Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
1
SECRETION AND ABSORPTION IN
THE SMALL INTESTINE
I: ABSORPTION OF MONOSACCHARIDES
Aim and objectives of lecture 4:
1. to describe the mechanism of secretion in the small intestin
2. to describe the mechanism of absorption in the small intestin
a. in general
b. of water and electrolytes
c. of monosacharides
3. to give examples of clinical disorderes of the above mechanisms
The small intestine is the portal for absorption of virtually all nutrients into blood.
Accomplishing this transport requires breaking down large supramolecular aggregates into
small molecules that can be transported across the epithelium.
By the time ingesta reaches the small intestine, foodstuffs have been mechanically broken
down and reduced to a liquid by mastication and grinding in the stomach. Once within the
small intestine, these macromolecular aggregates are exposed to pancreatic enzymes and
bile, which enables digestion to molecules capable or almost capable of being absorbed.
The final stages of digestion occur on the surface of the small intestinal epithelium.
The net effect of passage through the small intestine is absorption of most of the water
and electrolytes (sodium, chloride, potassium) and essentially all dietary organic molecules
(including glucose, amino acids and fatty acids).
Through these activities, the small intestine not only:
1. provides Nutrients to the body, but
2. plays a critical Role in water and acid-base balance.
Secretion in the Small Intestine
Large quantities of water are secreted into the lumen of the small intestine during the
digestive process. Almost all of this water is also reabsorbed in the small intestine.
Regardless of whether it is being secreted or absorbed, water flows across the mucosa in
response to osmotic gradients.

Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
2
In the case of secretion, two distinct processes establish an osmotic gradient that pulls
water into the lumen of the intestine:
1. Increases in luminal osmotic pressure resulting from influx and digestion of
