1
Baghdad medical college 2015 - 2016
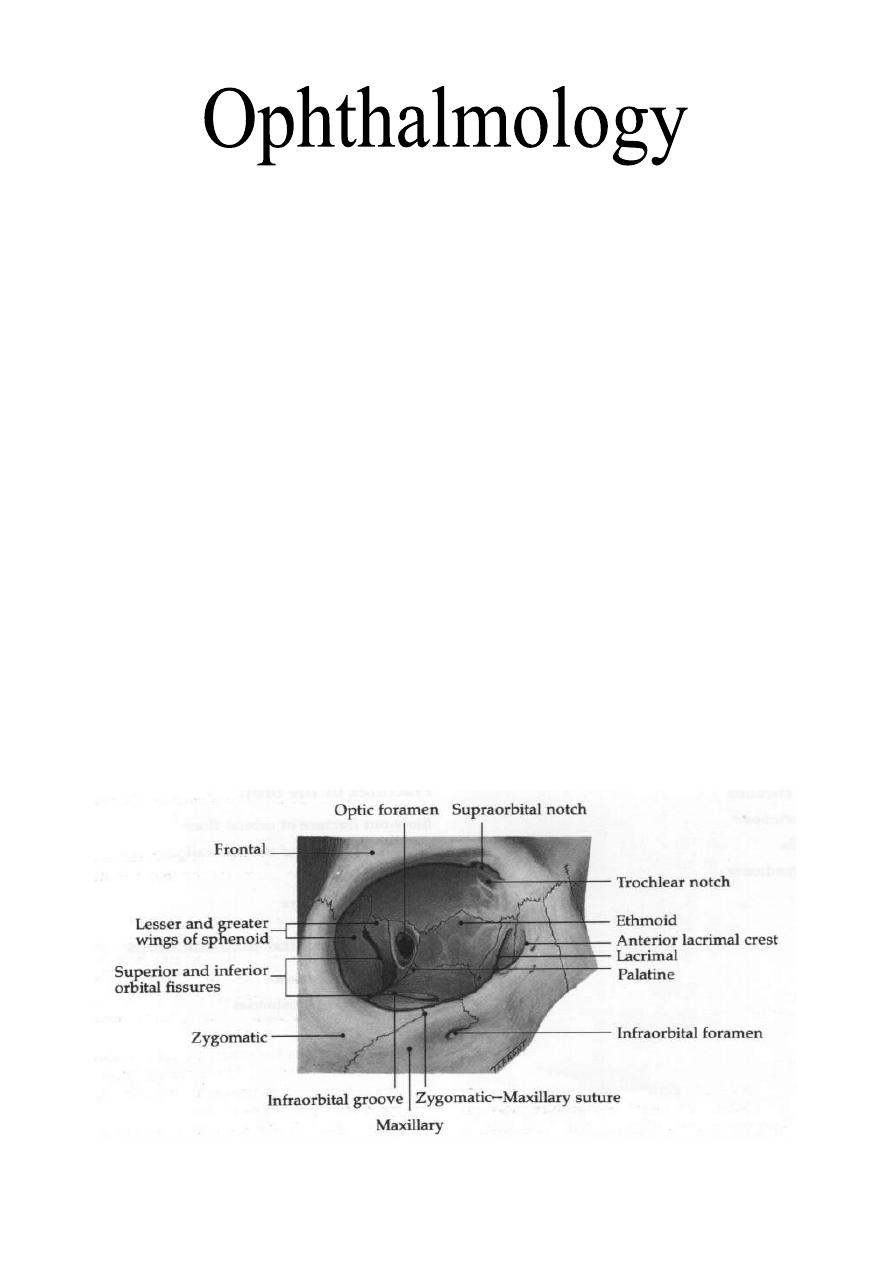
The Orbit
The anatomy of the orbit
The orbit is a pear-shaped cavity, the stalk of which is the optical canal
through which the optic nerve pass from the orbit to the anterior cranial fossa.
1- The Roof: it is made of two bones; the lesser wing of sphenoid and the
orbital plate of the frontal bone, located subjacent to the anterior cranial fossa
and frontal sinus. A defect in the orbital roof (that occurs in some diseases
like neurofibromatosis) may cause pulsatile proptosis due to transmission of
CSF pulsation (that gets its pulsation from the pulsation of the intra cranial
parts of internal carotid arteries).
