Infectious disease 5
MENINGITIS مهم جدا جداMeningitis, inflammation of the leptomeninges, can be caused by bacteria, viruses, or, rarely, fungi.
The term aseptic meningitis refers principally to viral meningitis, but meningitis with negative cerebrospinal fluid (CSF) bacterial cultures may be seen with:
Other infectious organisms (tuberculosis)
Parameningeal infections (brain abscess, epidural abscess).
Chemical exposure (NSAI drugs, IV immunoglobulin).
Autoimmune disorders.
Partially treated meningitis refers to bacterial meningitis complicated by antibiotic treatment before the lumbar puncture, which may result in negative CSF cultures, although other CSF findings suggestive of bacterial infection persist. The etiology can sometimes be confirmed by polymerase chain reaction of the CSF.
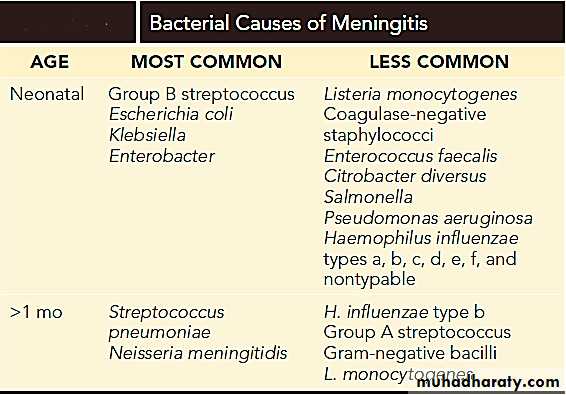
ETIOLOGY of bacterial meningitis
ETIOLOGY of viral meningoencephalitis
Enteroviruses, parechoviruses, and arboviruses are the principal causes of meningoencephalitis.Other viruses include: HSV, EBV, CMV, HIV & Mumps virus in unvaccinated children.
Risk factors for bacterial meningitis:
The incidence of bacterial meningitis is highest among children under 1 year of age.
Acquired or congenital immunodeficiencies.
Hemoglobinopathies such as sickle cell disease.
Functional or anatomic asplenia.
Crowding .
CSF leak (fistula), resulting from congenital anomaly or following a basilar skull fracture.
CLINICAL MANIFESTATIONS
Indications of meningeal inflammation include headache, irritability, lethargy, nausea and vomiting, photophobia, fever usually is present. Nuchal rigidity, Kernig and Brudzinski signs of meningeal irritation are often positive in children older than 12 months.
In young infants, signs of meningeal inflammation may be minimal with only irritability, restlessness, depressed mental status, poor feeding and vomiting present & a bulging.
Focal neurologic signs, seizures, arthralgia, myalgia, petechial or purpuric lesions, sepsis, shock, and coma may occur.
Ptosis, sixth nerve palsy, bradycardia with hypertension, and apnea are signs of increased intracranial pressure with brain herniation.
LABORATORY AND IMAGING STUDIES
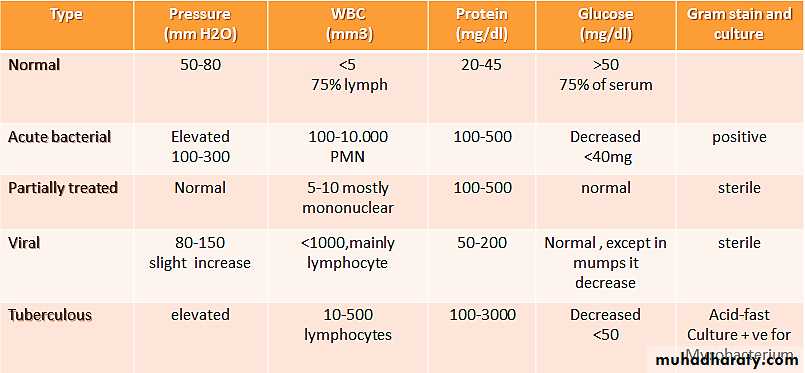
CSF examination, includes:
Pressure.
WBC count & differential.
Protein.
Glucose levels.
Gram stain.
CSF culture.
PCR.
Blood cultures are positive in 90% of cases of bacterial meningitis.
Peripheral leukocytosis.
EEG may confirm an encephalitis.
CT/ MRI.
Contraindication of LP:
Increased intracranial pressure as indicated by FND, persistent tense bulging fontanele (in case of still open), or if the patient is depressed in mentation, bradycardia and papilloedema.
Cardiorespiratory compromise.
Infection at the lumber site
CSF FINDINGS IN MENINGITIS حفظ مهم
TREATMENT
Treatment of bacterial meningitis focuses on sterilization of the CSF by antibiotics and maintenance of adequate cerebral and systemic perfusion.Empirical cefotaxime (or ceftriaxone) plus vancomycin should be administered until antibiotic susceptibility testing is available.
For infants younger than 2 months of age, ampicillin is added to cover the possibility of Listeria monocytogenes.
Duration of treatment is
5 to 7 days for N. meningitidis.
7 to 10 days for H. influenzae.
10 to14 days for S. pneumoniae.
Dexamethasone (0.6 to 0.8 mg/kg daily in two to three divided doses for 2 days), as adjunctive therapy initiated just before or concurrently with the first dose of antibiotics, significantly diminishes the incidence of hearing loss and neurologic deficits resulting from H. influenzae meningitis.
Supportive therapy involves treatment of dehydration, shock, DIC, SIADH, seizures, increased ICP, apnea, arrhythmias, and coma.
COMPLICATIONS
SIADH.
Subdural effusions.
Prolonged fever
The most common neurologic sequelae include hearing loss, cognitive impairment, recurrent seizures, delay in acquisition of language, visual impairment, and behavioral problems, paresis, ataxia, or hydrocephalus..
Anemia may be a result of hemolysis or BM suppression.
Meningococcemia & DIC is most often associated with the rapidly progressive pattern of presentation and is noted most commonly in patients with shock and purpura.
Pericarditis or arthritis (infectious or immune complex).
NOTE: All patients with meningitis should have a hearing evaluation before discharge and at follow-up.
Poor prognosis is associated with:
Young age.
Long duration of illness before effective antibiotic therapy.
Seizures, coma , shock at presentation.
Low or absent CSF WBC count in the presence of visible bacteria on CSF Gram stain.
Immunocompromised
PREVENTION
Vaccination and antibiotic prophylaxis of susceptible at-risk contacts represent the 2 available means of reducing the likelihood of bacterial meningitis.
Close contacts should be treated with rifampin 10 mg/kg/dose every 12 hr (maximum dose of 600 mg) for 2 days as soon as possible after identification of a case of suspected meningococcal meningitis or sepsis.