AFTER MID
TOTAL LEC: 32
Gynaecology
Dr. Yusra
Lec 32 - Urinary Fistulas
DR. YUSRA - LEC 4
مكتب املدينة

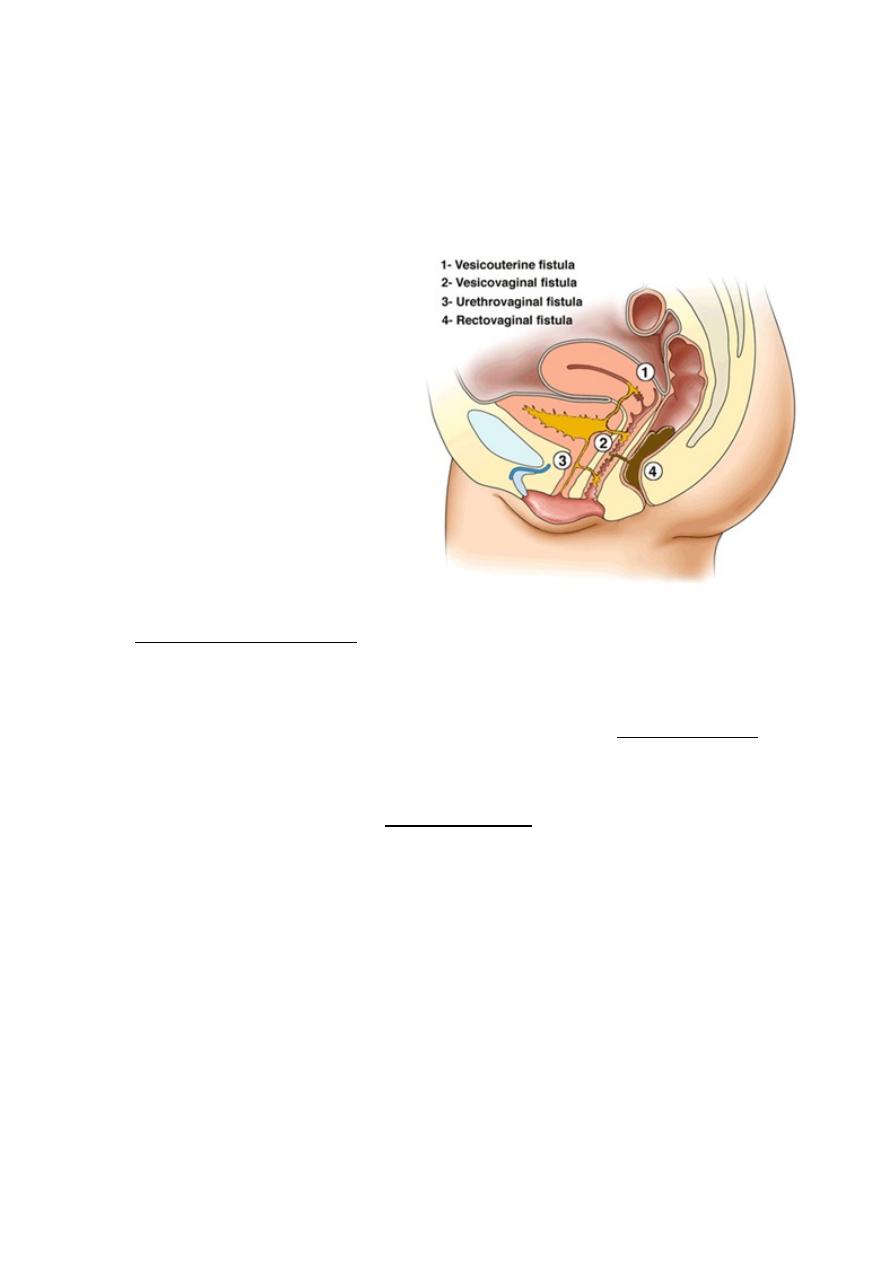
Urinary Fistulas
The development of a genitourinary fistula has profound effects on both
the physical and psychological health of the woman.
The most common simple
genitourinary fistulas are:
• Vesicovaginal (42 %)
• Ureterovaginal (34 %)
• Urethrovaginal (11 %)
• Vesicocervical (3 %)
Vesicovaginal fistula
Etiology:
The most common cause of vesicovaginal fistulas in the developed world
is gynecological surgery. Among those surgeries, the one with the
highest incidence of post operative fistula formation is hysterectomy
(75% of cases). While In the developing world, the most common cause
remains obstetric trauma (the incidence is 1-3/1000 deliveries).
Particular risk factors include:
o Distorted anatomy, for example previous surgery, fibroids or
endometriosis.
o Other procedures include anterior colporrhaphy, laparoscopic
pelvic surgery and urological surgery.
o Pelvic malignancy, trauma and radiotherapy.
Presentation:
The majority present with continuous leakage of urine, this
usually leads to discomfort and excoriation in the genital region but
If
the fistula is small, a woman may just complain of increased vaginal
discharge.
The timing of presentation is variable, although the most
common time to present is 5- 10 days following surgery.
Diagnosis:
A large fistula is usually obvious and may be easily seen by
examining the woman in the left lateral position using simm's speculum.
If no fistula can be seen, a useful diagnostic test is the introduction of
methylene blu into the bladder via a urethral catheter,
the blue dye may
then be seen draining into the vagina. Alternatively, Bonneys three
swab test (in which three swabs are placed in the vagina prior to
instilling the dye) may help to locate the site of fistula.
Intravenous urogram (IVU) is not usually helpful in the diagnosis of
vesicovaginal fistula but is mandatory to rule out a ureterovaginal fistula
or ureteric obstruction.
When the woman is anaesthetized, it is often possible to palpate the
vaginal opening of the fistula tract.
If not, the vesical opening can also be
seen on the posterior wall or at the bladder base using cystoscopy.
If the fistula is not related to surgery both vaginal and vesical openings
should be biopsied to exclude the possibility of malignancy.
This box was added by the students: The standard three-swab test was performed
to differentiate between vesicovaginal and ureterovaginal fistula and to rule out
stress incontinence. In this test, 100 ml of 1:5 diluted methylene blue solution was
instilled into the bladder via a urethral catheter after three dry sterile swabs were
placed in the upper, middle and lower third of the vagina. The patient was asked to
walk around for ten minutes, after which the swabs were removed and examined. If
the lower swab is wet and stained blue, it indicates stress incontinence. If the upper
swabs are wet and blue, that indicates vesicovaginal fistula, and if the upper swabs
are wet but not stained blue, it is an indication of ureterovaginal fistula.
Treatment
Treatment options range from simple conservative measures to more
complex surgical procedures .
o
Barrier creams may help prevent the skin becoming sore and
excoriated.
o
Advice about incontinence pads, the increased risk of urinary tract
infection and in some cases the need for prophylactic antibiotics.
Urethrovaginal fistula
In the developed world, these occur most commonly following an
anterior repair with or without a vaginal hysterectomy. Urethrovaginal
fistula may also develop as a result of a urethral diverticulum (or its
repair) or following bladder neck suspension procedures.
In the developing world, the overwhelming majority are again caused by
childbirth.
Symptoms
(vary depending on the site of fistula).
A fistula high up in the urethra may present with continuous
incontinence. If the fistula is near the bladder neck, stress incontinence
and recurrent urinary tract infections can be the presenting symptoms.
When the fistula is lower down, it may cause symptom of spraying of
urine at micturition or post –micturition dribble.
Treatment
: surgical and women are referred to specialized centers.