2- The Lateral Wall: it is made of two bones; the greater wing of the
sphenoid and zygomatic bone. It protects only the posterior half of globe, and
the anterior half is uncovered, that is why the eyeball liable for trauma
laterally.
3- The Floor: it is made of three bones; the zygomatic, maxillary (both form
the anterior 2/3) and palatine (forms posterior 1/3) bones. The posteromedial
portion of maxillary bone is weak liable for fracture and may be involved in a
blowout fracture.
4- The Medial Wall: It is made of four bones; the maxillary (frontal process),
lacrimal, ethmoid and the body of sphenoid. Lamina papyracea covers the
medial wall is a paper-thin and perforated by foramina for nerves and blood
vessels. Orbital cellulitis is therefore commonly occurs secondary to
ethmoidal sinusitis.
Dr. Najah
Lecture : 22 & 23
2
Clinical signs of orbital disease
1- Soft tissue involvement:
a- Signs:
i- Lid and periorbital oedema.
ii- Ptosis: Mechanical ptosis due to swelling of lid.
iii- Conjunctival chemosis (oedema) and conjunctival injection.
b- Causes:
i- Thyroid eye disease.
ii- Orbital cellulitis.
iii- Inflammatory orbital disease.
iv- Arterio-venous shunts.
2- Proptosis:
Abnormal forward displacement of the globe caused by retro-bulbar lesion or
less frequently by shallow orbit which is usually congenital. Diagnosis of
proptosis by inspection from above and behind is difficult especially if it is
bilateral.
a- The direction of proptosis: it is either axial or eccentric (upwards,
downwards, medial or lateral). An intraconal mass, e.g. cavernous
haemangioma and optic nerve glioma, will push the eyeball axially. However,
an extraconal mass will cause eccentric proptosis.'
b- The severity of proptosis: is usually evaluated either by simple plastic
ruler (placed at the lateral margin to measure the position of the apex of
cornea), or by Hertel exophthalmometer (a plate attached to it 2 mirrors
placed at 45°). Normally, the apex of the cornea is up to 20 mm anterior to
lateral orbital margin, and anything more than 21 mm is considered proptosis,
which is divided according to severity into:
- Mild: 21-23mm.
- Moderate: 24-27mm.
- Severe: >28mm.
proptosis diagnosed by inspection.
