AFTER MID
TOTAL LEC: 33
Gynaecology
Dr. Raghad AbdulHalim
Lec 33 - Operative Gynecology
DR. RAGHAD - LEC 4
مكتب املدينة

Operative Gynecology
Hysterectomy
Hysterectomy is the surgical removal of the uterus. It may also
involve removal of the cervix, ovaries, fallopian tubes and other
surrounding structures.
Usually performed by a gynecologist, hysterectomy may be total
(removing the body, fundus, and cervix of the uterus; often called
"complete") or partial (removal of the uterine body while leaving the
cervix intact; also called "supracervical"). It is the most commonly
performed gynecological surgical procedure.
Oophorectomy (removal of ovaries) is frequently done together
with hysterectomy to decrease the risk of ovarian cancer
Incidence
In the UK, 1 in 5 women are likely to have a hysterectomy by the
age of 60, and ovaries are removed in about 20% of hysterectomies.
Indications
1. Certain types of reproductive system cancers (uterine, cervical,
ovarian, endometrium) or tumors, including uterine fibroids, that
do not respond to more conservative treatment options.
2. Severe and intractable endometriosis and/or adenomyosis, after
pharmaceutical or other surgical options have been exhausted.
3. Chronic pelvic pain, after pharmaceutical or other surgical options
have been exhausted.
4. Postpartum to remove either a severe case of placenta praevia (a
placenta that has either formed over or inside the birth canal) or
placenta accreta (a placenta that has grown into and through the
wall of the uterus to attach itself to other organs), as well as a last
resort in case of excessive obstetrical haemorrhage.
5. Several forms of vaginal prolapse.
6. Prophylaxis against certain reproductive system cancers,
especially if there is a strong family history of reproductive system
cancers (especially breast cancer in conjunction with BRCA1 or
BRCA2 mutation), or as part of recovery from such cancers.
7. Part of overall gender transition for trans men.
8. Severe developmental disabilities, though this treatment is
controversial at best, and specific cases of sterilization due to
developmental disabilities.
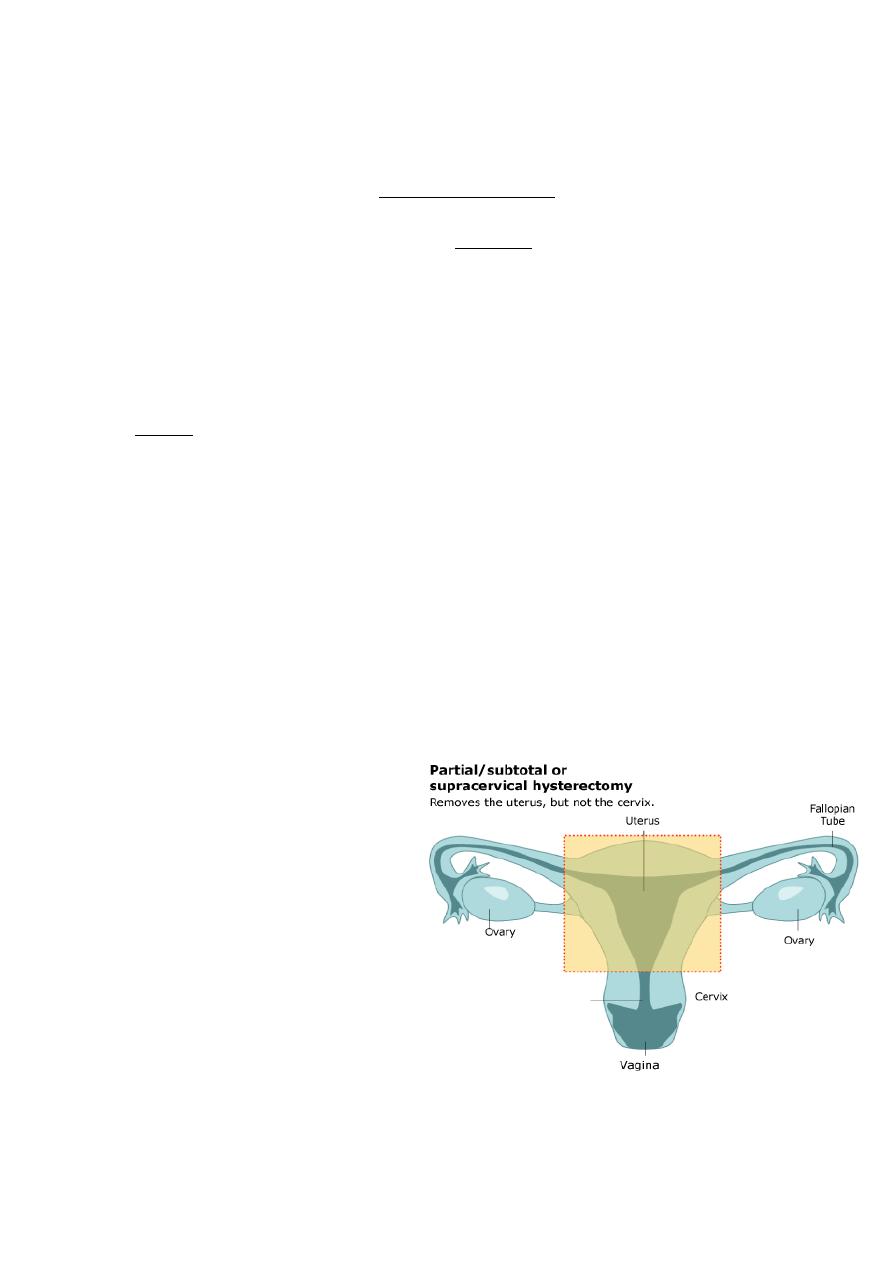
Types
Hysterectomy, in the literal sense of the word, means merely
removal of the uterus. However other organs such as ovaries, fallopian
tubes and the cervix are very frequently removed as part of the surgery.
