
Medicine
Dr. Zuhair
Neurology
“
Central nervous system infections
”
Dr. Zuhair
LECTURE 16

Central nervous system infections
Dr. Zuhair
3
Central nervous system infections
Objectives
To know about clinical presentation of meningitis and Encephalitis
To know about the common infective organisms responsible meningitis
and encephalitis.
To know about the pathophysiology of meningitis and Encephalitis
To know how to investigate a patient suspected of intracranial infection
To know the main differential diagnosis of meningitis and of encephalitis
To know about empirical treatment of meningitis and encephalitis
To know about complications of meningitis and Encephalitis
Sites of CNS infection
In the meninges called meningitis
In the brain parenchyma called encephalitis
In the sinus, mastoid, middle ear, brain abscess and spinal epidural
abscess called parameningeal
So the clinical features of nervous system infections depend on the location of
the infection (the meninges or the parenchyma of the brain and spinal cord), the
causative organism (virus, bacterium, fungus or parasite), and whether the
infection is acute or chronic.
Note
: This lecture has been extensively edited by the students and contains much
more information than the one presented by the doctor, if you want you can find the
original unedited lecture in muhadharaty.com as a pdf or a slideshow.
Central nervous system infections
Dr. Zuhair
4
Meningitis
Is an acute inflammation of the protective membranes covering the brain and
spinal cord, known collectively as the meninges.
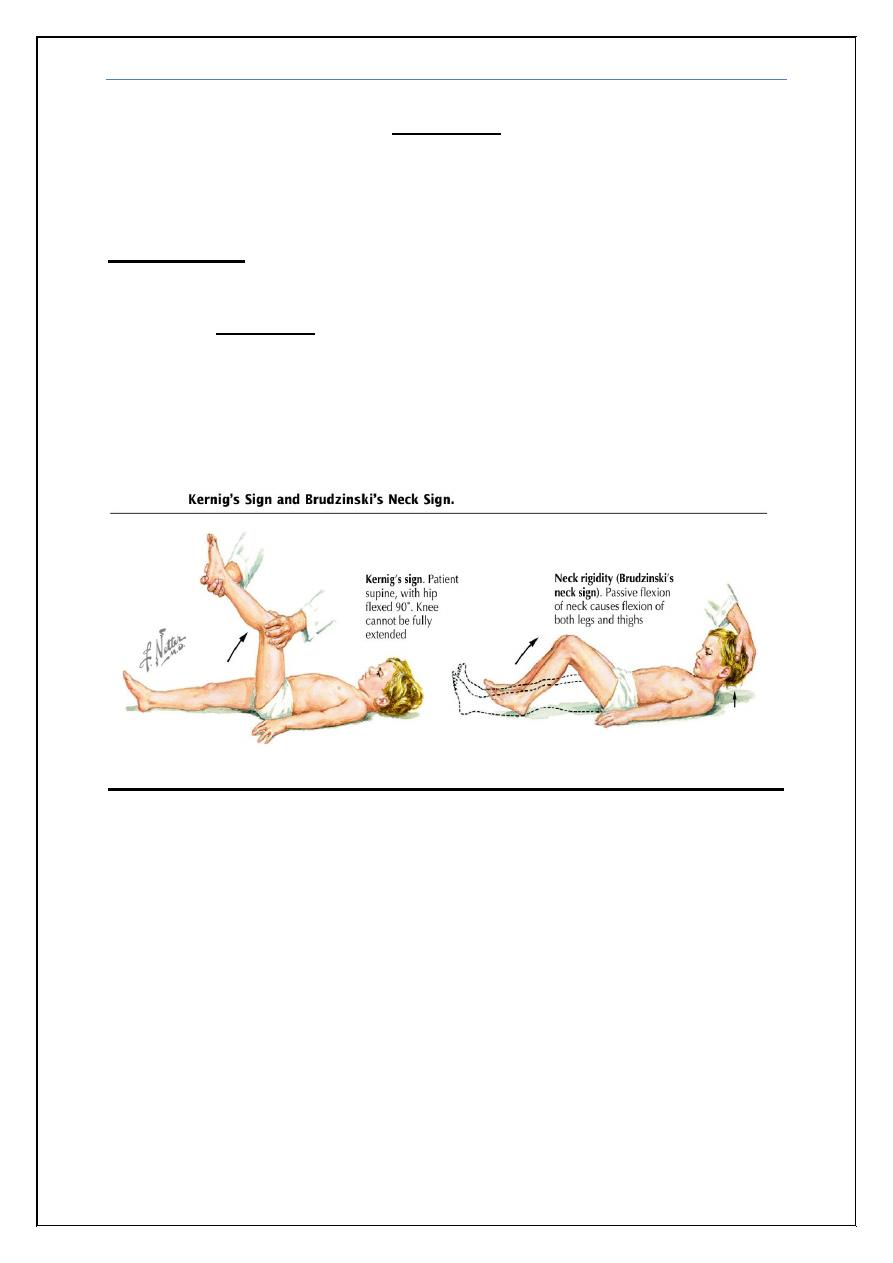
Presentation:
It presents with a characteristic combination of pyrexia, headache and
meningism. Meningism consists of headache, photophobia and stiffness of
the neck, often accompanied by other signs of meningeal irritation, including
Kerning’s sign (extension at the knee with the hip joint flexed causes spasm in
the hamstring muscles) and Brudzinski’s sign (passive flexion of the neck
causes flexion of the hips and knees). Meningism is not specific to meningitis
and can occur in patients with subarachnoid haemorrhage.