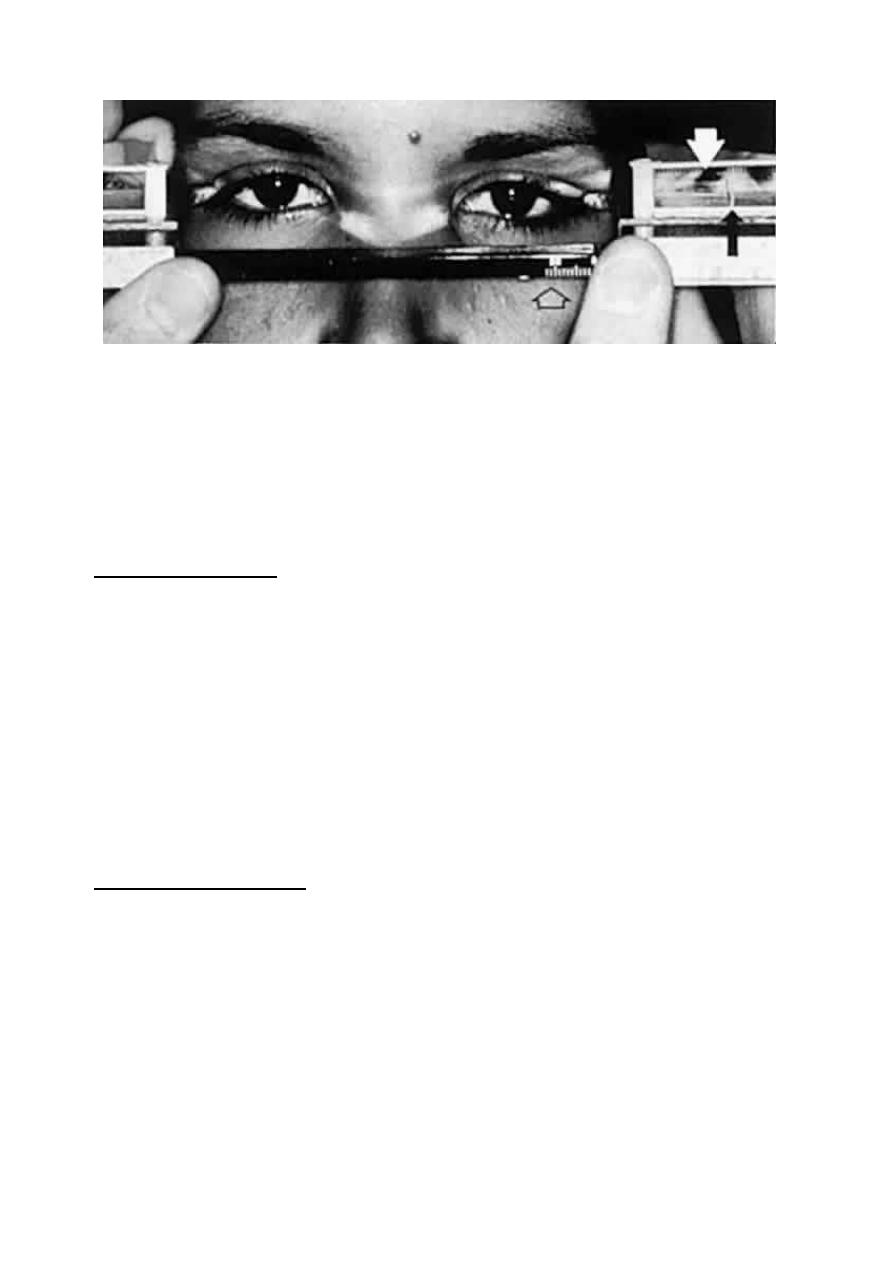
3
Exophthalmometry with Hertel instrument. White arrow indicates cornea of left eye as
viewed through right-angle prism. Black arrow indicates mires fixed at 18 mm. Open
arrow indicates baseline gauge. Note position of footplates placed against lateral orbital
rims.
c- Exclude pseudo-proptosis: As in ipsilateral lid retraction, contralateral
enophthlamos, enlargement of eyeball in unilateral high myopia and
buphthalmos.
3- Enophthalmos:
The globe is recessed within the orbit. Causes:
a- Small globe, congenital anomaly, e.g. microphthalmos or nanophthalmos.
b- Structural bony abnormalities, blowout fracture of floor or lamina
papyracea that causes herniation of orbital fatty tissue causing enophthalmos,
congenital bone defects is another cause for enophthalmos.
c- Atrophy of orbital contents, after radiotherapy in malignant tumors of the
orbit or trauma.
d- Cicatrizing orbital lesions, such as chronic sclerosing inflammatory orbital
disease, secondary malignancy or carcinoma of orbit causing fibrosis of
intraorbital structure and traction of eyeball.
4- Ophthalmoplegia:
defective ocular motility, caused by:
a- Orbital mass: Due to large intraorbital mass, there will be restriction of
movement to one side or another.
b- Restrictive myopathy in thyroid diseases.
c- Ocular motor nerves lesions: damage to 3
rd
, 4
th
or 6
th
cranial nerves.
d- Tethering of extraocular muscles or fascia in a blowout fracture: herniation
of muscles or tethering (entrapment) of these muscles in the fracture.
e- Splinting of optic nerve by optic nerve sheath meningioma.
4
5- Visual dysfunction (reduced visual acuity):
a- Exposure keratopathy.
b- Compressive optic neuropathy.
c- Choroidal folds at macula.
6- Dynamic properties:
a- Increasing venous pressure: by dependant head posture, valsalva
maneuver, jugular compression, during the crying of the child, there is
enlargement of the size of the mass. This is
seen in venous anomalies, cavernous and
capillary haemangiomas.
b- Pulsation: It is caused by either A-V
communication or herniation of meninges
with CSF from the anterior cranial fossa
through a defect in the orbital roof.
c- Bruit: it is a sign of carotid-cavernous
fistula.
