4th stage
ObstetricsLec-
Dr.Wildan
6/4/2016
Hypertensive Disorders in PregnancyHypertension is one of commonest complications of pregnancy and it is a common cause of fetal and maternal morbidity and mortality .
It complicates 8-11% of all pregnancies .
Classification of hypertension:
Pre-existing (chronic) hypertension:Hypertension is present before pregnancy, detected in early pregnancy (before 20 weeks in absence of vesicular mole) and postpartum.
Examples:
Essential hypertension.
Secondary to chronic renal disorders e.g. (pyelonephritis and renal artery stenosis).
Coarctation of the aorta.
Systemic lupus erythematosus.
Pheochromocytoma.
Pregnancy-induced hypertension (PIH):
Transient hypertension : Late onset hypertension, without proteinuria or pathologic oedema.
Pre-eclampsia : Hypertension with proteinuria and / or oedema after 20 weeks of pregnancy, but may be earlier in vesicular mole.
Eclampsia : Pre-eclampsia + convulsions.
Superimposed pre-eclampsia or eclampsia:
Development of pre-eclampsia or eclampsia in pre-existing hypertension detected by a further increase of 30 mmHg or more in systolic blood pressure or 15 mmHg or more in diastolic blood pressure.Pre-eclampsia:
Incidence: 5-10%.
Aetiology:
Although eclampsia had been described since 200 years, no definite aetiology is found for PIH and it is still a disease of theories.
Predisposing factors:
Primigravidae more than multigravidae.Pre-existing hypertension.
Previous history of pre-eclampsia.
Family history of pre-eclampsia.
Hyperplacentosis i.e. excessive chorionic tissue as in hydatidiform mole, multiple pregnancy, uncontrolled diabetes mellitus and foetal haemolytic diseases.
Obesity.
Climatic variations.
Theories:
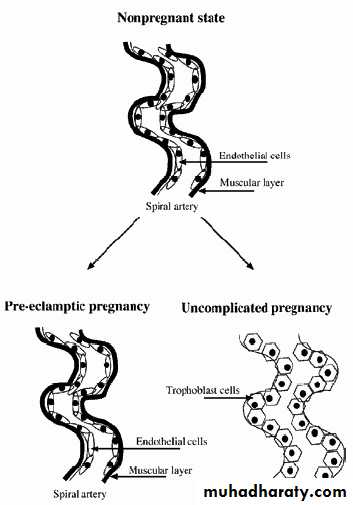
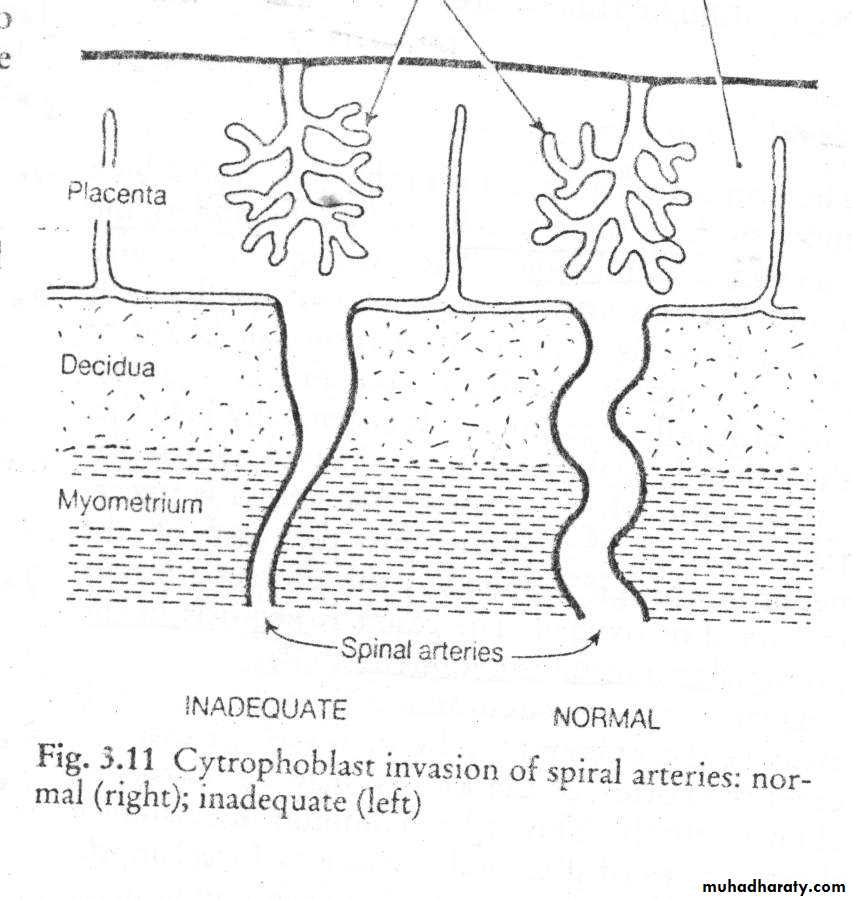
The uteroplacental bed:
In early pregnancy, the cytotrophoblasts invade the decidual arteries making their musculature more flaccid and dilated. During the second trimester of normal pregnancy, a second wave of invasion occurs into the myometrial segments of the spiral arteries. If the second invasion does not occur pre-eclampsia develops.
Immunological factor:
Stimulation of the maternal immune system by the early conceptus is essential for production of the blocking factors that prevent rejection of the foetus and placenta. Hypo immune response results in damage of the placenta and subsequent pre-eclampsia.Genetic factor:
A maternal autosomal recessive gene or a foetal genetic component could be responsible. An increase in HLA-DR4 (subtype of human leucocyte antigen) has been noted in pre-eclamptic women.Renin- angiotensin system:
It was found that the vascular sensitivity to angiotensin II is reduced in normal pregnancy while it increases in PIH.Angiotensin II-binding sites on platelets increase in women with PIH in comparison with normal pregnancy. This can identify the women in risk of developing PIH and hence prophylaxis against it can be achieved by anti-platelets as aspirin.
Atrial natriuretic peptide (ANP):
It’s release is stimulated by volume expansion and increase in atrial pressure. It is increased in normal pregnancy to ameliorate the effect of the increased angiotensin II. Actually, there is no evidence that there is decrease in ANP in PIH, but in contrast, it may be increased as a response to increased blood pressure.Prostaglandins:
Prostacyclin is a vasodilator and an inhibitor for platelets aggregation while thromboxane is a vasoconstrictor and platelets aggregator. In PIH, there is imbalance towards an increase in thromboxane production.
Neutrophils:
Neutrophils activation causes damage and dysfunction of the vascular endothelium leading to platelets aggregation, coagulation activation, hypertension and proteinuria.Pathological Changes:
VasospasmThe vascular changes and local hypoxia of the surrounding tissues lead to haemorrhage, necrosis and others.
Central nervous system: ischaemia, haemorrhages and oedema.
Liver: subcapsular haemorrhage, periportal necrosis and infarctions.
Endocrine glands: necrosis and haemorrhage in pituitary,pancreas and adrenal glands.
Heart and lungs: myocardial and endocardial haemorrhage and necrosis.
Lungs show haemorrhage and secondary bronchopneumonia.
Kidney: decrease in renal blood flow glomerular damage (glomerular endotheliosis)
leading to:
Decrease glomerular filtration rate by about 50%,
Loss of protein in urine (albuminuria),
Elevated serum levels of uric acid, urea and creatinine. Serum uric acid level is diagnostic and prognostic for severe pre-eclampsia.
Placenta:
Reduced utero-placental blood flow leading to intrauterine growth retardation (IUGR) and even death.
Placental thrombosis, infarction and abruptio placentae.
Retina: Vascular spasm,haemorrhage, exudate and rarely retinal detachment in
severe cases.
Coagulation status
Fibrin production is increased.
Fibrinolytic activity is decreased.
Factor VII, factor VIII- related antigen and fibrin/ fibrinogen degradation products (FDP) concentrations in the plasma are all increased.
Fibrin and platelet deposition is increased particularly in the placental arteries.
Thrombocytopenia.
Platelets are activated in the microcirculation of the placenta, kidney and liver, release their products as 5-hydroxytryptamine and re-enter the circulation in an exhausted state, unable to respond normally to aggregating agents.
The end result of these changes is hypercoagulability and disseminated intravascular coagulation in severe pre-eclampsia and eclampsia.
Sodium and water retention
There is haemoconcentration with fluid shift from the intravascular to the extravascular compartment.
HELLP syndrome is described in PIH which consists of: H = Haemolysis, EL= Elevated Liver enzymes, LP= Low Platelet count.
Diagnosis:
SignsHypertension: Blood pressure of 140/90 mmHg or more or an increase of 30 mmHg in systolic and/ or 15 mmHg in diastolic blood pressure over the pre- or early pregnancy level.
How to measure the blood pressure in pregnancy?
The patient should rest for at least 30 min. after arriving to the clinic.Remove any tight clothing from the right arm.
The patient lies comfortably on the left side that her back makes an angle of about 30o with the bed. The right arm is supported to be with the sphygmomanometer at the same level with the patient’s sternum i.e. her heart. Each cm above or below the level of the heart induces a difference of 0.7mmHg in blood pressure reading. She should lie undisturbed in this position for 2-3 min. before blood pressure is measured.
The cuff should be applied to the right upper arm with the connecting tubes pointing downwards, the centre of the rubber bag in the cuff is directly over the brachial artery leaving ante-cubital fossa free.
Apply cuff firmly but not tightly around the arm.
Feel the brachial artery and apply the stethoscope directly over it without undue pressure.
Pump up cuff rapidly to 20-30 mmHg above the point at which the pulse sound disappears, and take blood pressure reading without delay.
Let air out slowly so that mercury falls steadily by 2-3 mm/sec.
Blood pressure measurement phases (Korotkoff ( :
Korotkoff I Appearance of the sound systolic reading.
Korotkoff II Accentuation of the sound.
Korotkoff III Sound becomes harsh.
Korotkoff IV Sound becomes muffled diastolic reading.
Korotkoff V Disappearance of the sound.
Korotkoff I and IV is the reading for systolic and diastolic blood pressure respectively. If you wait the disappearance of the sound to take the diastolic reading (as in non-pregnant state) you may reach down to zero because of the hyperdynamic circulation during pregnancy.
Use the right arm for measuring because it is more convenient to the physician, but if the reading is 10 mmHg or more higher in the left arm use it in the future readings.
The blood pressure should be measured in two occasions at least 6 hours apart.
Proteinuria (albuminuria):
It is urinary protein greater than 0.3gm/L in 24 hours collection or greater than 1gm/L in two random samples obtained at least 6 hours apart.
It indicates glomerular damage and almost always occurs after hypertension.
Proteinuria is usually in the range of 1-3 gm daily, of which 50-60% is albumin but in severe cases it may exceed 15gm.
Oedema:
It is weight gain of more than 1 kg in any one week or 2.25 kg in any one month.Clinical oedema is present in about two-thirds of patients with PIH. However, two-thirds of pregnant women with clinical oedema do not develop hypertension.
Symptoms:
These are usually manifestations of severe pre-eclampsia :Headache: usually frontal but may be occipital. It is due to cerebral oedema and hypertension.
Visual disturbances: blurring of vision, flashes of light or blindness.
Epigastric or right upper quadrant pain: due to enlargement and subcapsular haemorrhage of the liver.
Nausea and vomiting: due to congestion of gastric mucosa and/ or cerebral oedema.
Oliguria or anuria: due to kidney pathology.