Nephrology
Dr. Mohamad hanoon
Medicine
”
Renal stone
“
Dr.Mohamad
Lecture
# 6
Total Lec: 43
2
3
Urinary tract calculi nephrolithiasis and nephrocalcinosis
-Very common , a lifetime risk of
10% higher in the Middle East.
-Most stones occur in the upper urinary tract.
-composed of calcium oxalate and phosphate
-Frequently a recurrent problem
-50% recurrence rate within 10 years due to metabolic defect (hyperurecemia and
hypercalcemia)
-recurrence increases if a metabolic or other predisposing factor
to stone formation is
present and is not modified by treatment.
Nephrolithiasis
refers to stone formation within the renal tubules or collecting system ,
although calculi are often found within the ureters or in the bladder
Nephrocalcinosis
not stones but just augmented calcium content within the Kidney
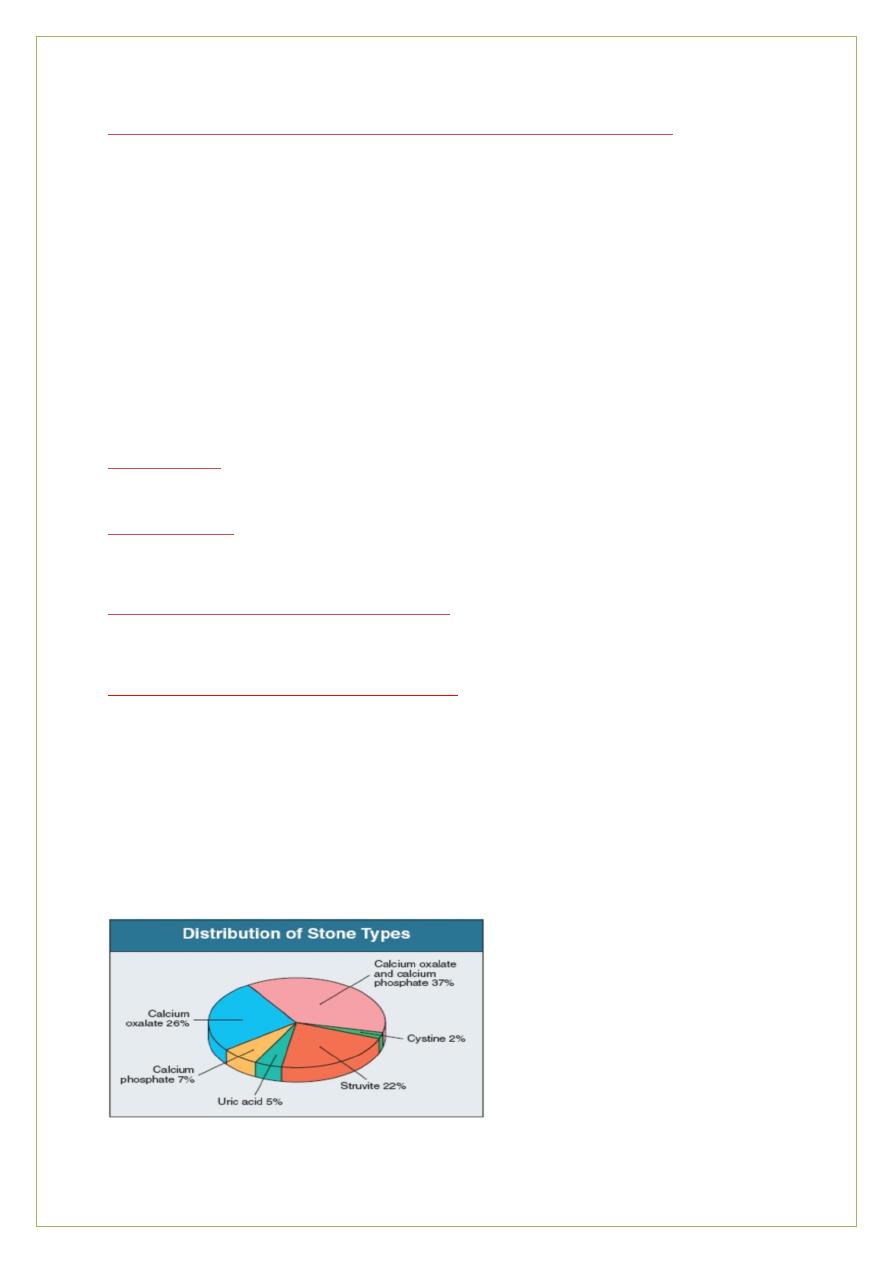
Type and frequency of renal stones in the UK
Type of renal stone
Percentage
Calcium oxalate usually with calcium phosphate 65%
Calcium phosphate alone 15%
Magnesium ammonium phosphate struvite 10-15%
Uric acid
3-5%
Cystin 1-2%
Rare drugs
4
Aetiology
Normal urine
:
-
-
has crystals (at times). So it is normal to find crystals in urine
-
extremely effective in maintaining a stable supersaturated state by certain components,
Inhibitors of crystal formation , preventing the formation of stones .
Postulated inhibitors include
;
-
Inorganic
:-
magnesium, pyrophosphate and citrate
.
Organic :-
glycosaminoglycans and nephrocalcin (an acidic protein of tubular origin) . Tamm–Horsfall
protein may have a dual role in both inhibiting and promoting stone formation
-
Many stone-formers have no detectable metabolic defect
‘ idiopathic stone-formers .’
Factors predisposing to stone formation in those are
:-
-
Chemical composition of urine
-
Concentrated urine as a consequence of dehydration
-
hot climate or work in a hot environment.
