Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
1
Digestion and Digestive Secretion from
Mouth and Stomach
Aim and objectives of lecture 2:
1. to describe the digestion process that occurs in the oral cavity
2. to describe the digestion processes that ocurs in the stomach
3. to define gastric secretions and the functions of its constituents
4. to describe the mechanism of secretion of gastric acid
5. to state the control of gastric acid secretion
6. to define Alkaline Tide
7. to define Intrinsic Factor
8. to state the absorption in the stomach
The Mouth
Ingestion: In the mouth food is ground, moistened and lubricated by saliva
(secreted by three pairs of salivary glands).
Digestion: salivary glands secrete
α-amylase, which digests starch into small
segments of
-dextrins and into individual soluble sugars. Salivary glands
also secrete lysozyme, which kills bacteria but is not classified as a digestive
enzyme.
Then the resulting bolus of food is swallowed into the esophagus and carried
by peristalsis to the stomach.
Pop quiz:
1. The swallowing of food or fluid from he mouth to the esophagus is
called:
a. deglutition
b. ingestion
c. absorption
d. peristalsis
2. Which of the following statements is false concerning saliva?
a. it aids in the formation of the bolus
b. it contains digestive enzymes
c. it is secreted from exocrine salivary glands
d. between 1000 and 1500 ml are secreted daily
e. none of the above
Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
2
The Stomach
Foodstuffs entering the stomach have been, crushed and reduced in size by
mastication, with saliva. The stomach provides four basic functions that assist in
the early stages of digestion and prepare the ingesta for further processing in the
small intestine:
1. It serves as a short-term storage reservoir, allowing a rather large
meal to be consumed quickly and dealt with over an extended period.
2. It is in the stomach that substantial chemical and enzymatic digestion is
initiated, particularly of proteins.
3. Vigorous contractions of gastric smooth muscle mix and grind foodstuffs with
gastric secretions, resulting in liquefaction of food, a prerequisite for
delivery of the ingesta to the small intestine.
4. As food is liquefied in the stomach, it is slowly released into the small
intestine for further processing.
Pop quiz: which of the following is not a function of the stomach:
a. Formation of chyme
b. Secretion of gastric juice
c. Storage of ingested food
d.
Absorption of fat
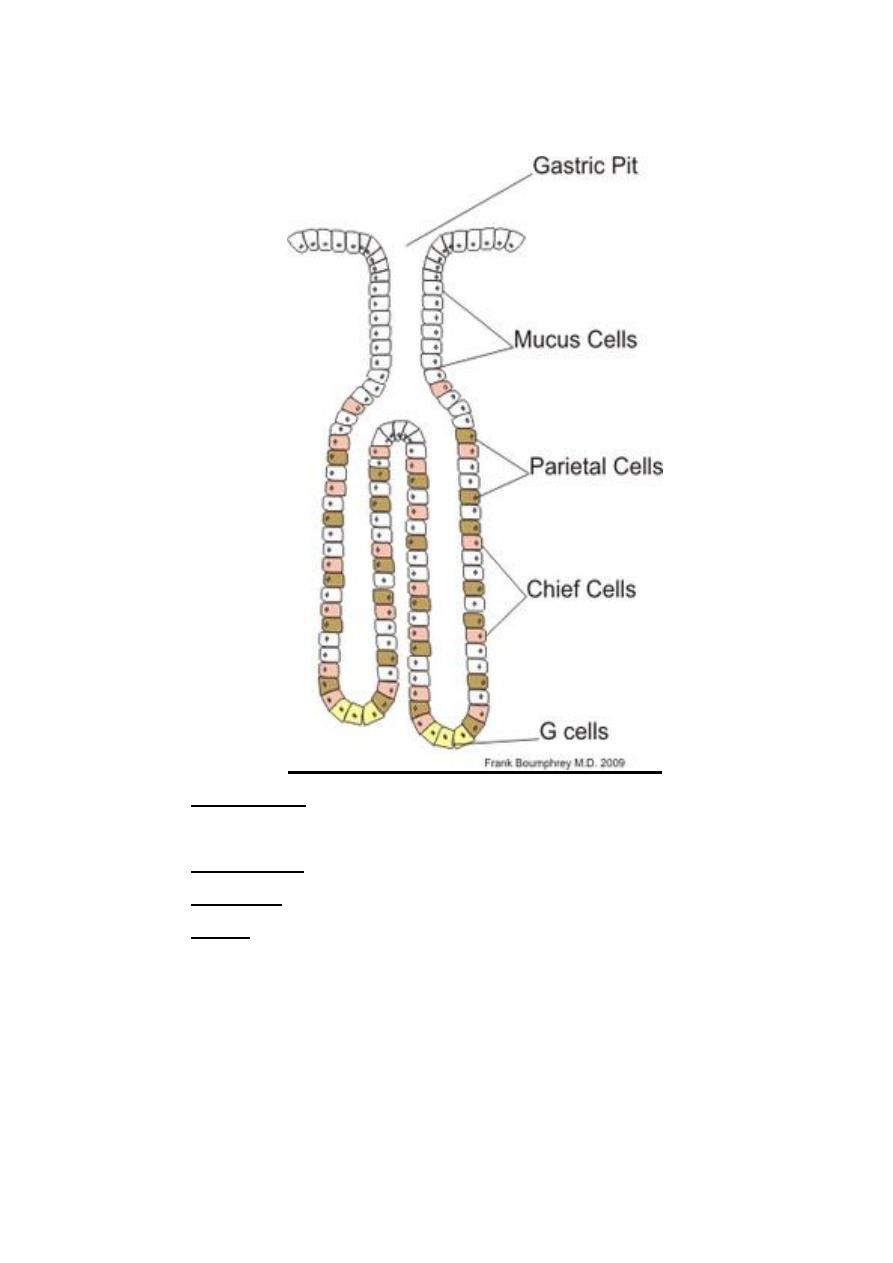
The wall of the stomach is lined with millions of gastric glands (appearing as
gastric pits extended into the mucosa as straight and branched tubules)
,
which together secrete 400
–800 ml of gastric juice at each meal. Several
kinds of cells are found in the gastric glands.
Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
3
Four major types of secretory epithelial cells cover the surface of the stomach and
extend down into gastric pits and glands:
1. Mucous cells: secrete an alkaline mucus that protects the
epithelium against shear stress and acid
2. Parietal cells: secrete hydrochloric acid.
3. Chief cells: secrete pepsin, a proteolytic enzyme
4. G cells: secrete the hormone gastrin

Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
4
Gastric secretions
1. Mucosal Protection
Mucus layer on gastric surface forms a mucosal barrier to damage against
several forms of potential injury to the gastric mucosa.
1. A gel 0.2mm thick; 80% CHO; 20% protein
2. Secreted by neck cells, surface epithelium
3. Can be cleaved by pepsin, so continual production is required
4. Release is stimulated by acetylcholine from nerve endings
5. Also rich in bicarbonate
a. HCO
3
-
content creates a "micro-environment" around surface cells to
prevent acid damage
b. HCO
3
-
secretion is inhibited by adrenergic input (prominent in stress)
2. Acid Secretion
Hydrochloric acid is secreted from parietal cells into the lumen where it
establishes an extremely acidic environment. This acid is important for activation
of pepsinogen and inactivation of ingested microorganisms such as bacteria.
2.1. Function of Gastric acid
1. To kill micro-organisms: (but H. pylori survives by making ammonia (basic) from
urea using urease).
2. to activate pepsinogens (cleaved to form pepsin) and provide the optimal pH for
pepsin action
3. to facilitate absorption of iron by converting colloidal iron into ionic form.
4. to stimulate duodenum to liberate secretin
5. breaks down connective tissue in food
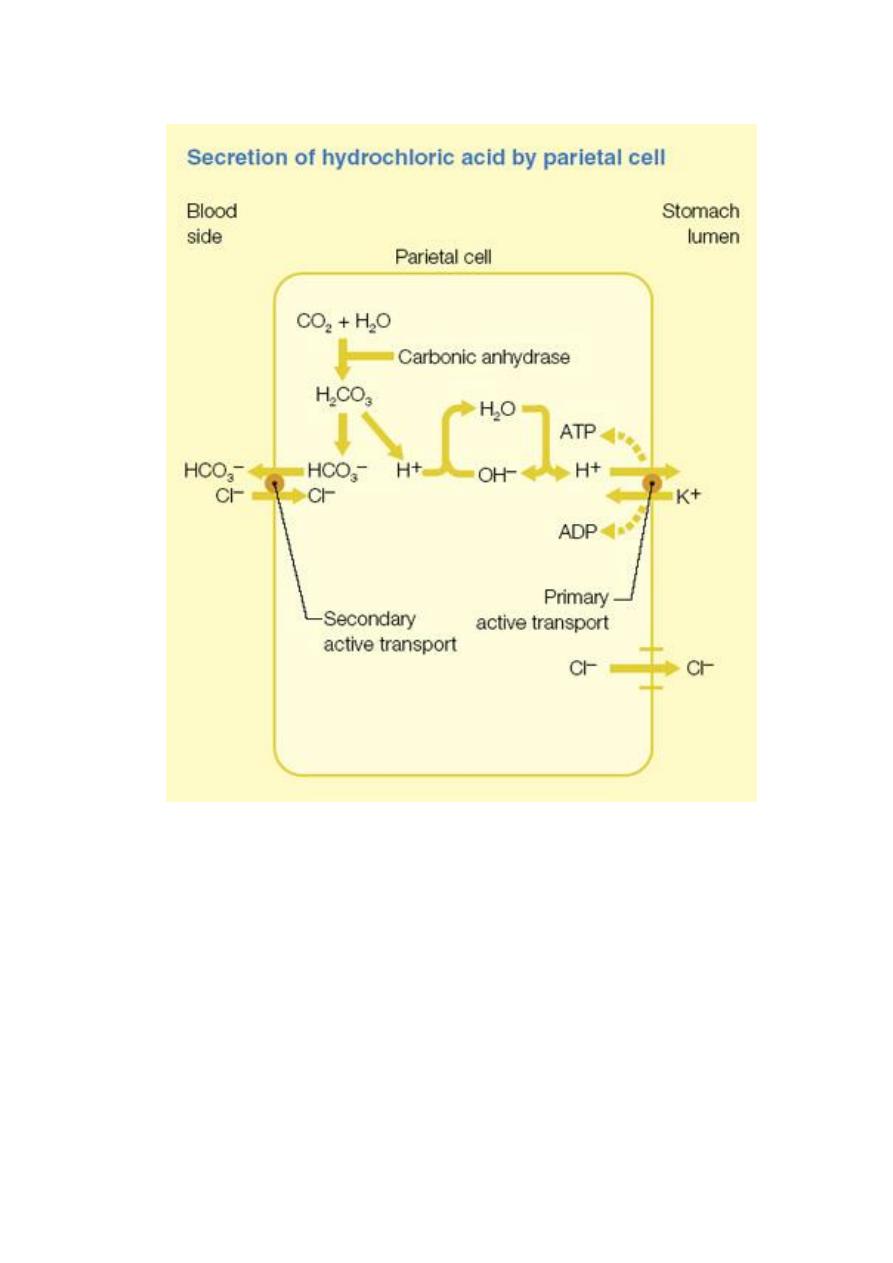
2.2.Mechanism of gastric acid secretion
As the plasma pH = 7.4, the parietal cell transports protons against a
concentration gradient of 10
6.6
. The free energy required for HCl secretion
under these conditions is minimally 9.1 kcal
mol-1
of HCl. That is why parietal
cells are stuffed with mitochondria and uses huge amounts of energy as they carry
out this three-million fold concentration of protons.
Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
5
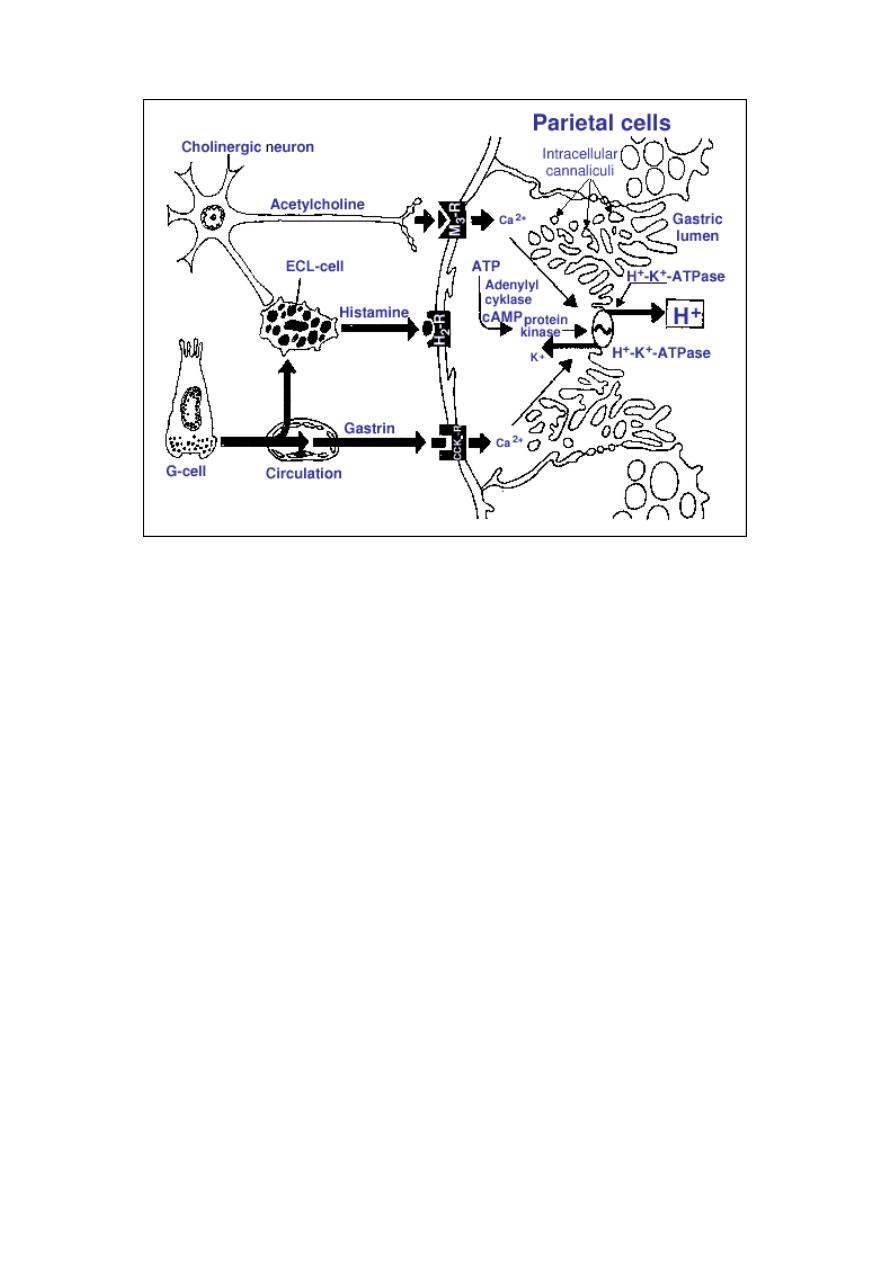
Acid secretion mechanisms in the parietal cell
The key player in acid secretion is a H+/K+ ATPase or "proton pump" located in
the cannalicular membrane. This ATPase is magnesium-dependent. This
enzyme is unique to the parietal cell and is found only in the luminal region
of the plasma membrane. It couples the hydrolysis of ATP to an electrically
neutral obligatory exchange of K
+
for H
+
, secreting H
+
and taking K
+
into
the cell.
As the K
+
/H
+
ATPase generates a very acidic solution, protein reagents that
are activated by acid can become specific inhibitors of this enzyme. This
fact is a key in most drugs used to treat peptic ulcers.

Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
6
Pop quiz: Parital cells in the stomach secretes gastric juice by transporting
protons from a low concentration to a very high concentration, this requires
a huge amount of energy. That is why they are stuffed with:
a. lyosomes
b. mitochondria
c. Golgi apparatus
d. RNA
The current model for explaining acid secretion is as follows:
1. Hydrogen ions are generated within the parietal cell from dissociation of water. The
hydroxyl ions formed in this process rapidly combine with carbon dioxide to form
bicarbonate ion, a reaction cataylzed by carbonic anhydrase.
2. Bicarbonate is transported out of the basolateral membrane in exchange for
chloride. The outflow of bicarbonate into blood results in a slight elevation of blood
pH known as the "alkaline tide". This process serves to maintain intracellular pH in
the parietal cell.
3. Chloride and potassium ions are transported into the lumen of the cannaliculus by
conductance channels, and such is necessary for secretion of acid.
4. Hydrogen ion is pumped out of the cell, into the lumen, in exchange for potassium
through the action of the proton pump; potassium is thus effectively recycled.
2.3. Control of gastric acid secretion
Parietal cells bear receptors for three stimulators of acid secretion, reflecting a
neural, paracrine and endocrine control:
ACETYLCHOLINE
o released from cholinergic nerve fibres
o binds to (M3) receptor on cell surface
o opens Ca
++
channels in apical surface
o promotes release of Ca
++
from intracellular stores
GASTRIN
o binds to CCK-B receptor on cell surface
o releases intracellular Ca
++
HISTAMINE
o released from mast cells
o binds to parietal cell surface receptor
o activates adenyl cyclase (increases cyclic AMP, an intracellular
messenger)
Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
7
Histamine's effect on the parietal cell is to activate adenylate cyclase, leading to elevation
of intracellular cyclic AMP concentrations and activation of protein kinase A (PKA). One
effect of PKA activation is phosphorylation of cytoskeletal proteins involved in transport of
the H+/K+ ATPase from cytoplasm to plasma membrane. Binding of acetylcholine and
gastrin both result in elevation of intracellular calcium concentrations.
INHIBITORY CONTROL
• acid at less than pH 2 is a direct inhibitor of acid release
• acid in duodenum releases secretin which inhibits gastric secretion
• fatty acids, peptides stimulate release of GIF (gastric inhibitory polypeptide)
and CCK (cholecystokinin)
Pop quiz: inhibitory controllers of gastric acid secretion include:
a. pH< 2 and secretin
b. pH> 2 and secretin
c. pH< 3 and gastrin
d. pH> 3 and gasretin
e. pH> 4 and gasretin
Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
8
Several additional mediators have been shown to result in gastric acid secretion when
infused into animals and people, including e.g. calcium.
Calcium simulates gastrin release. lt is unclear whether these molecules have a
significant physiologic role in parietal cell function.
Alkaline tide during gastric secretion: Owing to secretion of a large amount of
H
+
as HCl, there is surplus of OH
-
in the parietal cell which is taken up not only
by the CO
2
to form HCO
3
-
but also by other buffer systems of parietal cell
initially and later by those of plasma.
4
2
2
4
PO
H
HPO
3
2
3
CO
H
HCO
acid
Lactic
Lactate
All tend to increase on the side of the base i.e.:HPO
4
-2
, HCO
3
-
and lactate,
with the result that the pH of plasma is raised and an alkaline urine is
excreted for some hours following intake of food and gastric secretion. This
is known as the alkaline tide.
Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
9
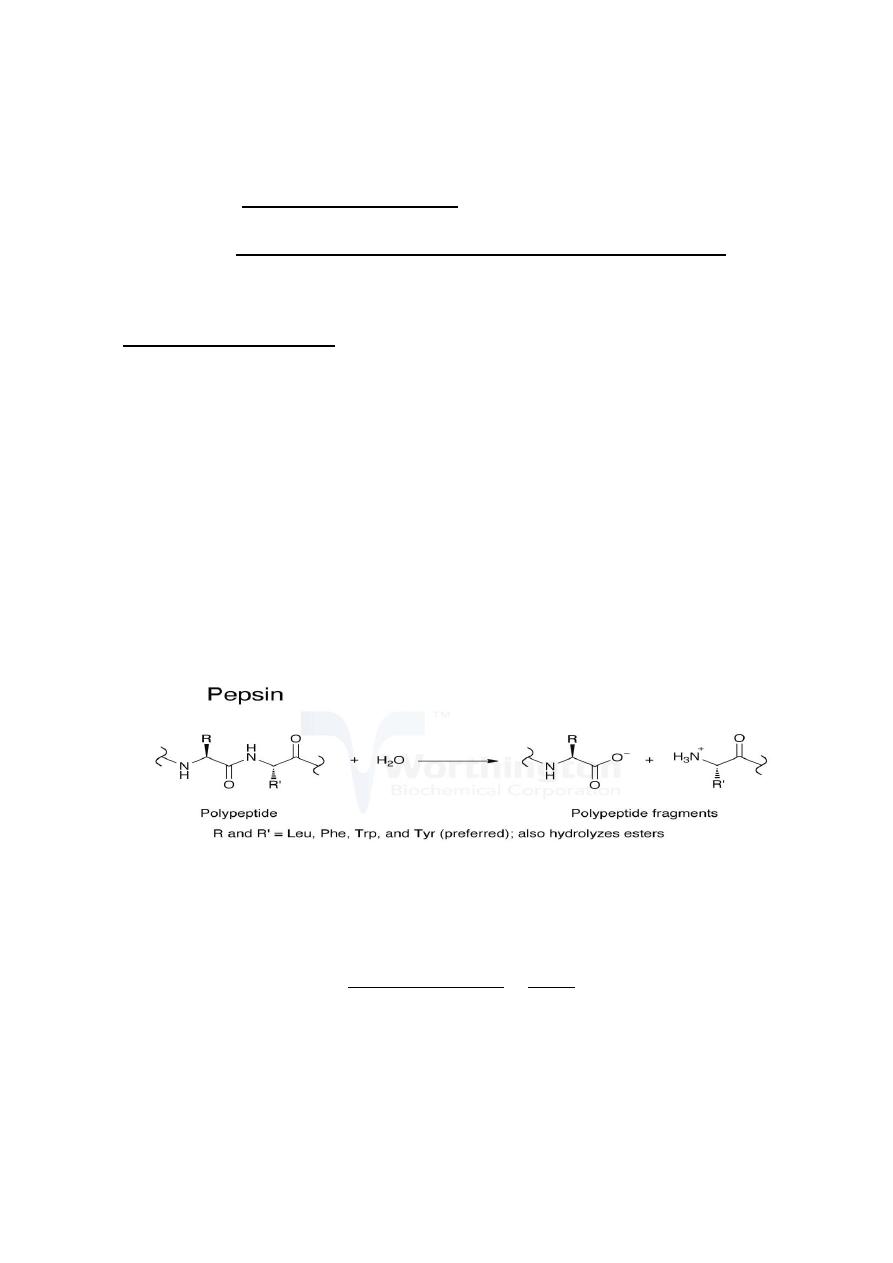
3. Proteases:
Pepsinogen, an inactive zymogen, is secreted into gastric juice from both
mucous cells and chief cells. Once secreted, pepsinogen is activated by stomach
acid into the active protease pepsin, which is largely responsible for the
stomach's ability to initiate digestion of proteins, in young animals; chief cells
also secrete chymosin (rennin), a protease that coagulates milk protein allowing
it to be retained more than briefly in the stomach.
Pepsinogens and Pepsins
Pepsinogens are secreted in a form such that the activation peptide
assumes a compact structure that occludes the active site. On exposure to an
acidic (pH < 4) environment such as occurs in the lumen of the stomach, the
activation peptide unfolds, allowing the active site to clip it off, yielding mature,
catalytically active pepsin.
Optimal activity of pepsins is at pH of 1.8 to 3.5, depending on the isoform, They
are reversibly inactivated at about pH 5 and irreversibly inactivated at pH 7 to 8.
The mature, active enzymes are roughly 325 amino acids with a mass of
approximately 35 kDa.
Pepsin initiates protein digestion by splitting certain amino acid linkages in
proteins (Cleaves preferentially C-terminal. It does not cleave at V, A or G. Other
residues may be cleaved, with very variable rates) to yield peptide fragments.
Because pepsin can digest protein, it must be stored and secreted in an inactive
form so that it does not digest the cells in which it is formed.
In general, secretion of pepsinogens is coupled to secretion of acid from
the parietal cell.
Pepsin was discovered by Theodor Schwann in 1836. It was the first animal
enzyme to be discovered.
Pop quiz: pepsinogen:
a. is a secretion of the G cells o gastric glands
b. is converted to pepsin in the acidic environment of the stomach
c. is a hormone
d. a and c
Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
10
Chymosin (Rennin) and the Coagulation of Milk
Chymosin, known also as rennin, is a proteolytic enzyme synthesized by chief
cells in the stomach. Its role in digestion is to coagulate milk in the stomach,
a process of considerable importance in the very young animal. If milk
were not coagulated, it would rapidly flow through the stomach and miss the
opportunity for initial digestion of its proteins.
Chymosin efficiently converts liquid milk to a semisolid like cottage cheese,
allowing it to be retained for longer periods in the stomach. Chymosin
secretion is maximal during the first few days after birth, and declines
thereafter, replaced in effect by secretion of pepsin as the major gastric
protease.
Chymosin is secreted as an inactive proenzyme called prochymosin that, like
pepsin, is activated on exposure to acid. Chymosin is also similar to pepsin
in being most active in acidic environments, which makes sense considering its
mission.
4. Hormones
The principle hormone secreted from the gastric epithelium is gastrin, a peptide
that is important in control of acid secretion and gastric motility. Gastrin is
secreted by G-cells and released into the blood where it travels to the parietal
cells to stimulate acid secretion, and to Enterochromaffin-Like (ECL) Cells to
stimulate histamine secretion.
The net result of gastrin secretion is increased acid production through
two mechanisms:
1. Direct stimulation of the parietal cells,
2. Tropic action on parietal cells increasing their number.
N.B. in gastrinoma (Zollinger-Ellison syndrome) increased production of gastrin
causes hypersecretion of acid which is not subject to normal inhibitory
mechanisms.
Pop quiz: In gastrinoma (Zollinger-Ellison syndrome) , all true except:
a. there is an increased production of gastrin
b. there is an increase in secretion of acid
c. hyper secretion is subject to normal inhibitory mechanisms
d. there is a significant decrease in the pH of the stomach
Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
11
A number of other enzymes are secreted by gastric epithelial cells, including
a lipase and gelatinase. One secretory product of considerable importance in
man is intrinsic factor, a glycoprotein secreted by parietal cells that is
necessary for intestinal absorption of vitamin B
12
.
Intrinsic Factor
Intrinsic factor is a glycoprotein secreted by parietal (humans) of the gastric
mucosa. In humans, it has an important role in the absorption of vitamin B
12
(cobalamin) in the intestine, and failure to produce or utilize intrinsic factor
results in the condition pernicious anemia.
— as a result of an autoimmune
attack against parietal cells. In all mammals, vitamin B
12
is necessary for
maturation of erythrocytes, and a deficiency of this vitamin leads to
development of anemia. Since efficient absorption of vitamin B
12
in
humans depends on intrinsic factor, diseases which decrease the
secretion of intrinsic factor (e.g. atrophic gastritis), interfere with cleavage
of the binding proteins (e.g. pancreatic exocrine insufficiency) or decrease
binding and absorption of the intrinsic factor-vitamin B
12
complex (e.g. ileal
disease or resection) can result in this type of anemia.
Pop quiz: "pernicious anemia" a condition resulted from:
a. The failure to produce or utilize Vitamin K
b. Deficiency in iron
c. The failure to produce hemoglobin
d. The failure to produce or utilize transferrin
e. The failure to produce or utilize intrinsic factor
Absorption in the Stomach
The stomach absorbs very few substances, although small amounts of certain
lipid-soluble compounds can be taken up, including aspirin, other non-
steroidal anti-inflammatory drugs, and ethanol.
Notably, these substances are also well-recognized causes of gastric
irritation and their use (especially overuse) is commonly associated with
development of gastritis and gastric ulcers.
Pop quiz: The stomach absorbs very few substances including:
a)
carbohydrates and ethanol
b)
aspirin and minerals
c)
proteins and carbohydrates
d)
aspirin and ethanol
e)
ethanol and proteins

Lecture 2
Tuesday 24/9/2013
Prof. Dr.H.D.El-Yassin
2013
12
Conclusions:
1. In the mouth food is ground, moistened and lubricated by saliva which secrete
amylase, that digests starch.
2. In the stomach digestion of proteins begins and initiates
3. Gastric secretions has four main constituents
a. alkaline mucus
b. hydrochloric acid.
c. pepsin, a proteolytic enzyme
d. the hormone gastrin
each having its own function and regulators as mentioned in the text.
4. The parietal cells of gastric glands are capable of secreting HCl into the gastric
lumen. Luminal H
+
concentrations of up to 0.14 M (pH 0.8) have been observed.
5. Acid secretion is under a neural, paracrine and endocrine control
6. Alkaline Tide : Due to secretion of a large amount of H
+
as HCl, there will be a
surplus of OH
-
in the parietal cell which is taken up not only by the CO
2
to form
HCO
3
-
but also by other buffer systems of parietal cell all tend to increase on the
side of the base i.e.:HPO
4
-2
, HCO
3
-
and lactate, causing the pH of plasma to be
raised and an alkaline urine excreted
7. Intrinsic factor is a glycoprotein secreted by parietal (humans) of the gastric mucosa.
important for absorption of vitamin B
12
8. The stomach absorbs very few substances as mentioned in the text
