Cancer chemotherapy attempts to cause a lethal
cytotoxic event or apoptosis in the cancer cell that can
arrest a tumor’s progression.
Chemotherapy is used primarily to treat systemic
disease rather than localized lesions that are amenable to
surgery or radiation
An understanding of this treatment helps patients better
recognize and tolerate side effects, if they occur
Ideally, these anticancer drugs should interfere only with
cellular processes that are unique to malignant cells.
Unfortunately, most currently available anticancer drugs
do not specifically recognize neoplastic cells but, rather,
affect all kinds of proliferating cells, both normal and
abnormal.
The use of combination chemotherapy is
important for several reasons.
1.
It provides maximal cell kill within the
range of toxicity tolerated by the host for each
drug as long as dosing is not compromised.
2.
It provides a broader range of interaction
between drugs and tumor cells with different
genetic abnormalities in a heterogeneous tumor
population.
3.
It may prevent or slow the subsequent
development of cellular drug resistance.
Treatment strategies
Goals of treatment: The ultimate goal of chemotherapy is a cure (that is, long-term, disease-free
survival). A true cure requires the eradication of every neoplastic cell. If a cure is not attainable, then the
goal becomes control of the disease (stop the cancer from enlarging and spreading) to extend survival and
maintain the best quality of life. Thus, the individual maintains a “near-normal” existence, with the cancer
being treated as a chronic disease. In advanced stages of cancer, the likelihood of controlling the cancer is far
from reality and the goal is palliation (alleviation of symptoms and avoidance of life-threatening toxicity).
Indications for treatment: Chemotherapy is sometimes used when neoplasms are disseminated and are
not amenable to surgery. Chemotherapy may also be used as a supplemental treatment to attack
micrometastases following surgery and radiation treatment, in which case it is called adjuvant
chemotherapy. Chemotherapy given prior to the surgical procedure in an attempt to shrink the cancer is
referred to as neoadjuvant chemotherapy, and chemotherapy given in lower doses to assist in prolonging a
remission is known as maintenance chemotherapy.
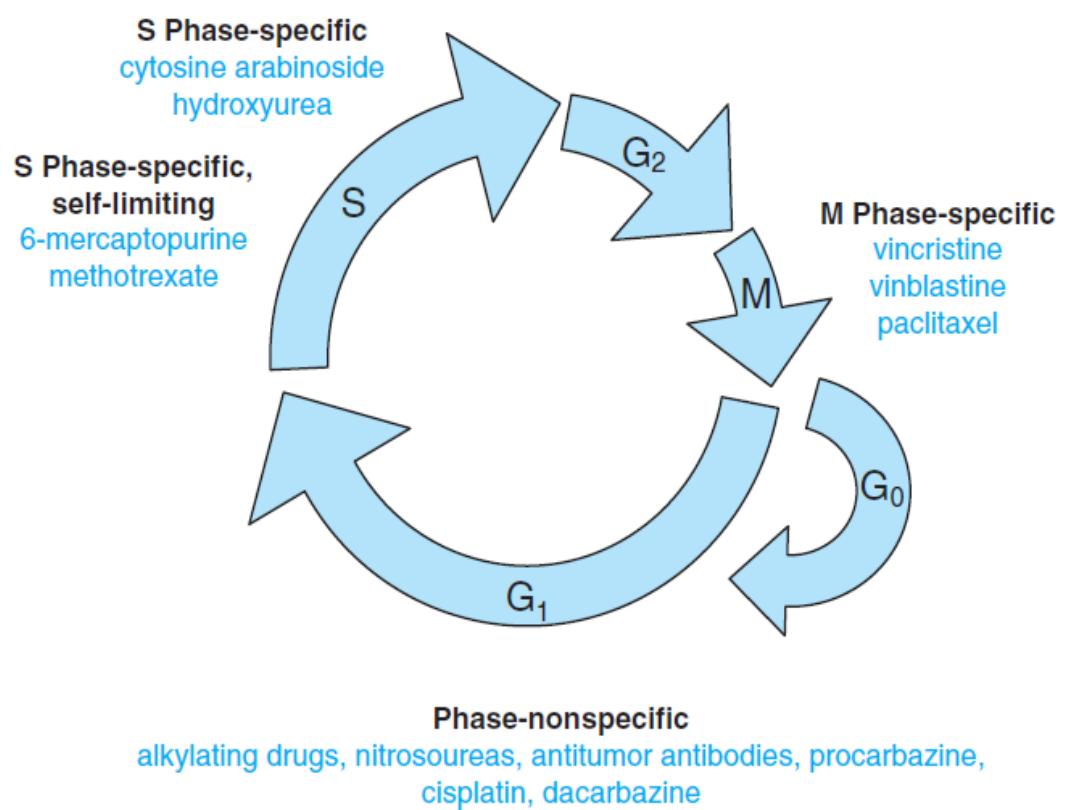
Tumor susceptibility and the growth cycle: The fraction of tumor cells that are in the replicative
cycle (“growth fraction”) influences their susceptibility to most cancer chemotherapeutic agents. Rapidly
dividing cells are generally more sensitive to chemotherapy, whereas slowly proliferating cells are less
sensitive to chemotherapy
How Does
Chemotherapy Work?