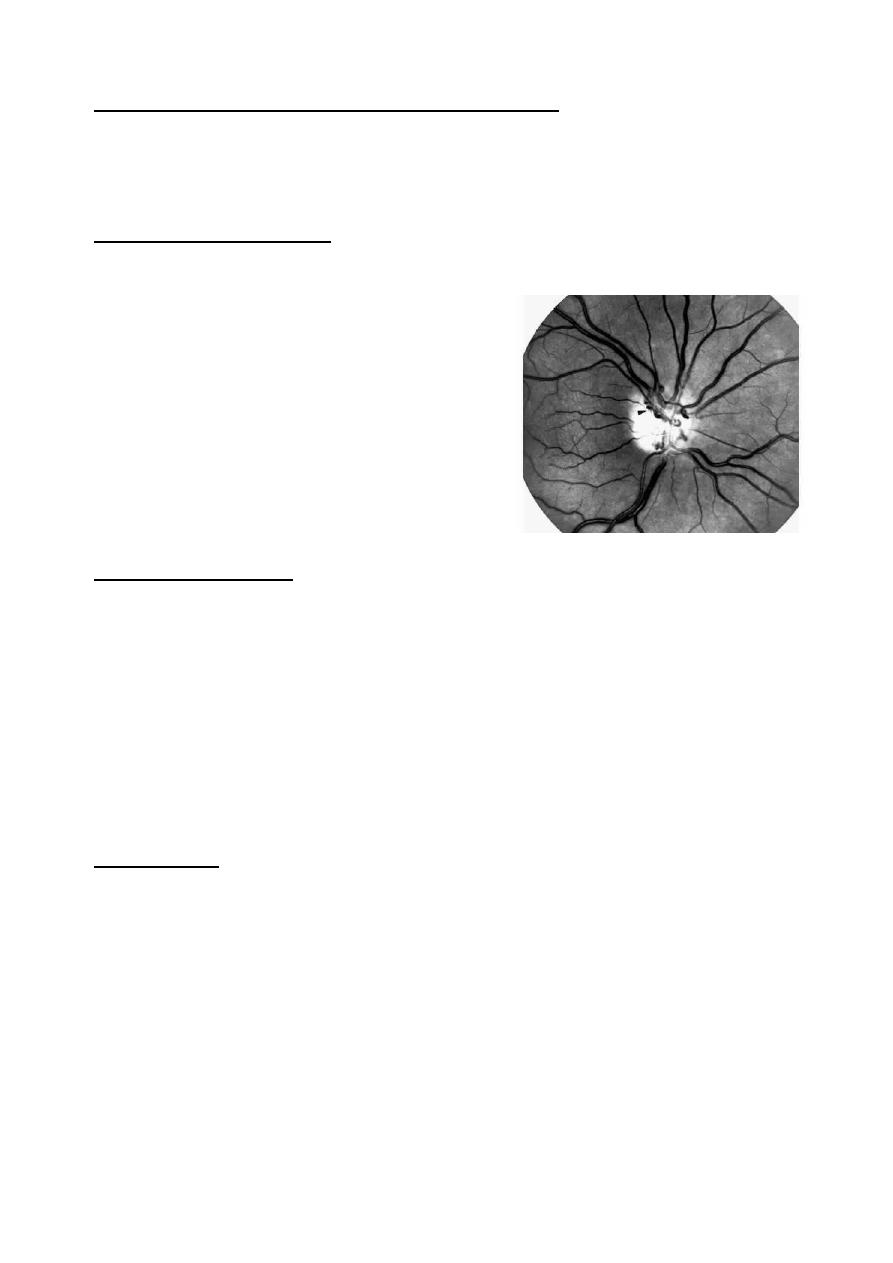
7- Fundus changes:
a- Optic disc atrophy. Caused by inflammation or compressing on the optic
nerve.
b- Optociliary shunt; Optociliary veins can be seen only when there is
central retinal vein occlusion; so these vessels shunting the blood from the
retina to the choroidal venous circulation. Common tumors associated with
this shunt are optic nerve sheath meningioma and glioma.
c- Choroidal folds (tumors, Thyroid ophthalmopathy).
d- Retinal vascular changes (venous dilatation, tortuosity, swollen disc and
vascular occlusions).
8- Dystopia:
Displacement of the eyeball across the coronal plane of orbit, as in case of
tumor of lacrimal gland, that is situated between the roof and the lateral wall,
which will lead to displacement of the eyeball downwards and medially. The
degree of displacement can be measured by a ruler whether horizontal or
vertical.
Investigation:
CT, MRI (contraindicated in case of metallic foreign bodies), Plain X-Ray,
and fine needle biopsy (FNB) under guidance of CT especially in orbital
metastasis.

5
Orbital infection
1- Preseptal cellulitis:
It is relatively common infection of subcutaneous tissue anterior to the
orbital septum.