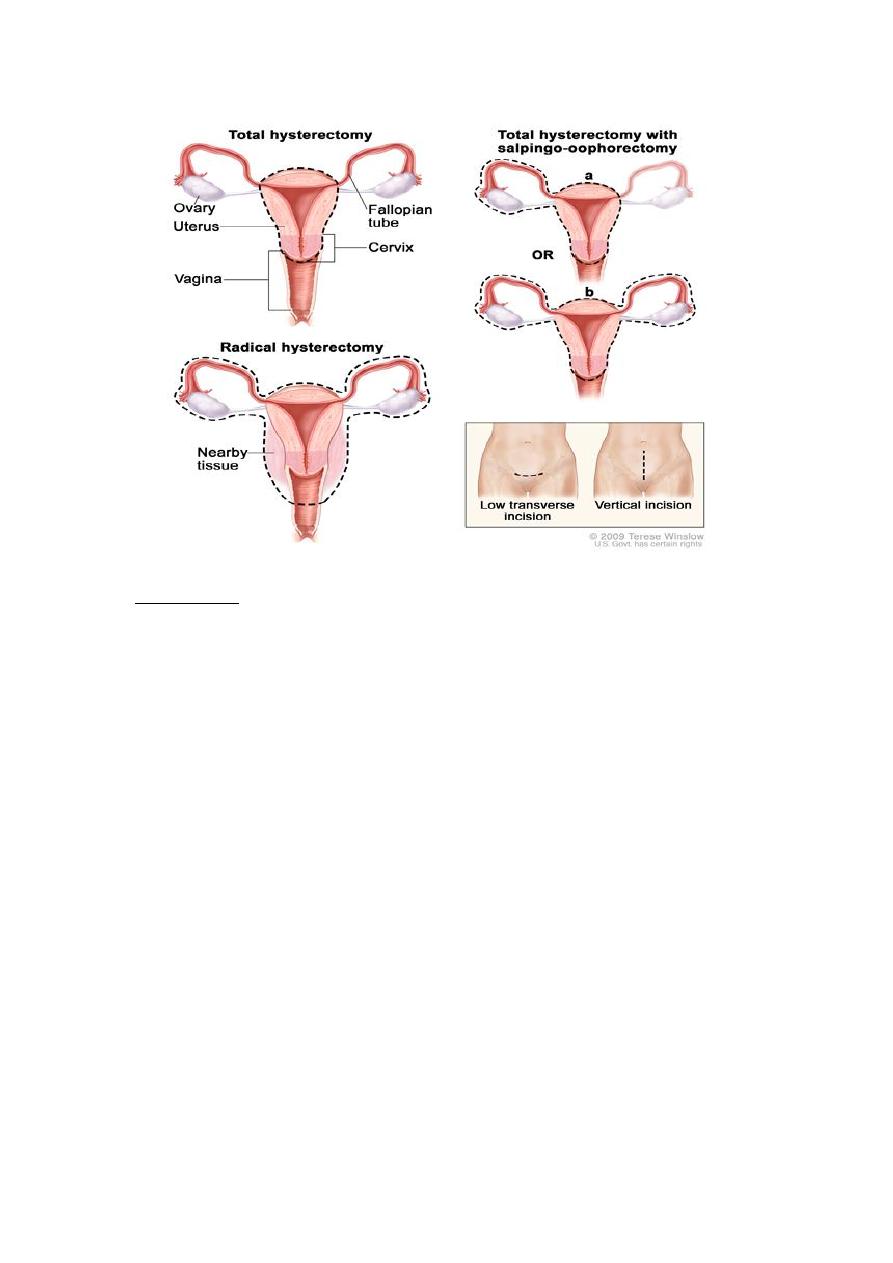
1)
Radical hysterectomy: complete removal of the uterus, cervix,
upper vagina, and parametrium. Indicated for cancer. Lymph
nodes, ovaries and fallopian tubes are also usually removed in this
situation, such as in Wertheim's hysterectomy.
2)
Total hysterectomy: Complete removal of the uterus and cervix,
with or without oophorectomy.
3)
Subtotal hysterectomy:
removal of the uterus,
leaving the cervix in situ.
Supracervical (subtotal)
hysterectomy does not
eliminate the possibility
of having cervical cancer
since the cervix itself is
left intact and may be
contraindicated
in
women with increased
risk of this cancer.
Regular pap smears to check for cervical dysplasia or cancer are
still needed after subtotal hysterectomy.
Technique
v
Abdominal hysterectomy
It is done via laparotomy (abdominal incision, not to be confused
with laparoscopy). A transverse (Pfannenstiel) incision is made through
the abdominal wall, usually above the pubic bone, as close to the upper
hair line of the individual's lower pelvis as possible, similar to the incision
made for a caesarean section. This technique allows doctors the greatest
access to the reproductive structures and is normally done for removal
of the entire reproductive complex.
The recovery time for an open hysterectomy is 4–6 weeks and
sometimes longer due to the need to cut through the abdominal wall.
