4 to 12 weeks and is often followed by a hypothyroid (low thyroid output) phase that can last for up to 6 months. The majority of affected women return to a state of normal thyroid function. Thyroiditis can be diagnosed by a thyroid scan.
6. Excessive iodine intake
The thyroid gland uses iodine to make thyroid hormones. An excess of iodine may cause hyperthyroidism. Iodine-induced hyperthyroidism is usually seen in patients who already have an underlying abnormal thyroid gland. Certain medications, such as amiodarone, which is used in the treatment of heart problems, contain a large amount of iodine and may be associated with thyroid function abnormalities.
the symptoms of hyperthyroidism
Hyperthyroidism is suggested by several signs and symptoms; however, patients with mild disease usually experience no symptoms. In patients older than 70 years, the typical signs and symptoms also may be absent. In general, the symptoms become more obvious as the degree of hyperthyroidism increases. The symptoms usually are related to an increase in the metabolic rate of the body.Common symptoms include:
1. Excessive sweating
2. Heat intolerance
3. Increased bowel movements
4. Tremor (usually fine shaking)
5. Nervousness; agitation
6. Rapid heart rate
7. Weight loss
8. Fatigue
9. Decreased concentration
10.Irregular and scant menstrual flow
In older patients, irregular heart rhythms and heart failure can occur. In its most severe form, untreated hyperthyroidism may result in "thyroid storm," a condition involving high blood pressure, fever, and heart failure. Mental changes, such as confusion and delirium, also may occur.
hyperthyroidism diagnosis
Hyperthyroidism can be suspected in patients with:tremors, excessive sweating, smooth velvety skin, fine hair, a rapid heart rate, and
an enlarged thyroid gland.
There may be puffiness around the eyes and a characteristic stare due to the elevation of the upper eyelids. Advanced symptoms are easily detected, but early symptoms, especially in the elderly, may be quite inconspicuous. In all cases, a blood test is needed to confirm the diagnosis.
The blood levels of thyroid hormones can be measured directly and usually are elevated with hyperthyroidism. However, the main tool for detection of hyperthyroidism is measurement of the blood TSH level. As mentioned earlier, TSH is secreted by the pituitary gland. If an excess amount of thyroid hormone is present, TSH is "down-regulated" and the level of TSH falls in an attempt to reduce production of thyroid hormone. Thus, the measurement of TSH should result in low or undetectable levels in cases of hyperthyroidism. However, there is one exception. If the excessive amount of thyroid hormone is due to a TSH-secreting pituitary tumor, then the levels of TSH will be abnormally high. This uncommon disease is known as "secondary hyperthyroidism."
Although the blood tests mentioned previously can confirm the presence of excessive thyroid hormone, they do not point to a specific cause. If there is obvious involvement of the eyes, a diagnosis of Graves' disease is almost certain. A combination of antibody screening (for Graves' disease) and a thyroid scan using radioactively-labelled iodine (which concentrates in the thyroid gland) can help diagnose the underlying thyroid disease. These investigations are chosen on a case-by-case basis.
hyperthyroidism treatment
The options for treating hyperthyroidism include:
1. Treating the symptoms
2. Antithyroid drugs
3. Radioactive iodine
4. Surgery treating symptoms
1. Treating the symptomsThere are medications available to immediately treat the symptoms caused by excessive thyroid hormones, such as a rapid heart rate. One of the main classes of drugs used to treat these symptoms is the beta-blockers [for example, propranolol , atenolol , metoprolol ]. These medications counteract the effect of thyroid hormone to increase metabolism, but they do not alter the levels of thyroid hormones in the blood. A doctor determines which patients to treat based on a number of variables including the underlying cause of hyperthyroidism, the age of the patient, the size of the thyroid gland, and the presence of coexisting medical illnesses.