foodstuffs: The chyme that floods into the intestine from the stomach
typically is not hyperosmotic, but as its macromolecular components are
digested, osmolarlity of that solution increases dramatically.
Starch, for example, is a huge molecule that contributes only a small amount to osmotic
pressure, but as it is digested, thousands of molecules of maltose are generated, each of
which is as osmotically active as the original starch molecule.
Thus, as digestion proceeds lumenal osmolarity increases dramatically and water is pulled
into the lumen. Then, as the osmotically active molecules (maltose, glucose, amino acids)
are absorbed, osmolarity of the intestinal contents decreases and water can be absorbed.
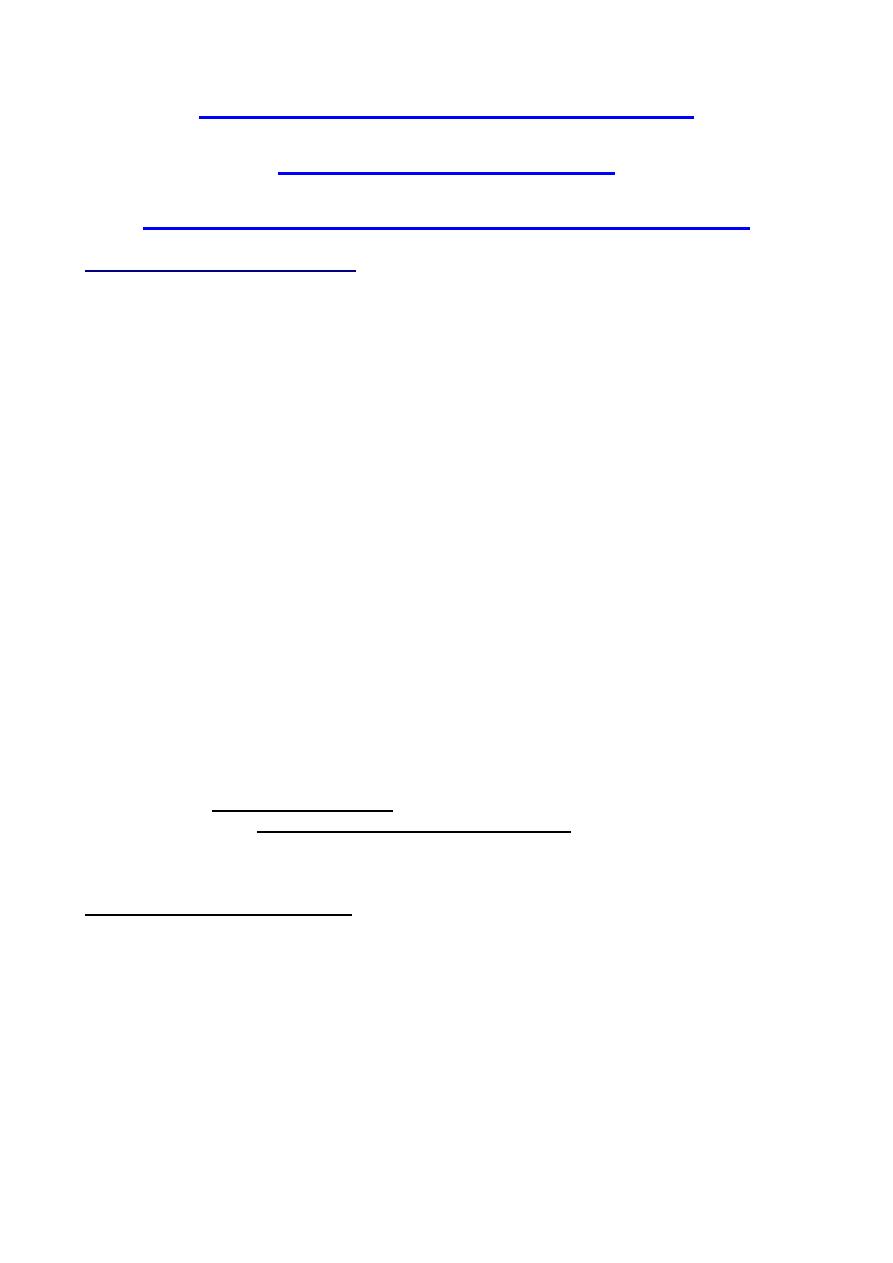
2. Crypt cells actively secrete electrolytes, leading to water secretion: The apical
or lumenal membrane of crypt epithelial cells contain an ion channel of
immense medical significance - a cyclic AMP-dependent chloride channel
known also as the cystic fibrosis transmembrane conductance regulator or
CFTR. Mutations in the gene for this ion channel result in the disease cystic
fibrosis. This channel is responsible for secretion of water by the following
steps:
1. Chloride ions enter the crypt epithelial cell by cotransport with sodium and
potassium; sodium is pumped back out via sodium pumps, and
potassium is exported via a number of channels.
2. Activation of adenylyl cyclase by a number of so-called secretagogues
leads to generation of cyclic AMP.
3. Elevated intracellular concentrations of cAMP in crypt cells activate the
CFTR, resulting in secretion of chloride ions into the lumen.
4. Accumulation of negatively-charged chloride anions in the crypt creates
an electric potential that attracts sodium, pulling it into the lumen,
apparently across tight junctions - the net result is secretion of NaCl.
5. Secretion of NaCl into the crypt creates an osmotic gradient across the
tight junction and water is drawn into the lumen.
Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