Historically, the biggest problem with this technique were
infections, but infection rates are well-controlled and not a major
concern in modern medical practice.
An open hysterectomy provides the most effective way to explore
the abdominal cavity and perform complicated surgeries.

v
Vaginal hysterectomy
Vaginal hysterectomy is performed entirely through the vaginal
canal and has clear advantages over abdominal surgery such as fewer
complications, shorter hospital stays and shorter healing time.
Abdominal hysterectomy, the most common method, is used in
cases such as after caesarean delivery, when the indication is cancer,
when complications are expected or surgical exploration is required.
v
Laparoscopic-assisted vaginal hysterectomy
With the development of the laparoscopic techniques in the 1970-
1980s, the "laparoscopic-assisted vaginal hysterectomy" (LAVH) has
gained great popularity among gynecologists because compared with
the abdominal procedure it is less invasive and the post-operative
recovery is much faster.
It also allows better exploration and slightly more complicated
surgeries than the vaginal procedure. LAVH begins with laparoscopy and
is completed such that the final removal of the uterus (with or without
removing the ovaries) is via the vaginal canal.
Thus, LAVH is also a total hysterectomy, the cervix must be
removed with the uterus.
v
Laparoscopic-assisted supracervical hysterectomy
The "laparoscopic-assisted supracervical hysterectomy" (LASH)
was later developed to remove the uterus without removing the cervix
using a morcellator which cuts the uterus into small pieces that can be
removed from the abdominal cavity via the laparoscopic ports
v
Total laparoscopic hysterectomy
TLH is performed solely through the laparoscopes in the abdomen,
starting at the top of the uterus, typically with a uterine manipulator.
The entire uterus is disconnected from its attachments using long
thin instruments through the "ports". Then all tissue to be removed is
passed through the small abdominal incisions.
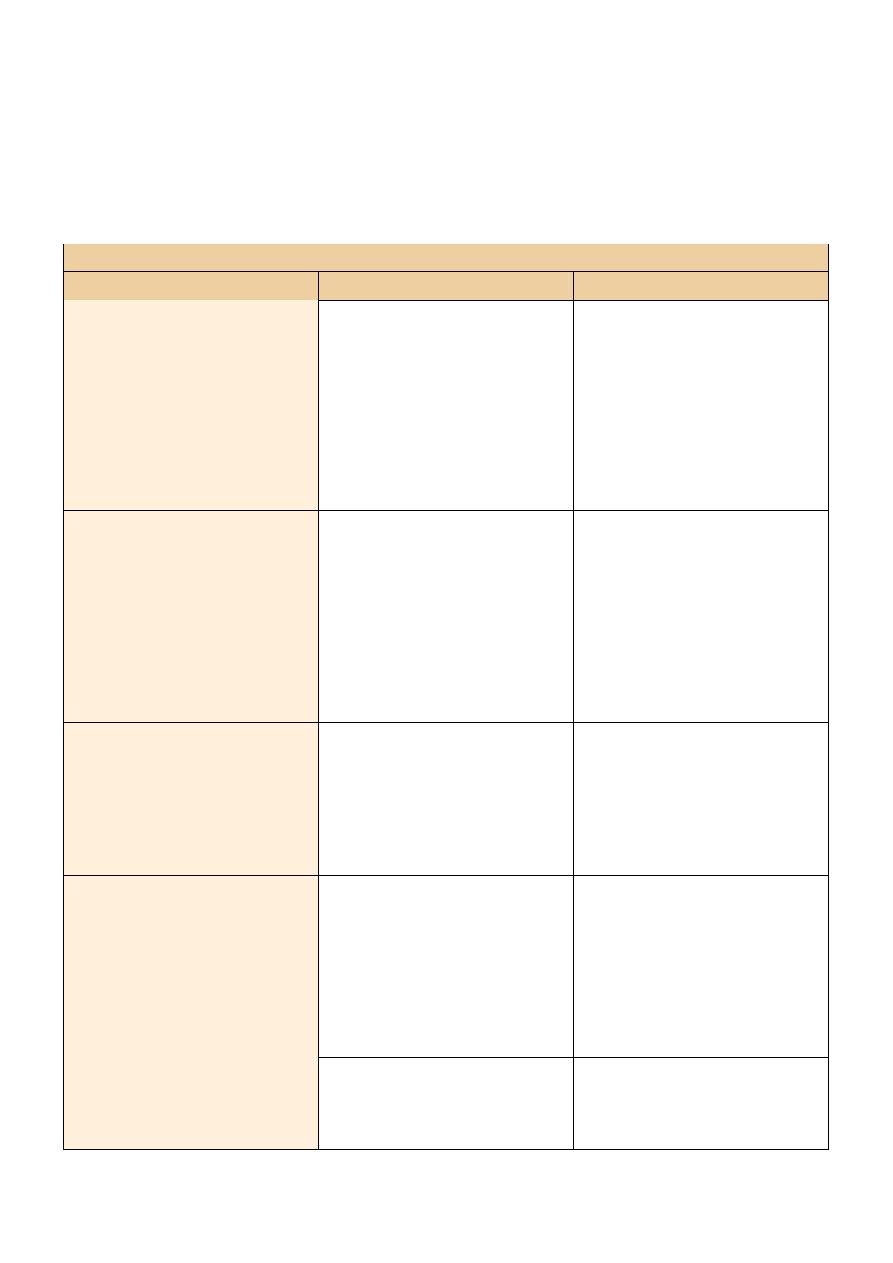
Advantages and disadvantages of different hysterectomy techniques
Technique
Benefits
Disadvantages
Abdominal hysterectomy
• No limitation by the
size of the uterus
• Combination with
reduction and
incontinence surgery
possible
• Longest duration of
hospital treatment
• Highest rate of
complications
• Longest recovery
period
Vaginal hysterectomy
• Shortest operation
time
• Short recovery period
• Combination with
reduction operations
are possible
• Limitation by the size
of the uterus and
previous surgery
• Highest blood loss
• Limited ability to
evaluate the fallopian
tubes and ovaries
Laparoscopic supracervical
hysterectomy
• Low risk of
complication
• Less blood loss
• Short inpatient
treatment duration
• 10-17% of patients
continue to have
minimal menstrual
bleeding
Laparoscopic-assisted
vaginal hysterectomy
• Possible even with
larger uterus and after
previous surgery
• Combination with
reduction operations
are possible
• Long operation time
• High instrumental
costs by changing the
access path
Total laparoscopic
hysterectomy
• Less blood loss
• Short inpatient
treatment duration
• None to date
Adverse effects and Complications
Hysterectomy has like any other surgery certain risks and side
effects.