-Impairment of inhibitors of crystallization in urine
Causes of urinary tract stone formation, Predisposing factors for kidney stones
Environmental and dietary
•Low urine volumes: Dehydration ,high temp., low fluid intake
•Diet: high protein, Hyperuricaemia
, hyperuricosuria, high sodium, low calcium
•High sodium , oxalate
& urate excretion
•Low citrate excretion
5
Acquired causes
• Hypercalcaemia
• Ileal disease or resection (increases oxalate absorption and urinary excretion (
RTA type I , .Infection
Congenital and inherited causes
• .Familial hypercalciuria
• APKD
,
• Medullary sponge kidney
• Cystinuria
• Renal tubular acidosis type I (distal )
• Primary hyperoxaluria
- Drugs
Hypercalcaemia
If the GFR is normal, hypercalcaemia almost leads to hypercalciuria .The common causes of
hypercalcaemia leading to stone formation are: - primary hyperparathyroidism )
most
common), vitamin D ingestion , sarcoidosis
Hypercalciuria the most common metabolic abnormality detected in calcium stone-
formers .Defined as 24 hour calcium excretion of > 7.5 mmol in male and more than 6.25
mmol in female stone-formers .
Causes of hypercalciuria are :
- Hypercalcaemia
- Excessive dietary intake of calcium
,
- Excessive resorption of calcium from the skeleton ,prolonged immobilization or
weightlessness
- Idiopathic hypercalciuria ..
Hyperoxaluria
-Autosomal recessive inborn errors of glyoxalate metabolism ,increased endogenous
oxalate biosynthesis associated with calcium oxalate stone formation
-poor prognosis is owing to widespread calcium oxalate crystal deposition in the kidneys. .
CRF
, in the late teens or early twenties .
-Successful liver transplantation
-
cure the metabolic defect
6
Much more common causes of mild hyperoxaluria are:-
-
excess ingestion of foodstuffs high in oxalate, spinach
& tea.
-dietary calcium restriction, with compensatory increased absorption of oxalate.
-GIT disease (e.g .Crohn’s), usually with an intestinal resection, associated with increased
absorption of oxalate from the colon.
Hyperuricaemia and hyperuricosuria
-
Uric acid stones 3-5% in the UK. 40% in the middle east.
-
primary or secondary ( increased cell turnover MPD (
-
Some have hyperuricosuria )
>4 mmol per 24 hours on a low-purine diet) without
hyperuricaemia .
-Dehydration alone may also cause uric acid stones to form .
-
Patients with ileostomies (dehydration and loss of bicarbonate from GIT secretions
results in the production of an acid urine (uric acid is more soluble in an alkaline than in an
acid medium ).
Etiology
Some patients with calcium stones also have hyperuricaemia and/or hyperuricosuria;
-
it is believed the calcium salts precipitate upon an initial nidus of uric acid in such patients.
Cystinuria
is a rare condition in which reabsorption of filtered cystine, ornithine, arginine
and lysineis defective. It is caused by mutations in the SLC3A1 amino acid transporter gene.
The high concentration of cystine in urine leads to cystine stone formation
Medications associated with nephrolithiasis and nephrocalcinosis .
Calcium Stone Formation
Loop diuretics
, Vitamin D
, Corticosteroids
Calcium supplements
Antacids (calcium and non calcium antacids (
Theophylline
*
Acetazolamide* Amphotericin B *
7
Uric Acid Stone Formation
Salicylates* Probenecid* Allopurinol* (xanthine stones)
Melamine (in contaminated infant formula and milk product)
Medications That May Precipitate into Stones
Acyclovir (if infused rapidly intravenousl)
Triamterene
*
Indinavir* Nelfinavir
*
Urinary tract calculi and nephrocalcinosis
-
In developed countries, most calculi occur in healthy young men in whom investigations
reveal no clear predisposing cause.
*Urinary concretions vary greatly in size
-particles like sand anywhere in the urinary tract.
-
large round stones in the bladder.