Sometime it may be associated with:
Disturbed level of consciousness
Vomiting and inability to tolerate light or loud noises
Seizures
Focal neurological manifestations
Young children often exhibit only nonspecific symptoms, such as
irritability, drowsiness, or poor feeding
Manifestations of the causative agent (e.g. : rash seen in meningococcal
Central nervous system infections
Dr. Zuhair
5
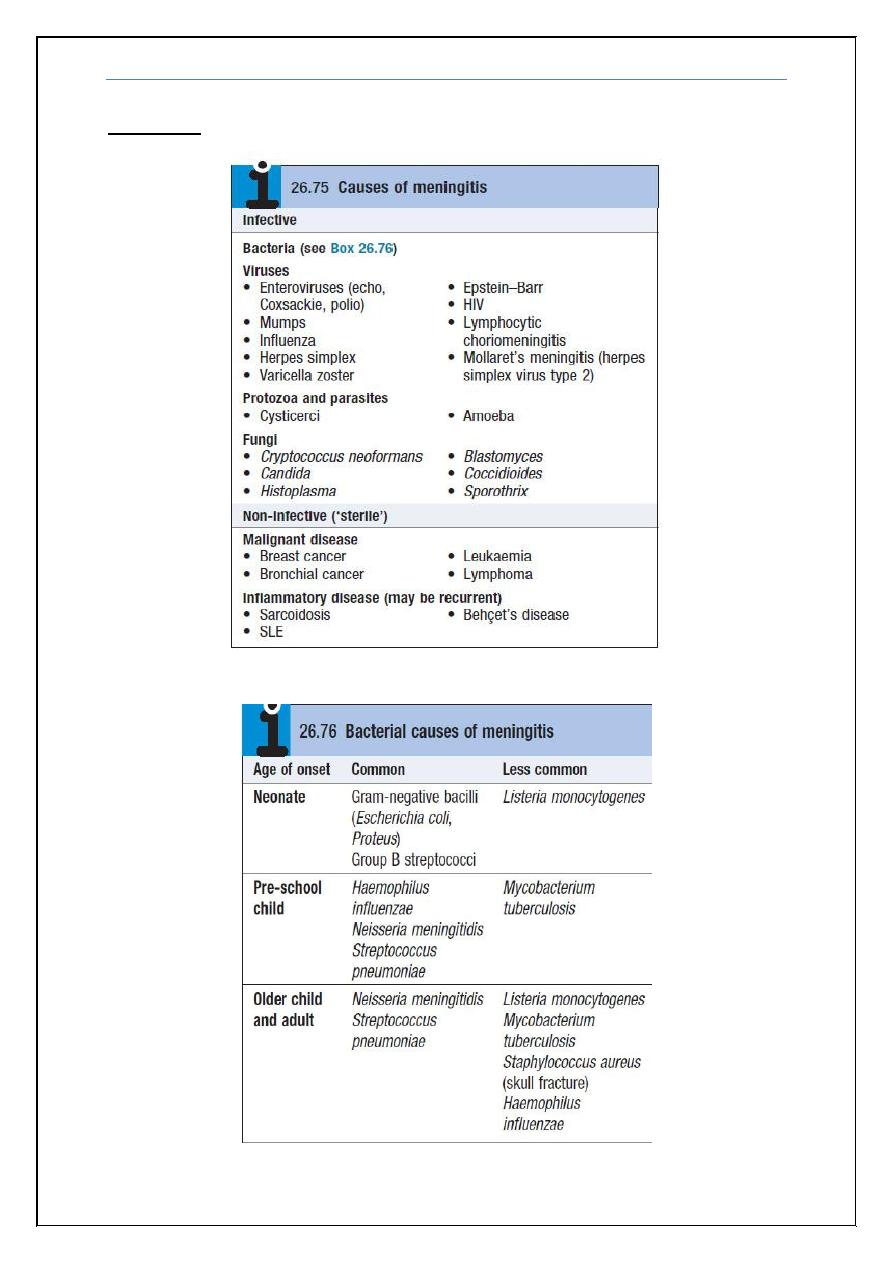
Etiology:
Central nervous system infections
Dr. Zuhair
6
Viral meningitis
Viruses are the most common cause of meningitis, usually resulting in a benign
and self-limiting illness requiring no specific therapy. It is much less serious
than bacterial meningitis, the most common being enteroviruses.
Clinical features
Viral meningitis occurs mainly in children or young adults, with acute onset of
headache and irritability and the rapid development of meningism. The
headache is usually the most severe feature. There may be a high pyrexia but
focal neurological signs are rare.
Investigations
The diagnosis is made by lumbar puncture. The CSF usually contains an excess
of lymphocytes but glucose and protein levels are commonly normal; the
protein level may be raised. It is extremely important to verify that the patient
has not received antibiotics (for whatever cause) prior to the lumbar puncture, as
this picture can also be found in partially treated bacterial meningitis.
Management
There is no specific treatment and the condition is usually benign and self-
limiting. The patient should be treated symptomatically in a quiet environment.
Recovery usually occurs within days.
Bacterial meningitis
Many bacteria can cause meningitis and certain organisms are particularly
common at different ages (see Box 26.76 above). Bacterial meningitis is usually
secondary to a bacteraemic illness or direct spread from an adjacent focus
of infection such as otitis media, skull fracture or sinusitis.
Bacterial meningitis has become less common because of the antibiotics
but mortality and morbidity remain significant. Streptococcus pneumoniae
and Neisseria Meningitides (meningococcus) are the most frequent causes
in Western Europe, while Haemophilus influenzae and Strep. pneumoniae are
most common in India and other part of the world. Epidemics of meningococcal
meningitis occur, particularly in cramped living conditions or where the climate
is hot and dry.
Central nervous system infections
Dr. Zuhair
7
Clinical features
Headache, drowsiness, fever and neck stiffness are the usual presenting
features.
Around 90% of patients with meningococcal meningitis have two of the
following:
Fever.
Neck stiffness.
Altered consciousness.
Purpuric rash.
When accompanied by septicaemia, it may present very rapidly, with
abrupt obtundation due to cerebral oedema and circulatory collapse.
Pneumococcal meningitis may be associated with pneumonia and occurs
especially in older patients, alcoholics and patients with no spleen.
Listeria monocytogenes is seen increasingly as a cause of meningitis and
brainstem encephalitis in the immunosuppressed, people with diabetes,
alcoholics and pregnant women.