There is a risk of general anesthesia, DVT, And pulmonary embolism.
Short term mortality (within 40 days of surgery) is usually reported in
the range of 1–6 cases per 1000 when performed for benign causes. The
mortality rate is several times higher when performed in patients that
are pregnant, have cancer or other complications.
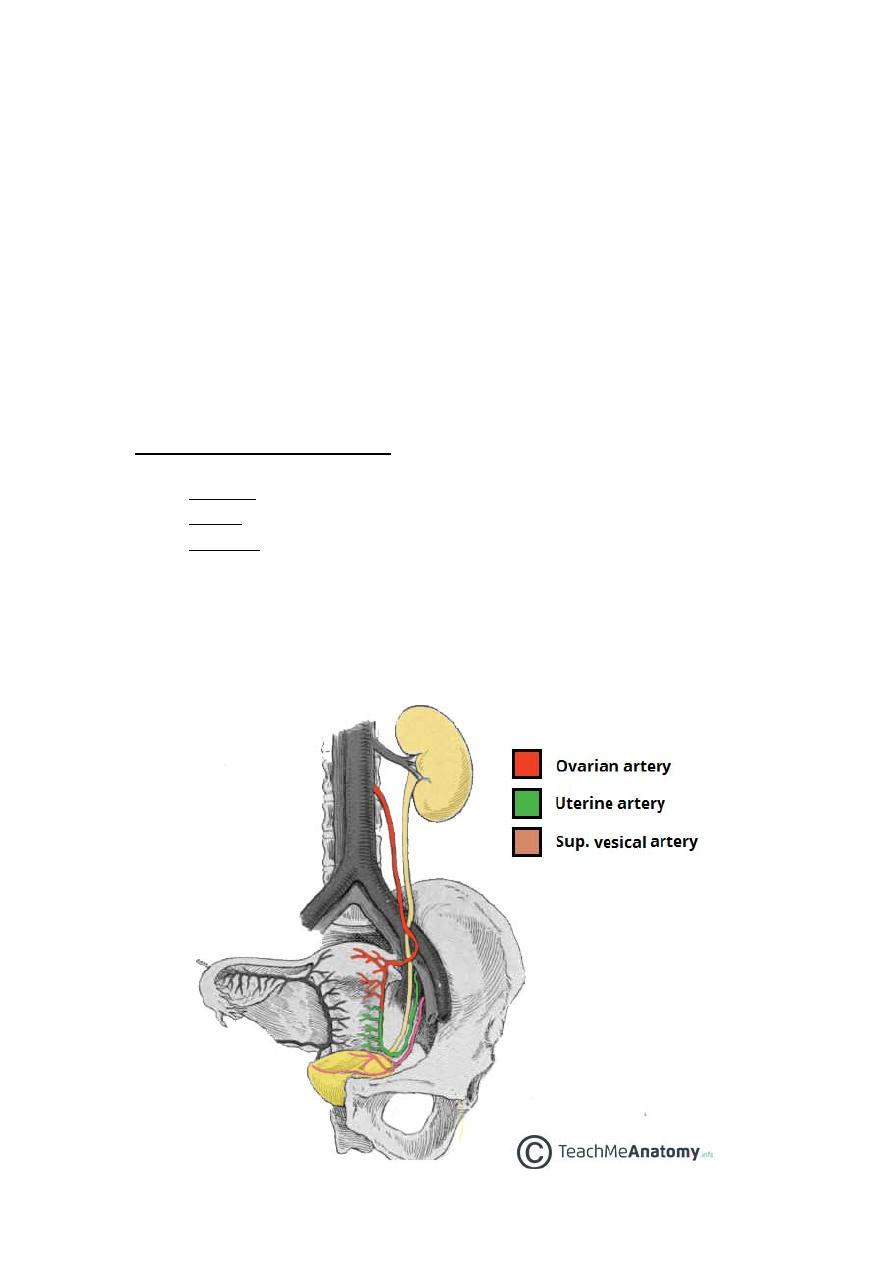
Injury to adjacent organs:
o
Bladder injury.
o
Bowel injury.
o
Ureteral injury is not uncommon and can range from 2.2% to 3%
depending on whether the modality is abdominal, laparoscopic, or
vaginal. The injury usually occurs in the distal ureter close to the
infundibulopelvic ligament or as a ureter crosses below the
uterine artery, often from blind clamping and ligature placement
to control hemorrhage.
