AFTER MID
TOTAL LEC: 28
Gynaecology
Dr. Shaima’a Kadhim Al-Khafaji
Lec 28 - Abnormal Uterine Bleeding
DR. SHAIMA’A - LEC 1
مكتب املدينة

Abnormal Uterine Bleeding
Normal menstrual cycle:
v
Mean duration of menstrual cycle: 28 days.
Range: 21-35 days
v
Average duration of menses: 2-7 days.
v
Average blood loss is 80 ml.
Abnormal uterine bleeding:
is any disturbance in regularity,
duration, or amount of menstrual loss.
Terms used to describe various forms of Abnormal uterine bleeding:
1) Heavy menstrual bleeding (menorrhagia) (hypermenorrhea):
excess in amount (loss of more than 80 ml) and duration of
uterine menstrual bleeding, with regular intervals.
2) Hypomenorrhea: decreased uterine menstrual bleeding in
amount and duration with regular intervals.
3) Polymenorrhea: episodic menstrual flow at intervals less than 21
days (frequent menstrual flow).
4) Oligomenorrhea: episodic menstrual flow at intervals more than
35 days (infrequent menstrual flow).
5) Metrorrhagia: uterine bleeding at irregular intervals.
Combination of these terms may be used. For example,
metromenorrhagia which means excessive bleeding at irregular
intervals.

Heavy menstrual bleeding: (HMB)
The presentation of HMB is common, e.g. each year in UK, 5% of
women between 30-49 years of age consult their doctors with this
complaint.
Etiology:
1. fibroids.
2. Endometrial polyps.
3. Coagulation disorders: 10-20% of women with heavy menstrual
bleeding have a systemic disorder of coagulation. The most
common inherited disorder is Von Willebrand’s disease which is
found in 13% of female with HMB. Acquired disorders include
severe thrombocytopenia.
4. Pelvic inflammatory disease: data do exist to support an
association between chronic infection and HMB e.g. Chlamydia
trachomatis infection.
5. Thyroid disease: untreated hypothyroidism leads to anovulation
that typically present with amenorrhea, but this endocrine
disorder may be also associated with HMB.
6. Malignancy: both endometrial and cervical cancer are potential
causes for HMB and postcoital bleeding.
7. Iatrogenic causes: include drugs like warfarin and drugs that
affect ovulation by disruption of the hypothalamic-pituitary
ovarian axis like tricyclic antidepressants and phenothiazine.
IUCD may be associated with HMB and the effect is thought to be
due to local inflammatory process.
8. Arteriovenous malformation: is congenital or acquired localized
collection of abnormally connected arteries and veins, when they
are in the uterus they can be associated with attacks of excessive
bleeding.
9. Bleeding of endometrial origin (BEO): Despite appropriate
investigations, often no pathology can be identified, BEO is a
diagnosis of exclusion. BEO replaces the older term (dysfunctional
uterine bleeding DUB).
The exact cause is still an area of research but is thought to be due
to disordered endometrial prostaglandin production, as well as
abnormalities of endometrial vascular development.
Control of menstrual blood loss is mainly by vasoconstriction.
Factors regulating vascular tone thus play an important role and include
prostaglandins, endothelin and nitric oxide. For example: reduced
endometrial expression of endothelin (a vasoconstrictor) has been
described in women with HMB.
Also studies showed increased level of total prostaglandins in the
endometrium of women with HMB. Therefore administration of Cox
inhibitors is a first line treatment during menses for women with HMB.
Homeostasis in the endometrium differs from homeostasis
elsewhere in the body. Platelets in the endometrial cavity are
deactivated. The endometrium is a rich source of plasminogen
activators but coagulation is rapidly reversed by marked fibrinolysis.
Because the menstrual loss is mainly controlled by vasoconstriction,
There is a lesser need for coagulation.
Women with HMB are reported to have increased fibrinolytic
activity, therefore Antifibrinolytic commonly prescribed for complaint
of HMB, they reduce blood loss by 40-50%.
History:
Useful questions to ask:
-
How often does the patient need to change soaked sanitary
napkins.
-
Does she notice passing clots, is the bleeding so heavy leading to
flooding (it spills over clothes, bedding??).
-
Does she need to take any time off work and need to be confined
to her house? (i.e. we want to determine the impact of HMB on
the quality of life).