Causes:
a- Skin trauma, lacerations or insect bites. Organism is usually
staphylococcus aureus or streptococcus pyogenes.
b- Spread of local infection; such as dacryocystitis and acute hordeolum
(internal or external).
c- From remote infection: of the upper respiratory tract infection or middle
ear infection by hematogenous spread.
Signs:
Unilateral, tender, red periorbital and lid swelling, proptosis is absent, visual
acuity and pupillary reaction and ocular motility are normal (to differentiate it
from orbital cellulitis).
Treatment:
Oral co-amoxiclav 250mg is given every 6 hours. Severe infections are
requiring IM benzyl penicillin 2.4 - 4.8mg in four divided doses and oral
flucloxacillin 250-500mg every 6 hours in addition to topical antibiotic in
forms of drop and ointment. (e.g. Gentamycin or chloramphenicol)
2- Bacterial orbital cellulitis:
An infection of the soft tissues behind the orbital septum, it is a
polymicrobial infection including anaerobes, streptococcus pneumonia,
staphylococcus aureus and streptococcus pyogenes, and in children under 5
years, haemophilus influenza may be included.
Causes:
a- Sinus-related: The most common one is ethmoidal sinusitis (as there is
only the thin plate in between "lamina papyracea".
b- Extension of Preseptal cellulitis.
c- Spread from adjacent dacryocystitis, mid-facial and dental infection.
d- Post-traumatic: Develops within 72 hours of injury that penetrates the
orbital septum.
e- Post-surgical: May complicates retinal, lacrimal or orbital surgery.
f- Haematogenous spread.
Clinical features:
Occur at any age but more common in children (as they are more prone to
develop upper respiratory tract infection), patient usually presented with severe
malaise, fever, pain and visual impairment.
Signs:
a- Swollen, tender, red and warm lids (unilateral).

6
b- Proptosis.
c- Painful ophthalmoplegia (may cause diplopia).
d- Signs of optic nerve dysfunction (seen in advanced cases).
Complications:
a- Ocular: Exposure keratopathy (due to proptosis), increased intraocular
pressure (due to pressure from outside), central retinal vein occlusion CRVO,
central retinal artery occlusion CRAO (also due to external pressure).
and optic neuritis (infection).
b- Intracranial: They are rare like; meningitis, brain abscess and cavernous
sinus thrombosis.
c- Orbital abscess.
Management:
a- Hospitalization: It is mandatory as the infection is life threatening.
b- Antibiotics: - IV Ceftazidine 1g x 3.
- IV Metronidazole 500mg x 3.
- IV Penicillin (or vancomycin).
* We must use triple antibiotics (for anaerobes, G+ve and G-ve)
c- Optic nerve function: should be monitored every four hours:
i- Light pupillary reaction.
ii- Visual acuity.
iii- Color vision.
iv- Light brightness appreciation.
d- Investigations:
i- WBC count.
ii- Blood culture (to exclude Haematogenous spread and septicemia).
iii- CT of the orbit, sinuses and brain. It is used to differentiate Preseptal
from orbital cellulitis.
iv- Lumbar puncture: if meningeal or cerebral signs develop.
e- Surgical intervention: should be considered in:
i- Unresponsiveness to antibiotics.
ii- ↓ visual acuity.
iii- Orbital abscess.
iv- Atypical picture, which may merit diagnostic biopsy.
* Surgery is done to drain abscess or decompress the walls of orbit to decrease
pressure on optic nerve.