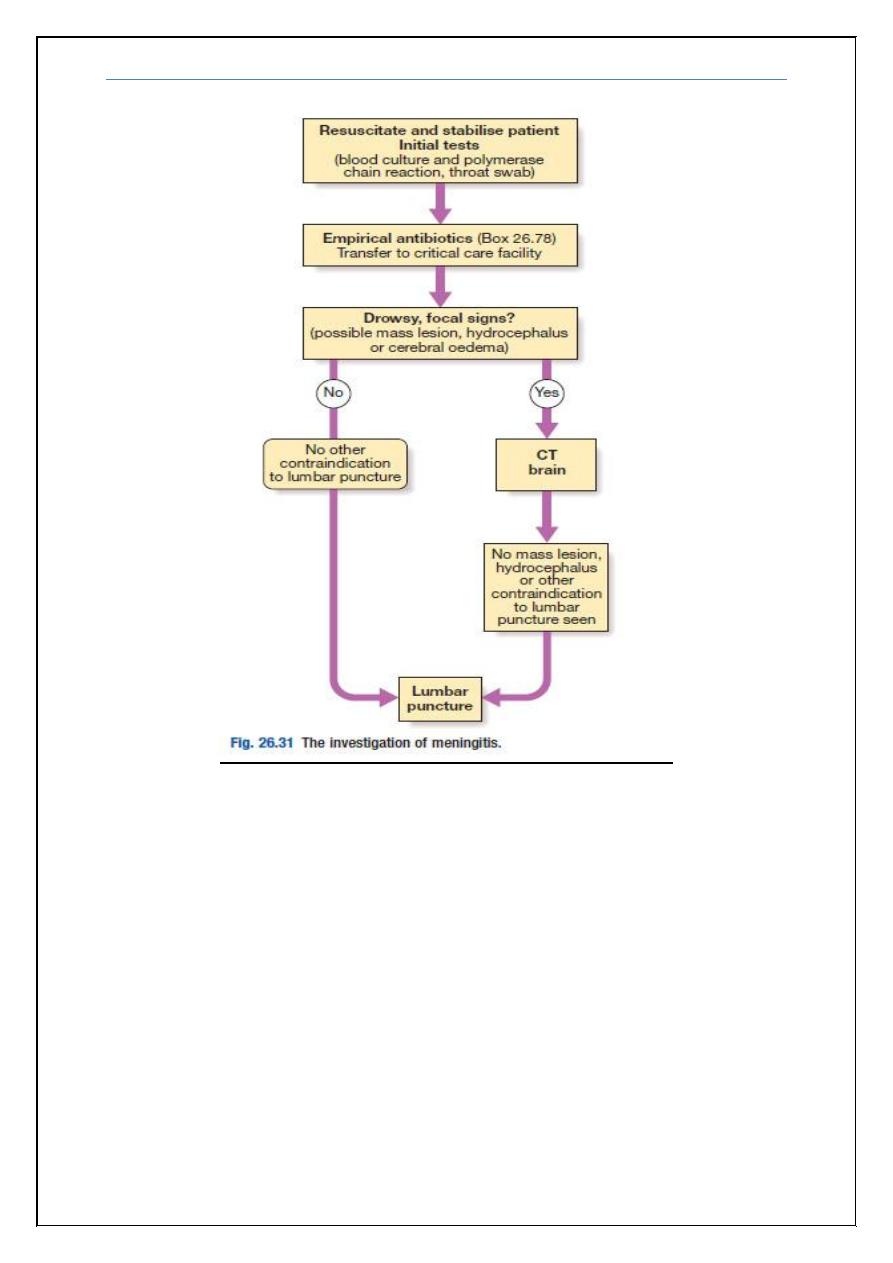
Investigations
CT head: If there is drowsiness, focal neurological signs or seizures, CT is
required prior to LP to exclude a mass lesion (there is a risk of coning and
herniation if LP is performed with raised intracranial pressure).
LP: CSF is cloudy due to neutrophils (often > 1000 × 106 cells/L).
Protein is significantly elevated and glucose is reduced. A Gram film
and culture may identify the organism.
Other: Blood cultures may be positive. PCR of blood and CSF can
identify bacterial DNA.
Central nervous system infections
Dr. Zuhair
8
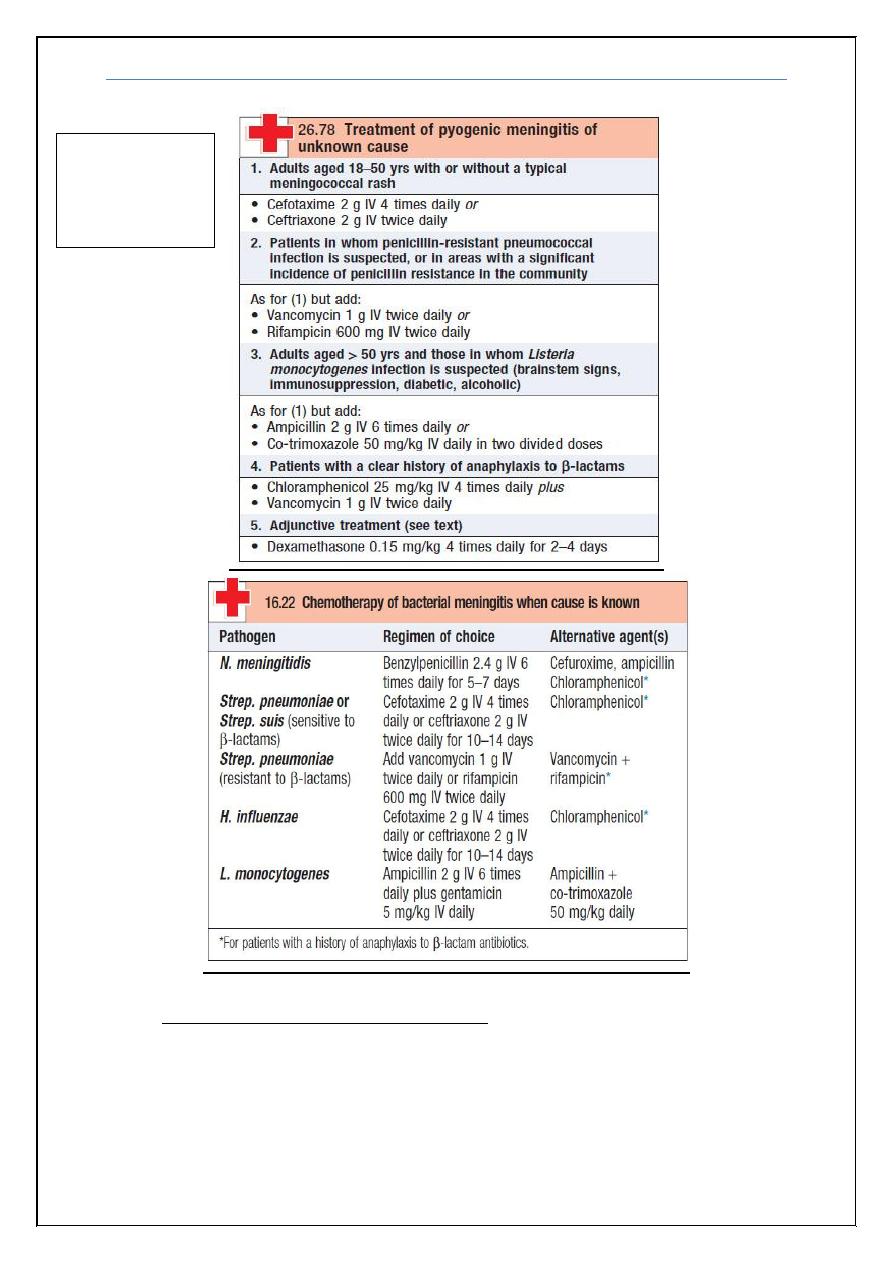
Management
If bacterial meningitis is suspected, the patient should be given parenteral
antibiotics immediately and admitted to hospital. Before the cause of
meningitis is known, patients should receive cefotaxime (2 g IV 4 times daily)
or ceftriaxone (2 g IV twice daily) (
Recommended empirical therapy before the cause of
meningitis is known is given in Box 26.78).