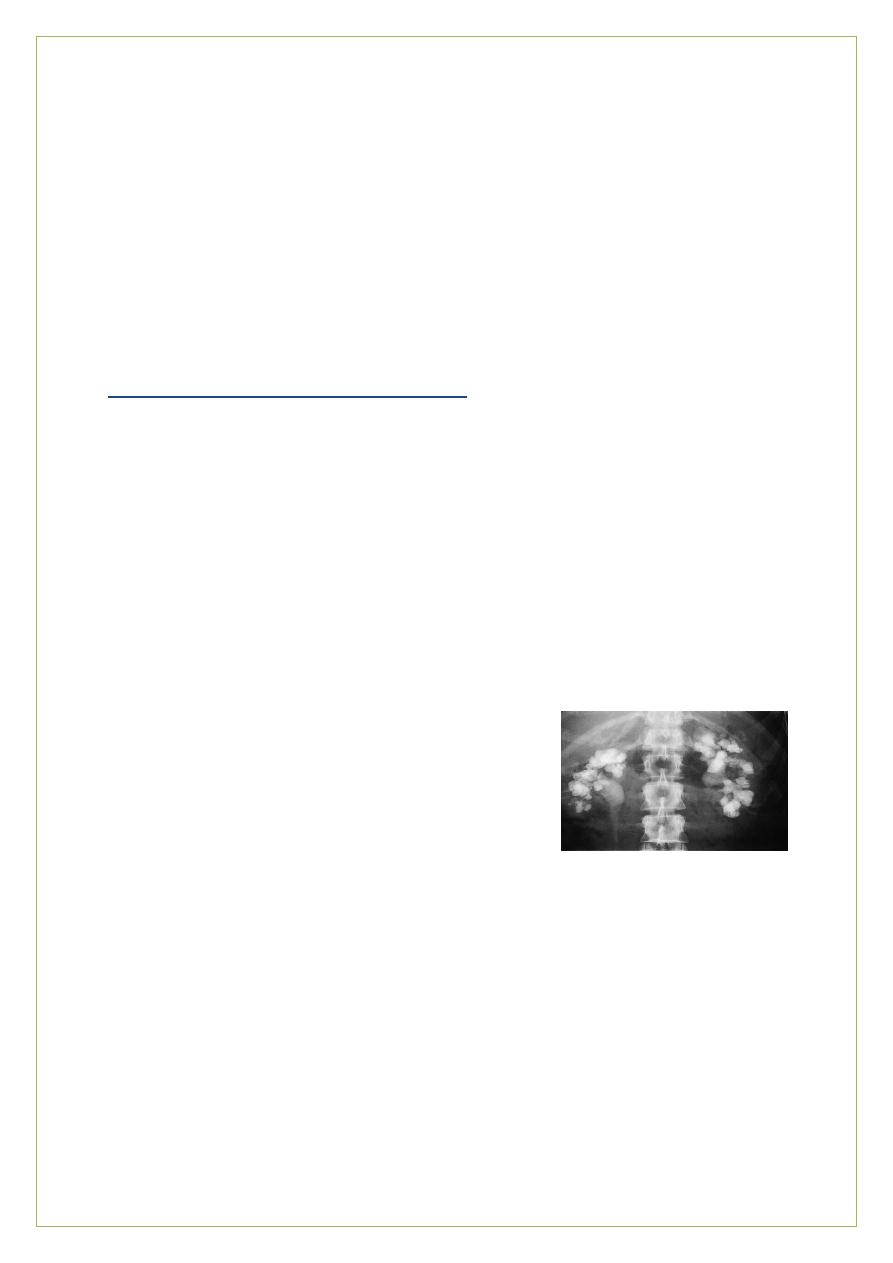
Staghorn calculi fill the whole renal pelvis and branch into the calyces ( they are usually
associated with infection and composed largely of struvite).
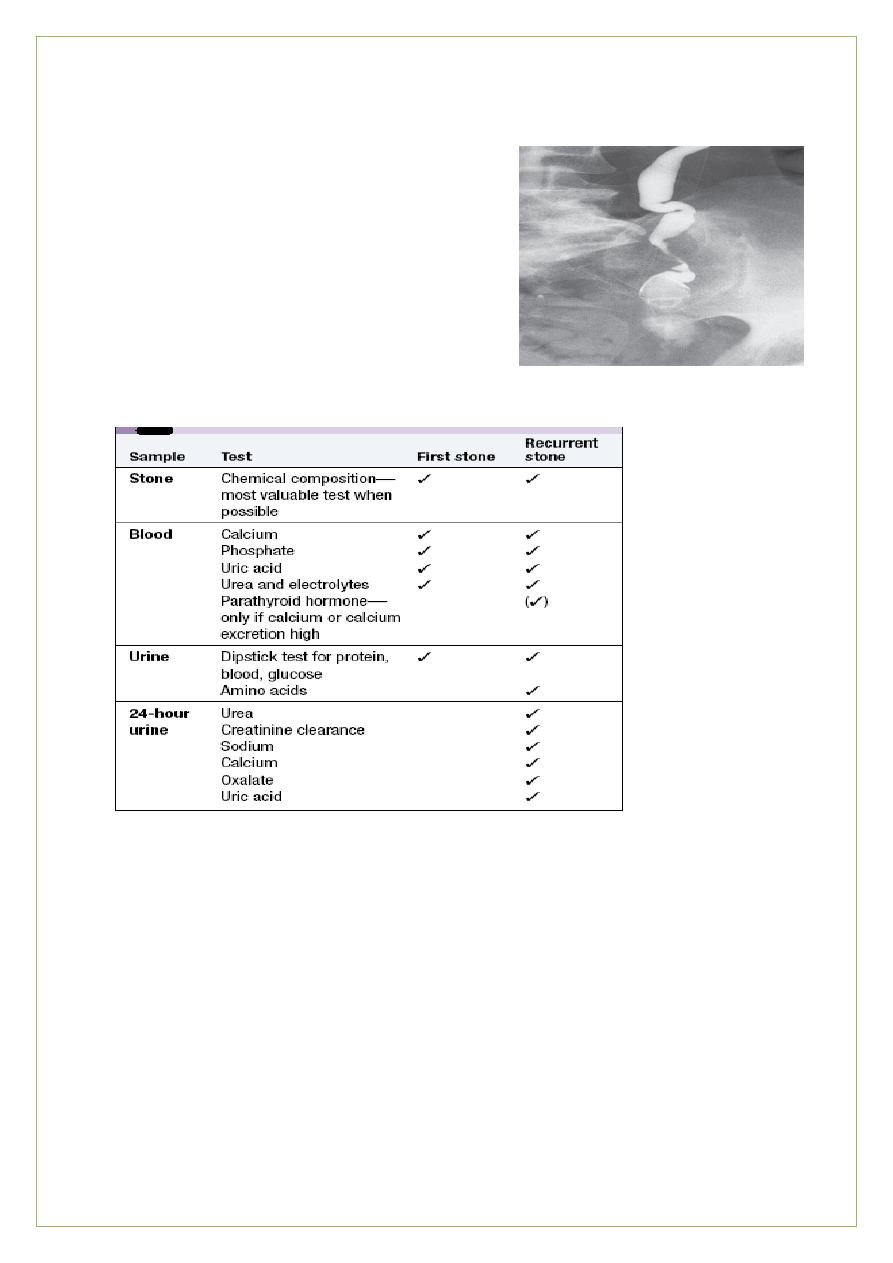
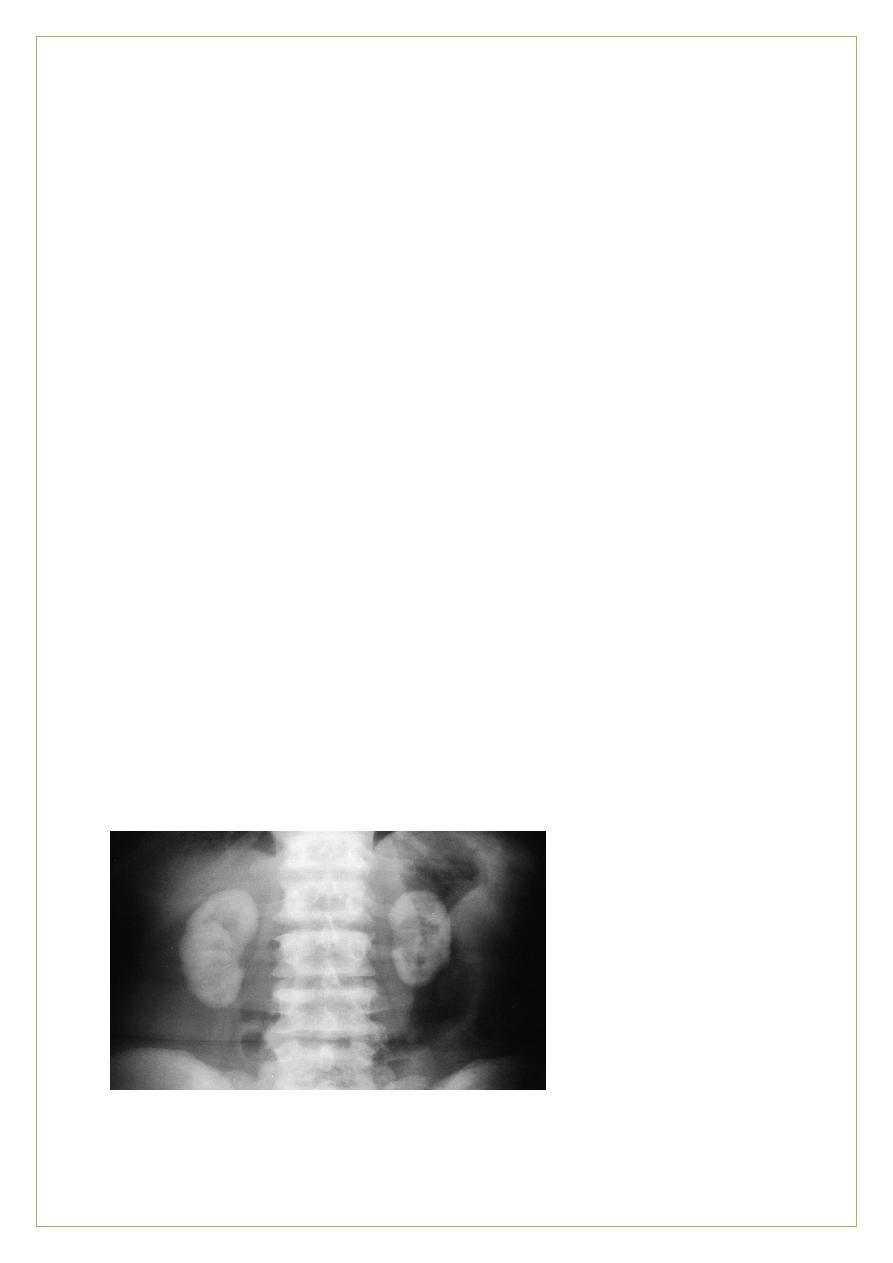
this image shows a radio-opaque bilateral staghorn calculi visible during IVU .The intravenous pyelogram
demonstrates that, while some dye is being excreted by the right
kidney, there is little function on the left
.
Clinical assessment:-
-The most common presentation is with
renal colic
-Acute loin pain radiating anteriorly and often to the groin ,together with haematuria, is
typical of ureteric obstruction ( stone becomes impacted in the ureter) most commonly due
to calculi (D.Dx sloughed renal papilla, tumour or blood clot)
-radiates round the flank to the groin and often into the testis or labium (sensory
distribution of the L1)
-The pain steadily increases in intensity
/ peak in a few minutes.
-The patient is restless and generally tries unsuccessfully to obtain relief by changing
position or pacing the room .
8
-pallor, sweating and often vomiting.
-Frequency, dysuria and haematuria may occur.
-The intense pain usually subsides within 2 hours, but may continue unabated for hours or
days .
-
It is usually constant during attacks, although slight fluctuations in severity may occur
- Contrary to general belief, attacks rarely consist of intermittent severe pains coming and
going every few minutes .
-
Subsequent to colic, there may be intermittent dull pain in the loin or back .
Asymptomatic Stone Disease
-Even large staghorn calculi may be asymptomatic.
-Obstructive uropathy may also be painless.
therefore ,nephrolithiasis should always be considered in the D.Dx of unexplained
renal failure.
-
In the recent outbreak of melamine-associated nephrolithiasis in Chinese infants, the
majority presenting to a screening clinic had no symptoms or signs of stones .The diagnosis
of nephrolithiasis was made by ultrasound in at-risk infants and toddlers .