3
CLINICAL CORRELATION
Cystic fibrosis
Abnormal activation of the cAMP-dependent chloride channel (CFTR) in crypt cells has
resulted in the deaths of millions upon millions of people. Several types of bacteria
produce toxins that strongly, often permanently, activate the adenylate cyclase in crypt
enterocytes. This leads to elevated levels of cAMP, causing the chloride channels to
essentially become stuck in the "open" position". The result is massive secretion of water
that is manifest as severe diarrhea. Cholera toxin, produced by cholera bacteria, is the
best known example of this phenomenon, but several other bacteria produce toxins that
act similarly.
Pop quiz: The cystic fibrosis results from defective ion channels of:
1. Na
+
2. Cl
-
3. Ca
++
4. ClO
3
-
5. H
+
Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
4
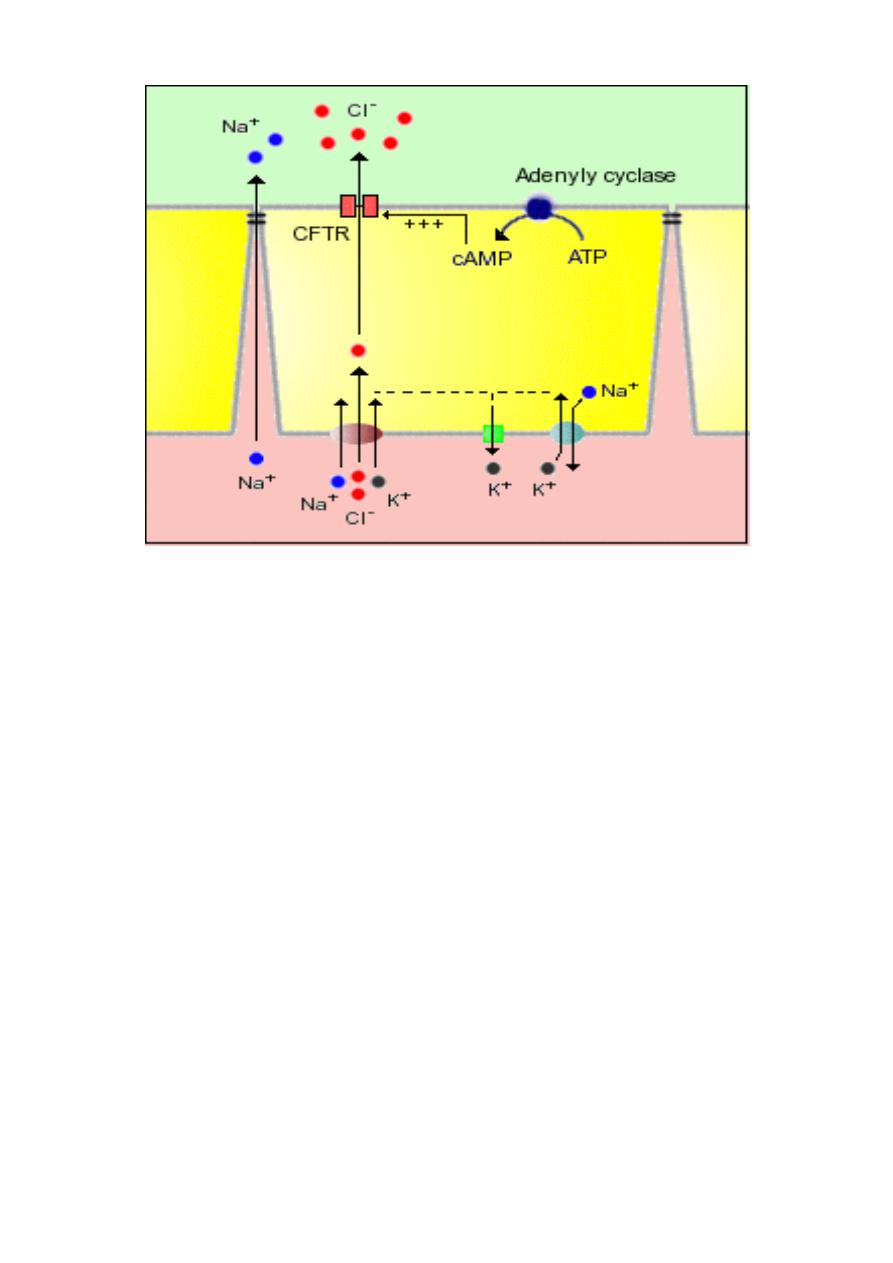
Absorption in the Small Intestine: General Mechanisms
Virtually all nutrients from the diet are absorbed into blood across the mucosa of the small
intestine.To remain viable, all cells are required to maintain a low intracellular
concentration of sodium. In polarized epithelial cells like enterocytes, low intracellular
sodium is maintained by a large number of Na
+
/K
+
ATPases – (sodium pumps) -
embedded in the basolateral membrane. These pumps export 3 sodium ions from the cell
in exchange for 2 potassium ions, thus establishing a gradient of both charge and sodium
concentration across the basolateral
membrane.
Pop quiz: the sodium –potassium pump
passes:
1. More Na
+
out than K
+
in
2. K
+
out and Na
+
in on a one for one
bases
3. Na
+
out and K
+
in on a one for one
bases
4. K
+
and Na
+
in the same direction
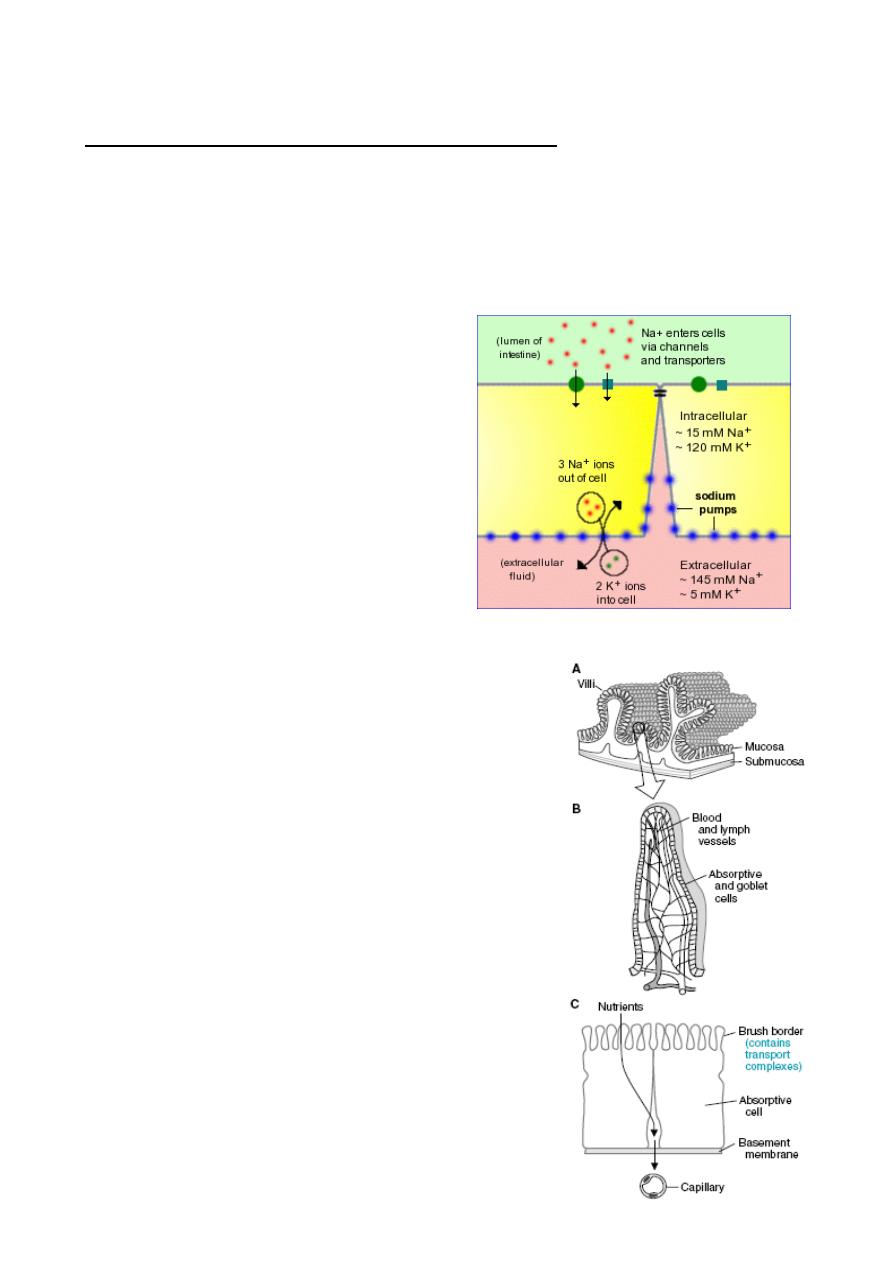
Pop quiz: What is the function of the villi in the small
intestine?
1. To decrease the amount of exposed surface
2. To facilitate enzyme retention and dispersal
3. To increase the surface area for absorption
and secretion
4. To sweep peptides across the surface with
wavelike actions
Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
5
1) Absorption of Water and Electrolytes
The small intestine must absorb massive quantities of water. A normal person takes in
roughly 1 to 2 liters of dietary fluid every day. On top of that, another 6 to 7 liters of fluid is
received by the small intestine daily as secretions from salivary glands, stomach,
pancreas, liver and the small intestine itself.
By the time the ingesta enters the large intestine, approximately 80% of this fluid has been
absorbed. Net movement of water across cell membranes always occurs by osmosis, and
the fundamental concept needed to understand absorption in the small gut is that
absorption of water is absolutely dependent on absorption of solutes, particularly sodium:
•
Sodium is absorbed into the cell by several mechanisms, but chief among them is
by co-transport with glucose and amino acids - this means that efficient sodium
absorption is dependent on absorption of these organic solutes.
•
Absorbed sodium is rapidly exported from the cell via sodium pumps - when a lot of
sodium is entering the cell, a lot of sodium is pumped out of the cell, which
establishes a high osmolarity in the small intercellular spaces between adjacent
enterocytes.
•
Water diffuses in response to the osmotic gradient established by sodium - in this
case into the intercellular space. It seems that the bulk of the water absorption is
transcellular, but some also diffuses through the tight junctions.
•
Water, as well as sodium, then diffuses into capillary blood within the villus.
2) Absorption of Monosaccharides
Monosaccharides, are only rarely found in normal diets. Rather, they are derived by
enzymatic digestion of more complex carbohydrates within the digestive tube.
Particularly important dietary carbohydrates include starch and disaccharides such as
lactose and sucrose. None of these molecules can be absorbed for the simple reason that
they cannot cross cell membranes unaided and, unlike the situation for monosaccharides,
there are no transporters to carry them across.