2. Antithyroid Drugs
There are two main antithyroid drugs available for use in the United States, methimazole and propylthiouracil (PTU). These drugs accumulate in the thyroid tissue and block production of thyroid hormones. PTU also blocks the conversion of T4 hormone to the more metabolically active T3 hormone. The major risk of these medications is occasional suppression of production of white blood cells by the bone marrow (agranulocytosis). (White cells are needed to fight infection.) It is impossible to tell if and when this side effect is going to occur, so regular determination of white blood cells in the blood are not useful.It is important for patients to know that if they develop a fever, a sore throat, or any signs of infection while taking methimazole or propylthiouracil, they should see a doctor immediately. While a concern, the actual risk of developing agranulocytosis is less than 1%. In general, patients should be seen by the doctor at monthly intervals while taking antithyroid medication. The dose is adjusted to maintain the patient in as close to a normal thyroid state as possible (euthyroid). Once the dosing is stable, patients can be seen at three month intervals if long-term therapy is planned.
Usually, long-term antithyroid therapy is only used for patients with Graves' disease, since this disease may actually go into remission under treatment without requiring treatment with thyroid radiation or surgery. If treated from one to two years, the data shows remission rates of 40%-70%. When the disease is in remission, the gland is no longer overactive, and antithyroid medication is not needed.
Recent studies also have shown that adding a pill of thyroid hormone to the antithyroid medication actually results in higher remission rates. The rationale for this may be that by providing an external source for thyroid hormone, higher doses of antithyroid medications can be given, which may suppress the overactive immune system in persons with Graves' disease. This type of therapy remains controversial, however. When long-term therapy is withdrawn, patients should continue to be seen by the doctor every three months for the first year, since a relapse of Graves' disease is most likely in this time period. If a patient does relapse, antithyroid drug therapy can be restarted, or radioactive iodine or surgery may be considered.
3. Radioactive Iodine
Radioactive iodine is given orally (either by pill or liquid) on a one-time basis to ablate a hyperactive gland. The iodine given for ablative treatment is different from the iodine used in a scan. (For treatment, the isotope iodine 131 is used, while for a routine scan, iodine 123 is used.) Radioactive iodine is given after a routine iodine scan, and uptake of the iodine is determined to confirm hyperthyroidism. The radioactive iodine is picked up by the active cells in the thyroid and destroys them. Since iodine is only picked up by thyroid cells, the destruction is local, and there are no widespread side effects with this therapy.Radioactive iodine ablation has been safely used for over 50 years, and the only major reasons for not using it are pregnancy and breast-feeding. This form of therapy is the treatment of choice for recurring Graves' disease, patients with severe cardiac involvement, those with multinodular goiter or toxic adenomas, and patients who cannot tolerate antithyroid drugs. Radioactive iodine must be used with caution in patients with Graves' related eye disease since recent studies have shown that the eye disease may worsen after therapy. If a woman chooses to become pregnant after ablation, it is recommended she wait 8-12 months after treatment before conceiving.
In general, more than 80% of patients are cured with a single dose of radioactive iodine. It takes between 8 to 12 weeks for the thyroid to become normal after therapy. Permanent hypothyroidism is the major complication of this form of treatment. While a temporary hypothyroid state may be seen up to six months after treatment with radioactive iodine, if it persists longer than six months, thyroid replacement therapy (with T4 or T3) usually is begun.
4. Surgery
Surgery to partially remove the thyroid gland (partial thyroidectomy) was once a common form of treatment for hyperthyroidism. The goal is to remove the thyroid tissue that was producing the excessive thyroid hormone. However, if too much tissue is removed, an inadequate production of thyroid hormone (hypothyroidism) may result. In this case, thyroid replacement therapy is begun. The major complication of surgery is disruption of the surrounding tissue, including the nerves supplying the vocal cords and the four tiny glands in the neck that regulate calcium levels in the body (the parathyroid glands). Accidental removal of these glands may result in low calcium levels and require calcium replacement therapy.With the introduction of radioactive iodine therapy and antithyroid drugs, surgery for hyperthyroidism is not as common as it used to be. Surgery is appropriate for:
1. pregnant patients and children who have major adverse reactions to antithyroid medications.
2. patients with very large thyroid glands and in those who have symptoms stemming from compression of tissues adjacent to the thyroid, such as difficulty swallowing, hoarseness, and shortness of breath.