Investigations and
management
Dx of renal colic is usually made easily from the history and by finding red cells in the urine .
Investigations are required to confirm:
- the presence, number
& site of the stone.
- is stone overlying bone.
- degree of obstruction
& the condition of involved kidney.
-90% of stones contain calcium and are radiopaque / seen on a plain abdominal X-ray .
-When the stone is in the ureter an IVU shows delayed excretion of contrast from the
kidney and a dilated ureter down to the stone
-IVU the most commonly used, but spiral CT gives the most accurate assessment and will
identify non-opaque stones (e.g .uric acid (

9
-Ultrasound may show dilatation of the ureter if the stone is obstructing urine flow.
The stone may also cast an acoustic shadow.it is not sensitive to the lower 2/3
rd
of the
ureter as it is retroperitoneal that is why CT is the best
CT uses and benefits: for radiolucent stones, stones in the lower 2/3
rd
of the ureter, shows
kidney and the bladder
Urine crystals. A ,
calcium oxalate B ,Uric acid crystals :
C ,A typical hexagonal cystine crystal .D ,Coffin lid crystals of magnesium ammonium
phosphate (struvite
.)
-
Patients with a first renal stone should have a minimum set of investigations
-
the yield of more detailed investigation is low, and hence usually reserved for those
with :
-
recurrent or multiple stones
-
complicated
-
unexpected presentations ( e.g .in the very young (
-
Chemical analysis of stones is helpful .(the most important investigation)
-
Since most stones pass spontaneously through the urinary tract, urine should be
sieved for a few days after an episode of colic in order to collect the calculus for
analysis
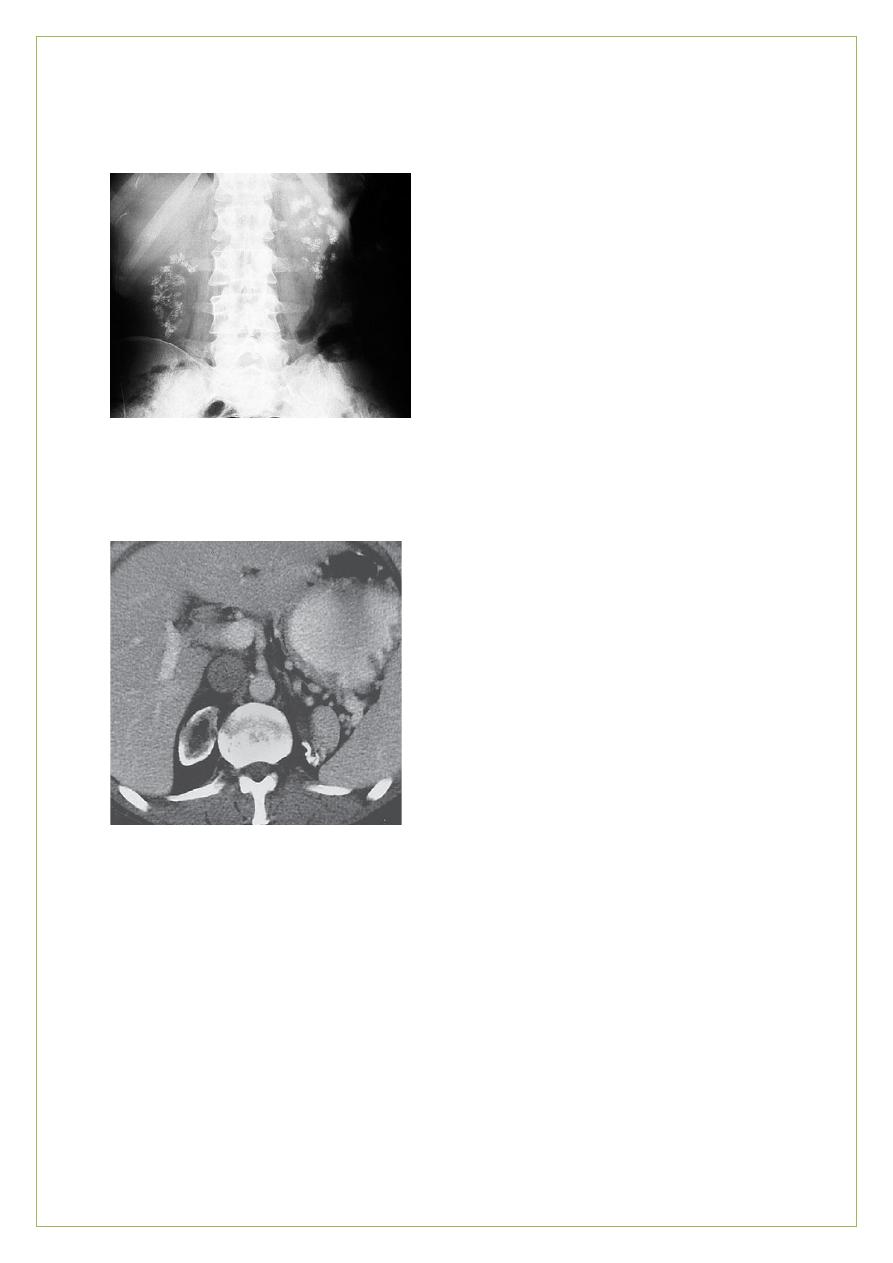
This image shows a Unilateral obstruction .IVU of a patient wit a stone (not visible) at the lower end of th right
ureter .This film, taken 2 hours post-contrast injection, demonstrates persistence of contrast medium in the
right kidney, pelvicalyceal system and ureter, whereas only asmall amount remains visible in the normal left
pelvicalyceal system
.