Convalescence
Hospital stay is 3 to 5 days or more for the abdominal procedure
and between 2 to 3 days for vaginal or laparoscopically assisted vaginal
procedures.
Time for full recovery is very long and largely independent on the
procedure that was used. Depending on the definition of "full recovery"
3 to 12 months have been reported. Serious limitations in everyday
activities are expected for a minimum of 4 months.
Unintended oophorectomy and premature ovarian failure
Removal of one or both ovaries is performed in a substantial
number of hysterectomies that were intended to be ovary sparing.
The general extraction by surgery of an ovary and a fallopian tube
is called unilateral salpingo-oophorectomy, but if both pairs of ovaries
and fallopian tubes are surgically removed the process is called a
bilateral salpingo-oophorectomy.
The procedure is carried out to treat ovarian cancers or other
gynecological cancers, also pelvic inflammatory disease or relative
infections. In some instances the extraction of one or both ovaries is
recommended to treat a condition called endometriosis.
The average onset age of menopause in those who underwent
hysterectomy is 3.7 years earlier than average even when the ovaries
are preserved.
Effects on sexual life and pelvic pain
After hysterectomy for benign indications the majority of women
report improvement in sexual life and pelvic pain. A smaller share of
women report worsening of sexual life and other problems.
Premature menopause and its effects
Estrogen levels fall sharply when the ovaries are removed,
removing the protective effects of estrogen on the cardiovascular and
skeletal systems.
This condition is often referred to as "surgical menopause",
although it is substantially different from a naturally occurring
menopausal state; the former is a sudden hormonal shock to the body
that causes rapid onset of menopausal symptoms such as hot flashes,
while the latter is a gradually occurring decrease of hormonal levels over
a period of years with uterus intact and ovaries able to produce
hormones even after the cessation of menstrual periods.
Consequences of this is cardiovascular disease, osteoporosis
(decrease in bone density) and increased risk of bone fractures.
This has been attributed to the modulatory effect of estrogen on
calcium metabolism and the drop in serum estrogen levels after
menopause can cause excessive loss of calcium leading to bone wasting.
Urinary incontinence and vaginal prolapse
Urinary incontinence and vaginal prolapse are well known adverse
effects that develop with high frequency a very long time after the
surgery. Typically, those complications develop 10–20 years after the
surgery.
Vault prolapse complicate 1% of total hysterectomy.
Adhesion formation and bowel obstruction
The formation of postoperative adhesions is a particular risk after
hysterectomy because of the extent of dissection involved as well as the
fact that hysterectomy wound is in the most gravity-dependent part of
the pelvis into which a loop of bowel may easily fall.
Uterine Myomectomy
Myomectomy, sometimes also fibroidectomy, refers to the
surgical removal of uterine leiomyomas, also known as fibroids. In
contrast to a hysterectomy the uterus remains preserved and the
woman retains her reproductive potential.
Indications
The presence of a fibroid does not mean that it needs to be
removed. Removal is necessary when the fibroid causes pain or
pressure, abnormal bleeding, or interferes with reproduction. The
fibroids needed to be removed are typically large in size, or growing at
certain locations such as bulging into the endometrial cavity causing
significant cavity distortion.
Procedure
A Myomectomy can be performed in a number of ways,
depending on the location and number of lesions and the experience
and preference of the surgeon. Either a general or a spinal anesthesia is
administered.
v
Laparotomy
Traditionally a myomectomy is performed via a laparotomy with a
full abdominal incision, either vertically or horizontally. Once the
peritoneal cavity is opened, the uterus is incised, and the lesion(s)
removed. The open approach is often preferred for larger lesions. One
or more incisions may be set into the uterine muscle and are repaired
once the fibroid has been removed. Recovery after surgery takes six to
eight weeks.
v
Laparoscopy
Using the laparoscopic approach the uterus is visualized and its
fibroids located and removed. Morcellators are available to shred larger
fibroids so that they can be removed through the small port holes of
laparoscopy.
Studies have suggested that laparoscopic Myomectomy leads to
lower morbidity rates and faster recovery than does laparotomic
myomectomy.
As with hysteroscopic myomectomy, laparoscopic myomectomy is
not generally used on very large fibroids (3-10cm).
v
Hysteroscopy
A fibroid that is located in a submucous position (that is,
protruding into the endometrial cavity) may be accessible to
hysteroscopic removal. This may apply primarily to smaller lesions not
greater than 5 cm.
Complications and risks
Complications of the surgery include:
o
The possibility of significant blood loss leading to a blood
transfusion.
o
The risk of adhesion or scar formation around the uterus or within
its cavity.
o
It is well known that myomectomy surgery is associated with a
higher risk of uterine rupture in later pregnancy. Thus, women
who have had myomectomy (with the exception of small
submucosal myoma removal via hysteroscopy, or largely
pedunculated myoma removal) should get Cesarean delivery to
avoid the risk of uterine rupture that is commonly fatal to the
fetus.
o
It may not be possible to remove all lesions, nor will the operation
prevent new lesions from growing. Development of new fibroids
will be seen in 42-55% of patients undergoing a myomectomy.