To understand how chemotherapy works as
a treatment, it is helpful to understand the
normal life cycle of a cell in the body.
All living tissue is composed of cells. Cells
grow and reproduce to replace cells lost
during injury or normal "wear and tear."
The cell cycle is a series of steps that both
normal cells and cancer cells go through in
order to form new cells.
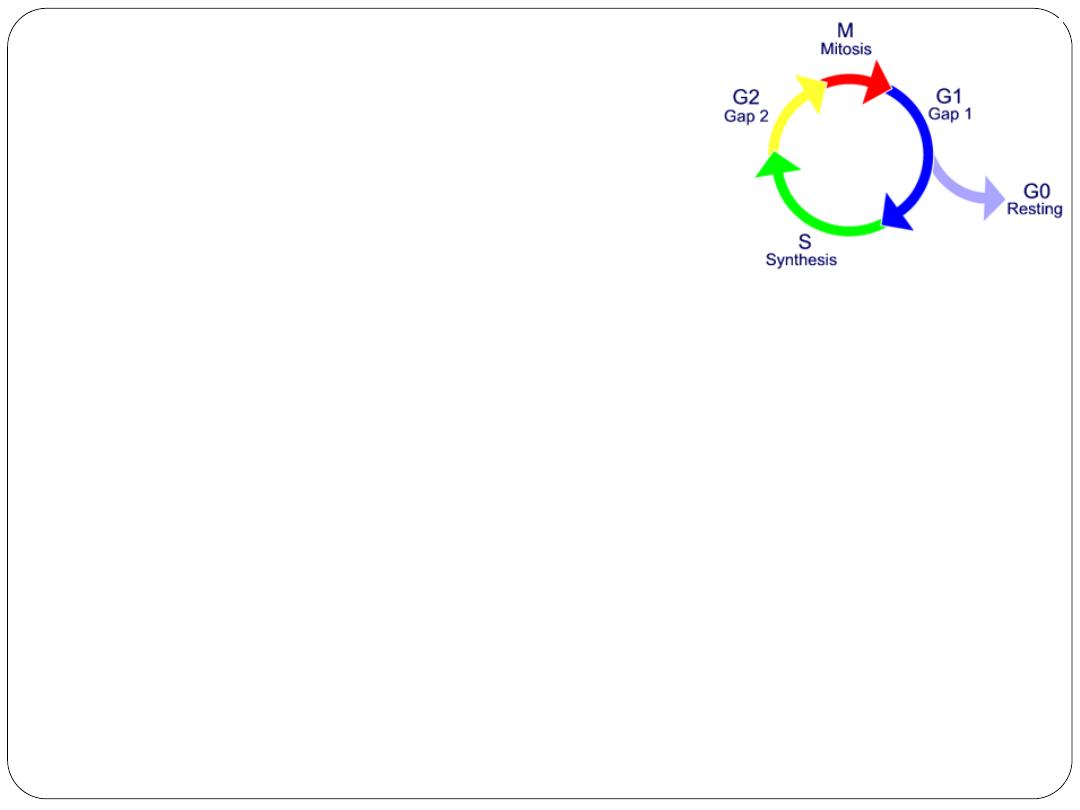
The cell cycle phases are:
resting (G0; nothing is
happening),
G1 (or gap 1; a growth phase),
S (synthesis; the replication of
DNA occurs),
G2 (gap 2; another growth
phase), and
M (mitosis; the actual division
from 1 cell into 2).
