Forth stage
SurgeryLec-2
د.احمد أبراهيم
16/4/2016
Anal conditions IIPILONIDAL SINUS (PNS)
Pilonidal means "nest of hairs".It is an infected tract under the skin, usually between the buttocks, in the natal cleft.
Consisting of one or more, usually non infected, midline openings, which communicate with a fibrous track lined by granulation tissue and containing hair lying loosely within the lume and possibly can be oozing pus.
Anyone can develop a pilonidal sinus.
However it mainly affects people between the age of 16 and 30, common minor condition of skin overlying the sacrum.
A sinus developed after an abscess is cleared (by itself or by medical treatment), then one of more of the small openings (tracts) join the cavity to the skin surface.
Some people can develop a pilonidal sinus without ever having a pilonidal abscess.
Aetiology:-
Affect young adult males with dense, dark, strong hair.Females also affected but less than male.
Rare below 30 years.
A common affliction amongst the military, it has been referred to as ‘jeep disease’.
The exact cause is not clear, there are various theories.
Congenital Theory: -
The problem may develop from a minor congenital or hereditary abnormality in the skin of the natal cleft.
This may explain why the condition tends to run in some families.
Part of the abnormality in this part of the skin may be that the hairs grow into the skin rather than outwards.
Acquired theory :-
Is more acceptable, hair from the head and back pentrate to the skin over the sacrum and coccyx.In the presence of pressure from sitting , a rolling movement of the buttocks , sweat, and poor hygiene , the hairs are drawn through the skin to accumulate in the subcutaneous tissue with debris and M.O .
The following facts support this theory:-
P.N.S may occur in umbilicus, webs of fingers of barbers.Microscopic examination show loose hairs in the cavity but no hair follicles.
The tip of hair is always directed inward.
Liability for recurrences.
Pathology:-
Originally there is a cavity that contains loose hairs, lined by granulation tissue and lined in the subcutaneous space overlying the lower sacrum.The cavity opens on the skin in the midline by one or more openings, their tracks being partially epithelized.
Intermittently aerobes and anaerobes proliferate causing an abscess which empty through the midline opening or point and open laterally and inferiorly producing secondary sinuses.
Abscess formation has tendency to recurrence.
Clinical Features:-
Patient may be Asymptomatic.
Patient present with Local Discomfort.
Discharge.
Acute Abscess formation.
P.N.S disease tends to reoccur if not properly treated.
Differential Diagnosis:-
Perianal abscess.Anal fissure.
Treatment:-
Conservative treatmentIn those whose symptoms are relatively minor: simple cleaning out of the tracks.
Removal of all hair,
Regular shaving of the area
Strict hygiene recommended.
Pilonidal abscess:-
Incision and drainage of pus, hairs are removed and the wound is left open, packed and is allowed to heal by granulation tissue formation.
If a sinus recurs it is formally treated by exesion of the sinus.
Pilonidal sinus:-
Different options are available:-
Laying out the cavity and side tracks and curettage, wound is left open and allows healing by secondary intension.
Localized excision of the cavity and side tracks, the wound may be left open to granulate or is closed by sutures to hasten healing.
Patient should keep area clean and shave it to reduce recurrence.
Recurrent pilonidal sinus
Three possibilities account for this disappointment:Part of the sinus complex has been overlooked at the primary operation.
New hairs enter the skin or the scar.
There is persistence of a midline wound caused by shearing forces and scarring.
In this situation, revisional surgery may include re-excision followed by wound closure and obliteration of the natal cleft either by myocutaneous rotational buttock flap or cleft closure.
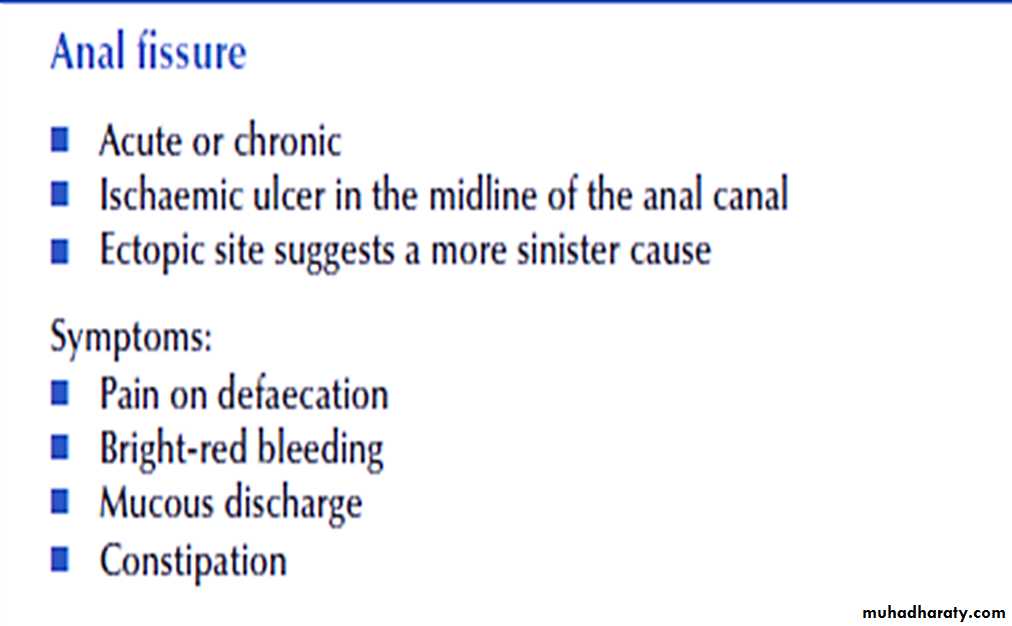
ANAL FISSURE (synonym: fissure-in-ano)
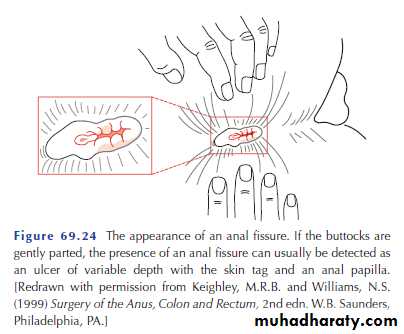
An anal fissure is a longitudinal split (ulcer) in the distal anal canal which extends from the anal verge proximally towards, but not beyond, the dentate line always in the midline .In 90 % of cases it lies in the midline posteriorly , while in the remaining 10 % the fissure is anterior .