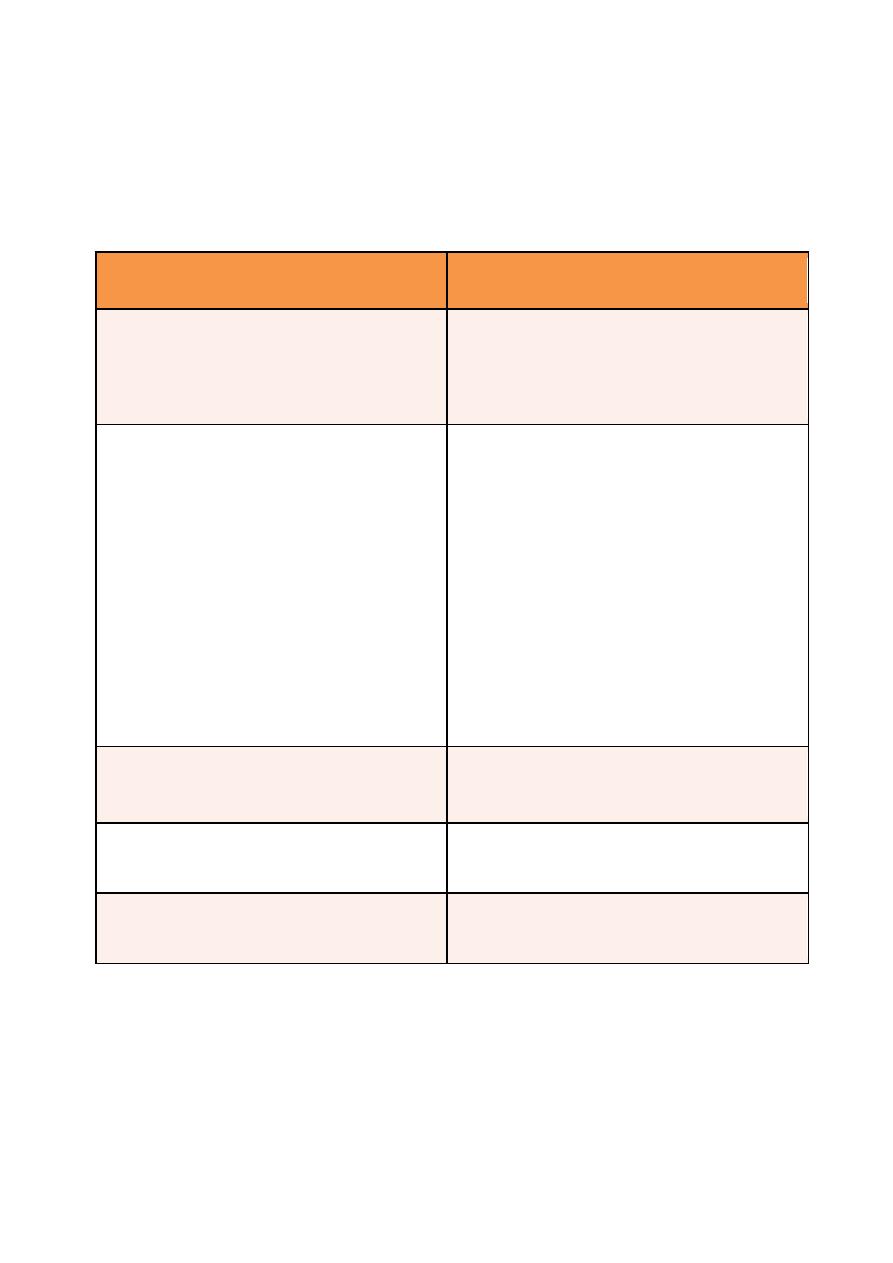
Symptoms which can be associated with HMB and related pathologies
Suggestive of:
Associated symptoms
Endometrial or cervical polyp
§
Irregular bleeding
§
Intermenstrual bleeding
§
Postcoital bleeding
Coagulation disorder (coagulation
disorders will be present in 20% of
those presenting with ‘unexplained’
heavy menstrual bleeding.)