The Cell Cycle
G0 phase (resting stage): The cell has not yet
started to divide. Cells spend much of their
lives in this phase. Depending on the type of
cell, G0 can last for a few hours to a few
years. When the cell is signaled to reproduce,
it moves into the G1 phase.
G1 phase: During this phase, the cell starts
making more proteins and growing larger, so
the new cells will be of normal size. This
phase lasts about 18 to 30 hours.
S phase: In the S phase, the chromosomes
containing the genetic code (DNA) are copied
so that both of the new cells formed will have
matching strands of DNA. This phase lasts
about 18 to 20 hours.
G2 phase: In the G2 phase, the cell checks the
DNA and prepares to start splitting into 2
cells. It lasts from 2 to 10 hours.
M phase (mitosis): In this phase, which lasts
only 30 to 60 minutes, the cell actually splits
into 2 new cells.
I. Cytotoxic drugs:
they act directly on
cells
A. Alkylating agents
1- Nitrogen mustards: (Form DNA cross-links,
resulting in inhibition of DNA synthesis and
function) like: Cyclophosphamide (the most
commonly used alkylating agent, haemorrhagic
cystitis is its potential adverse effect),
Chlorambucil, Melphalan, Mechlorethamine.
Drugs
2- Ethylenimide: ThioTEPA (an organophosphorus
compound, releases free radicals which disrupt the
bonds of cell DNA).
3- Alkyl sulfonate: Busulfan (has a selective effect on
the bone marrow and used in chronic granulocytic
leukaemia).
4- Nitrosoureas: Carmustine, Lomustine (both have good
penetration to CNS), streptozocin (specifically toxic to
the β cells of the islets of Langerhans, hence its use in
the treatment of insulinomas).
5- Platinum analogs: cisplatin , carboplatin, and
oxaliplatin (Form intrastrand and interstrand DNA
cross-links; binding to nuclear and cytoplasmic
proteins).
B. Anti metabolites
(1)
Folate antagonist: Methotrexate, Pemetrexed
(2)
Purine antagonist: 6-Mercaptopurine, 6-Thioguanine ,
Fludarabine, Cladribine.
(3)
Pyrimidine antagonists: 5-Fluorouracil, Cytarabine,
Capecitabine, Gemcitabine.
C. Vinca alkaloids:
Vincristine, Vinblastine and
Vinorelbine (inhibition of tubulin polymerization)
D. Taxanes:
Paclitaxel, Docetaxel (derived from the bark
of the yew tree, mitotic spindle poison results in inhibition
of mitosis and cell division).
E. Epipodophyllotoxin:
Etoposide and Teniposide
(inhibition of topoisomerase II)
F. Campothecin:
Topotecan and Irinotecan (inhibit
the activity of topoisomerase I, the key enzyme
responsible for cutting and religating single DNA
strands).
G. Antibiotics:
Anthracyclines (Doxorubicin,
Daunorubicin, Idarubicin, Epirubicin, Mitoxantrone),
Bleomycin, Mitomycin C (Oxygen free radicals bind to
DNA causing single- and doublestrand DNA breaks).
H. Miscellaneous:
Bendamustine (bifunctional
alkylating agent consisting of a purine benzimidazole
ring and a nitrogen mustard moiety), Procarbazine,
Dacarbazine (Methylate DNA and inhibit DNA
synthesis and function).
H. Miscellaneous: continue......
Monoclonal antibodies (Trastuzumab, rituximab, bevacizumab,
and cetuximab) They are created from B lymphocytes.