Aetiology: -
The cause of an anal fissure, and particularly the reason why the posterior midline is so frequently affected, is not completely understood.Constipation: - hard faecal material cause injury of the posterior wall below dentate line.
Repeated passage of Diarrhoea.
Anterior fissure occur more in female due to weakness in the perineum may arise following vaginal delivery.
Rarely fissure due to Crhon’s disease.
Complication of haemorrhoids operation in which too much skin is removed. This results in anal stenosis and tearing when a hard motion is passed.
Sexually transmitted diseases.
Pathology:-
Acute fissure: -Superficial tear in the lower half of the anal canal in the mid line usually posteriorly, pain lead to spasm of internal sphincter muscle which prevents its healing.
Chronic fissure: -
If acute fissure not treated properly, chronic fissure with changes include:-The margin becomes indurated.
Fibrosis leads to narrowing of anal canal.
Anal papilla may develop at the upper end of the fissure.
Skin tage may form at the lower end called sentinel pile.
Anal suppuration leads to abscess and fistula formation.
And chronicity may result from repeated trauma, anal hypertonicity and vascular insufficiency, either secondary to increased sphincter tone.
Clinical Features:-
Although most sufferers are young adults, the condition can affect any age, from infants to the elderly. Men and women are affected equally.
Pain: sharp start during defecation and continue then relieved after few hours, remission for few days or weeks then pain recurs.
Bleeding: streaks of blood around the stool.
Constipation: - due to pain patient postpone defecation.
Slight anal discharge:
May be present, secondary to irritation from the sentinel tag, discharge from the ulcer or discharge from an associated intersphincteric fistula, which has arisen through infection penetrating via the fissure base
Reflex symptoms:
Commonly present burning micturation, dysmenorrhoea and pain along thighs.
Examination: -
Acute fissure:Inspection reveals tightly contracted anal verge, contracted, puckered anus.
Small tear seen in the midline.
It is very painful and in advisable to do digital rectal examination.
Chronic fissure:-
Indurations of the edge.Anal papilla or a sentinel pile may be present.
Examination done using anesthetic gel.
DDx:-
A fissure sited elsewhere around the anal circumference or with atypical features should raise the suspicion of a specific aetiology, and failure of adequate examination in the clinic should prompt early examination under anaesthesia,
Early carcinoma of the anus.
Fissures due to Crohn’s disease, multiple, not indurated, not very tender.
T.B ulcers have undermined, cyanotic edges.
Anal chancre present as painful ulcer.
In any atypical presentation histopathology of the excised specimen should be performed.
Treatment:-
Acute fissure:-
Aim of treatment is to relieve the persistent spasm of internal sphincter to give chance for the fissure to heal.
Treatment is medical but surgery might be needed.
High fiber diet and some laxative to ensure bulky soft stool.
Local anesthetic 2% or 5% lignocaine .
Recently Glyceryl trinitrate ointment 0.2%applied four times per day to the anal margin (although this may cause headaches) and diltiazem 2% applied twice daily.
Analgesic.
Warm water bath.
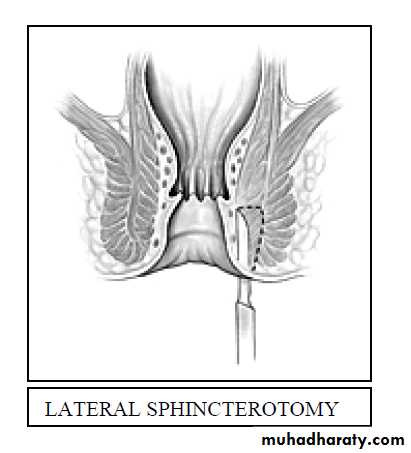
If no improvement internal sphinctrotomy under G .A.
Chronic fissure:-
1- If not very chronic, a lateral internal sphinctrotomy operation is very successful.
2- If the fissure is heavily fibrosed with a sentinel pile, the best procedure Fissurectomy with posterior internal sphinctrotomy.
3- Anal flap
excision of the edges of the fissure and, if necessary, its base overlying the internal sphincter, an inverted house-shaped flap of perianal skin is carefully mobilised with its blood supply and advanced without tension to cover the fissure, and then sutured with interrupted absorbable sutures.The patient is maintained on stool softeners and bulking agents postoperatively, and usually also on topical sphincter relaxants; minor breakdown of one anastomotic edge does not mean failure