The antibiotic regimen may be modified after CSF examination, depending on
the infecting organism (Box 16.22).
Adjunctive corticosteroid therapy is useful in both children and adults;
Corticosteroids significantly reduce hearing loss and neurological sequelae, but
do not reduce overall mortality.
Central nervous system infections
Dr. Zuhair
9
Prevention of meningococcal infection: Close contacts of patients with
meningococcal infections should be given 2 days of oral rifampicin. In adults,
a single dose of ciprofloxacin is an alternative. If not treated with ceftriaxone,
meningitis patients should be given similar treatment to clear nasopharyngeal
carriage. Vaccines against meningococcus are available but not for the most
common subgroup (B)
No need to
memorize all the
information on
these boxes.
Central nervous system infections
Dr. Zuhair
10
CNS Parenchymal infections
Viral encephalitis
Infection of nervous tissues will produce both focal dysfunction (deficits and/or
seizures) and general signs of infection. Only a minority of patients have a
history of recent viral infection. In Europe, the most serious cause is herpes
simplex. Acute encephalitis may occur in HIV infection.
Clinical features
Viral encephalitis presents with acute onset of headache, fever, focal
neurological signs (aphasia and/or hemiplegia) and seizures. Disturbance of
consciousness, ranging from drowsiness to deep coma, supervenes early.
Meningism is common
.
Investigations
CT (which should precede LP) may show low-density lesions in the
temporal lobes.
MRI is more sensitive to early abnormalities.
CSF usually contains excess lymphocytes but is occasionally normal. The
protein may be elevated but the glucose is normal.
The EEG is usually abnormal in the early stages, especially in herpes
simplex encephalitis.
Virological investigations of the CSF may reveal the causative organism
but treatment should not await this.
Management
Herpes simplex encephalitis responds to acyclovir (10 mg/kg IV 3 times daily
for 2–3 wks). This has reduced mortality from 70% to 10%, and should be
given early to all patients with suspected viral encephalitis. Raised
intracranial pressure is treated with dexamethasone, and seizures controlled with
anticonvulsants.
Note:
there are many types of parenchymal viral infections that are rare and
not very important and can be found in
Davidson’s Principles and Practice of
Medicine 22ed
2014 or Davidson's Essentials of Medicine, 2nd Edition.
These
include:
Rabies
Poliomyelitis