Cervical Polypectomy
Cervical polypectomy is a procedure to remove small tumors
(polyps), often growing on a stalk, from the opening of the cervix or
inside the cervical canal (endocervix). The polyps are generally
noncancerous (benign).
Cervical polyps are caused by an overgrowth of normal tissue.
They are relatively common and most do not cause symptoms. Cervical
polyps are frequently the result of infection, and may be linked to
chronic inflammation, an abnormal response to higher levels of
estrogen, or local congestion of cervical blood vessels.
Reasons for Procedure
Cervical polyps do not usually cause symptoms. Some individuals
may experience light bleeding or spotting caused by irritation from a
tampon or sexual intercourse (postcoital bleeding).
Polyps are generally removed because of this bleeding, or to
prevent additional future irritation and bleeding. Although most polyps
are benign, all should be removed and examined because cancerous
(malignant) changes may develop; some cervical cancers first appear as
polyps.
How Procedure is Performed
Polypectomy is usually an outpatient procedure performed in the
physician's office. It is generally painless, so no anesthesia is required.
The woman lies on the exam table with her legs in the stirrups
(lithotomy position); a speculum is then inserted into the vagina to hold
it open to visualize the cervix. The cervix is cleansed using a vaginal swab
soaked in an antiseptic solution. The polyp is grasped with a surgical
clamp (hemostat), twisted several times, and pulled until it is freed. The
polyp is sent for microscopic examination (pathology) to rule out cancer.
The base of the polyp is then removed by scraping it off with a sharp
surgical instrument (curettage), or by using heat, cold, or chemicals to
destroy the tissue (cauterization).
If the polyp is large, or if it is attached by a broad base rather than
a stalk, it may need to be cut off and the wound stitched (sutured)
closed. This procedure may be done under local anesthesia in the
hospital because of the possible risk of excessive bleeding
(hemorrhage).
If the cervix is soft, distended, or partially opened, and the polyp is
large or not clearly visible, dilation and curettage (D&C) will be done.
The cervical opening will be widened (dilated) so that the cervical canal
and uterus may be examined for other polyps. All removed polyps will
be biopsied for evidence of cancer.
Complications of cervical polypectomy
Complications following cervical polypectomy are rare; however,
hemorrhage and infection can occur.
Cone Biopsy (Conization) for Abnormal Cervical Cell
Changes
A cone biopsy is an extensive form of a cervical biopsy. It is called
a cone biopsy because a cone-shaped wedge of tissue is removed from
the cervix and examined under a microscope. A cone biopsy removes
abnormal tissue that is high in the cervical canal. A small amount of
normal tissue around the cone-shaped wedge of abnormal tissue is also
removed so that a margin free of abnormal cells is left in the cervix.
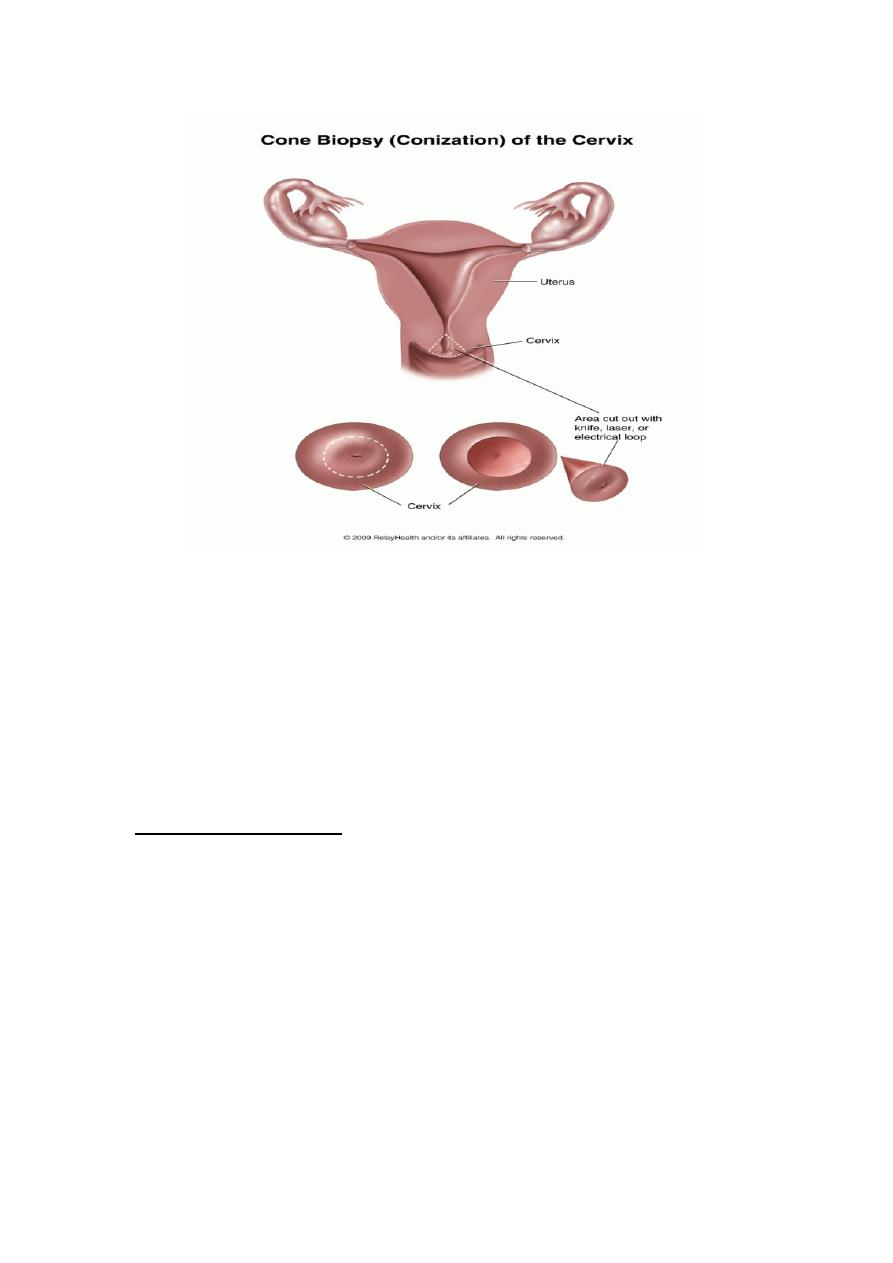
A
sample of tissue can be removed for a cone biopsy using:
}
A surgical knife (scalpel).