01
this image shows Radiolucent urate calculi .Antegrade pyelogram
showing multiple radiolucent urate stones obstructing the lower
ureter .
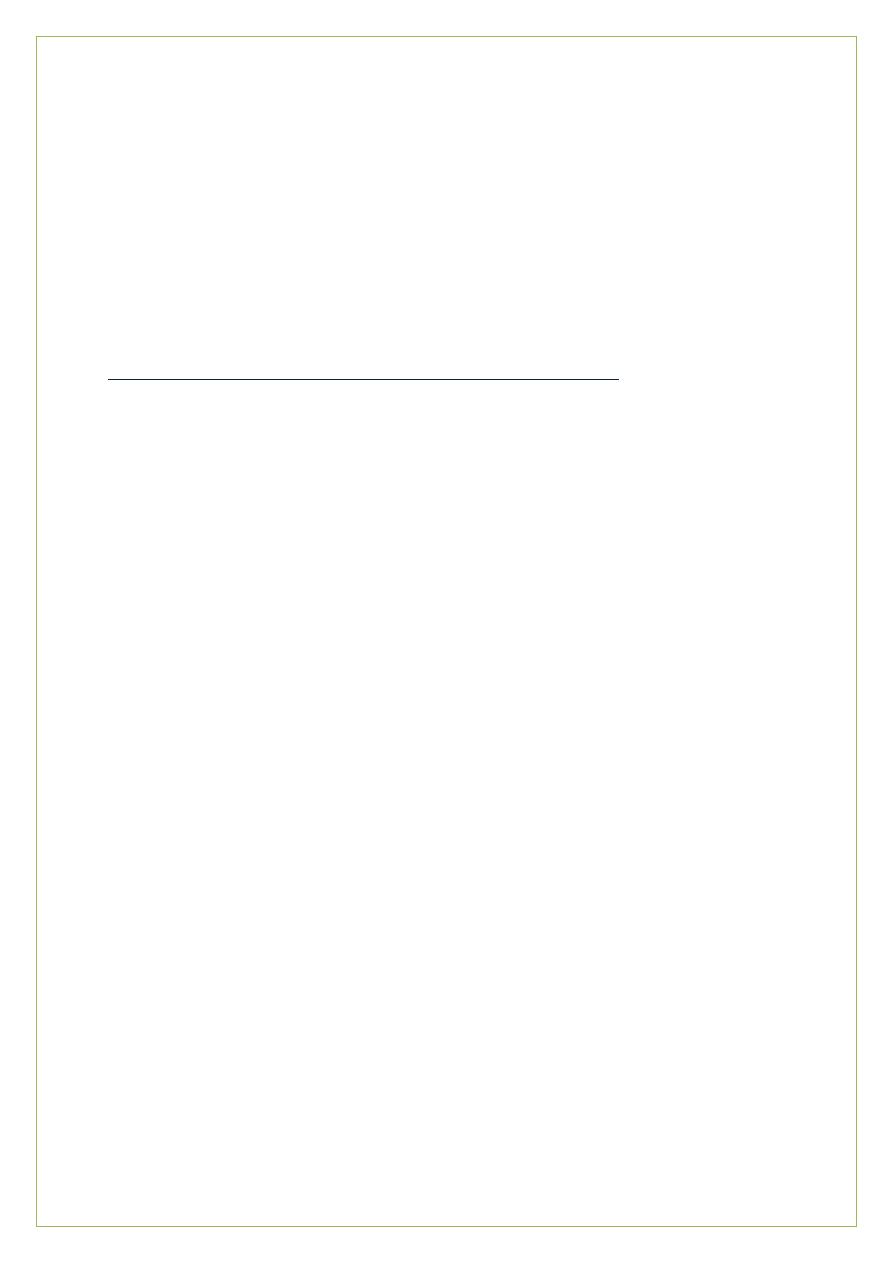
Investigations for renal stones
Management
General Treatment
;
-
Intervention for stone removal may be required when pain,
obstruction, and infection due to nephrolithiasis do not respond to conservative
management .
Surgical management of stones includes:
-extracorporeal shock wave lithotripsy.
-endoscopic or percutaneous surgical removal of stones.
00
The risk for development of renal impairment varies with types of stone, and this must be
considered in planning management .
The immediate treatment of renal pain or renal colic
is :-
bed rest and application of warmth to the site of pain .Powerful analgesia, morphine
(10–20 mg) pethidine (100 mg) IM or diclofenac as a suppository (100 mg (
Patients are advised to drink 2 L per day +/- IV fluids (no benefit from forced diuresis)
Size of stone dictates outcome
Diameter (mm) % of stones passing spontaneously
Less than 4
90
4-6
50
More than 6
10
-may require endoscopic surgical intervention .
-All stones are potentially infected and surgery should be covered with appropriate
antibiotics
-Immediate action is required if there is
anuria
or
pyonephrosis
)
severe Infection occurs
in the stagnant urine proximal to the stone (
.
-Attempts to develop drugs that dissolve stones was unsuccessful .
-stone in the upper 2/3rd usually Tx by surgery , in the lower 1/3
rd
usually Tx with Ca
channel blockers and alpha blockers to dilate the ureter but not for more than 2 weeks.
ESWL EXTRACORPOREAL SHOCK WAVE LITHOTRIPSY
-most stones can now be fragmented by shock waves generated outside the body are
focused on the stone ,breaking it into small pieces which can pass easily down the ureter .
This requires free drainage of the distal urinary tract .
-
Large stones, or stones which do not pass spontaneously through the urinary tract, may
require surgical removal and/or fragmentation by extracorporeal shock wave lithotripsy.