Subacute sclerosing panencephalitis
Progressive multifocal leucoencephalopathy
Central nervous system infections
Dr. Zuhair
11
Bacterial encephalitis
Cerebral abscess
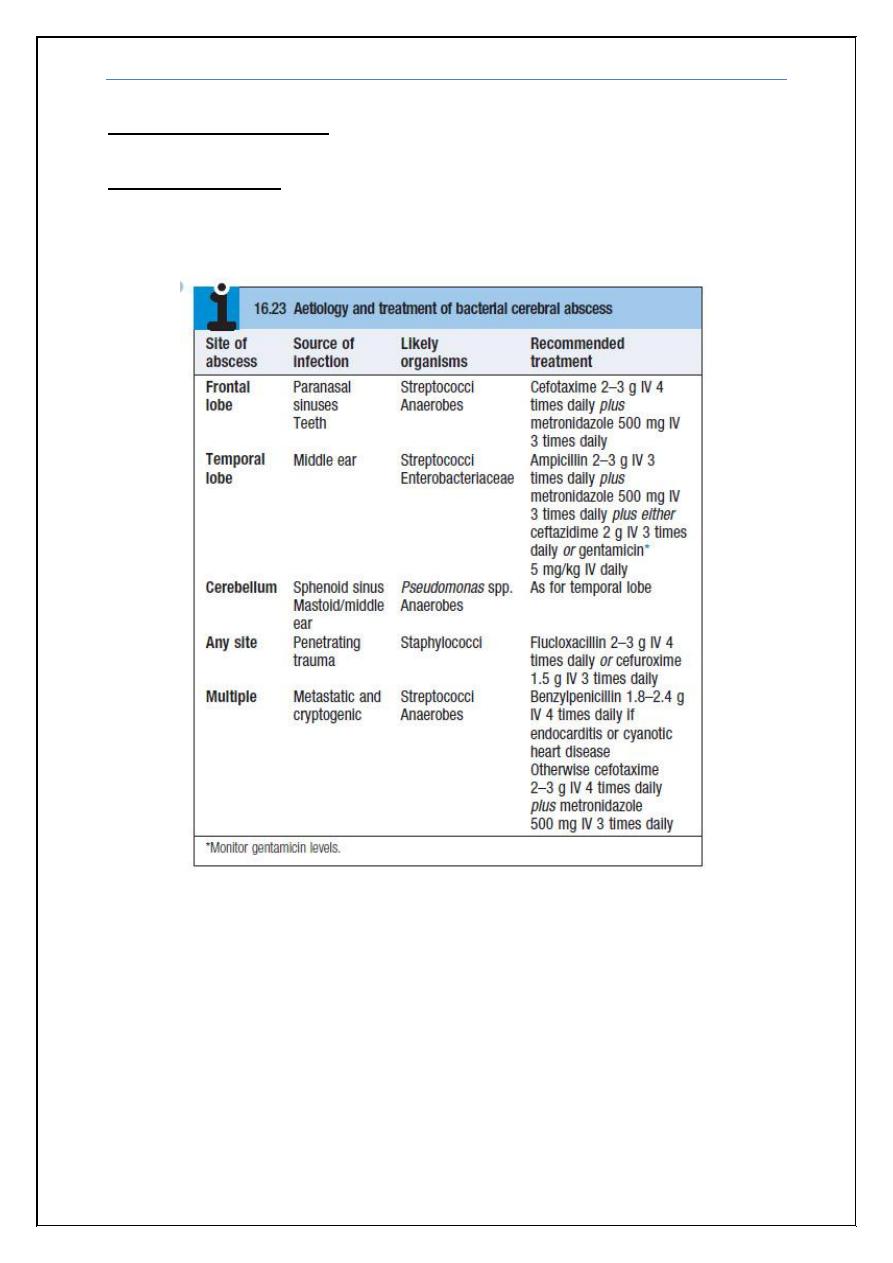
Bacteria can enter the cerebral substance in many ways. The site of abscess
formation and the causative organism are both related to the source of infection
(Box 16.23).
Clinical features
A cerebral abscess may present acutely with fever, headache, meningism and
drowsiness, but more commonly presents over days or weeks as a cerebral
mass lesion with little or no evidence of infection, making distinction from
tumour difficult. Seizures, raised intracranial pressure and focal hemisphere
signs occur alone or in combination.
Central nervous system infections
Dr. Zuhair
12
Investigations
LP is potentially hazardous in the presence of raised intracranial pressure and
CT should always precede it. CT reveals single or multiple low-density areas,
which show ring enhancement and surrounding cerebral oedema. There may be
an elevated WBC and ESR with active infection. Cerebral toxoplasmosis or
tuberculous disease secondary to HIV infection should always be considered.
Management and prognosis
Antimicrobial therapy is indicated once the diagnosis is made (see Box 16.23).
Surgical treatment by burr-hole aspiration or excision may be necessary.
Anticonvulsants are often required, as epilepsy frequently develops. The
mortality rate remains high at 10–20%.
Note:
You can review
Davidson’s Principles and Practice of Medicine 22ed
2014 or
Davidson's Essentials of Medicine, 2nd Edition
for further information on
Parenchymal bacterial infections.
Differential Diagnosis of:
Meningitis:
Subarachoid Hemorrhage
Venous Sinus Thrombosis
Encephalitis
Encephalitis
Venous Infarction
Hemorrhagive Leucoencphalitis
Meningitis
Complications:
• Hydrocephalus
• Cranial nerves palsies
• Stroke
• Dementia
• Amnesia
• Aphasias
• Venous sinus thrombosis
• Death
END
Central nervous system infections
Dr. Zuhair
13
Appendix:
Cases presented by the Dr. Zuhair
:
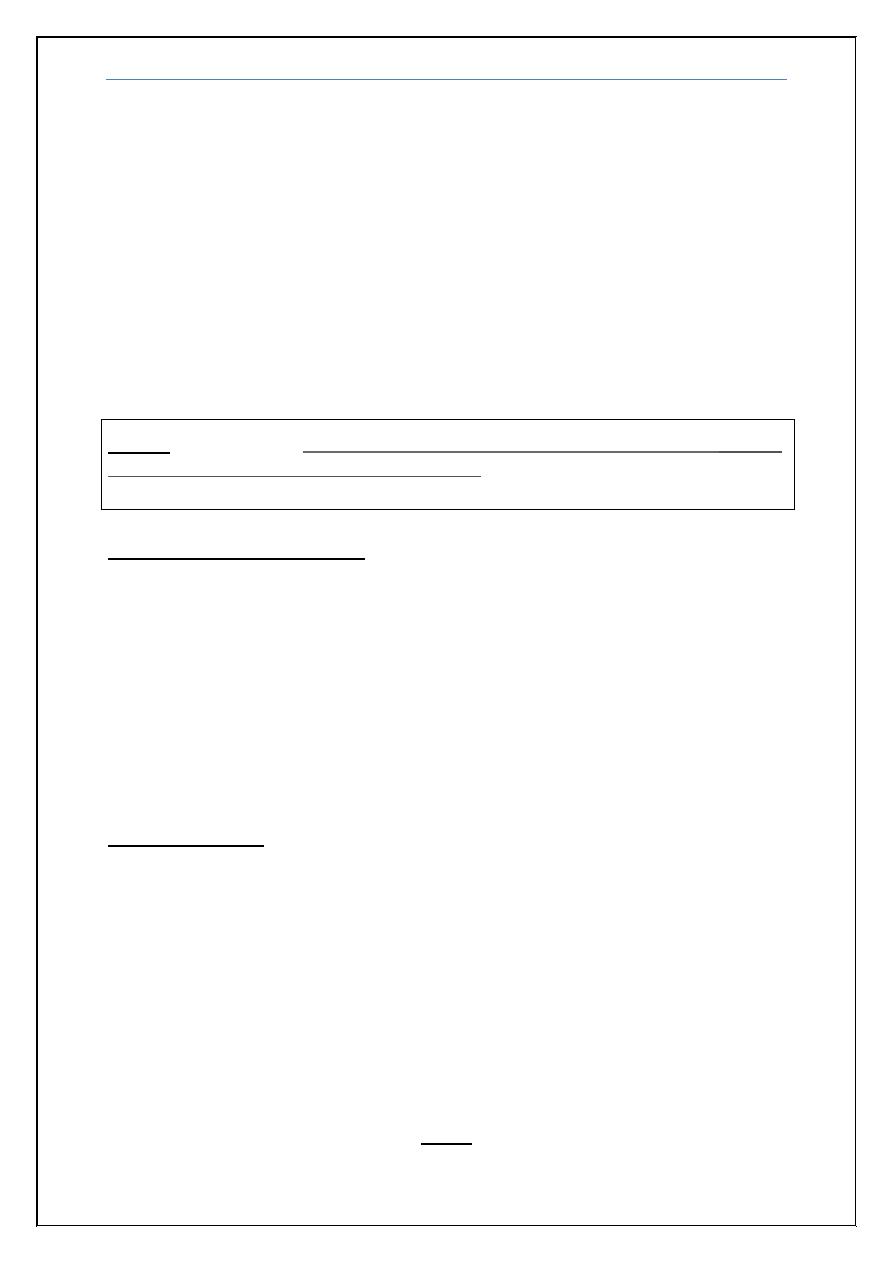
1) 10 years old boy presented with fever headache, photophobia and
vomiting of 3 days duration, was very toxic, history of similar condition
in his brother was noted, which lead to death. O/E Neck stiffness and
Kernig’s sign were positive. CSF: protein 120 mg/dl, sugar 39 mg/dl
(blood 99 mg/dl), cells: 600 WBC, 90% Neutrophils. Gram stain shown
below, also picture of his brother’s condition is shown below:
What is the most likely pathogen?