}
A carbon dioxide (CO2) laser.
}
Loop electrosurgical excision procedure (LEEP)
Risks of cone biopsy:
§
A few women may have serious bleeding that requires further
treatment.
§
Narrowing of the cervix (cervical stenosis) that causes infertility
may occur (rare).
§
Inability of the cervix to stay closed during pregnancy
(incompetent cervix) may occur. Women who have had a cone
biopsy may have an increased risk of miscarriage or preterm
delivery
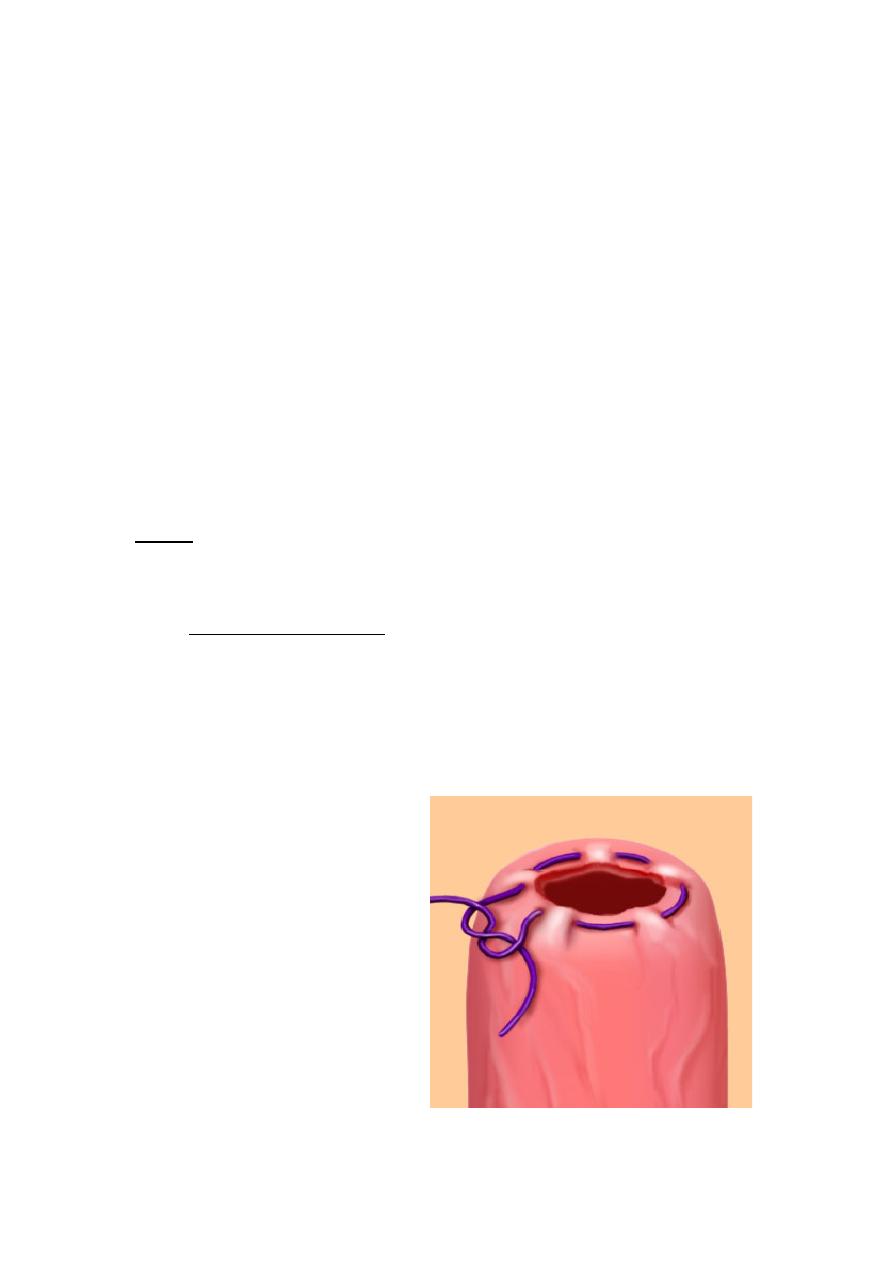
Cervical cerclage
Cervical cerclage (tracheloplasty), also known as a cervical stitch,
is used for the treatment of cervical incompetence (or insufficiency), a
condition where the cervix has become slightly open and there is a risk
of miscarriage because it may not remain closed throughout pregnancy.