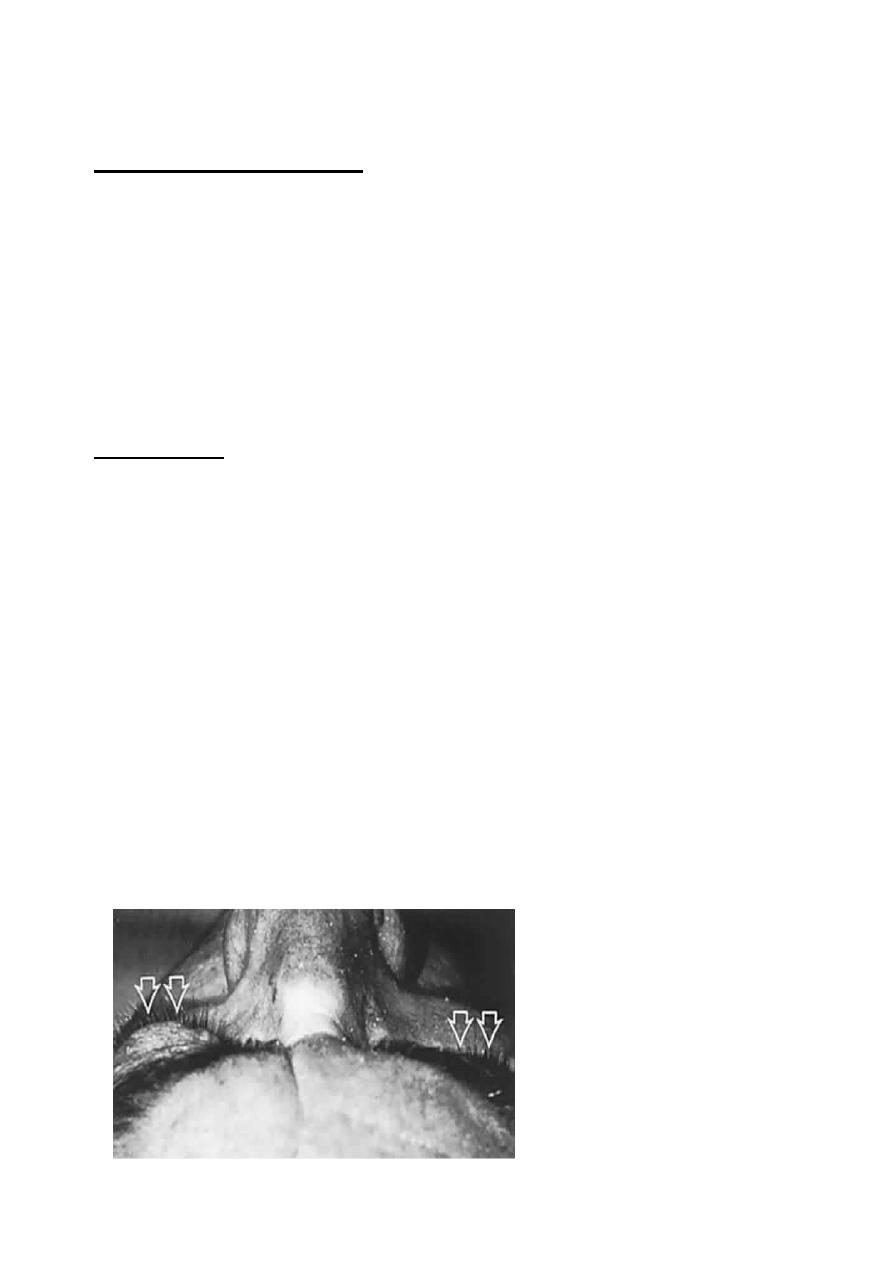
3- Rhino-orbital mucormycosis:
It is an opportunistic infection caused by fungi of the family mucoraceae,
which
typically
affects
patients
with
diabetic
ketoacidosis
or
immunosuppression.

7
This aggressive and fatal infection is acquired by the inhalation of spores,
which give rise to upper respiratory tract infection. The infection then spreads
to the sinuses, orbit and brain.
Invasion of blood vessels by the hyphae results in occlusive vasculitis with
ischemic infarction of orbital tissues.
Presentation:
Gradual onset facial and periorbital swelling, diplopia (due to
ophthalmoplegia) and visual loss.
Signs:
- Ischemic infarction superimposed on septic necrosis is responsible for the
black eschar which may develop on the hard palate, turbinate, nasal septum,
skin and eyelids
- Ophthalmoplegia.
- Progression is slower than in orbital cellulitis.
Treatment:
a- IV amphotericin.
b- Daily irrigation of involved area with amphotericin.
c- Wide excision of necrotic tissue.
d- Hyperbaric O2.
e- Exenteration (in severe unresponsive cases).
Orbital inflammatory diseases
1- Idiopathic orbital inflammatory disease IOID (Orbital pseudo
tumor):
Non-neoplastic,
non-infectious,
space
occupying
orbital
lesions,
inflammatory process may involve any or all soft tissue components of the
orbit. In adults, unilateral involvement is the rule, while in children; there is
bilateral involvement in 30% of cases.
Clinical features:
Presentation is usually at 20-50 years old with abrupt painful onset, usually
unilateral.