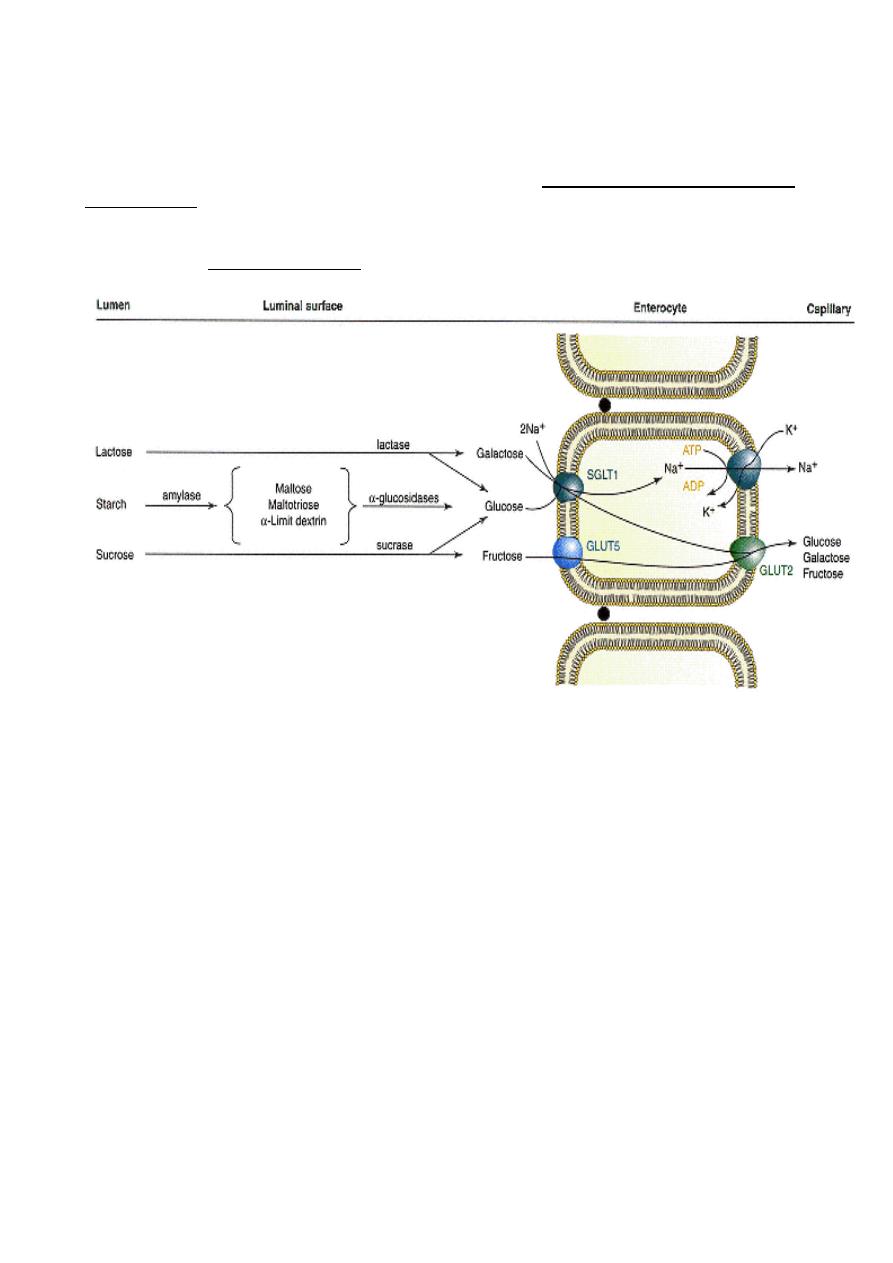
Brush Border Hydrolases Generate Monosaccharides
Polysaccharides and disaccharides must be digested to monosaccharides prior to
absorption and the key players in these processes are the brush border hydrolases, which
include maltase, lactase and sucrase. Dietary lactose and sucrose are "ready" for
digestion by their respective brush border enzymes. Starch, is first digested to maltose by
amylase in pancreatic secretions and, saliva.
Dietary lactose and sucrose, and maltose derived from digestion of starch, diffuse in the
small intestinal lumen and come in contact with the surface of absorptive epithelial cells
covering the villi where they engage with brush border hydrolases:
•
Maltase cleaves maltose into two molecules of glucose
•
Lactase cleaves lactose into a glucose and a galactose
•
Sucrase cleaves sucrose into a glucose and a fructose
Pop quiz: which enzyme splits a disaccharide to give out one molecule of fructose:
1.
Maltase
2.
Lactase
3.
Sucrase
4.
None
Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
6
Pop quiz Patient has a genetic defect that causes intestinal epithelial cells to produce
disaccharidases of much lower activity than normal. Compared with a normal person, after
eating a bowl of milk and oatmeal sweetened with table sugar, this patient will exhibit
higher levels of which of the following?