Indications for intervention
•Obstructive anuria or severe infection (pyonephrosis(
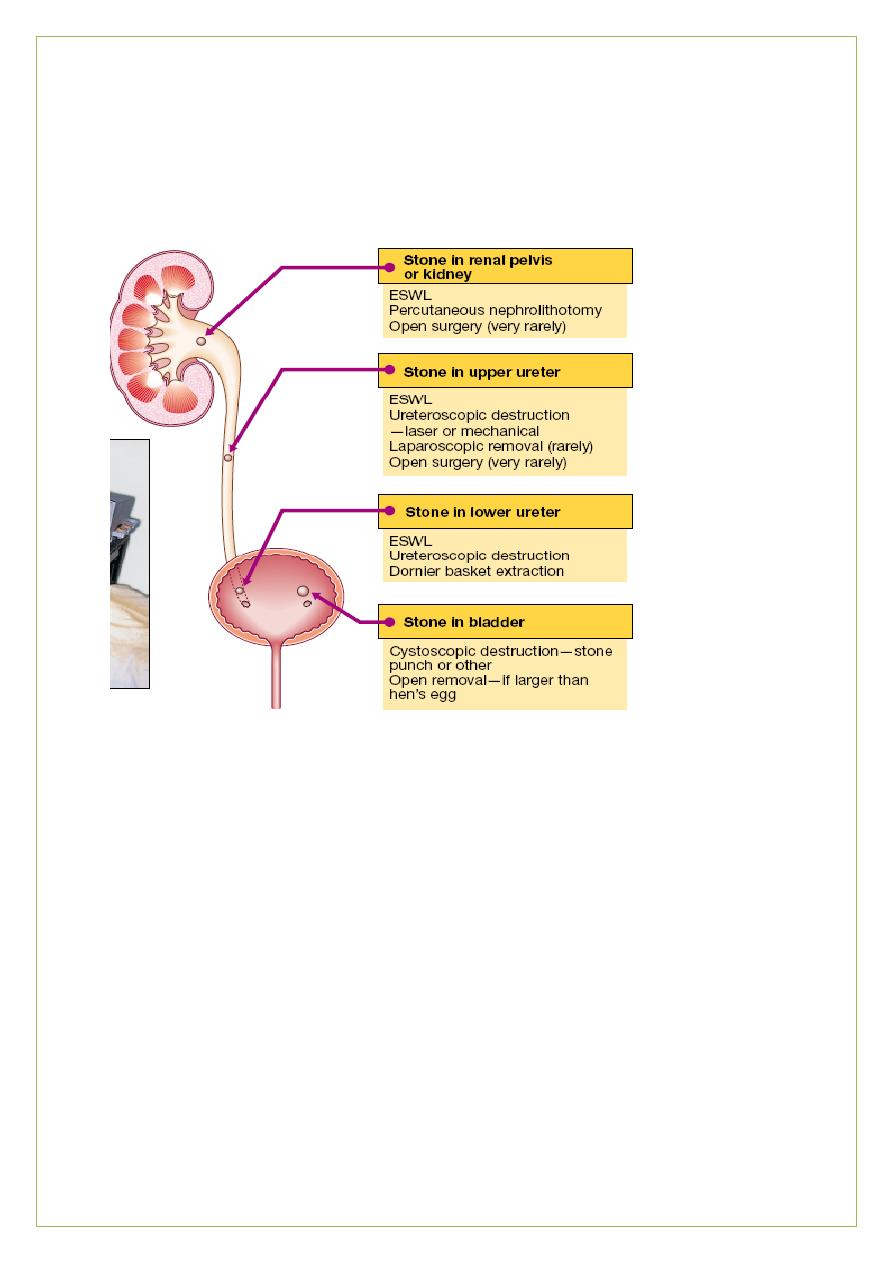
02
→Emergency percutaneous nephrostomy only
•Severe pain or solitary kidney → Urgent ESWL or surgery
•Pain and failure of the stone to move
→Elective ESWL or surgery
-Urate stones can be prevented by allopurinol
-Stones formed in cystinuria can be reduced by penicillamine therapy.
-attempt to alter urine pH with ammonium chloride (low pH discourages phosphate stone
formation)
-sodium bicarbonate (high pH discourages urate and cystine stone formation .)
Measures to prevent calcium stone formation
Diet Fluid prevent supersaturation.
-
Water! Water and more water enough to make at least 2 L UOP/day
( intake 3-4 L /
distributed throughout the day (especially before bed)
ز
03
Sodium Restrict intake.
Protein Moderate, not high.
Calcium Plenty in diet (because calcium forms an insoluble salt with dietary oxalate,
lowering oxalate absorption and excretion).
•Avoid supplements away from meals (increase calcium excretion without reducing oxalate
excretion).
Oxalate Avoid rich in oxalate (spinach, rhubarb).
N.B .Citrate supplementation is of unproven value.
Drugs
Thiazide diuretics
- Reduce calcium excretion
- Valuable in recurrent stone-formers and patients with hypercalciuria
Allopurinol
If urate excretion high (unproven except for uratestones(
Avoid
Vitamin D supplements as increase calcium absorption and excretion.
Vitamin C hypersupplementation as this increases oxalate excretion.