Answer: Neisseria meningitidis (also termed meningococcus)
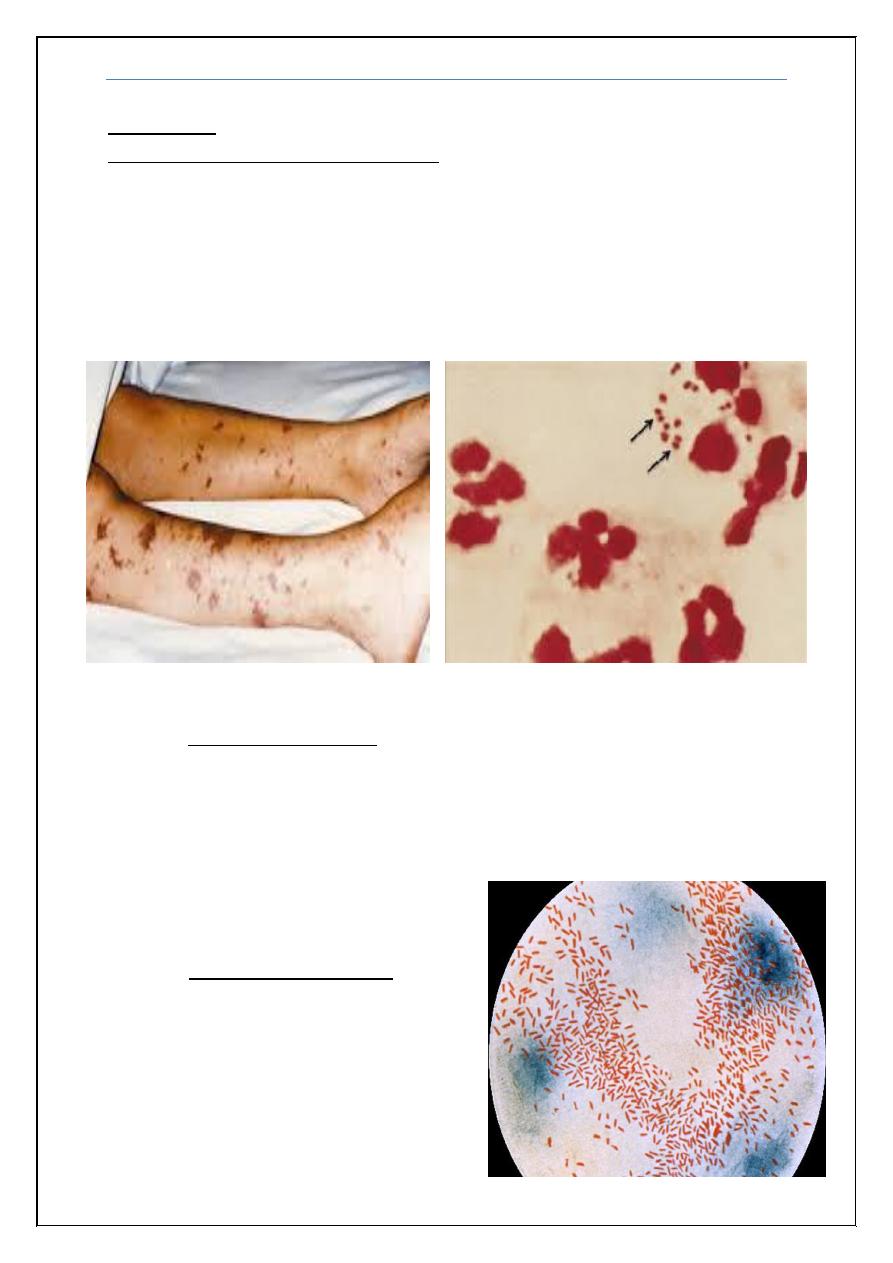
2) 5 years old boy presented with fever headache and vomiting of 3 days
duration, O/E Neck stiffness and Kernig’s sign were positive. CSF:
protein 120 mg/dl, sugar 39 mg/dl (blood 99 mg/dl), cells: 600 WBC,
90% Neutrophils. Gram stain shown below:
What is the most likely pathogen?