(A) Maltose, sucrose, and lactose in the stool
(B) Starch in the stool
(C) Galactose and fructose in the blood
(D) Glycogen in the muscles
(E) Insulin in the blood
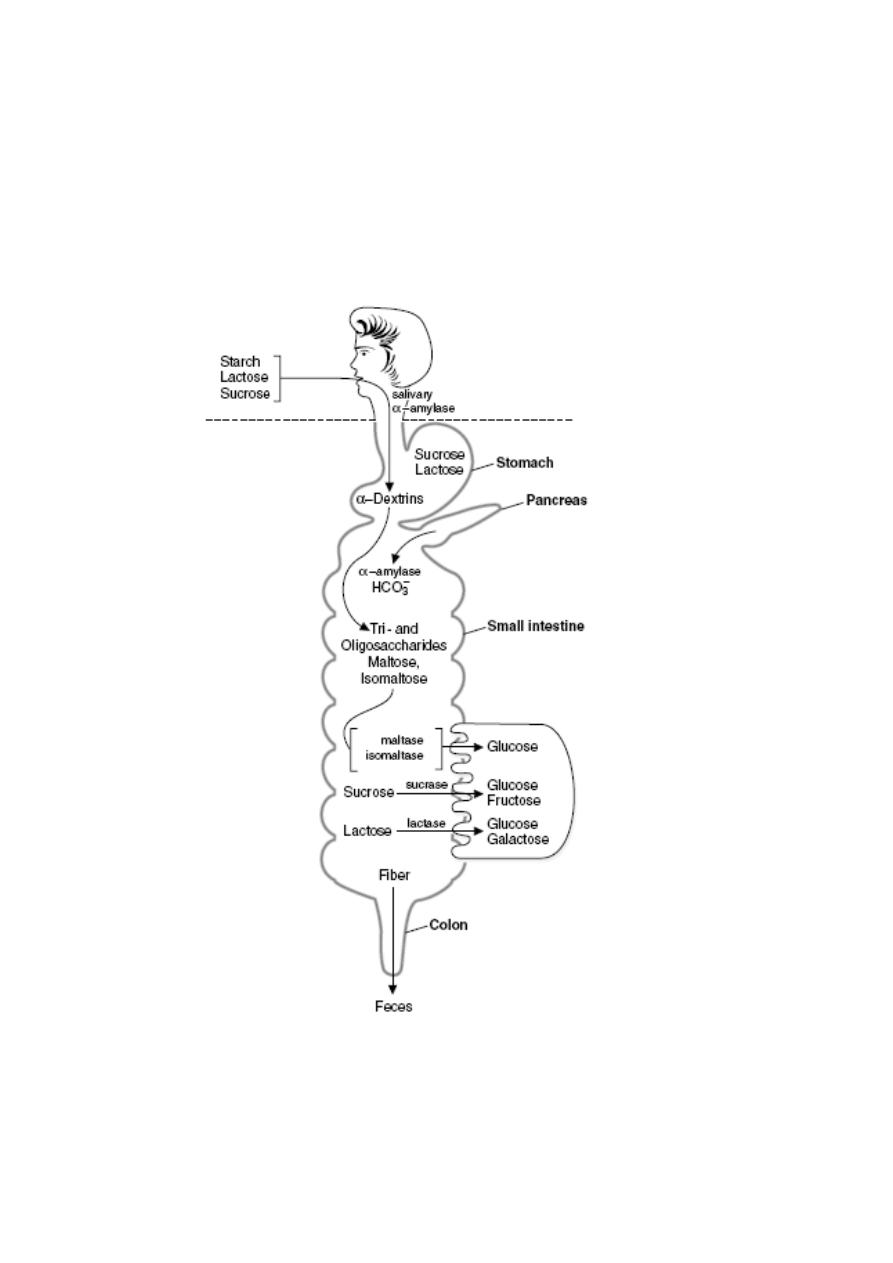
Overview of carbohydrate digestion. Digestion of the carbohydrates occurs first,
followed by absorption of monosaccharides. Subsequent metabolic reactions occur after
the sugars are absorbed.
Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
7
Absorption of Glucose and other Monosaccharides:
Transport across the Intestinal Epithelium
Absorption of glucose entails transport from the intestinal lumen, across the epithelium and
into blood.
