1
First stage
Biology
Lec / 8 Abeer H.Alkhafaf
Blood
Blood is a fluid, it is a specialized connective tissue, Propelled mainly by rhythmic
contractions of the heart, about five liters of blood in an average adult moves
unidirectionally within the closed circulatory system. The primary components are:
1- Plasma.
2- Formed elements circulating in the plasma include:
* Erythrocytes (Red blood cells).
* Leukocytes (white blood cells).
* Platelets.
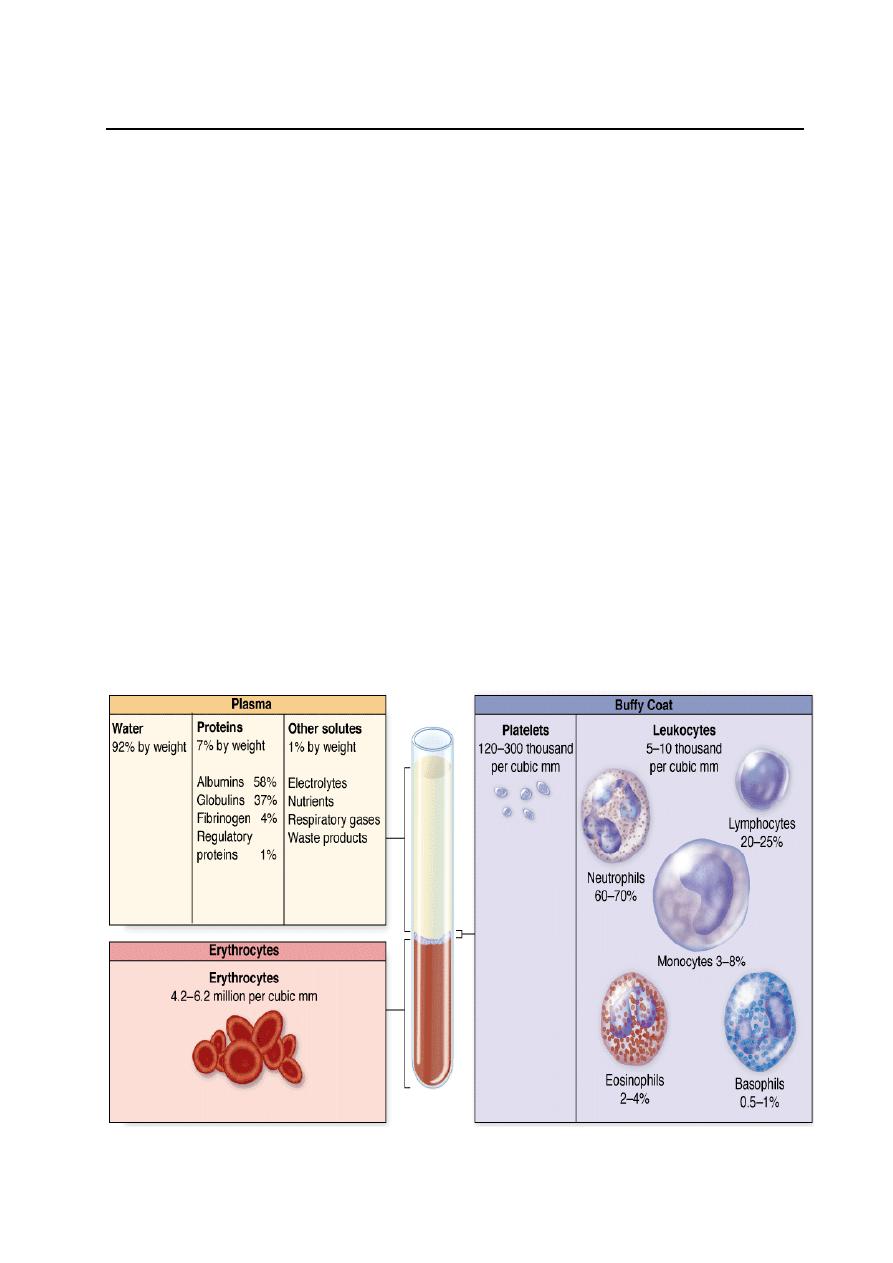
Collected blood in which clotting is prevented by the addition of anticoagulants
(e.g. heparin, citrate), can be separated by centrifugation into layers that reflect its
heterogeneity. Erythrocytes make up the bottom layer and their volume, normally
about 45% of the total blood volume in healthy adults, it is called the hematocrit.
Above this region buffy coat is white or grayish layer (about 1% volume) less dense
than erythrocytes consists of leukocytes and platelets. Plasma is the yellowish
translucent, slightly viscous supernatant comprising 55% at the top half of the
centrifugation tube.
Composition of whole blood

2
Functions of blood:
1- Distribution:
- Transporting O
2
, CO
2
, metabolites, hormones, Nutrients.