Answer: Haemophilus influenzae
Central nervous system infections
Dr. Zuhair
14
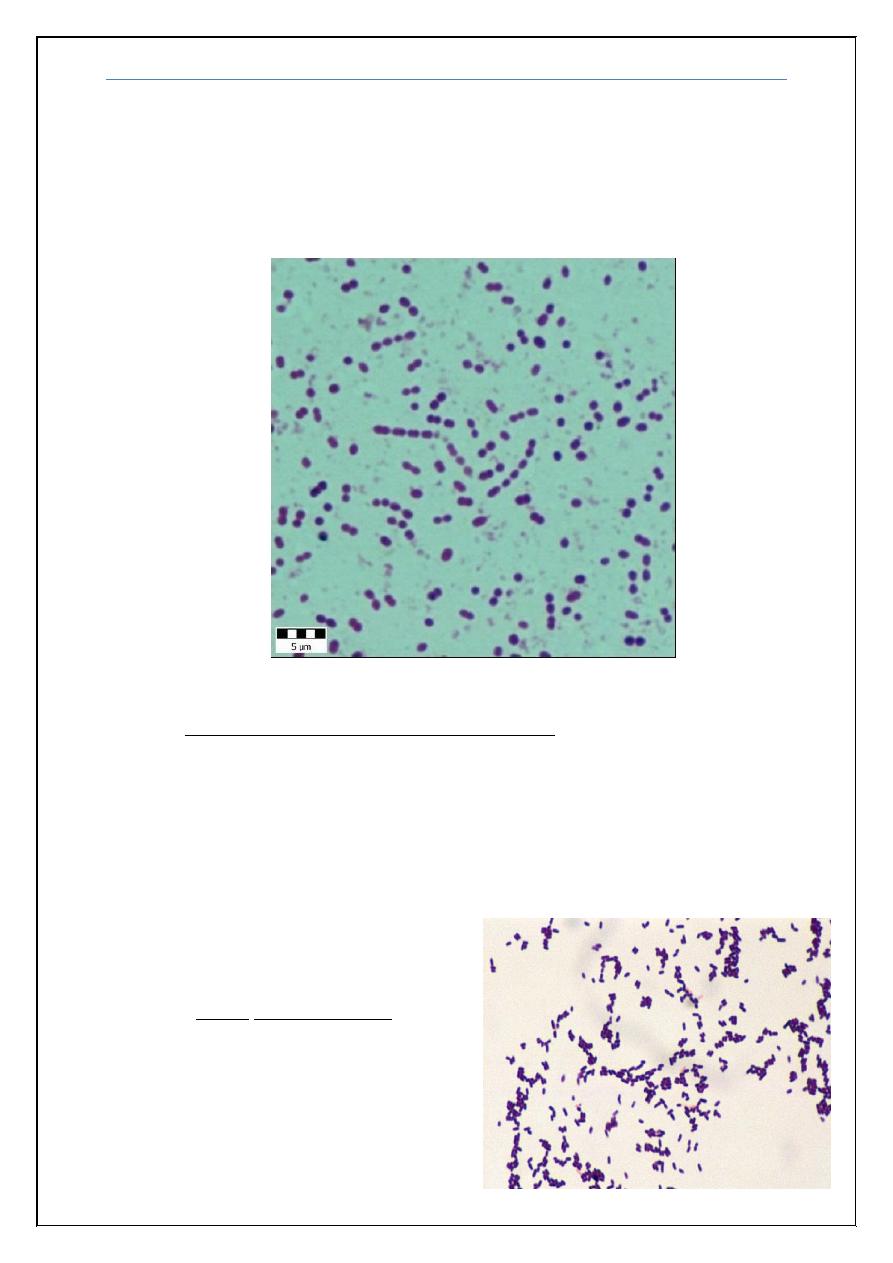
3) 35 years old man known thalasemic presented with fever headache and
vomiting of 3 days duration, O/E Neck stiffness and Kernig’s sign were
positive. CSF: protein 200 mg/dl, sugar 39 mg/dl (blood 99 mg/dl), cells:
2600 WBC, 90% Neutrophils. Had a history of splenctomy 1 year ago.
Gram stain shown below:
What is the most likely pathogen?
Answer: Pneumococcus (Streptococcus pneumoniae)
4) 30 years old pregnant lady with fever headache and vomiting of 5 days
duration, with acute onset deterioration in level of consciousnss following
a complaint of double vision.
O/E Neck stiffness and Kernig’s sign were positive. Bilateral VI, and
spastic quadriparesis. CSF: protein 200 mg/dl, sugar 39 mg/dl (blood 99
mg/dl), cells: 300 WBC, 90% Neutrophils.