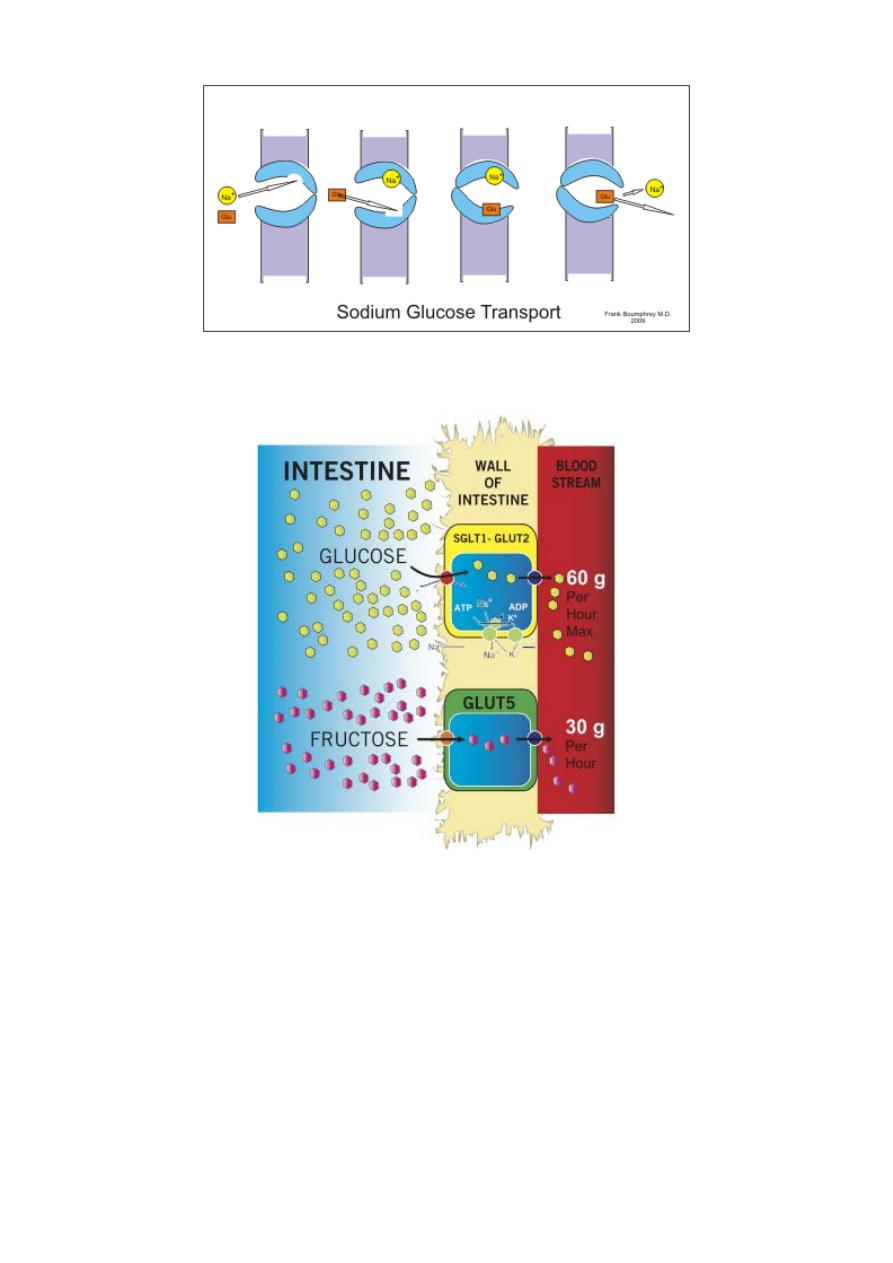
The transporter that carries glucose and galactose into the enterocyte is the sodium-
dependent hexose transporter, known more formally as SGLUT-1. As the name indicates,
this molecule transports both glucose and sodium ion into the cell and in fact, will not
transport either alone.
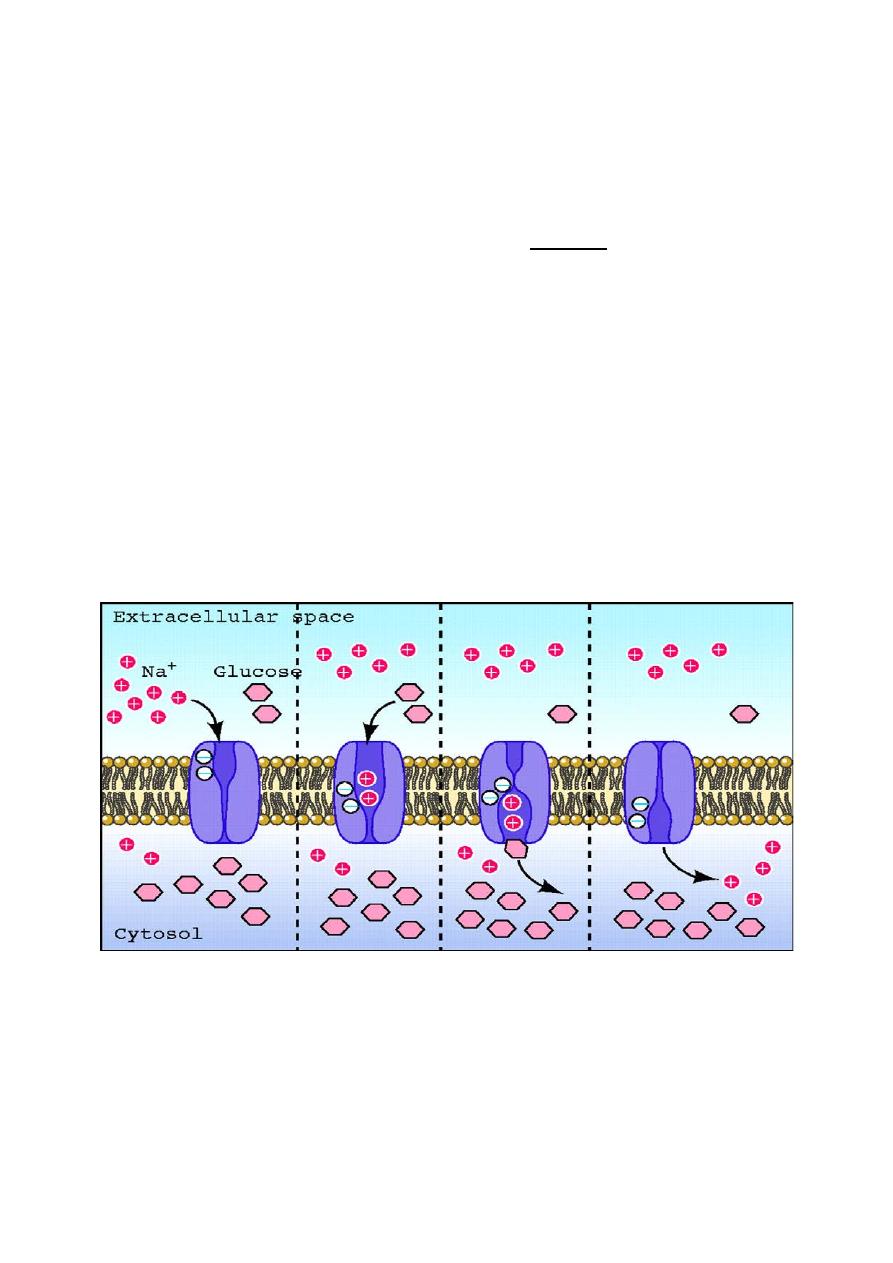
The essence of transport by the sodium-dependent hexose transporter involves a series of
conformational changes induced by binding and release of sodium and glucose, and can
be summarized as follow:
1. the transporter is initially oriented facing into the lumen - at this point it is capable of
binding sodium, but not glucose
2. sodium binds, inducing a conformational change that opens the glucose-binding
3. glucose binds and the transporter reorients in the membrane such that the pockets
holding sodium and glucose are moved inside the cell
4. sodium dissociates into the cytoplasm, causing glucose binding to destabilize
5. glucose dissociates into the cytoplasm and the unloaded transporter reorients back
to its original, outward-facing position
Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
8
Fructose is not co-transported with sodium. Rather it enters the enterocyte by another
hexose transporter (GLUT5).
Pop quiz : The facilitative transporter most responsible for transporting fructose from the
blood into cells is which of the following?
(A) GLUT 1
(B) GLUT 2
(C) GLUT 3
(D) GLUT 4
(E) GLUT 5
Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
