LIPOPROTEINS
OBJECTIVE:
List the types of lipoproteins (LPs)
and
their
basic
structures.
Recognize the function of each LP in
transporting of cholesterol and TG.
Classify the LPs as exogenous, endogenous, bad
lipid, and the good (protective) lipid.

Definition:
All the types of Lipid components are
relatively water insoluble and therefore cannot be
transported into the blood throughout the body in their
native lipid forms (TGs, Phospholipids, FFAs,
cholesterol,
etc).
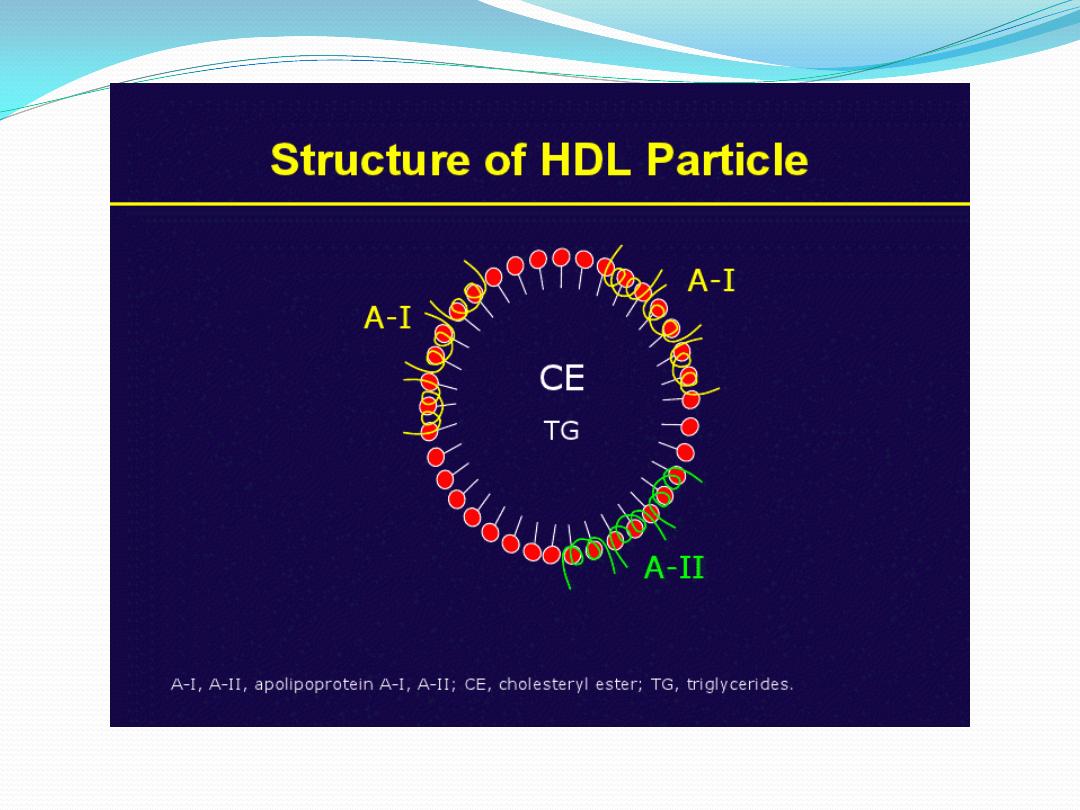
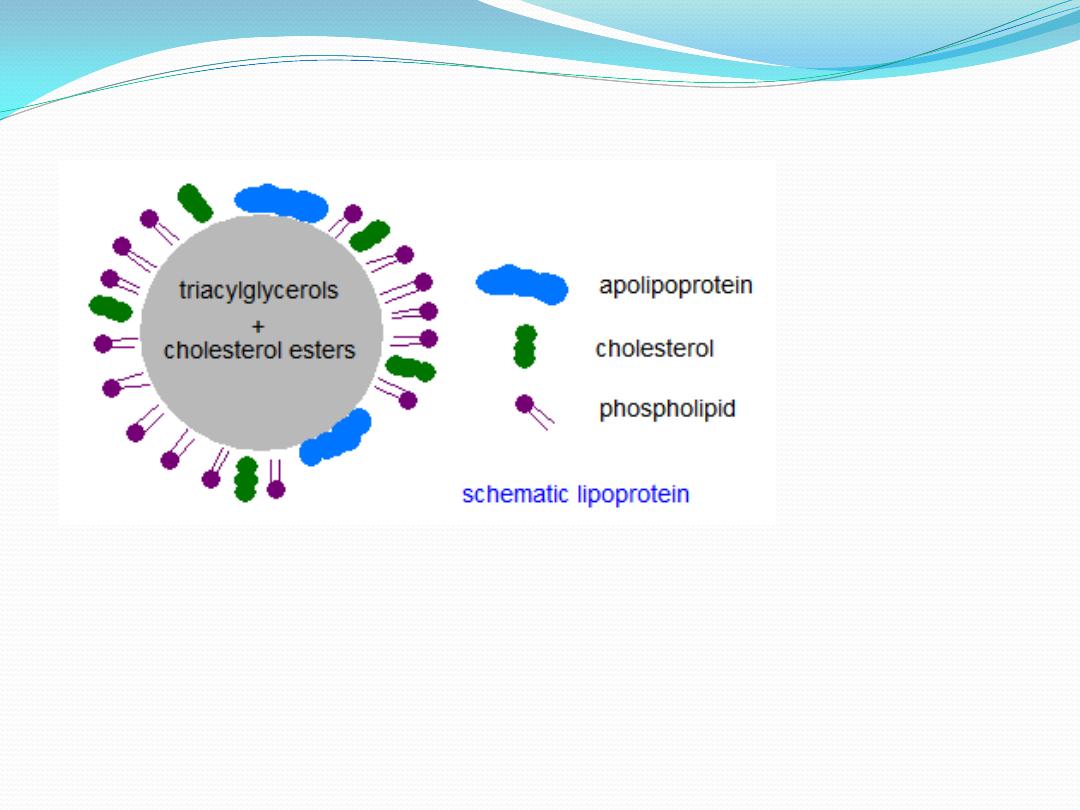
Lipoproteins(LPs)
are spherical structures composed
of native lipid components and specific proteins,
referred to apolipoproteins, function in transporting of
lipids throughout the human body.
To be able in
carrying the lipids
,
the no polar lipids directed to the
core, the TGs and Ech
,
while the relatively polar
components, Fch and phospholipids oriented to the
surface of the spherical structures
, and these structures
referred to
apolipoproteins(apoLPs).

Although,
the apoLPs still unable to be transported
throughout the body,
addition of sufficient amounts of
specific proteins, the
apolipoproteins
confer
the apoLP structures adequate polarity to be soluble and
transported in blood throughout the body.
Apoproteins
are
of
several
types
:
apoA;
I,II,III
apoB;
48,
100
apoC;
I,II,III
apoE;
2,3,4.
These apoproteins are poly peptide family function in
1. structural components of LPs, they are essential
constituents
for
integral
LP
structures
2. some as cofactor for Enzymes involved in lipid
metabolism
as,
apoCII
,apoAI
3. some as ligand for recognition of whole particle of LPs by
their
receptor
as
apoE3,
apoB100
4. some aid in secretion of LP particles from the site of
origin
as
apoB48
from
small
intestine.
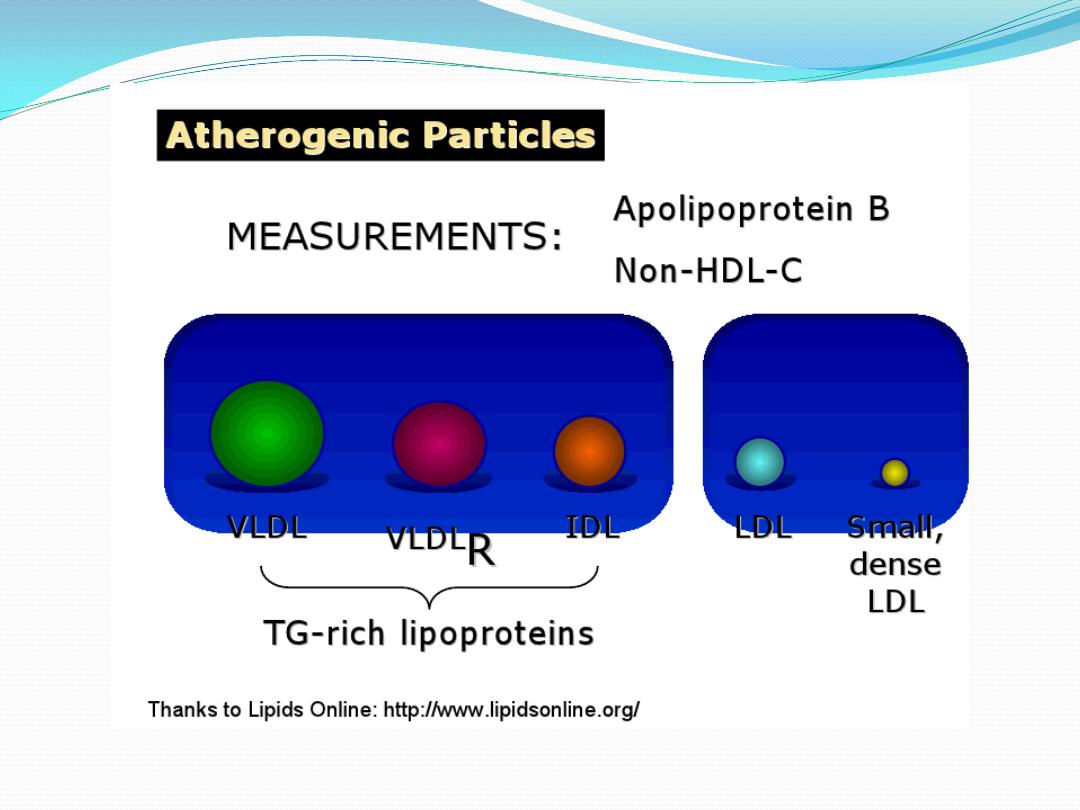
TYPES
OF
LPs
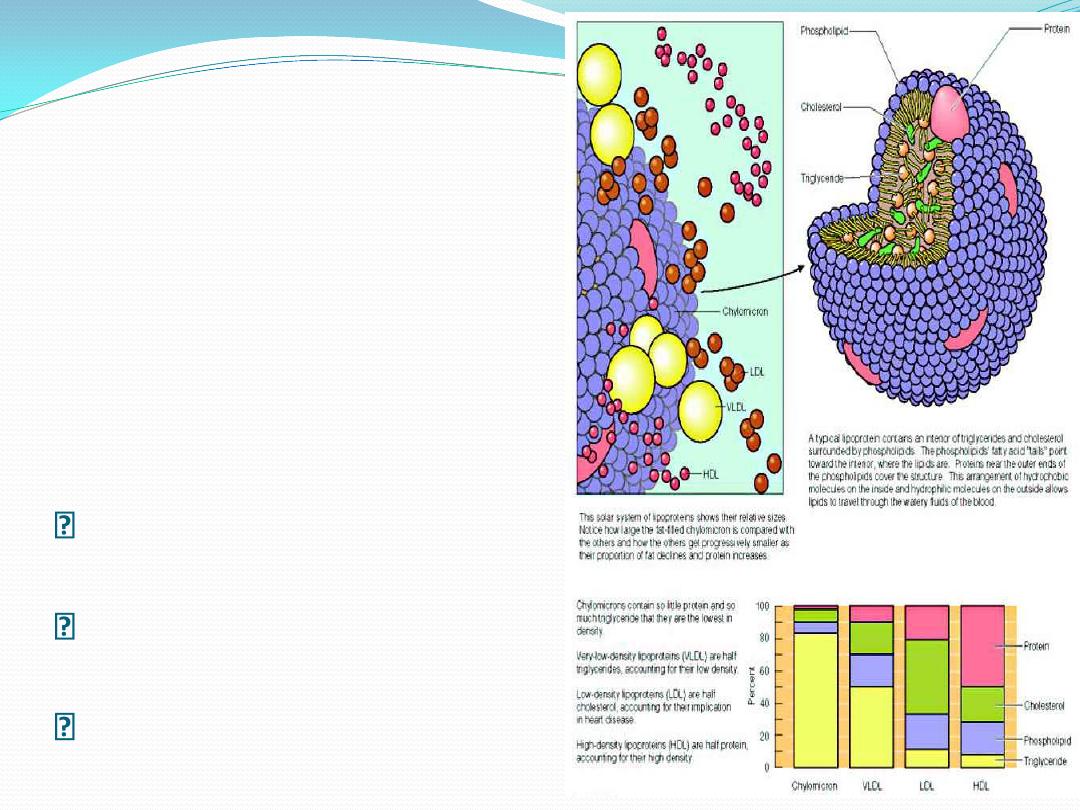
There are five types that are involved in lipid function; They
are classified according to their density(ratio of
protein/lipid
content,
or
size).
The ascending order for classification of these LPs according
to their density (opposite for size) are as follow:

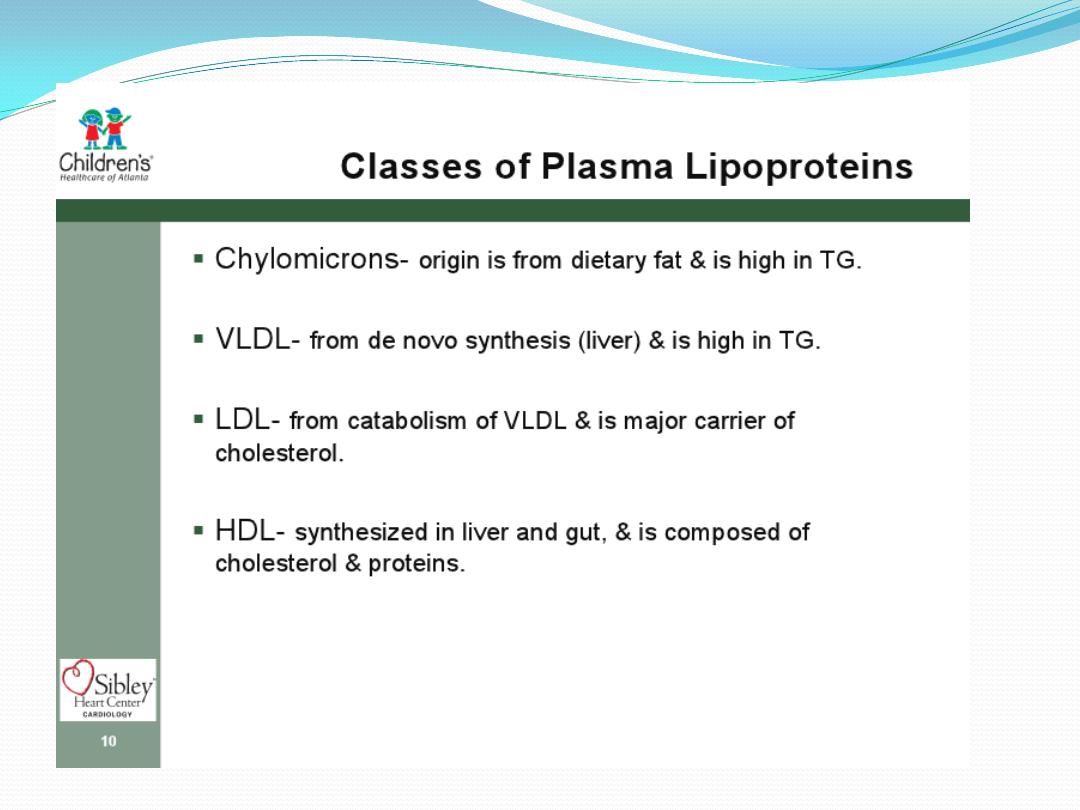
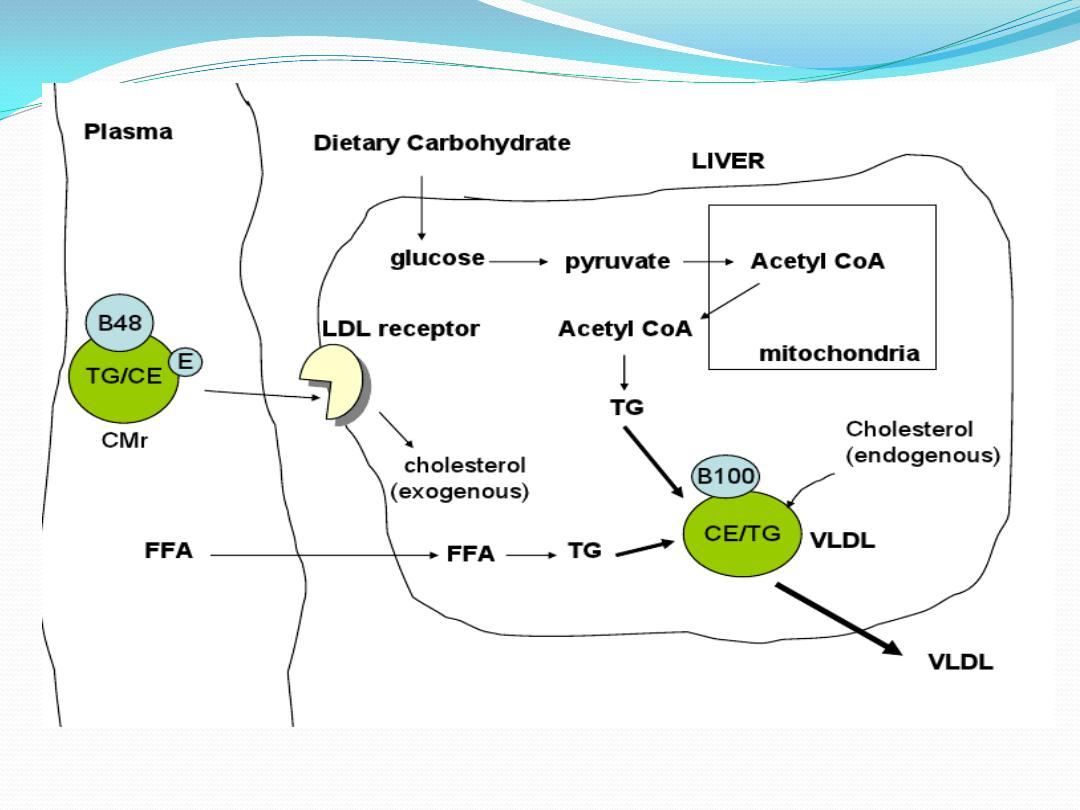
1.Chylomicrone(Exogenous lipid, TG-rich
particle)
2.Very Low Density Lipoprotein
VLDL
(Endogenous
lipid,
TG-rich
particle)
3.Intermediate
Density
Lipoprotein
IDL(Transient
lipid,
TG-Cholesterol)
4. Low Density Lipoprotein-Cholesterol
LDL-C
5. High Density Lipoprotein-Cholesterol
HDL-C
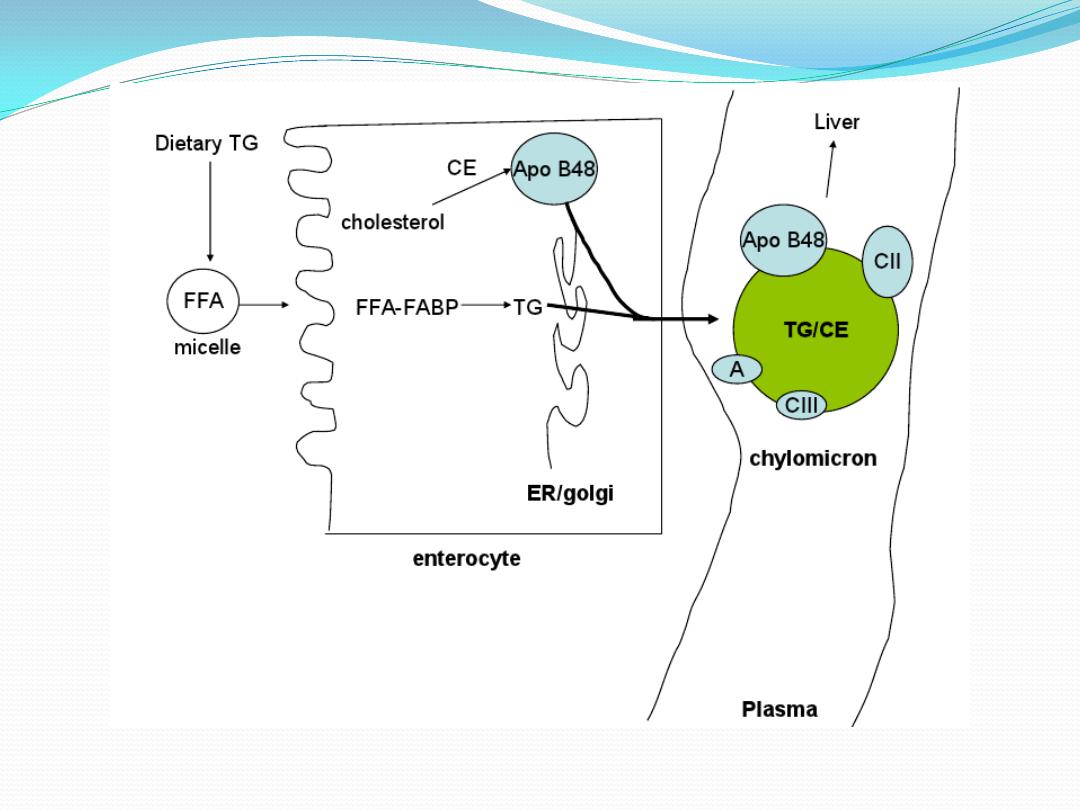
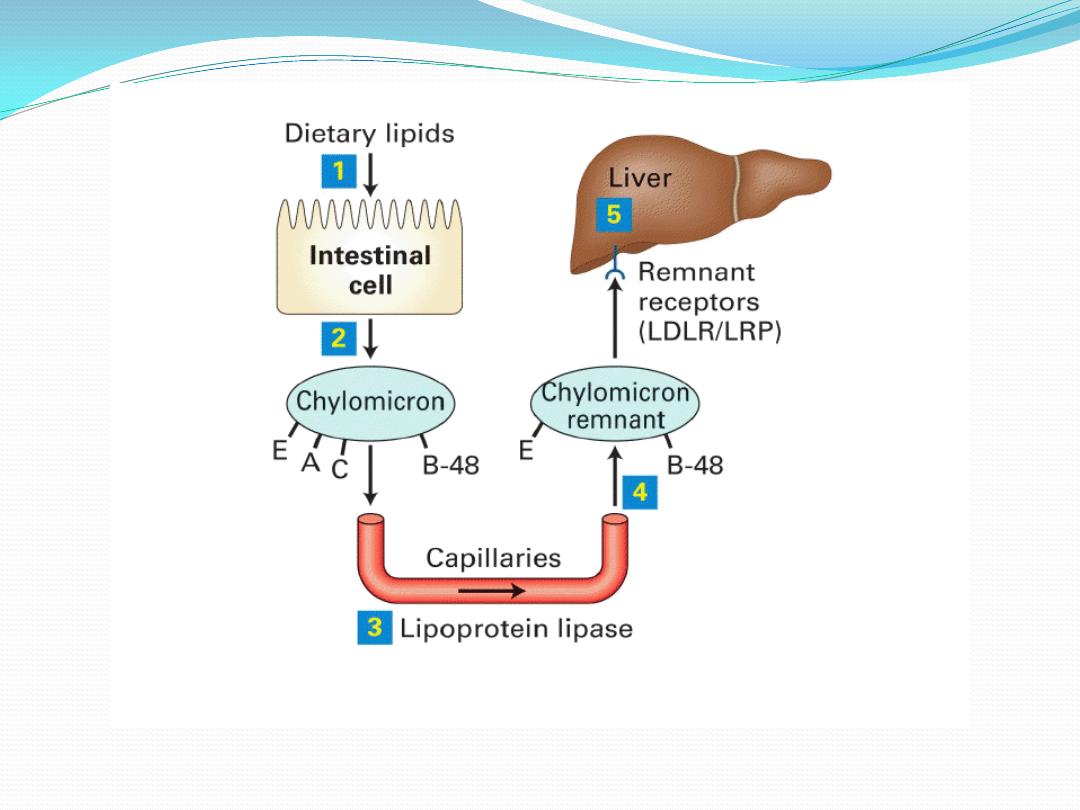
CHYLOMICRONE (Exogenous Lipid,TG-
rich particle):
Dietary lipid {90% TG+10%
(Phospholipids, cholesterol, Sphingolipids &free fatty
acids) are digested and absorbed by small intestine in
enterocytes, the absorbed lipids are resynthesized
again into TG, PLs, sphingolipids & small amounts of
FFAs
addition of apolipoproteins; mainly apoB48
Lipoprotein
Chylomicrone
,
the exogenous lipid.
So the Exogenous lipid source is small intestine which
secreted into lymphatic system (because of large size
?), blood circulation, where Chylomicrone acquired
apoCII and apoE, both are important for their
metabolism.
Chylomicrons
◦ Synthesized in small
intestine
◦ Transport dietary lipids
◦ 98% lipid, large sized,
lowest density
◦ Apo B-48
involved in secretion
◦ Apo C-II
Lipoprotein lipase activator
◦ Apo E
Remnant receptor binding
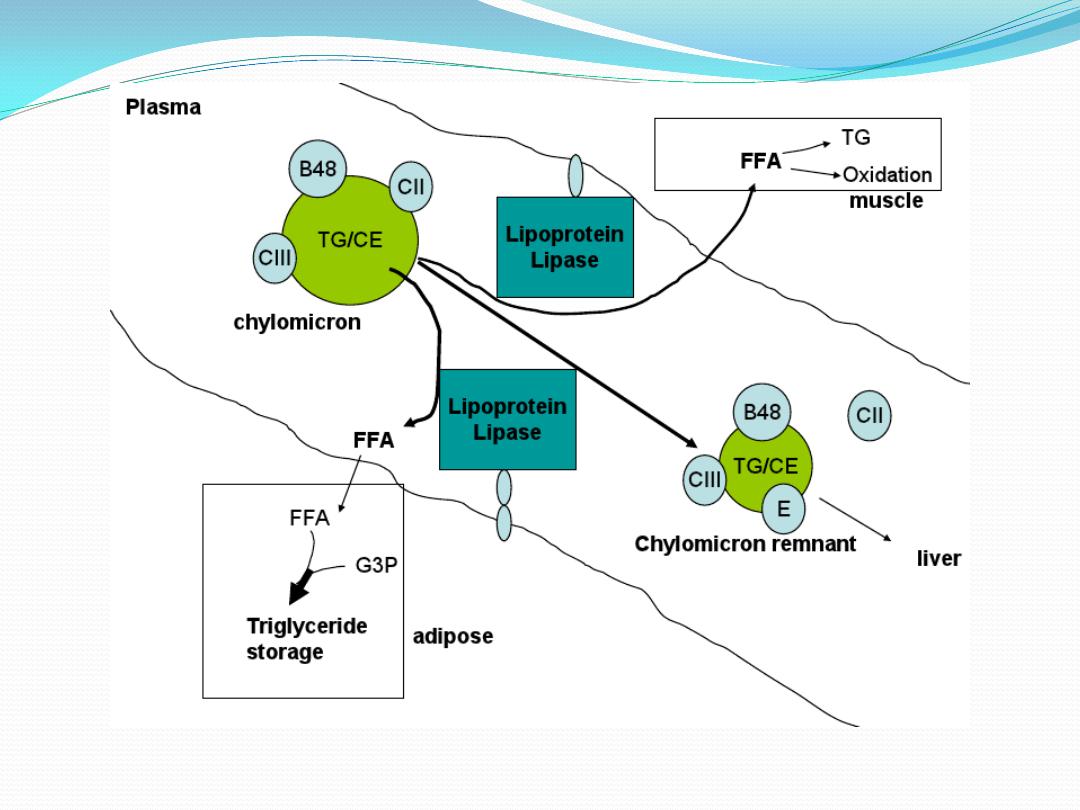
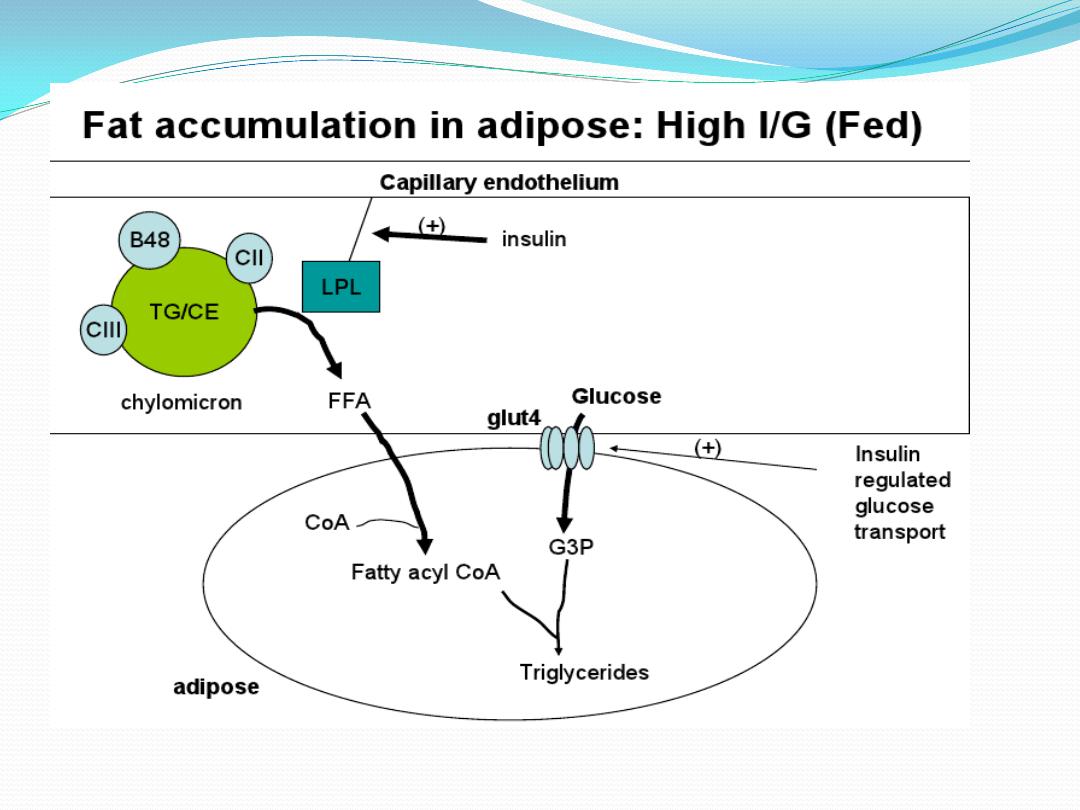
Secreted Circulated Chylomicrone transported to
adipose tissue(A.T) & Muscles (cardiac+skeletal) where
it hydrolyzed (the TG content) by enzyme Lipoprotein
Lipase LPL in the presence of apoCII as cofactor (this
enzyme coated into luminal surface of blood vessels
mainly of A.T , Sk.M and Cardiac M).
The hydrolysis of
chylomicrone-TG
=FFAs+
glycerol.
FFAs are taken by A.T, Sk.M+ Cardiac M, while
glycerol
returned
to
the
liver.
The chylomicron- remnant , which contain mainly
cholesterol, apoE,apoB100 and the remainder TG 10%
of original amount will be taken up by the liver which
has receptor for Chylomicrone remnant recognized the
apoE3 on the surface of remnant of LPs. This engulfed
or internalized hepatic remnant used in endogenous
lipid
synthesis.

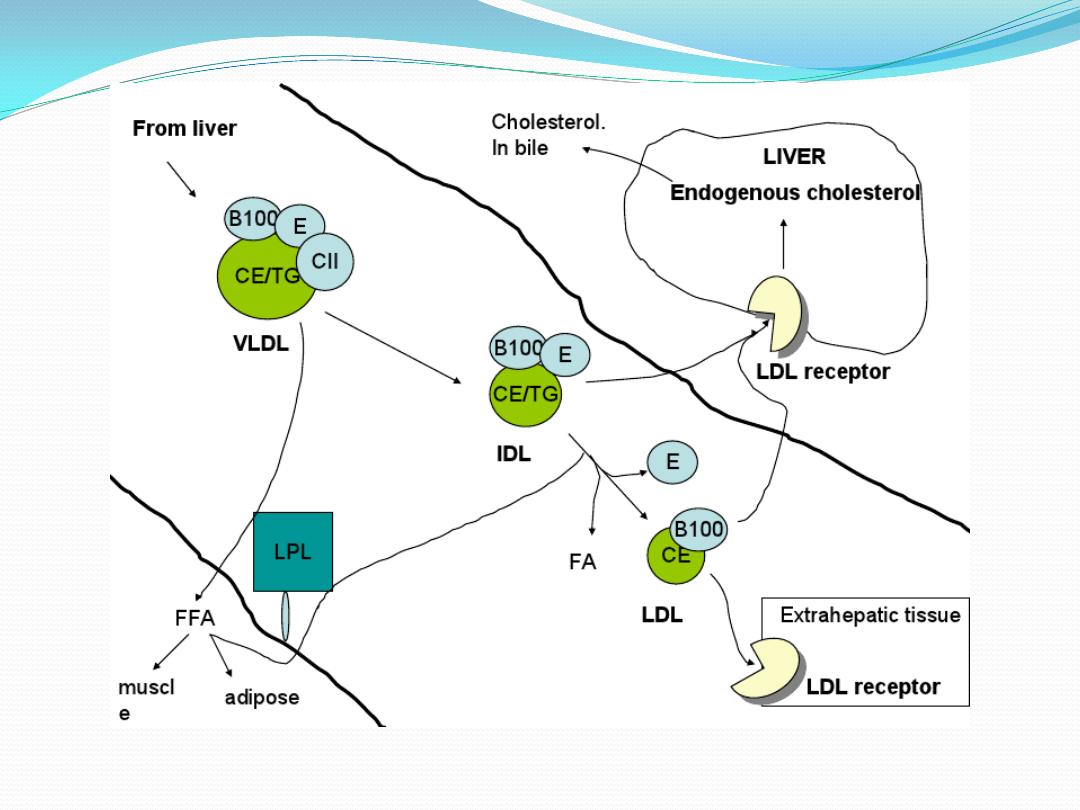
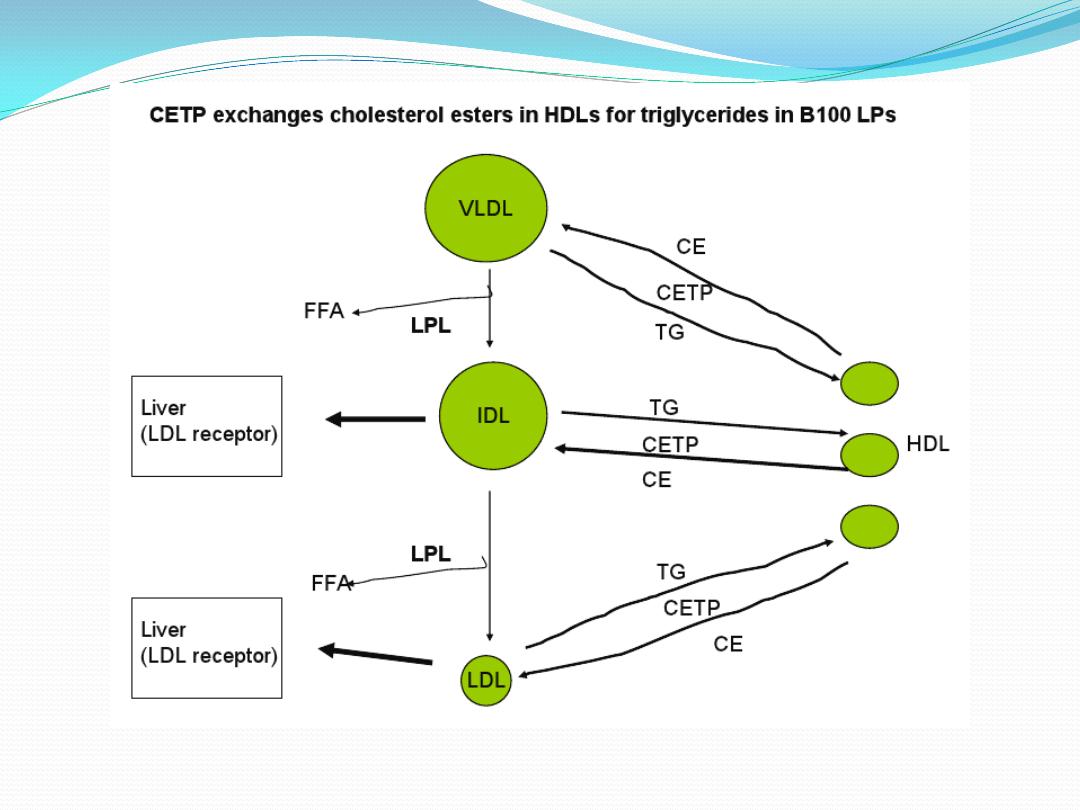
VLDL
(Endogenous
lipid,
TG-rich
particle):
This LP is synthesized in the Liver from the
remnant lipid of Chylomicrone & the Denovo
synthesized lipid in the liver (TG, PL+ cholesterol from
excess glucose and dietary FFAs
). ApoVLDL which after
addition of apoB100 and apoE3 is converted into LP
VLDL.
It is secreted directly into blood circulation where
it acquired apoCII, the cofactor of ?. Then as
Chylomicrone undergoes the removal of significant
amount of TG by LPL in A.T, Sk.M & cardiac M.
The
remainder component of this metabolism referred to
IDL which contains equal amount of TG and cholesterol
in addition to apoE3 and apoB100.
IDL
is transient LP component, 50% of which is retaken
by the liver via hepatic receptor recognized apoE3,
while the remainder 50% are converted into LDL after
removal
of
all
TG
from
IDL.
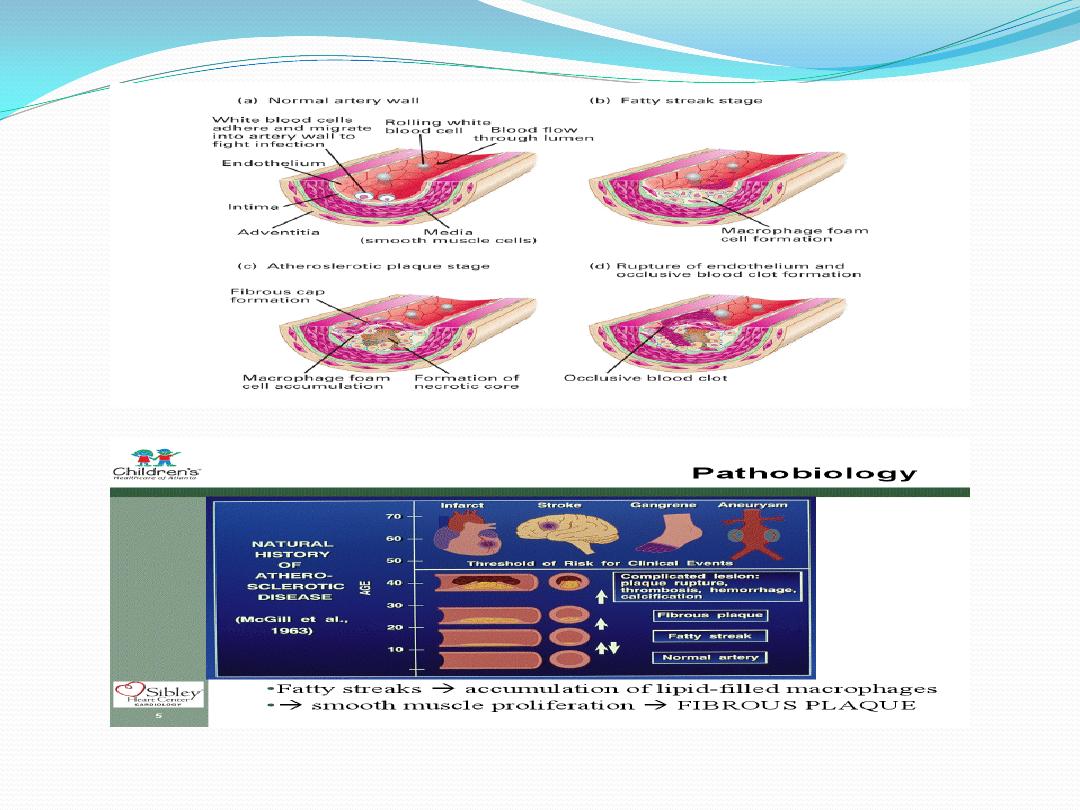
LDL
is exclusively cholesterol containing particle
with only apoB100 as apoLP, it is synthesized from
VLDL in the circulation and it is the carrier, mainly of
cholesterol from the principal site of synthesis, the
liver, to the peripheral tissues such as the endocrines,
skin,…, etc. LDL-C is the more dense and smaller size
compared with chylomicrone and VLDL, so it is the
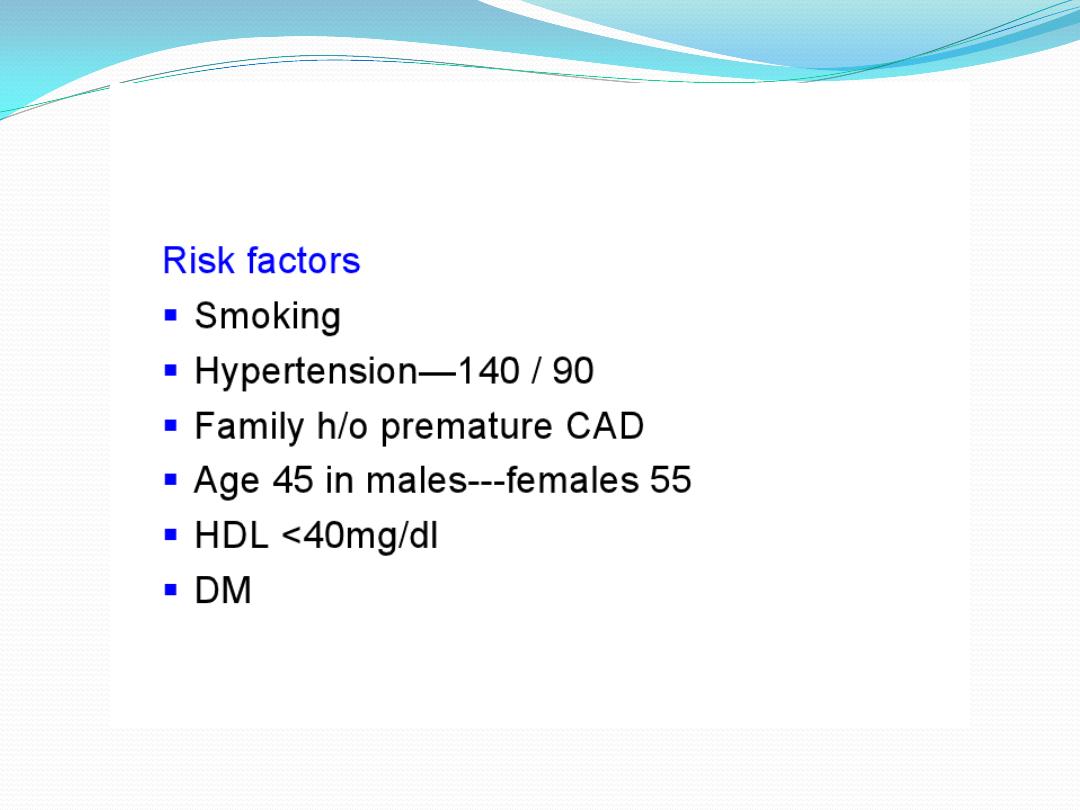
Atherogenic lipid, means its blood concentrations have
the direct correlation with risk and the incidence of
coronary heart disease CAD.
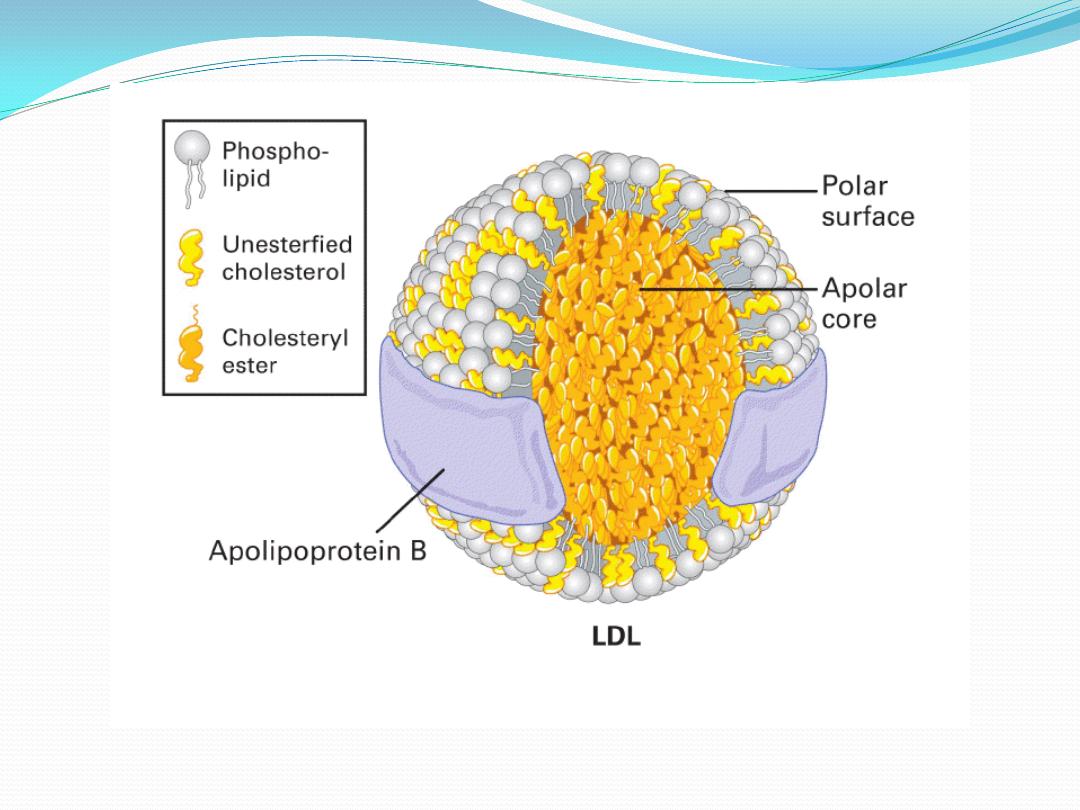

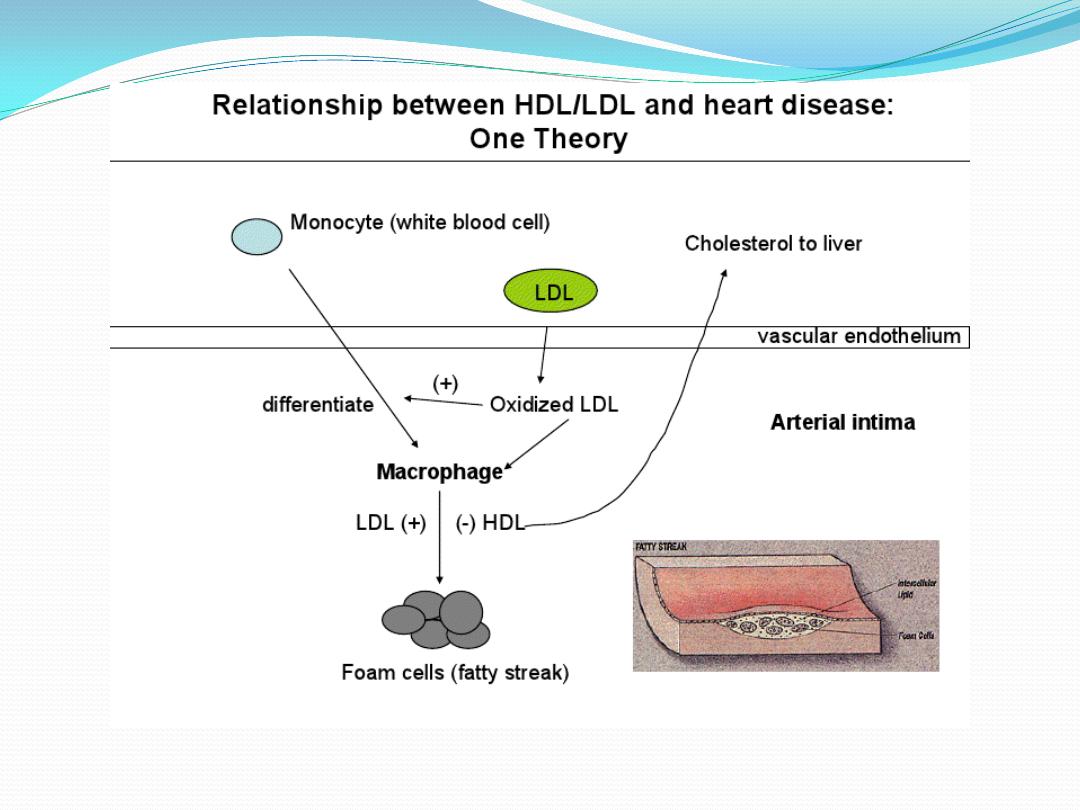
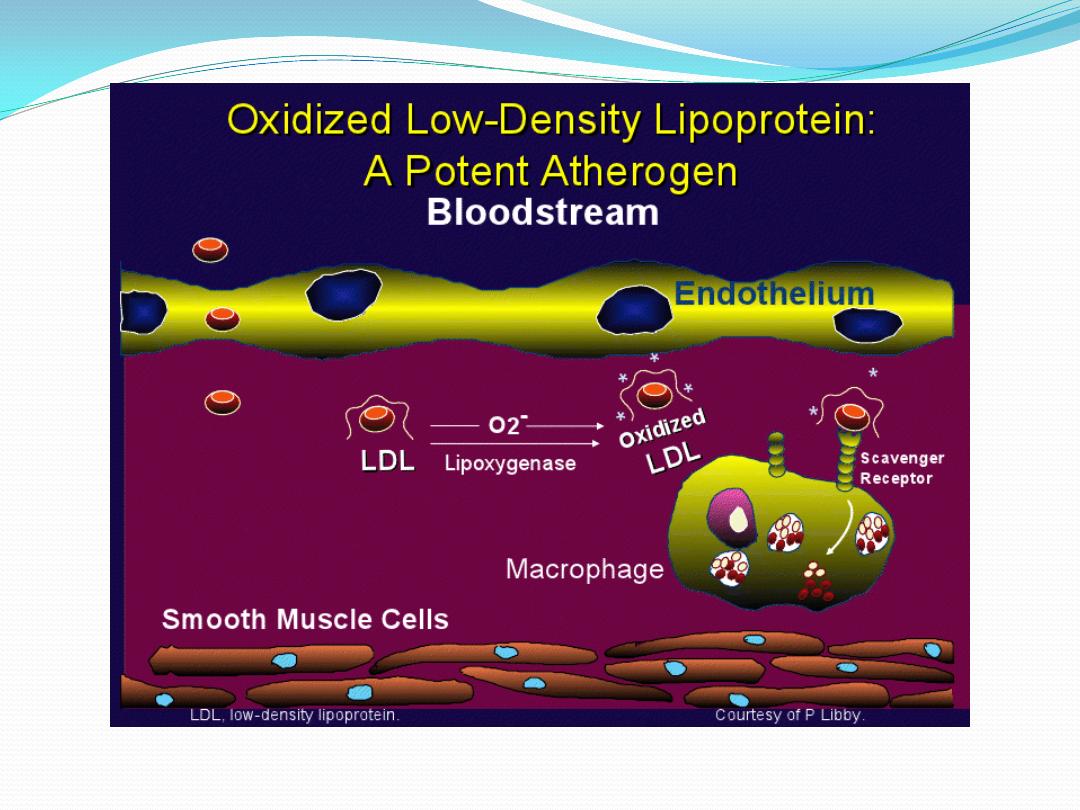
You must know that this lipid LDL is subdivided into several
fractions LDL1 to LDL 9, of which the LDL5 may be the
atherogenic one. Also, the native LDL-C molecule is not
atherogenic by itself, but the modified, such as the oxidized
LDL-C
is
the
atherogenic
lipid.
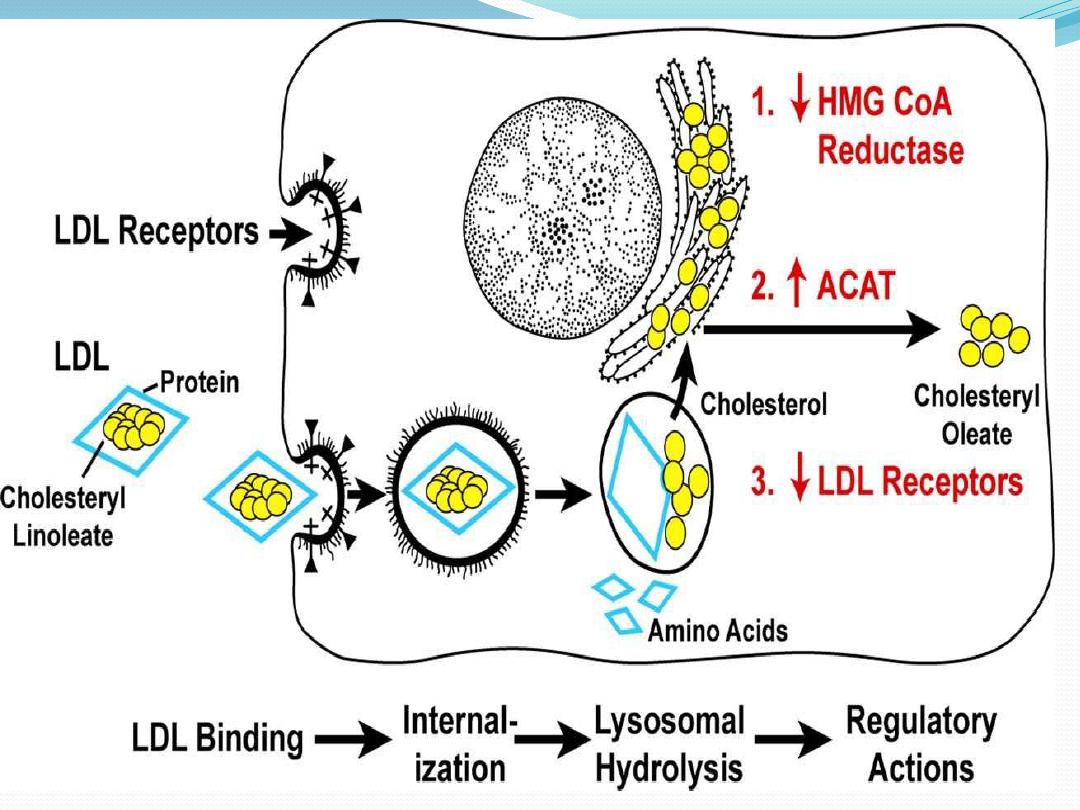
The control of blood LDL level is by two ways:
1. Hepatic tissue receptors; the hepatic LDL receptor
which account for 2/3 removal of blood LDL and is
regulable and saturable mechanism. These LDL receptors
recognize the apoB100 found on the surface of LDL-C
molecules and the complex of LDL-Receptor internalized by
hepatic cells and so regulate the blood cholesterol
concentrations.
2. Scavenger receptor 1/3 of blood LDL and is found in
many cell of tissues but predominant in Macrophage
cells (the native of them are Monocyte cells) and it is
nonsaturable
and
not
regulated
by
blood
LDL.
`

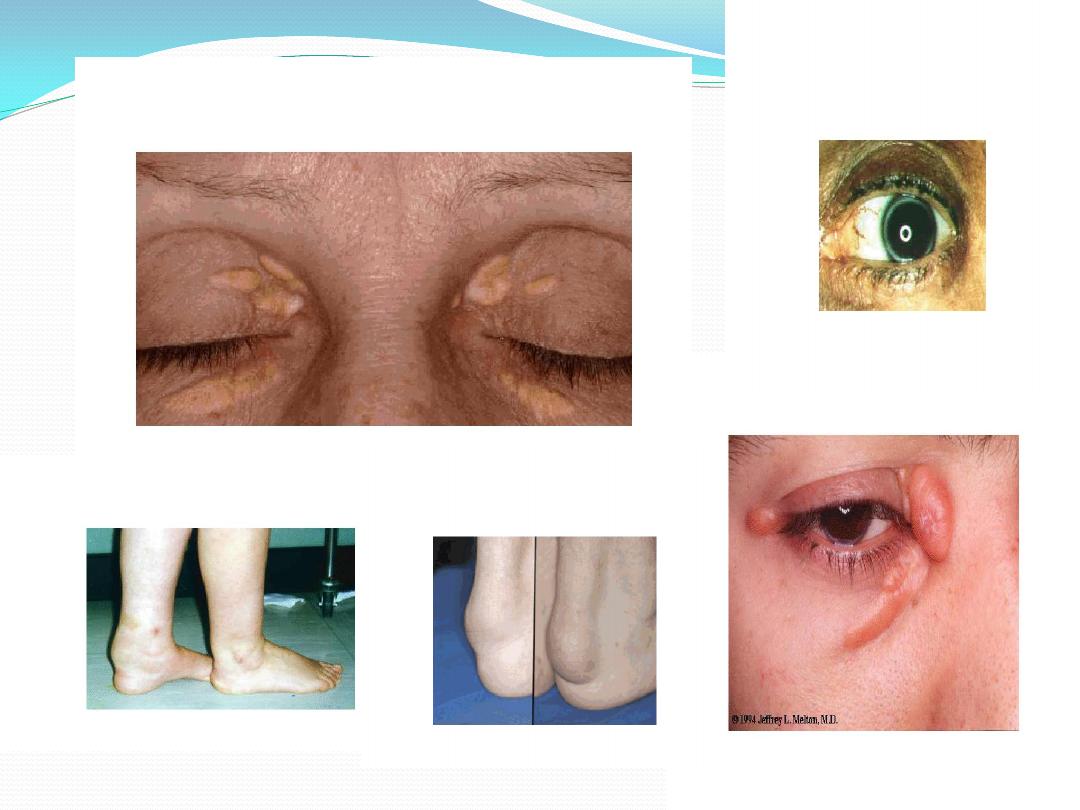
The vascular
sub endothelial LDL-rich macrophages
are the precursors and the early step in plaque
synthesis and consequent atherosclerosis.
The
entered LDL-C
to the liver regulates blood
cholesterol concentration by the following ways:
1. decreased the HMG-CoA reductase enzyme, so
decrease the endogenous cholesterol synthesis
2. Increased Acyl Cholesterol Acyl Transferase
(ACAT)
enzyme, which increased the intracellular cholesterol
synthesis,
the
less
toxic
cholesterol.
3. decreased the LDL-C receptor synthesis by inhibition
of gene expression to lower the LDL-C endocytosis and
prevents the intracellular cholesterol accumulation.

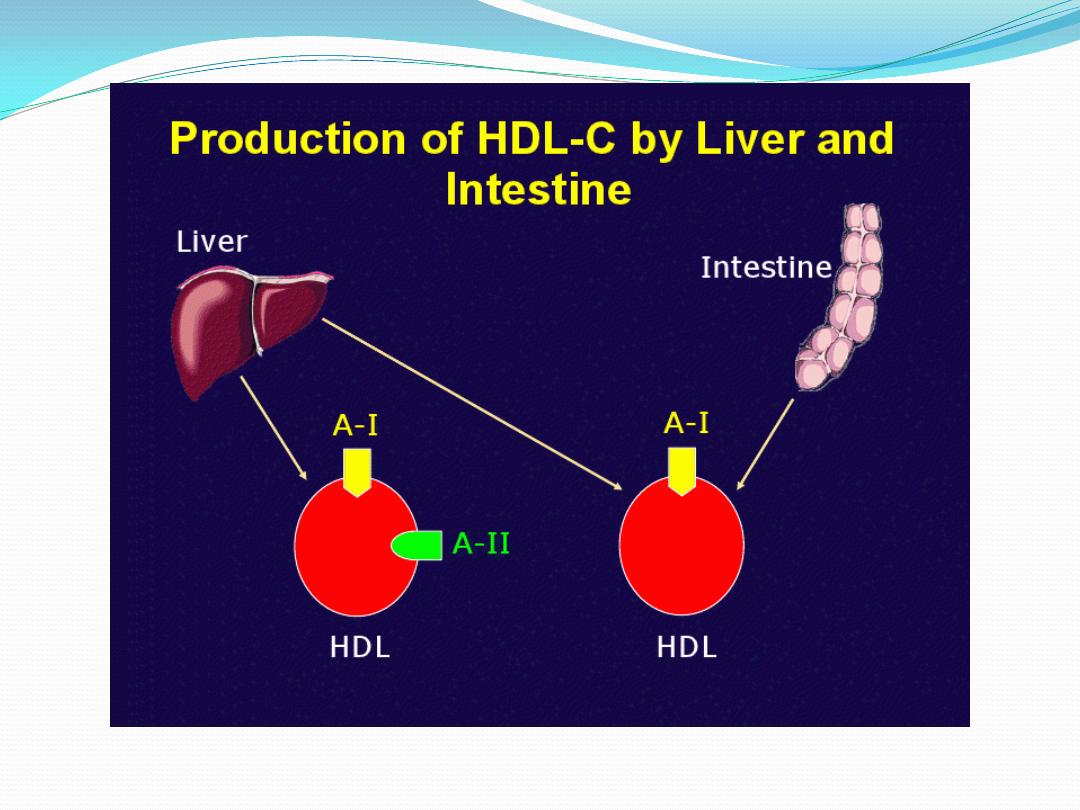
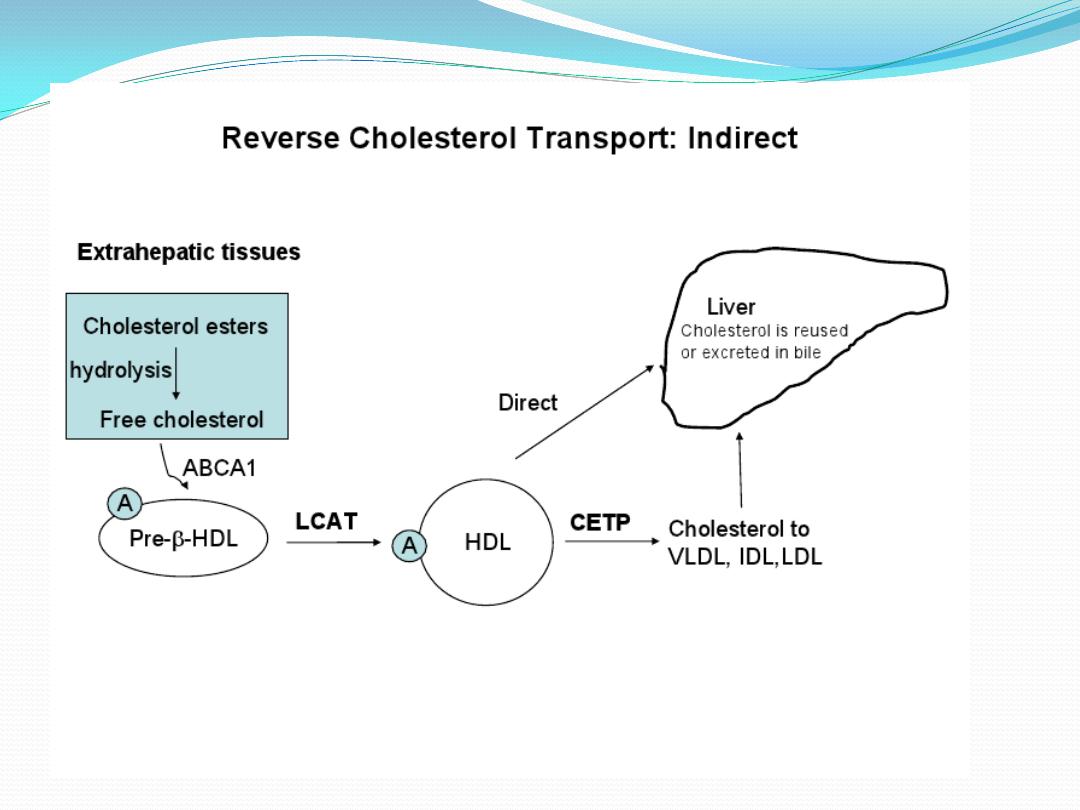
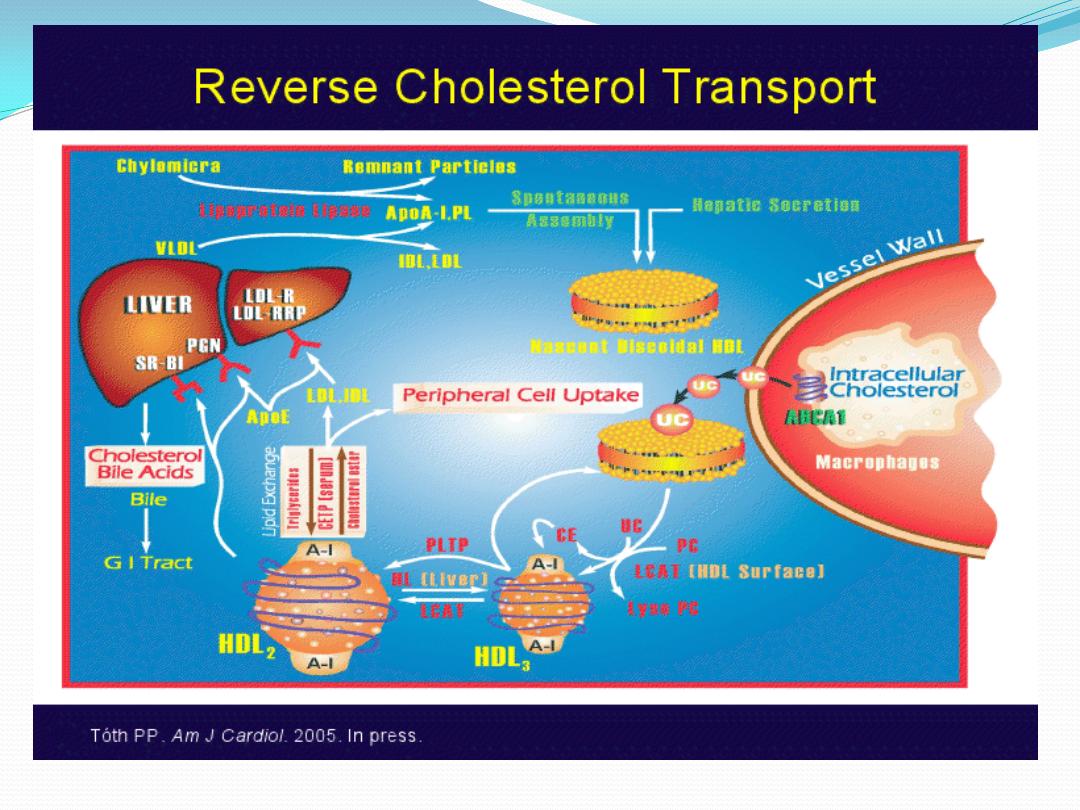
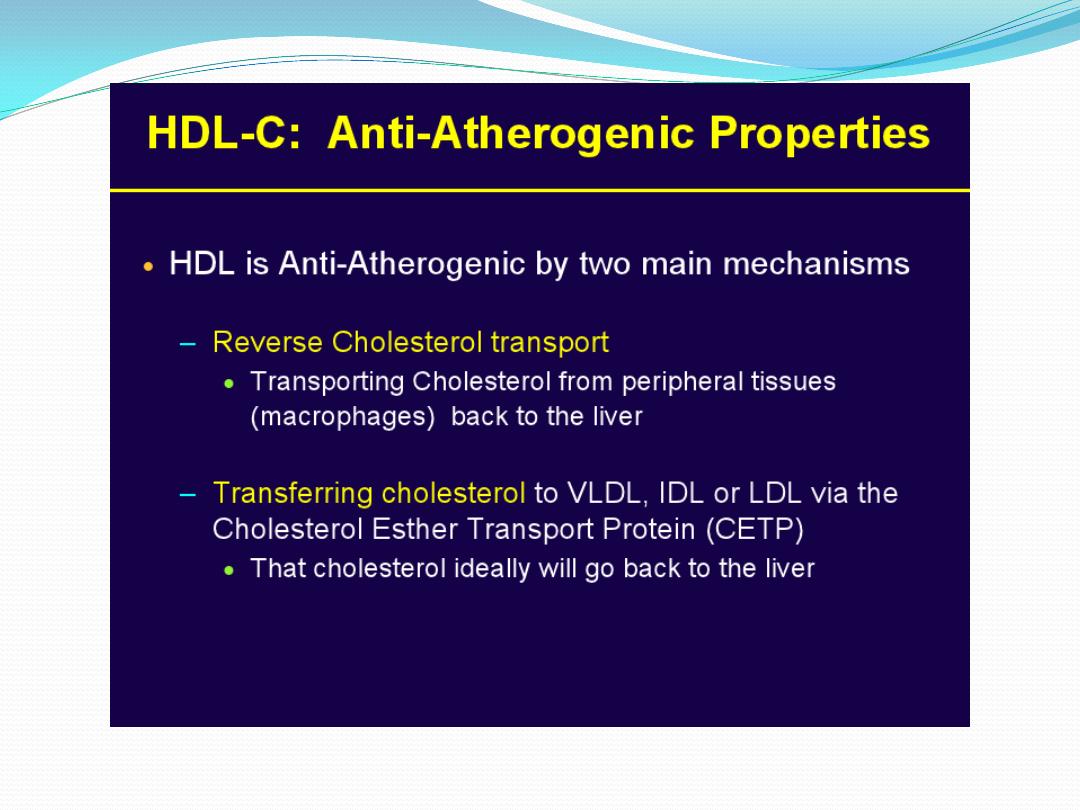
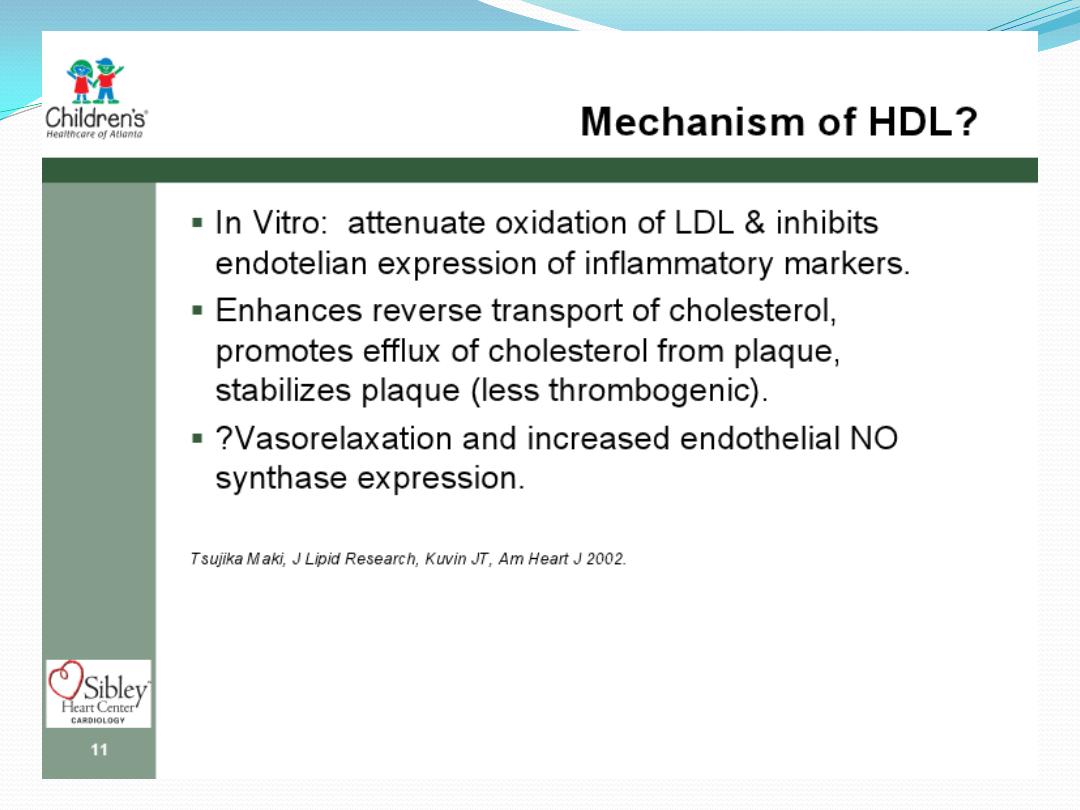
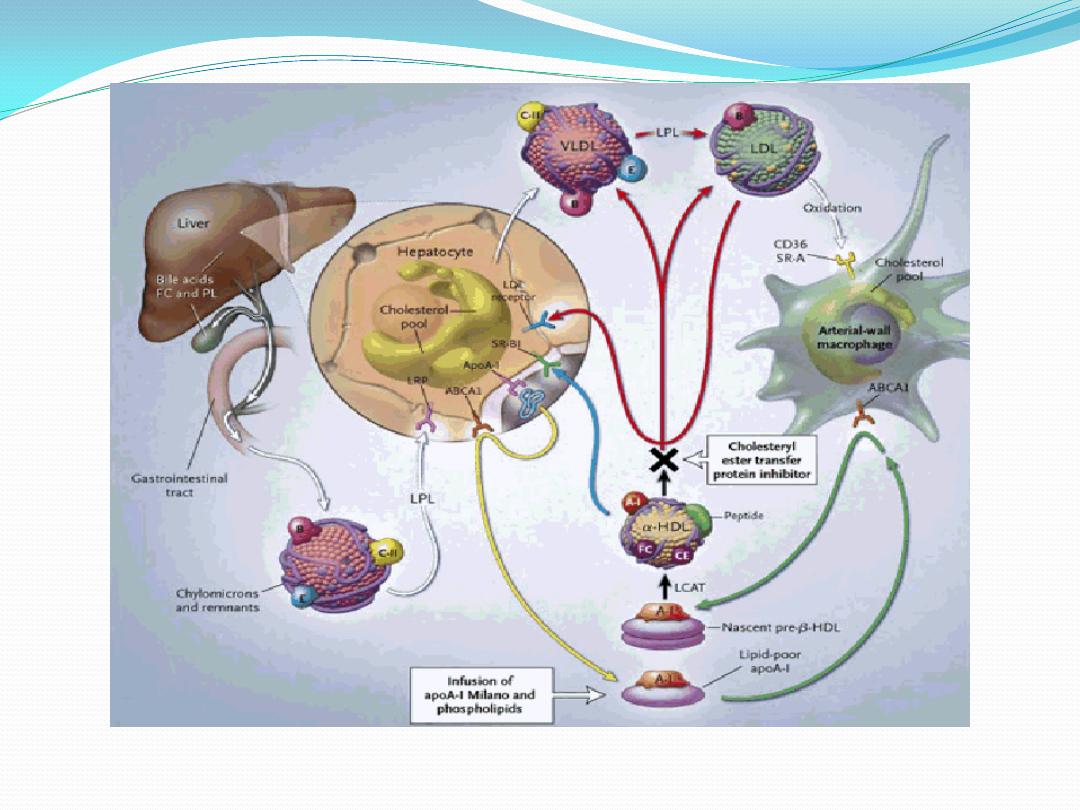
HDL-C
It
is cholesterol-rich particle and the
protective lipid. Its blood concentrations have inverse
correlation with the risk and the incidence of CAD.
It is
the carrier LP of excess amounts of cholesterol from the
peripheral tissues, such as the HEART (intracellular and
cell membranes) and returned it to the Liver, the only
route
for
removal
of
excess
cholesterol.
There are HDL3 and HDL2 which differ in their
cholesterol content. HDL2 is more cholesterol-
containing particle than HDL3. The reversed cholesterol
by HDL must be esterified to be captured and returned
to liver. LCAT, Lecithin Cholesterol Acyl Transferase, is
the enzyme responsible about esterification in the
presence
of
cofactor
apoAI.
CETP: Cholesterol Ester Transfer Protein.