Usually this treatment would be done, in the second trimester of
pregnancy, for a woman who had either suffered from one or more
miscarriages in the past, or is carrying multiples.
The treatment consists of a strong suture being inserted into and
around the cervix early in the pregnancy, usually between weeks 12 to
14, and then removed towards the end of the pregnancy when the
greatest risk of miscarriage has passed.
Types
There are three types of cerclage:
1)
A McDonald cerclage, is essentially a purse string stitch; the
cervix stitching involves a band of suture at the upper part of the
cervix while the lower part has already started to efface. This
cerclage is usually placed between 12 weeks and 14 weeks of
pregnancy. The stitch is generally removed around the 37th week
of gestation.
Purse string suture
Placed in a circular
motion around a lumen
and then tightened to
invert the opening
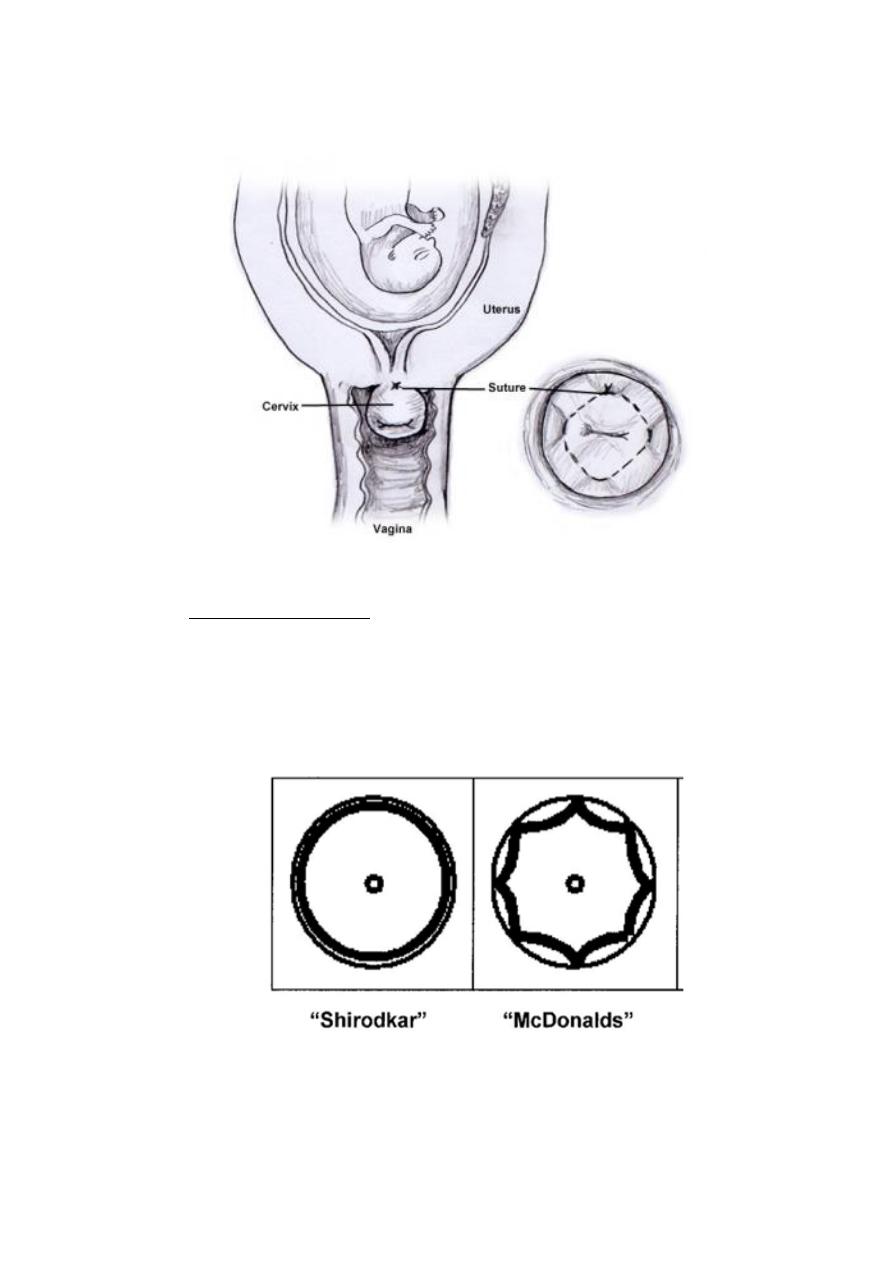
McDonald's cerclage
2)
A Shirodkar cerclage is very similar, but the sutures pass through
the walls of the cervix so they're not exposed. This type of
cerclage is less common and technically more difficult than a
McDonald, and is thought (though not proven) to reduce the risk
of infection.

3)
An abdominal cerclage, the least common type, is permanent
and involves stitching at the very top of the cervix, inside the
abdomen. This is usually only done if the cervix is too short to
attempt a standard cerclage, or if a vaginal cerclage has failed or is
not possible.
Risks of cerclage
While cerclage is generally a safe procedure, there are a number of
potential complications that may arise during or after surgery. These
include:
• risks associated with regional or general anesthesia
• premature labor
• premature rupture of membranes
• infection of the cervix
• infection of the amniotic sac (chorioamnionitis)
• cervical rupture (may occur if the stitch is not removed before
onset of labor)
• injury to the cervix or bladder
• bleeding
• Cervical Dystocia with failure to dilate requiring Cesarean Section