What is the most likely pathogen?
Answer:
Listeria monocytogenes
Central nervous system infections
Dr. Zuhair
15
5) 17 years old girl brought to A&E with severe agitation and speaking non
sense, sustained three fits each preceded by abnormal sense of smell for
few seconds. O/E there was mild neck stiffness, Kernig sign was
negative. However she was Dilerious. CSF showed protein 67 mg/dl,
sugar normal, cells 10 WBC, all lymphocytes. Gram stain negative.EEG
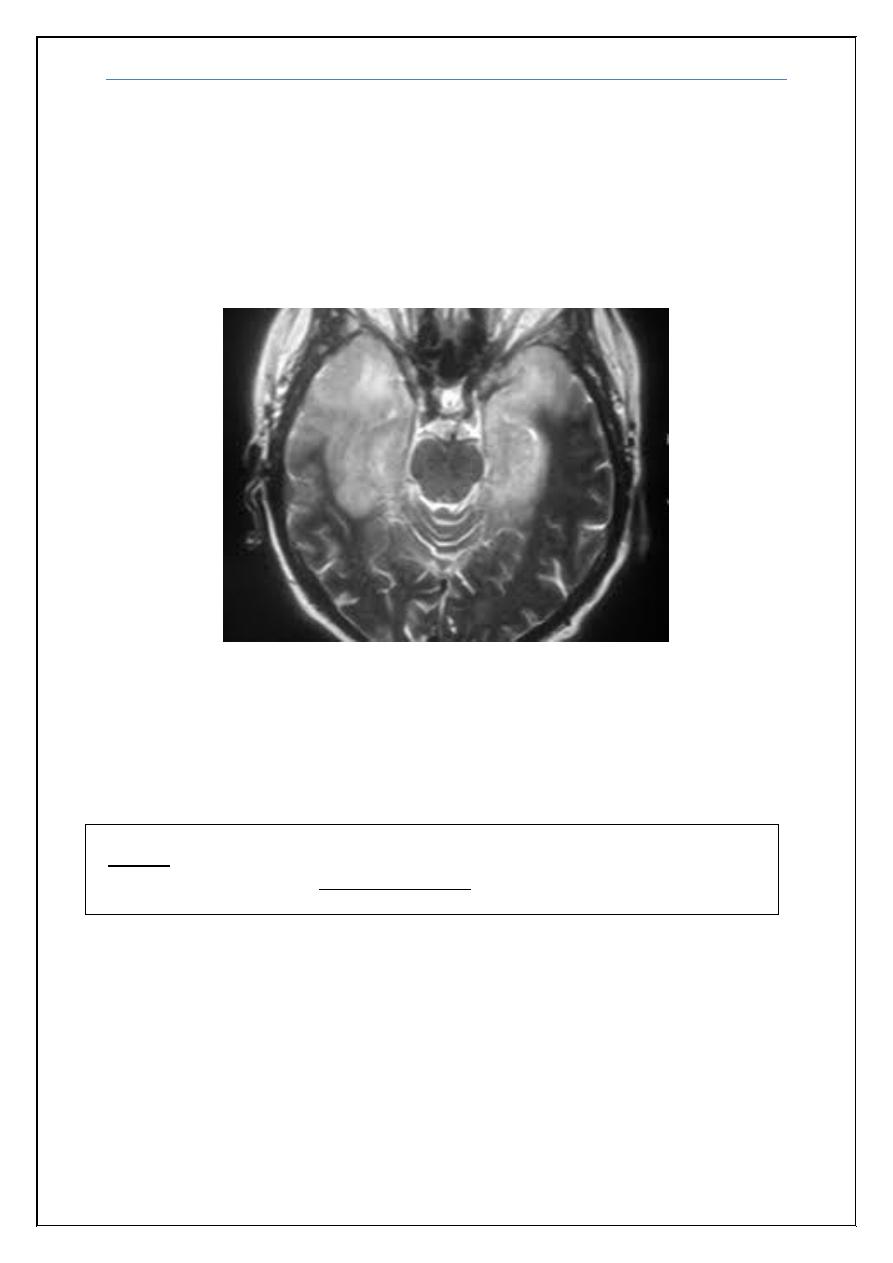
reveals bilateral temporal spikes and MRI picture shown below.
What is the diagnosis?
Answer: Bilateral inflammation of the temporal lobe diagnostic of HSV
encephalitis
Note:
there are 2 more cases with full explanation that can be found in a
separate file uploaded in muhadharaty.com.
Central nervous system infections
Dr. Zuhair
16
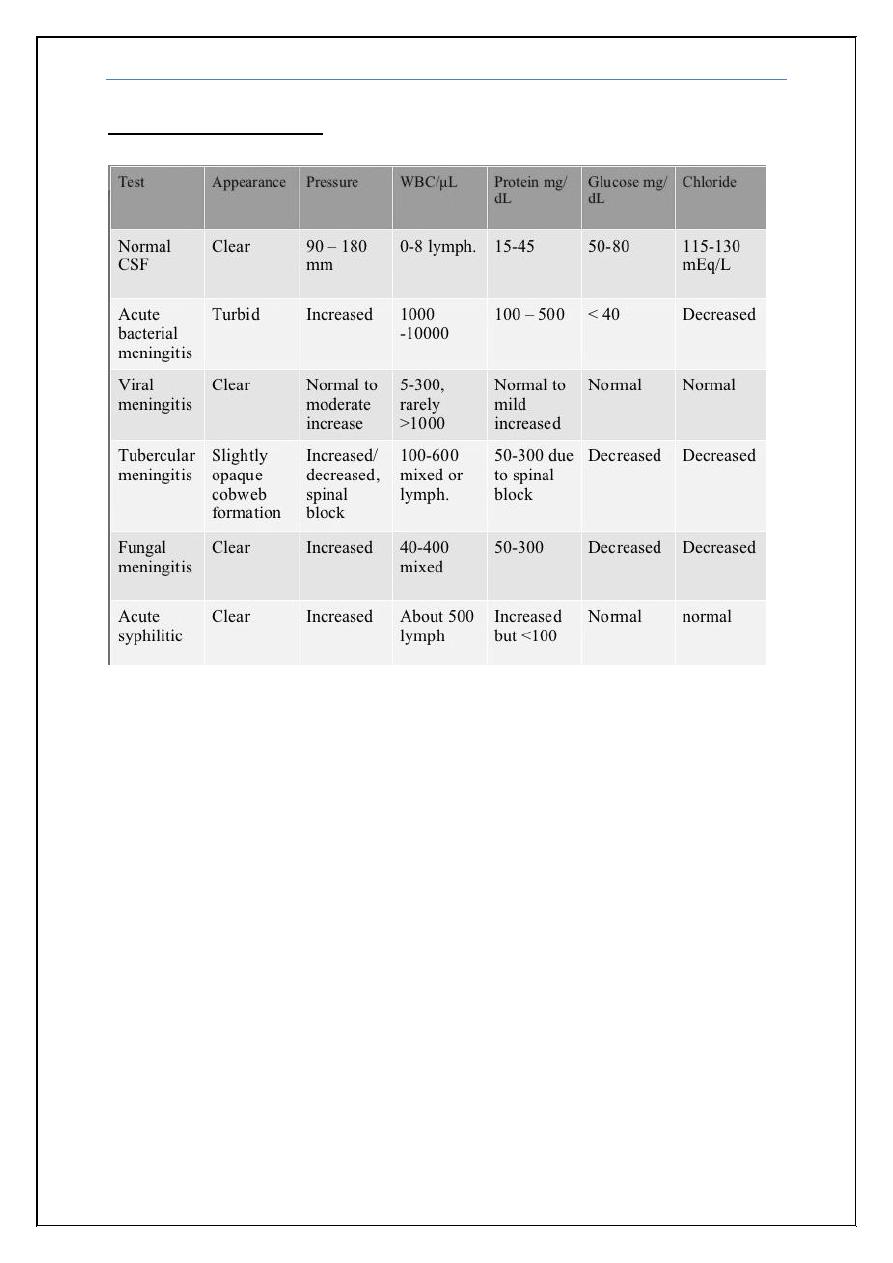
CSF analysis results:
