
AFTER MID
SURGERY
DR. Dawood Alobaidy
Orthopaedic
Disease of the spine:
Intervertebral disk lesion
Dr. Dawood Alobaidy
LECTURE 3

Diseases of the spine
Intervertebral disc lesions
• Lumbar backache is one of the most common causes of chronic disability,
• backache is associated with some abnormality of the intervertebral discs at the
lowest two levels of the spine (L4/5 and L5/S1).
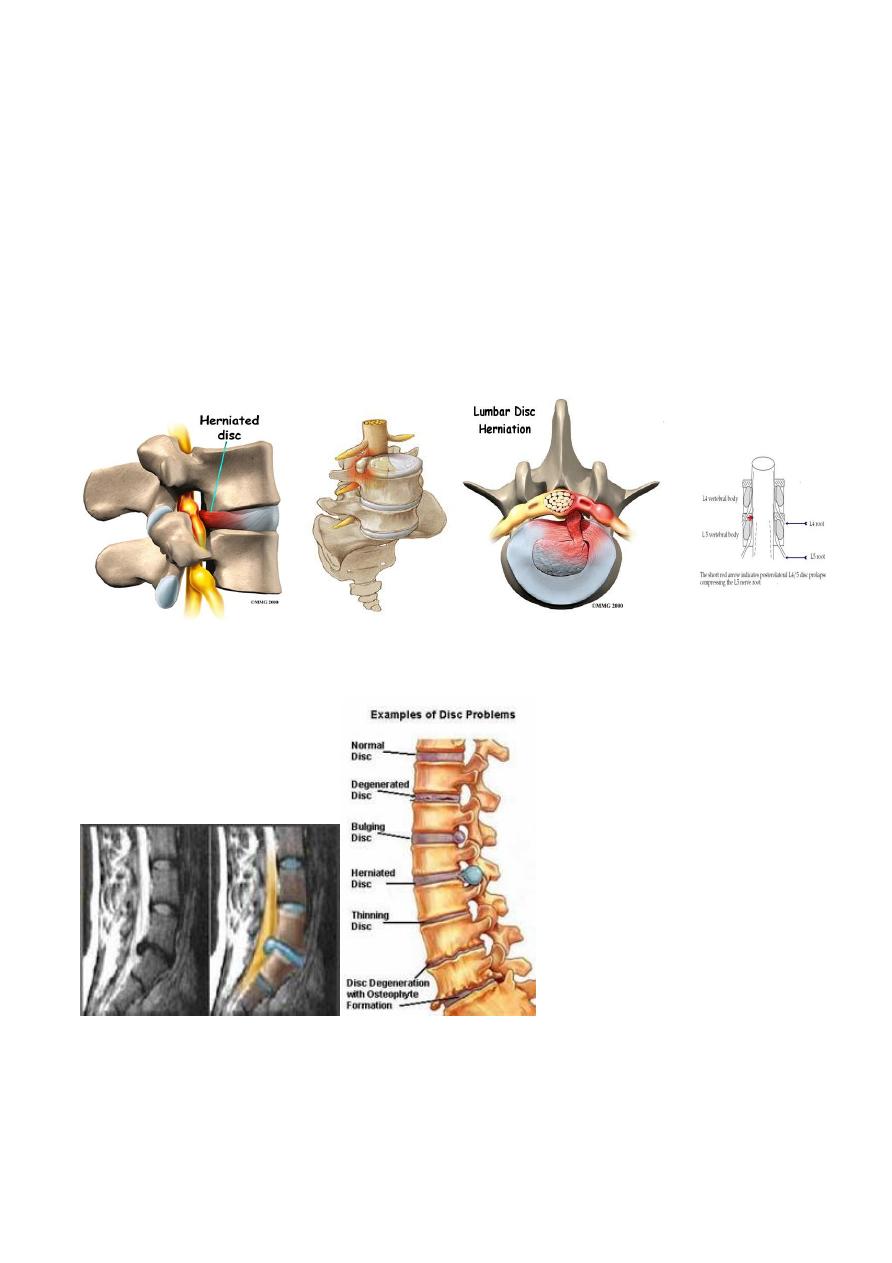
Prolapsed intervertebral disc
• In acute disc herniation the gelatinous nucleus pulposus squeezes through the
fibers of the annulus fibrosus and bulges posteriorly or posterolaterally beneath
the posterior longitudinal ligament.
• Local edema may add to the swelling, causing pressure on one of the nerve roots.
• With a complete rupture part of the nucleus may sequestrate and lie free in the
spinal canal.
Symptoms depend on the structure involved and the degree of compression.
• Pressure on the ligament probably accounts for backache;
• pressure on the dural envelope of the nerve root causes severe pain referred to
the lower limb (sciatica);
• compression of the nerve root itself causes pnumbness and parasthesia and
muscle weakness.
Clinical features:
• Patient is usually a young adult, during lifting or other severe activities
• sudden severe backache
• day or two later the pain is felt down in the buttocks or the calf (sciatica)
• Both backache and sciatica get worse by coughing or sneezing or straining.
• neurological symptoms may show according to the severity of the prolaps and its
direction and those may include sphenecteric disturbances.
• Patient stands with lateral deviation or list of the back (sciatica scoliosis), there is
limitation of all back movements.
• There is often tenderness in the midline of the low back, and paravertebral
muscle spasm.
• Straight leg raising is limited and painful on the affected side; dorsiflexion of the
foot may accentuate the pain.
• Sometimes raising the unaffected leg causes acute sciatic tension on the painful
side (crossed sciatic tension’).
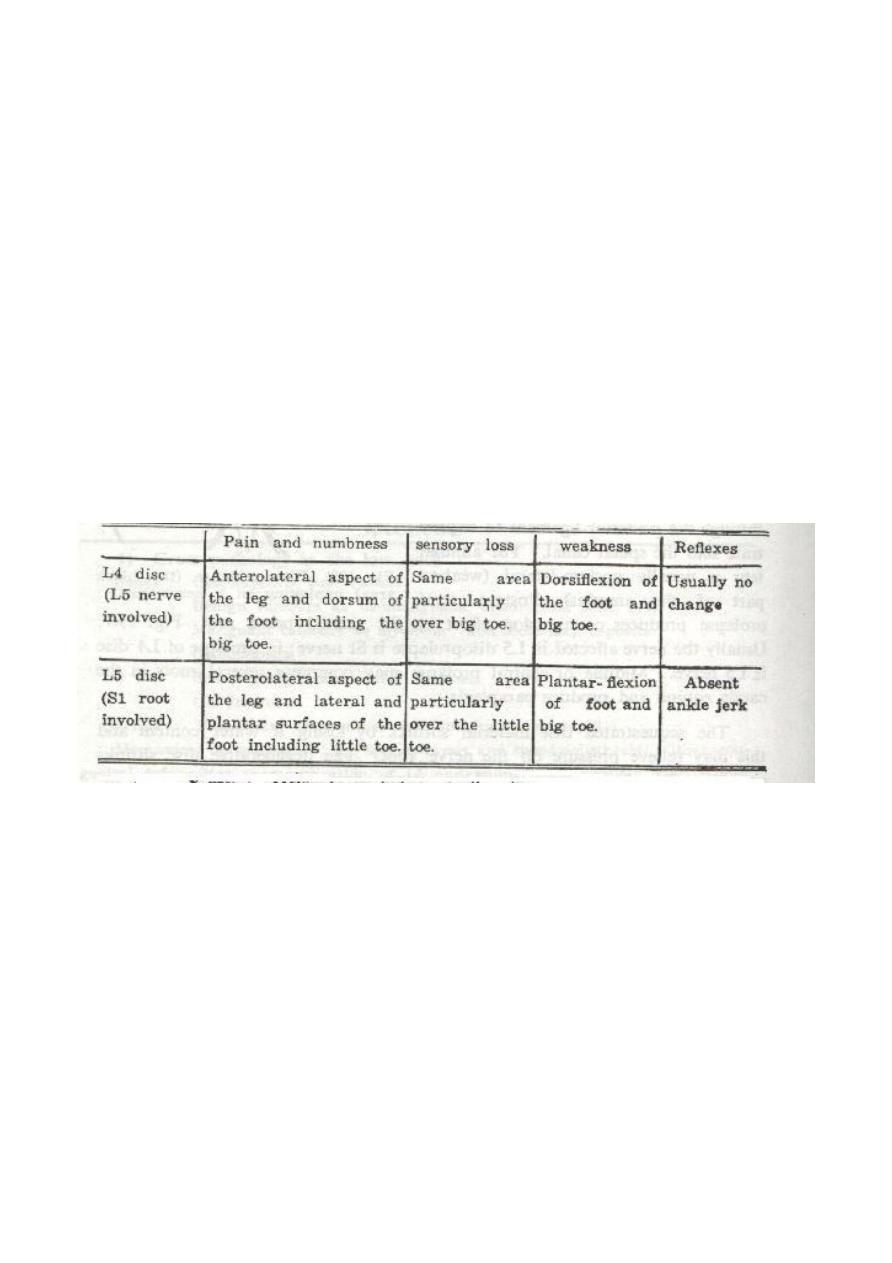
Neurological manifestations are:
X-ray:
• It does not show the disc itself,
• it exclude other bony lesions
• it can show associated muscle spasm as obliteration of lumber lordosis (straight
spine) or scoliosis or both.
• Later on there may be narrowing of the disc space.
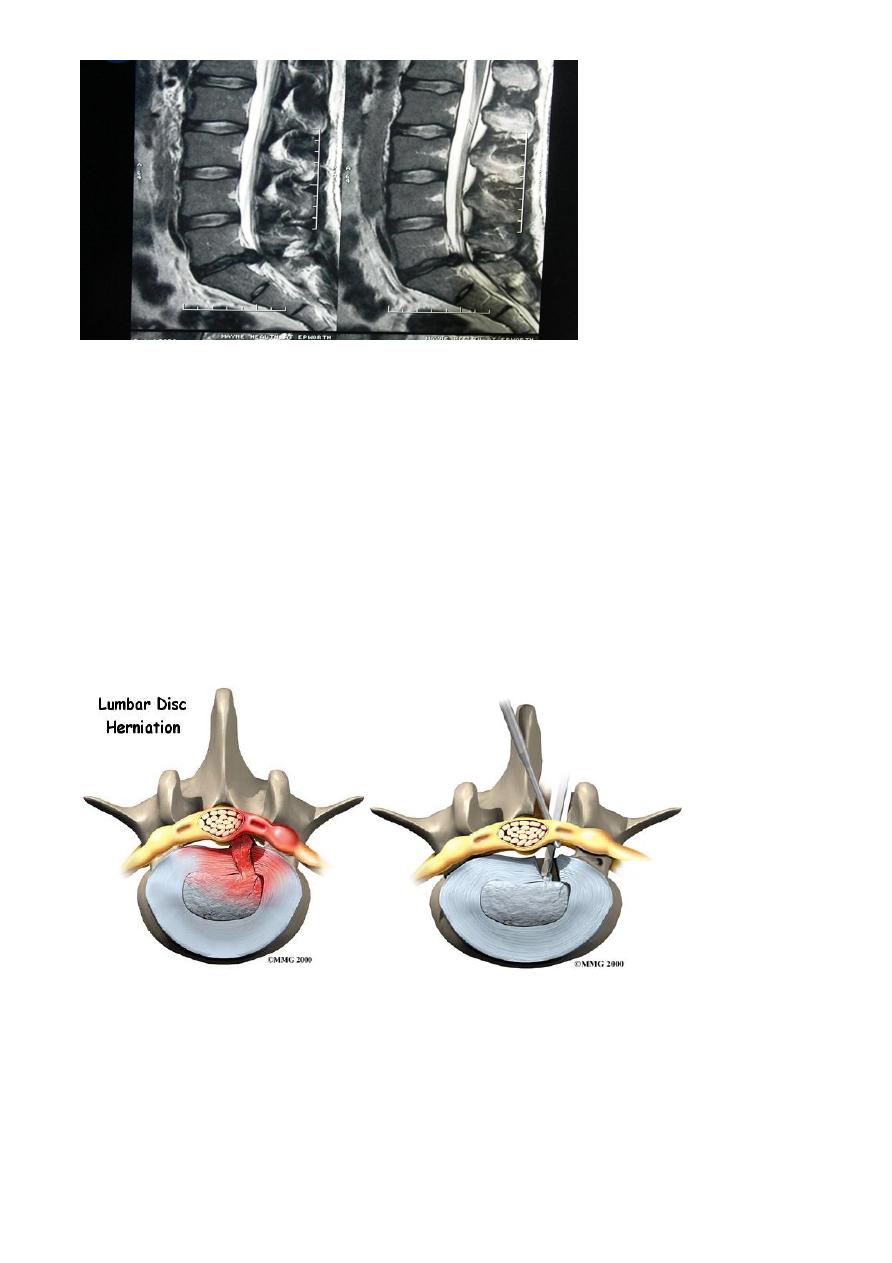
Mylography used to help but now it’s widely replaced by the more useful studies of MRI
or sometimes CT-scan
Treatment:
• Symptomatic drug treatment may include painkillers and NSAID with
physiotherapy
• 10-14 days of bed rest and skin traction on a hard mattress can help
autoreduction of the prolapsed disc,
• otherwise the prolapsed disc must be removed surgically (discectomy).
Indications for discectomy are:
• Cauda-eqina lesion (saddle parasthesia, paraparesis and uncontrolled bladder).
• Increasing complaint and pain despite treatment.
• Neurological deterioration despite treatment.
• Frequently recurrent attacks.
Complications:
• Lumber instability and later spondylosis.
• Spinal stenosis.
Done by : Murtedha Abbas