- Remove metabolic waste.
2- Regulation:
- Maintain body temperature.
- Maintain PH, and fluid volume.
3- Protection:
- Restrict loss blood at injury (clotting).
- Prevent infection (leukocytes).
Plasma
Plasma the liquid in which peripheral blood cells are suspended, pH 7.4. Composed
of water, electrolytes such as Na
+
and Cl, 7% plasma proteins (such as albumin,
fibrinogen, globulins), hormones, fats, amino acids, vitamins carbohydrates,
lipoproteins as well as other substances.
Serum: the clear liquid that can be separated from clotted blood. Serum differs
from plasma, serum does not contain white or red blood cells nor a clotting factors.
Serum includes all proteins not used in blood clotting (coagulation) and all the
electrolytes, antibodies, antigens, hormones, and any exogenous substances
(e.g. drugs and microorganisms). It is the clot that makes the difference between
serum and plasma.
3
Blood Cells
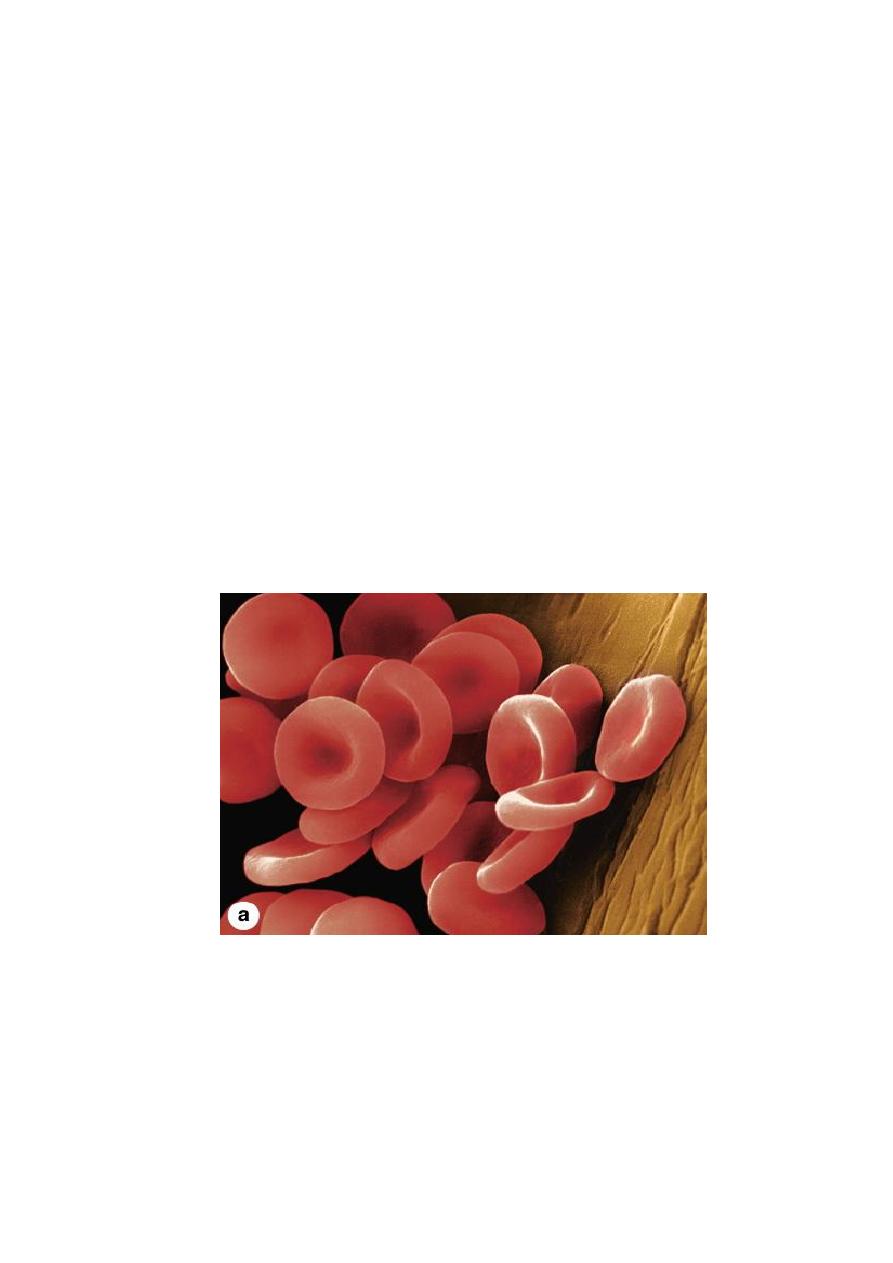
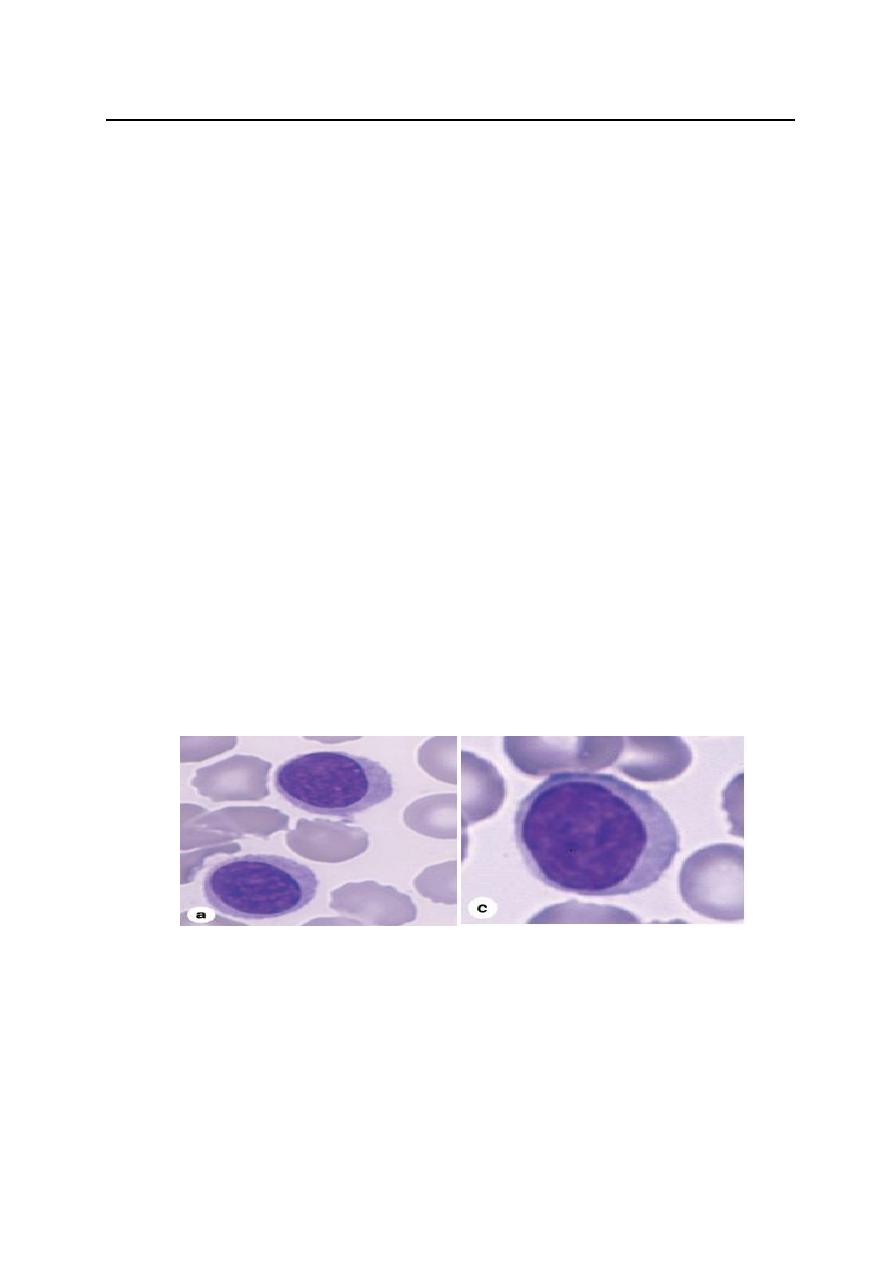
A. Erythrocytes ( RBC )
A normal red blood cell is a biconcave disk, lack nuclei, and the cytoplasm is
densely filled with hemoglobin, average RBC count ( 4.2 - 6.2 million/μl ), this
biconcave shape provides a large surface area for facilitates gas exchange.
Erythrocyte differentiation includes loss of the nucleus and all organelles, shortly
before the cells are released by bone marrow into the circulation.
Erythrocyte have flexible membrane. Flexibility required for passage through
capillaries and important for the normal low viscosity of blood. Cells frequently
assume a cup shape in capillaries.
Life span: The mature erythrocyte has a life span of approximately 120 days in the
circulation.
Fuction: Transport O
2
and CO
2
. hemoglobin combined with O
2
or CO
2
, forms
oxyhemoglobin or carbaminohemoglobin, respectively.