-
Excessive
bruising/bleeding
from other sites
-
History
of
postpartum
haemorrhage (PPH)
-
Excessive
postoperative
bleeding
-
Excessive bleeding with dental
extractions
-
Family history of bleeding
problems
Pelvic inflammatory disease
Unusual vaginal discharge
Pressure from fibroids
Urinary symptoms
Thyroid disease
Weight change, skin changes, fatigue
Examination:
1. General examination for signs of anemia, systemic coagulation
disorders (bruising and petechiae), or thyroid disease (goiter).
2. Abdominal and pelvic examination to assess for any mass.
Speculum examination to visualize the cervix for polyps,
carcinoma, and discharge suggesting infection. Swabs can be taken if
pelvic infection is suspected, smear to be taken if one is due.
Bimanual examination should be performed to elicit uterine
enlargement.
Investigations:
1)
Full blood count: should be done in all women with HMB, to
ascertain the need for iron therapy and sometimes blood
transfusion.
2)
Thyroid function test: when history is suggestive of thyroid
disease.
3)
Endocervical/ high vaginal swabs: when unusual vaginal discharge
is reported or observed on examination, or if there are risk factors
for PID.
4)
Coagulation screen: if history and examination are suggestive of
coagulation disorder with referral to hematological opinion.
5)
Colposcopic examination: suspicion of cervical malignancy.
6)
Evaluation of the uterus and its cavity by pelvic US including saline
infusion sonography and outpatient hysteroscopy, done when:
v
A pelvic mass is palpated on examination e.g. fibroid.
v
When there is intermenstrual or postcoital bleeding
suggestive of endometrial polyp.
v
When drug therapy for HMB is unsuccessful.
v
When there is irregular HMB.

MRI should be considered when uterine conservation is desired in
females with fibroids and US is unsuccessful in determining the depth of
myometrial involvement of a fibroid. The MRI precision in the
localization of submucosal fibroid can be obviate the need for
hysterectomy and permit hysteroscopic resection of the fibroid.
7) Histological assessment of the endometrium i.e. endometrial
biopsy should be performed in:
v
Those aged > 45 years.
v
Younger women when medical treatment has failed.
v
If irregular or intermenstrual bleeding.
v
All women prior to surgical intervention.
There are many methods for taking endometrial sample:
A. Pipelle endometrial biopsy can be performed in the outpatient
setting.
B. Outpatient hysteroscopy is indicated if:
o Pipelle biopsy attempt fails.
o Pipelle biopsy is insufficient for Histopathological
assessment.
o There is abnormality in US suggesting polyp or submucus
fibroid.
o Patient is known to poorly tolerate speculum examination.

C. If the patient fails to tolerate an outpatient procedure or the
cervix need to be dilated to enter the cavity, then hysteroscopy
and endometrial biopsy under GA may be required.
When hysteroscopy is not available then dilatation and curettage
to get endometrial biopsy under GA is done.
Management of Heavy Menstrual Bleeding
For some women, demonstrating that their blood loss is in fact
‘normal’ may be sufficient to reassure them, and make further
treatment unnecessary.
When treatment is required, it is important to consider and
discuss the following points in order to choose the most suitable
treatment options:
o Patient’s preference of treatment.
o Risk/benefit of each option.
o Contraceptive
requirement
(family
complete,
current
contraceptive).
o Past medical history.
o Any contraindication to medical therapies for HMB.
o Suitability for anesthesia, previous surgical history.
Medical Treatment
Non-hormonal treatment:
If a woman is wishing to conceive, hormonal treatment and most
surgical interventions are unacceptable.
a) Prostaglandin synthetase inhibitors:
as NSAIDs. Mefenamic
acid is the most frequently used agent, and is associated with a
reduction in mean menstrual loss of 20-25%.
Benefits: analgesia, hence helps when there is also dysmenorrhea.
Disadvantage: contraindicated with a history of duodenal ulcer or
severe asthma. There are also isolated reports of NSAIDs -
associated reversible female infertility, probably due to non
rupture of mature follicle.
Recommended dose: is 500mg PO tds (three times daily) during
menstruation.
b) Antifibrinolytic:
such as tranexamic acid. It reduces blood loss
by up to 50%.
Benefits: needs to be taken on days when bleeding is particularly
heavy. It is compatible with ongoing attempts at conception.
Disadvantage: gastrointestinal symptoms. Concerns that it may
increase risk of venous thrombosis, but this has not been proved
by the studies that have investigated it to date.