Signs:
a- Periorbital swelling, chemosis and Conjunctival inflammation.
b- Proptosis.
c- Painful ophthalmoplegia.
d- Due to pressure effect, Optic nerve dysfunction (impaired visual acuity,
color vision, visual field, diminished light brightness appreciation).
Clinical course:
- Spontaneous remission after a few weeks.
- Prolonged intermittent episodes of activity with eventual remission (on/off).

8
- Severe prolonged inflammation leading to fibrosis of orbital tissues
"Frozen orbit".
Management:
- Systemic steroids: effective in 50-75%, we use oral 60-80mg Prednisolone.
- Radiotherapy: if there is no response to systemic steroids.
- Cytotoxic drugs: cyclophosphamide 200 mg/day.
- Biopsy may be needed in persistent cases (to exclude other differential
diagnoses).
Differential diagnosis:
a- Bacterial orbital cellulitis.
b- Severe acute thyroid eye disease (TED).
c- Systemic disorders (Wegener's granulomatosis, polyarthritis nodosa).
d- Malignant orbital tumors.
e- Rupture dermoid cyst.
2- Acute dacryoadenitis:
Is inflammatory process involving the lacrimal gland, which occurs in about
25% of IOID. More commonly, it occurs in isolation.
It usually resolves spontaneously and does not require treatment.
Presentation:
Is acute discomfort in the region of the lacrimal gland (upper lateral part of
orbit).
Signs:
- Swelling of lacrimal aspect of the eyelid causing ptosis (mechanical ptosis).
- Mild downward and inward dystopia.
- Tenderness over the gland.
- Injection of the palpebral portion of the lacrimal gland and adjacent
conjunctiva.
- Decreased lacrimal secretion.
Differential diagnosis:
a- Infection of the lacrimal gland.
b- Ruptured dermoid cyst.
c- Malignant tumors of the lacrimal gland.
9
Thyroid eye diseases
Thyrotoxicosis (Graves' disease):
- It is an autoimmune disorder.
- Usually presents in the 3
rd
-4
th
decades of life.
- Affects women more than men.
- It is the most common cause of unilateral and bilateral proptosis.
The occurrence of signs of Graves' disease in a patient who is not clinically
hyperthyroid is referred to as euthyroid or ophthalmic Graves' disease.
Pathogenesis:
1- Inflammation of extraocular muscles (pleomorphic cellular infiltration,
increase secretion of glycosaminoglycans and osmotic imbibitions of water)
causes muscles enlargement up to 8 times and may compress the optic nerve.
Subsequently, muscles degeneration occurs and eventually leads to
fibrosis
which exerts a tethering effect on the involved muscle, resulting in restrictive
myopathy and diplopia.
2- Inflammatory cellular infiltration with Lymphocytes, plasma cells,
macrophages and mast cells of interstitial tissues, orbital fat and lacrimal
glands associated with accumulation of glycosaminoglycans and retention of
fluid. This causes increase in the volume of orbital contents and secondary
elevations of intraorbital pressure, which may itself cause further fluid
retention within the orbit.
Clinical manifestations:
There are two stages in the development of the disease:
1- Congestive (inflammatory or acute) stage:
The eyes are red and painful. This stage leads to remit within 3 years.
2- Fibrotic (quiescent) stage:
The eyes are white, painless and motility defects are present.
There are mainly five clinical manifestations:
1- Soft tissue involvement.
2- Lid retraction. 3- Proptosis. 4- Optic neuropathy. 5- Restrictive myopathy.
1- Soft tissue involvement:
Symptoms:
Grittiness, photophobia, lacrimation and retrobulbar discomfort.
Signs:
- Periorbital and lid swelling.
- Conjunctival and episcleral hyperaemia.
- Chemosis.
- Keratoconjunctival sicca (due to lacrimal gland involvement).
- Superior limbic keratoconjunctivitis.
11
Management:
a- Topical lubricant: e.g. artificial eye drops, for superior limbic
keratoconjunctivitis, corneal exposure (proptosis) and dryness.
b- Head elevation: to decrease periorbital oedema.
c- Taping of the eyelids: during sleep to prevent exposure keratopathy.
2- Lid retraction:
Retraction of upper and lower lids occurs in about 50% of patients with
Graves' disease. (It is something differs from lid lags. What is lid lags?)