Imatinib (acts as a signal transduction inhibitor, used
specifically to inhibit tumor tyrosine kinase activity).
Gefitinib (targets the epidermal growth factor receptor. It is
approved for the treatment of non–small cell lung cancer
that has failed to respond to other therapy).
L-Asparaginase (catalyzes the deamination of asparagine to
aspartic acid and ammonia, limits the amounts available to
tumour cells).
Interferons ( acts through suppression of cell proliferation,
activation of macrophages, and increased cytotoxicity of
lymphocytes.
II. Hormones
A. Glucocorticoids: Prednisolone,Dexamethasone.
B. Estrogens: Fosfestrol, Ethinylestradiol.
C. SERMs: Tamoxifen, Tormifene.
D. Aromatase inhibitors: Letrozole, Anastrazole,
Exemestane.
E. Anti androgens: Flutamide, Bicalutamide
F. 5-α reductase inhibitor: Finasteride, Dutasteride
G. GnRH analogues: Triptorelin,Naferelin.
H. Progestins: Hydroxyprogesterone acetate.
Sequence of treatments:
Adjuvant therapy: therapy given after surgery
to reduce the likelihood of the cancer
returning.
Neo-adjuvant therapy: therapy given before
surgery to shrink the tumor, allowing the
surgery to be more successful.
Concurrent therapy: when 2 or more therapies
are given together, such as chemotherapy and
radiation.

How is chemotherapy
given?
Orally (by mouth, in pill form)
Intravenously (IV, through a vein, either as
a short infusion or continuously for one or
more days)
As an injection or needle
Directly into a body cavity (i.e.: the bladder,
abdominal cavity)
Intra-arterially (in special cases, such as
limb perfusion treatment for melanoma)
What are the side effects
of chemotherapy?
SKIN
Alopecia
Hair loss occurs because chemotherapy
can sometimes damage healthy cells.
It is so common because hair follicle
cells multiply very quickly like cancer
cells and chemotherapy drugs have
difficulty in discerning the difference.
GASTROINTESTINAL SYSTEM
can cause irritation which can eventually
lead to inflammation of the mouth, a
condition known as stomatitis .
A stinging sensation in the throat may
develop and lead to dysphagia (difficulty in
swallowing).
Management:
Good oral hygiene
Nausea & Vomiting- most
common side effects of
chemotherapy and may
persist for as long as 24-48
hrs. after its administration.
Mucositis – inflammation of
the mucosal lining
Diarrhea can also be a side effect of
chemotherapy. Caused by the destruction of
normal, dividing cells of the gastrointestinal (GI)
tract, diarrhea varies from patient to patient. It is
better managed if treated early
RENAL SYSTEM
Rapid tumor cell lysis- increased urinary
excretion of uric acid, which can cause renal
damage
HEMATOPOIETIC SYSTEM
Myelosuppression- depression of bone marrow
function, resulting in decreased production of
blood cells.
Decreases the number of RBCs (anemia), WBCs
(leukopenia) and platelets (thrombocytopenia)
Growth factors:
G-CSF (granulocyte-colony stimulating factor)
GM-CSF (granulocyte macrophage colony-
stimulating factor)
EPO (erythropoietin)
REPRODUCTIVE SYSTEM
Take effective contraceptive precautions
when having chemotherapy, as the
chemotherapy drugs might harm the baby
if pregnancy occurs.
In some women, chemotherapy brings on
an early menopause. This may cause
symptoms such as dryness of the vagina and
a decreased interest in sex.
NEUROLOGIC SYSTEM
Peripheral neuropathies
Loss of deep tendon reflexes
Paralytic ileus
Fatigue
Nursing Management
in Chemotherapy
Assess fluid and electrolyte status
(Anorexia, nausea & vomiting,
altered taste and diarrhea put patient
at risk)
Modifying risk for infection and
bleeding
(suppression of the bone marrow and
immune system)
Administering Chemotherapy
- patient is observed for extravasation
(particularly of vesicant agents, which
may produce necrosis if deposited in
subcutaneous tissues
Protect caregivers