Recommended Dose: 1g PO qds (four times daily) when heavy
menstruating.
Hormonal treatment:
a)
COCP: Combined oral contraceptive pills
Benefits: effective in management of HMB, and offers a
contraceptive effect especially when taken properly.
Disadvantages:
§
Contraindicated in patients who have risk factors for
thromboembolism.
§
Unsuitable for patients > 35 years old who smoke.
§
Unsuitable if there is personal or family history of CA
breast.
§
Unsuitable for patients who are grossly overweight.
b)
Norethisterone:
It is an oral progesterone, it is helpful in the
management of women with irregular (anovulatory) HMB at the
extremes of reproductive life.
Benefits: safe and effective which can regulate bleeding pattern.
Disadvantage: it is not a contraceptive, can cause breakthrough
bleeding.
Recommended Dose: given in cyclical pattern from day 6 to day
26 of menstrual cycle as 5-10mg tds.
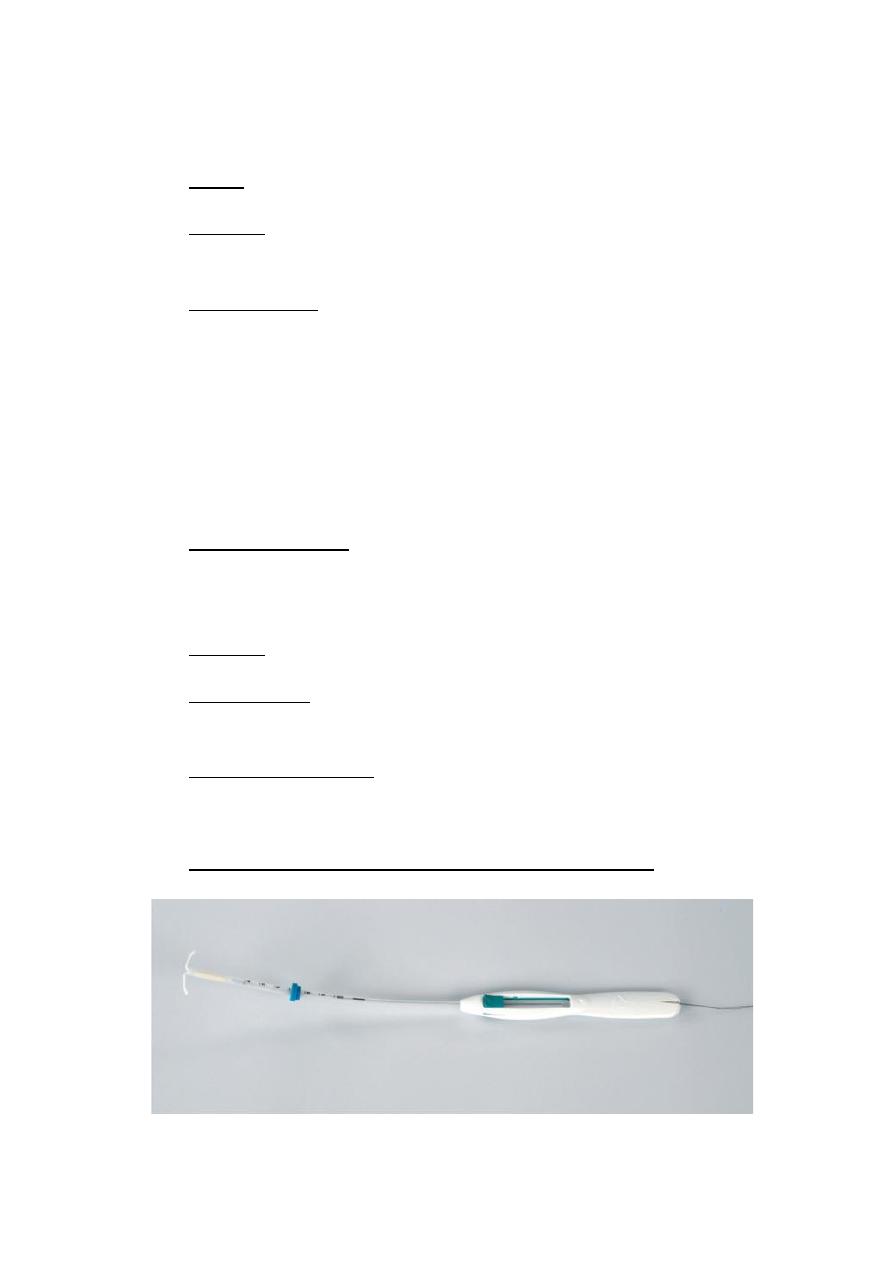
c)
Levonorgestrel - releasing intrauterine system:
It provides a highly effective alternative to surgical treatment.