Normal human erythrocytes
4
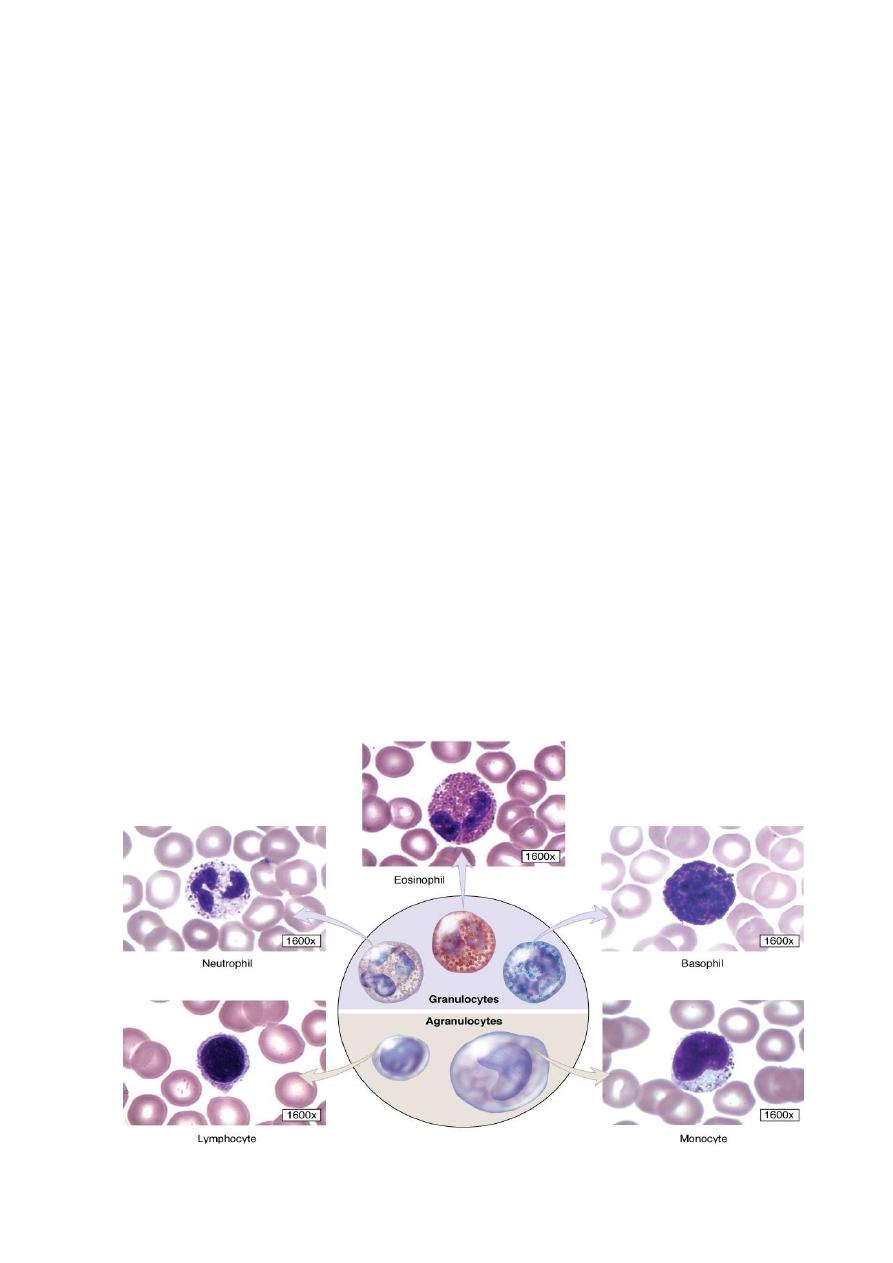
B. Leukocytes (WBC)
Leukocytes are generally spherical cells have nuclei & organelles, no
hemoglobin Unlike RBC, and inactive while suspended in circulating blood, but
become amoeboid and motile after leaving the blood vessels and invading the
tissues. Leukocytes migrate to the tissues where they become functional and
perform various functions:
* defend against pathogens
* remove toxins and wastes
* remove abnormal/damaged cells.