Foods High in Oxalate and Purine
High Purine Foods
(avoid in setting of hyperuricosuria)
- Organ meats: liver, kidney, brains, heart Shellfish
- Meat: beef, pork, lamb, poultry
- Fish sardines , tuna, carp
- Certain vegetables: cauliflower, peas ,spinach, mushrooms, lima and kidney beans,
lentils
High Oxalate Foods
(avoid in setting of hyperoxaluria)
- Green beans Beets Green onions Leeks Leafy greens , spinach ,
- Cocoa Chocolate Black tea
- Berries: blackberries, blueberries ,strawberries, raspberries ,
- Orange peel Lemon peel Dried figs , nuts , peanuts
04
Nephrocalcinosis
augmented calcium content within the Kidney
Deposits of calcium may be present throughout the renal parenchyma, giving rise to fine
calcification within the renal parenchyma (nephrocalcinosis)
Medullary Nephrocalcinosis (the majority)
calcification tends to occur in the area of the renal pyramids ,
-Elevated urinary Ca++, phosphate, and oxalate, any of hypercalcemia or hypercalciuria .
-Instead of stone formation, smaller parenchymal calcifications are deposited in the medulla
,usually bilateral and relatively symmetric
Urinary
tract calculi and nephrocalcinosis
Cortical Nephrocalcinosis
-
usually the result of dystrophic calcification, which follows parenchymal tissue destruction
rather than the precipitation of excessive urinary constituents .
-
typically asymmetric
& is usually localized to the renal cortex .
-
secondary to infarction, neoplasm, and infection .
-cortical nephrocalcinosis
Transplant rejection, cortical necrosis ,tuberculosis, ethylene glycol toxicity, and chronic GN
RTA ,
-
hyperparathyroidism ,
vitamin D intoxication
Nephrocalcinosis .Dense cortical and medullary calcification in the shrunken kidneys
(oxalosis and longstanding renal failure
05
Medullary nephrocalcinosis .Plain radiograph shows
bilateral metastatic medullary nephrocalcinosis Distal RTA
Cortical nephrocalcinosis .Non–contrast-enhanced CT scan ;- cortical nephrocalcinosis in
the right kidney ( cortical necrosis
(
The End
06
Appendix
How to differentiate between stones and musculoskeletal pain?
Stones musculoskeletal
Nausea and vomiting no
Urinary symptoms no
Radiate pain no
Not affected by movement affected by movement
Case
old woman presents to the emergency department (ED) with vomiting and severe right
-
year
-
A 45
flank pain that radiates to her groin. She has been to the ED twice in the past due to similar episodes
of renal colic. and was subsequently discharged on both occasions. She admits to not seeking further
hour urine collection
-
medical care because she has no insurance. KUB shows a renal stone. 24
an 250 mg in women). Laboratory
shows a urinary calcium excretion of 350 mg (normal is less th
ray film of the
-
studies show a serum calcium concentration of 8.9 mg/dL; serum PTH is normal. An x
chest shows no abnormalities. Further investigations fail to reveal the cause of her hypercalciuria.
to increase her fluid intake. which of the following interventions will benefit this
Apart from advising her
patient?
A. Restriction of calcium in her diet B. Thiazide diuretics
C. Low dose furosemide D. High sodium intake E. Potassium citrate
5% of the United States population is affected by renal stones
-
ation: Approximately 1
Explan
(nephrolithiasis). Men have twice the risk of women. The basic pathophysiology involves the abnormal
itors of crystal formation due to
forming salts and/or a deficiency of urinary inhib
-
excretion of stone
metabolic disorders or dietary factors. Renal stones are predominantly of four types: 1. Calcium
15%) 4. Cysteine
-
15%) 3. Struvite/triple phosphate ( 1 0
-
oxalate/phosphate (75%) 2. Uric acid (1 0
he most common type of renal stones seen. These are most commonly
(<1%) Calcium stones are t
seen in the third or fourth decade of life. Most patients present with hypercalciuria (24 hour urinary
females).
calcium excretion > 300 mg in males and >250 mg in females;> 4 mg/kg in both males and
The most common causes of calcium stones are:
1 . Idiopathic hypercalciuria: This is characterized by hypercalciuria. normal serum calcium levels. and
absent metabolic disease. It is the most common form of hypercalciuria.
2. Hypercalciuria due to systemic disorders (e.g .. primary hyperparathyroidism. sarcoidosis. etc.)
3. Hyperuricosuria 4. Hyperoxaluria: The cause may be hereditary, dietary (i.e., due to ingestion of a
large amount of vitamin C or green leafy vegetables). or secondary to short bowel syndrome. 5.
Decreased urinary citrate
6. Renal tubular acidosis: Typically, nephrocalcinosis is seen.
7. Chronic decrease in urine output This helps the precipitation of calcium salts.
07
This patient most likely has recurrent hypercalciuric stones due to idiopathic hypercalciuria. This is
best treated with increased fluid intake. dietary sodium restriction. and thiazide/amiloride diuretics.
Thiazide diuretics decrease urinary calcium excretion (primarily by inducing mild volume depletion.
which leads to a compensatory rise in proximal reabsorption of sodium and calcium) and preventthe
precipitation of calcium in the urine. Patients with recurrent calcium stones due to hyperuricosuria can
be treated with purine-restricted diet and allopurinol.
Recommendations for calcium oxalate urolithiasis (in order of relative importance):
1. Increased fluid intake (>3 L per day) 2. Normal or increased calcium diet (recommended daily
allowance is 1000 mg/dl) 3. Dietary sodium restriction ( < 1 DO mEq/dL) 4. Oxalate restriction (i.e ..
dark roughage. chocolate. and vitamin C) 5. Decreased dietary proteins (i.e .. beef. fish. eggs. and
poultry).
summary
So in
Patients with recurrent hypercalciuric renal stones should be treated with increased fluid intake.
sodium restriction. and a thiazide diuretic. Calcium restriction is not advised. The treatment of a first
uncomplicated calcium stone is hydration and observation.