Mean reduction of menstrual blood loss of around 95% by one year
after LNG-IUS insertion.
Benefits:
a. Provides contraceptive cover comparable with sterilization.
b. Evidence proves it is effective for associated dysmenorrhea.
c. Around 30% of women are amenorrhic by one year after insertion.
Disadvantage:
irregular menses and breakthrough bleeding for the first 3-9
months after insertion.
LNG-IUS may be inserted in the outpatient setting and requires
changes every 5 years.
d)
GnRH agonists:
they act by down regulating the HPO axis and
induce ovarian suppression leading to amenorrhea.
Benefits: effective for associated dysmenorrhea.
Disadvantages:
o They can cause irregular bleeding.
o They can be associated with flushing and sweating.
o Only suitable for short term usage (6 months), because of
their effect on bone density.
Their beneficial effect does not continue after stopping treatment.
Surgical Treatment
There are many options depending on the underlying pathology.
1. Polypectomy:
Endocervical polyp can be avulsed in the outpatient. Endometrial
polyps can be removed either blindly under GA or by
hysteroscopic resection.
2. Fibroid:
a. Myomectomy:
Surgical removal of a fibroid from the uterus wall with
conservation of the uterus. It can be done by laparotomy,
laparoscopy, or hysteroscopy, depending on number, site, size of
the fibroid.
GnRH analogue treatment is often used for 3 months prior
to surgical intervention in an attempt to reduce the vascularity of
the fibroids.
Pregnancy following Myomectomy appears to be safe, with
a very low risk of uterine rupture with a vaginal delivery.
b. Uterine artery embolisation:
An embolic agent is introduced to block both uterine
arteries which results in fibroids becoming avascular and thus
shrink.
As the normal myometrium subsequently derives its blood
supply from the vaginal and ovarian vasculature, UAE is thought to
have no permanent effect on the rest of uterus.
There is a theoretical risk of premature ovarian failure after
UAE, so this procedure is not currently recommended for women
who wish to maintain their fertility.
c. Hysterectomy
3. Endometrial ablation:
It is targeted destruction of the endometrial lining of the
uterus to sufficient depth, so that to prevent regeneration of the
endometrium.
Success rates:
Mean reduction in blood loss is 90% for those undergoing
2
nd
generation techniques, 40% will become amenorrhic, 40% will
have markedly reduced blood loss, 20% will have no difference.
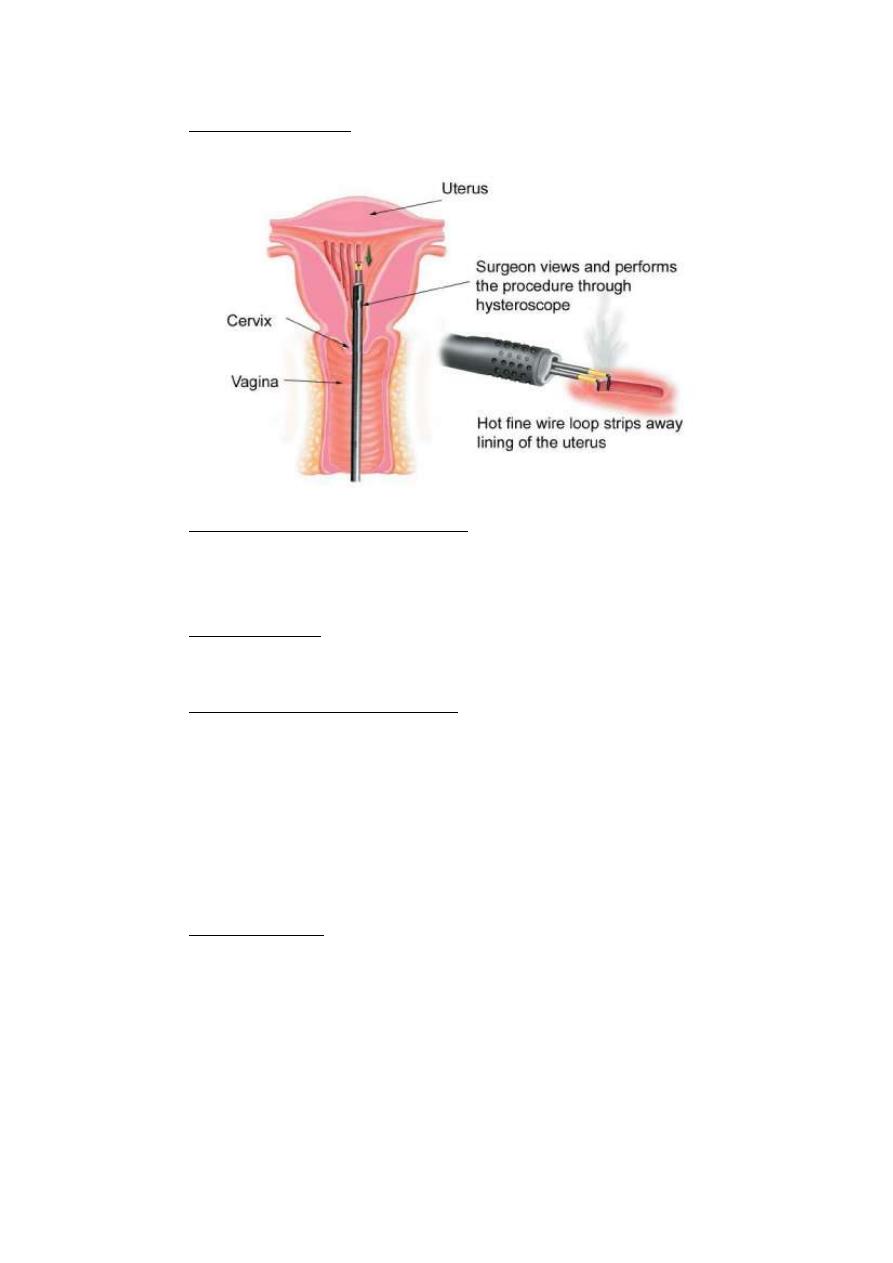
First generation: include transcervical resection of the
endometrium with electrical diathermy loop or rollerball ablation.
Second generation techniques: include thermal uterine balloon
therapy, microwave ablation, impedance controlled endometrial
ablation.
Pre-procedure: the patient should understand the description of
procedure, its success rate, alternative options.
Understand the complications:
Endometritis, hematometra, fluid overload (due to absorption of
distension medium), uterine perforation, and abdominal visceral
injury.
The procedure is taken as outpatient or day case procedure
under local or General Anesthesia. Prior to it hysteroscopy is
done, also after completing the ablation.
Post-procedure: symptoms to be expected:
v
Cramps and pain for 24 hours.
v
Watery brown discharge for 3-4 weeks.
v
Need to have prophylactic antibiotics.
v
Need to use long term effective contraception. The
rationale behind this is the lack of knowledge about the
effects of endometrial ablation on future reproductive
potential.
4. Hysterectomy:
Should only be considered in the treatment of HMB when
women has completed her family and when medical and less
invasive surgical options have failed or are inappropriate.
The UK NICE guidelines advice that hysterectomy route for
HMB should be considered in the following order:
o Vaginal
o Abdominal
o Laparoscopic
But individual patient characteristics and surgical expertise
are important determinants.
Vaginal hysterectomy: absence of abdominal wound and minimal
disturbance of the intestine result in less postoperative pain,
earlier mobilization and earlier discharge from hospital.
Abdominal hysterectomy: Is necessary in women with:
1) History of PID.
2) History of caesarian section.
3) Endometriosis.
4) Long vagina +/or narrow pubic arch making the vaginal
approach technically difficult.
It can be total or subtotal.
Laparoscopic hysterectomy:
This allows diagnosis and treatment of other pelvic diseases
like endometriosis.
It can be divided to laparoscopy – assisted vaginal
hysterectomy LAVH and total laparoscopic hysterectomy TLH.