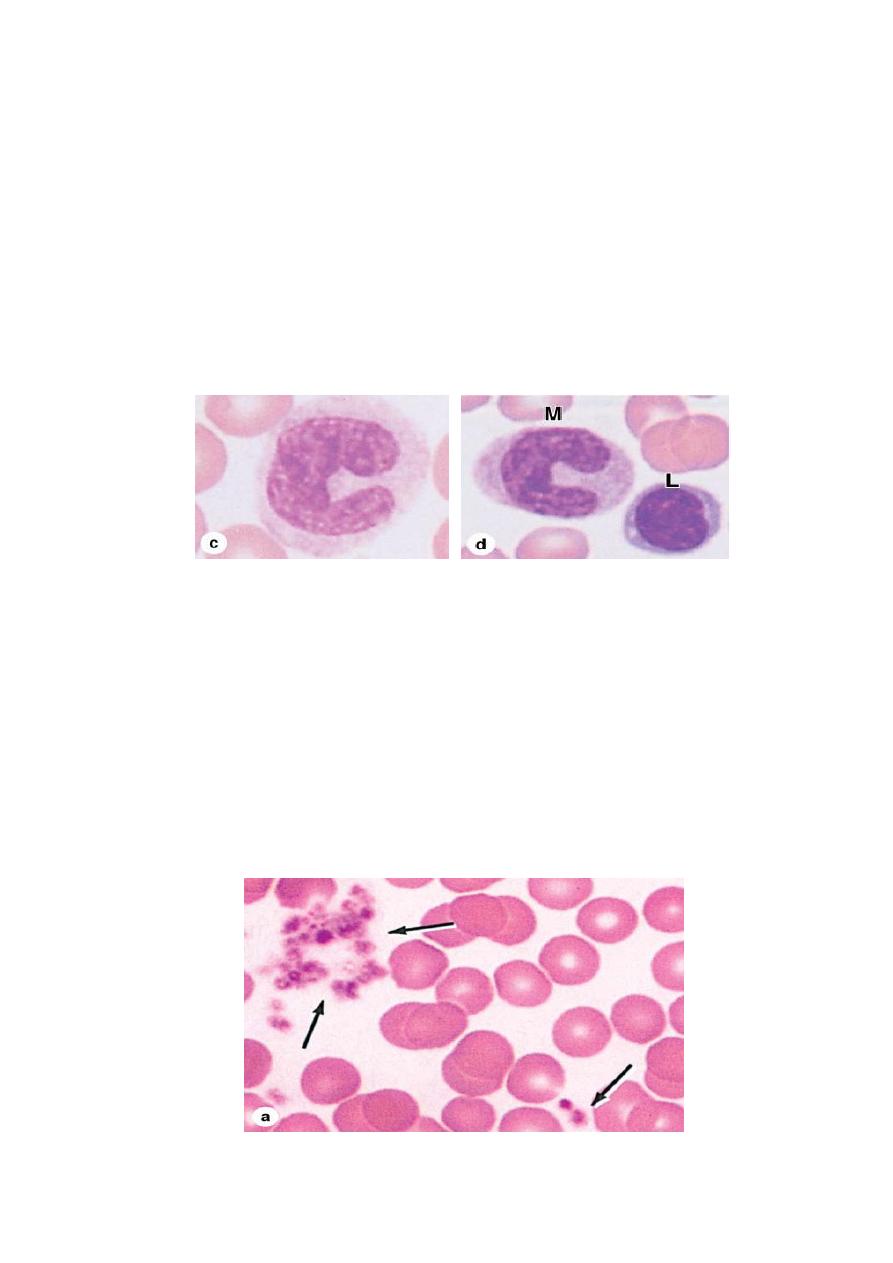
According to the type of cytoplasmic granules and the shape of their nuclei,
leukocytes are divided into two groups:
1- Polymorphonuclear granulocytes: which have polymorphic nuclei with two or
more lobes and this group includes the neutrophils, eosinophils, and basophils.
Granules posses two types in their cytoplasm:
* Specific granules that bind neutral, acidic or basic stain and have specific
functions.
* Azurophilic granules which are specialized lysosomes, stain darkly, and
present at some level in all leukocytes.
2- mononuclear a granulocytes, do not have specific granules, but they do contain
azurophilic granules (lysosomes). The nucleus is round or indented. This group
includes lymphocytes and monocytes.
Types of human leukocytes
5
1- Granulocytes
A- Neutrophils
Neutrophils are inactive and spherical while circulating, but become actively
amoeboid during diapedesis and upon adhering to solid substrates. They are
12–15 μm in diameter in blood smears, with nuclei having 2 to 5 lobes linked by
thin nuclear extensions. Constitute 60–70% of circulating leukocytes.
Life span: neutrophils are short-lived cells with a half-life of 6–7 hours in blood
and a life span of 1–4 days in connective tissues.
Functions: Neutrophils are the first line of defense against microorganisms,
especially bacteria. They are active phagocytes of bacteria and other small particles
using chemotaxis.
B- Eosinophils
Eosinophils are far less numerous than neutrophils, constituting only 2–4% of
leukocytes in normal blood. This cell is about the same size as a neutrophil, but with
a characteristic bilobed nucleus.The main identifying characteristic is the abundance
of large red specific granules that are stained by eosin.
Functions:
- Defense against parasites such as helminthic worms and protozoa.
- Eosinophils modulate inflammatory responses in many ways, and they are an
important source of the factors mediating allergic reactions and asthma.

6
C- Basophils
Basophils are about 12–15 μm in diameter, but make up less than 1% of blood
leukocytes and are therefore difficult to find in smears of normal blood. The nucleus
is divided into two or more irregular lobes, which are often difficult to see because
of the large, dark-staining specific granules. Basophilic specific granules also
contain much histamine and various mediators of inflammation.
Function: Although the basophil possesses phagocytic capabilities, it is mainly a
secretory cell which mediates the hypersensitivity reaction.
7
First stage
Biology
Lec Abeer H. Alkhafaf
2- Agranulocytes
A- Lymphocytes
Lymphocytes make 28 % of white blood cells, they are round cells. Mature
lymphocytes show a spectrum of sizes ranging from small lymphocytes to larger
forms. They contain a single, deeply-stained, spherical nucleus which can have a
slight indentation.
Life span: Lymphocytes vary in life span according to their specific functions;
some live only a few days and others survive in the circulating blood or other tissues
for many years.
They can be subdivided into functional groups according to surface molecules that
can best be distinguished immunocytochemically:
- T lymphocytes. - B lymphocytes. - natural killer (NK) cells.
Function: Lymphocytes have diverse functional roles related to immune defense
against invading microorganisms, foreign or abnormal antigens, and cancer cells.
8
B- Monocytes
Monocytes are the largest a granular leukocytes, derived from bone marrow, the
nucleus is large eccentrically placed, and may be oval, kidney-shaped, or U-shaped.
Constituting 5% of leukocytes in normal blood.
Life span: Monocytes can live in the blood for 2 - 3 days, after which they move
into the connective tissue, where they may remain for a few months or longer.
Functions:
- Circulating monocytes are precursor cells of macrophages.
- They ingest (phagocytize) and remove particulate matter, tissue debris, and
infectious agents.
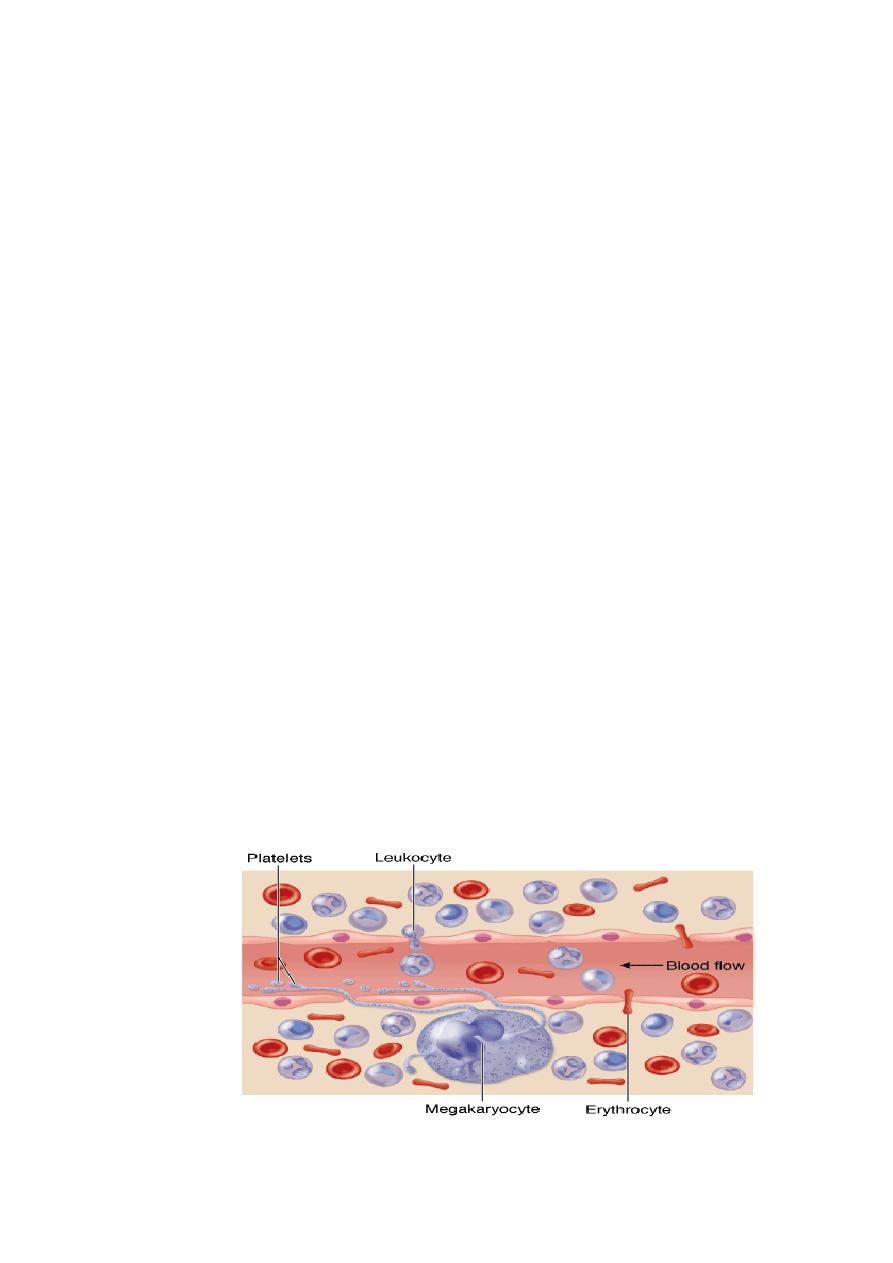
C. Platelets
Blood platelets (thrombocytes) are nonnucleated, disklike cell fragments (2–4)μm,
derived from megakaryocytes in the bone marrow. In stained blood smears,
platelets often appear in clumps. Normal platelet counts range from 200,000 to
400,000 /μl of blood. Platelets have a life span of about 10 days.
Function of Platelets:
- promote blood clotting and preventing loss of blood.
- help repair minor tears or leaks in the walls of blood vessels.
Platelets
9
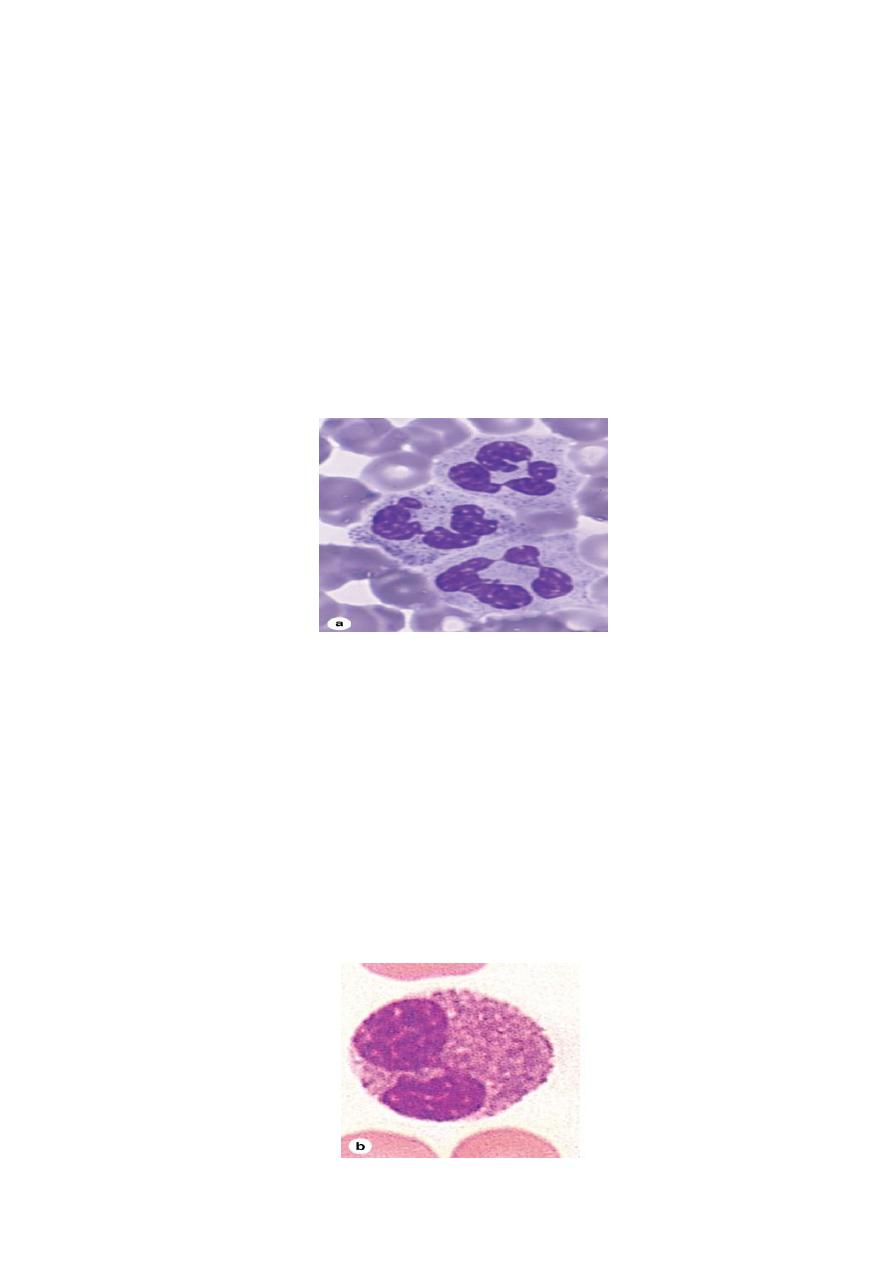
Hemopoiesis
The different blood cells have relatively short life spans and must be renewed to
maintain appropriate circulating levels. The process of renewal is known as
hematopoiesis (hemopoiesis).
All blood cells arise from a single type of stem cell in the bone marrow called
pluripotent stem cell, because it can produce all cell types. The pluripotent stem
cells proliferate and form two major cell lineages; one for lymphocytes (lymphoid
cells) and another for myeloid cells that develop in bone marrow (granulocytes,
monocytes, erythrocytes, and megakaryocytes). Early in their development,
lymphoid cells migrate from the bone marrow to the thymus, lymph nodes, spleen,
and other lymphoid tissues.
Erythropoiesis (RBCs): Process of formation and differentiation of RBCs. the
kidney secretes a hormone called erythropoietin stimulates the production of
erythrocytes in the bone marrow. These erythrocytes leave the bone marrow and
move into the blood stream.
Thrombocytopoiesis: platelets originate by fragmentation at the ends of
cytoplasmic processes extending from Megakaryocyte (a giant cell with irregularly
lobulated polyploidy nuclei) in bone marrow; each megakaryocyte can produce a
few thousand platelets. Thrombopoietin stimulates megakaryocytes and platelet
production.
Megakaryocyte
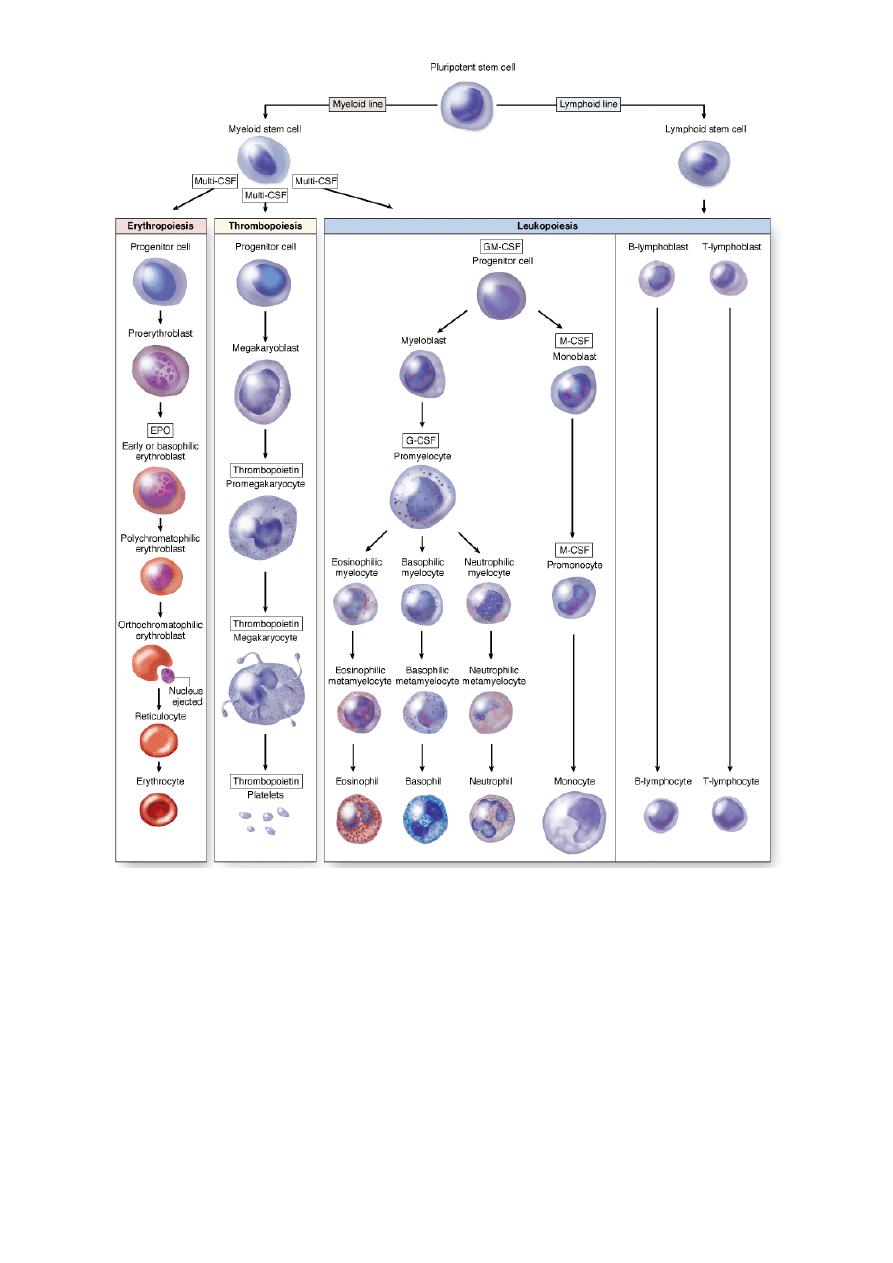
10
Origin and differentiative stages of blood cells