Pathogenesis of lid retraction:
a- Fibrotic contracture of the levator palpebrae superioris (for upper lid) and
inferior rectus (for lower lid) is one cause for lid retraction. Usually the
upper lid covers 2mm below the superior limbus and the lower lid lies at the
lower limbic margin, when the lids are away from these sites and there is
appearance of sclera between lid margin and limbus called lid retraction.
b- Overaction of levator-superior rectus complex due to fibrosis and
tethering of the inferior rectus muscle. The first (& most common) muscle
involved is the inferior rectus, so the superior rectus try to compensate for
overactivity of inferior rectus, but as there is a complex between super rectus
and levator palpebrae superioris (both lies in a common sheath), this will
cause contraction of the levator muscle and elevation of the upper lid.
c- Overaction of Muller muscle due to sympathetic overstimulation
secondary to high level of thyroid hormones.
Signs:
- The upper lid margin is either at level with or above the superior limbus
(allowing the sclera to be visible).
Treatment:
Mild cases usually resolve spontaneously specially if there is good control of
hyperthyroidism.
Surgical correction is indicated only with significant and stable retraction.
3- Proptosis:
It is axial (as all muscles, intraorbital tissues and fat are involved), unilateral
or bilateral, symmetrical or asymmetrical and frequently permanent.
Management:
a- Systemic steroids: in rapidly progressive and painful proptosis.
- Initially; we start with 60-80 mg oral Prednisolone.
- IV methyl Prednisolone (o.5 gm. in 200 ml saline over 30 min) which may
be repeated after 48 hours. It is indicated if there is compressive optic
neuropathy (at the annulus of Zinn, muscular enlargement leads to
compression of optic nerve).
11
b- Radiotherapy: when steroids are contraindicated or when there is
compressive optic neuropathy or to prevent it.
c- Combined therapy (Irradiation, azathioprine and low dose of steroids), it
is more effective than steroids or radiotherapy alone.
d- Surgical decompression: either as primary treatment or when non-
invasive methods are ineffective. It is two-wall (inferior and medial walls),
three-wall (inferior, medial and lateral walls) or four-wall (inferior, medial,
lateral and lateral part of the roof).
4- Optic neuropathy:
It is a serious complication affecting about 5% of patients. It is caused by
compression of the nerve or its blood supply by congested and enlarged recti
muscles. It may lead to severe and permanent but preventable visual acuity
impairment.
Presentation:
a- Decreased visual acuity.
b- Impaired color vision, e.g. TV screen.
Signs:
- RAPD (Relative Afferent Pupillary Defect)
- Abnormal visual parameters: e.g. Decreased visual acuity, Color
desaturation (lighter colors), Diminished light brightness appreciation, and
Visual field defect, like central and paracentral defects.
- Increased intraocular pressure.
- Optic disc: it is normal, but occasionally swollen and rarely atrophic.
Treatment:
a- IV methyl Prednisolone (it is a serious condition).
b- Orbital decompression if (a) not effective.
5- Restrictive myopathy:
Between 30-50% of patients with TED develop ophthalmoplegia which may
be permanent.
Signs:
- Restriction of ocular motility, initially by inflammatory oedema and later
by fibrosis.
- Increased intraocular pressure in up-gaze due to ocular compression a
fibrotic inferior rectus.
In order of frequency:
a- Elevation defect by inferior rectus involvement.
b- Abduction defect by medial rectus involvement.
c- Depression defect by superior rectus involvement.
d- Adduction defect by lateral rectus involvement.

12
Treatment:
a- Surgery:
Indication: Diplopia in primary or reading positions.
Goal: to achieve binocular single vision in primary and reading positions.
Technique: Recession of restricted muscle.
b- Botulinum toxin injection:
Into the involved muscle may be useful in selected cases (it is of temporary
effect).
General information's out of this lecture:
In ophthalmology we should differentiate between those 3 terms:
* Exenteration: Complete excision of the lids, conjunctiva, eyeball and all
other intraorbital structures (extraorbital muscles and orbital fat). In modified
type exenteration, the lids are splitting through the gray line in to 2 lamellae,
anterior and posterior, the posterior lamellae is excised only in addition to
conjunctiva, eyeball and other intra orbital structures. (anterior lamellae of lids
left for cosmetic reason)
* Evisceration: is excision of the cornea and take it out, then evacuation of all
intraocular contents. (We are leaving empty sclera only)
* Enucleation: excision of the eyeball as a whole

13