9
Once inside the enterocyte, glucose and sodium must be exported from the cell into blood.
Sodium is rapidly shuttled out in exchange for potassium by the battery of sodium pumps
on the basolateral membrane, this process maintains the electrochemical gradient across
the epithelium.
The massive transport of sodium out of the cell establishes the osmotic gradient
responsible for absorption of water.
Na-dependent and facilitative transporters in the intestinal epithelial cells.
Both glucose and fructose are transported by the facilitated glucose transporters on the luminal and serosal
sides of the absorptive cells.
Glucose and galactose are transported by the Na_-glucose cotransporters on the luminal (mucosal) side of
the absorptive cells.
Pop quiz: Monosaccharides are absorbed from the intestine
a. by a Na
+
dependent cotranspoter for glucose and galactose (SGLUT1)
b. by a Na
+
independent facilitated transport for fructose (GLUT5)
c. by a Na
+
independent traspoter (GLUT2) across the contraluminal
membrane.
d. Against a concentration gradient if the transporter is Na
+
dependent
e. All of the above
Pop quiz: After digestion of a piece of cake that contains flour, milk, and sucrose as its
primary ingredients, the major carbohydrate products entering the blood are which of the
following?
(A) Glucose
(B) Fructose and galactose
(C) Galactose and glucose
(D) Fructose and glucose
(E) Glucose, galactose and fructose
Lecture 4
Sunday 29/9/2013
Prof. Dr. H.D.El-Yassin
2013
10
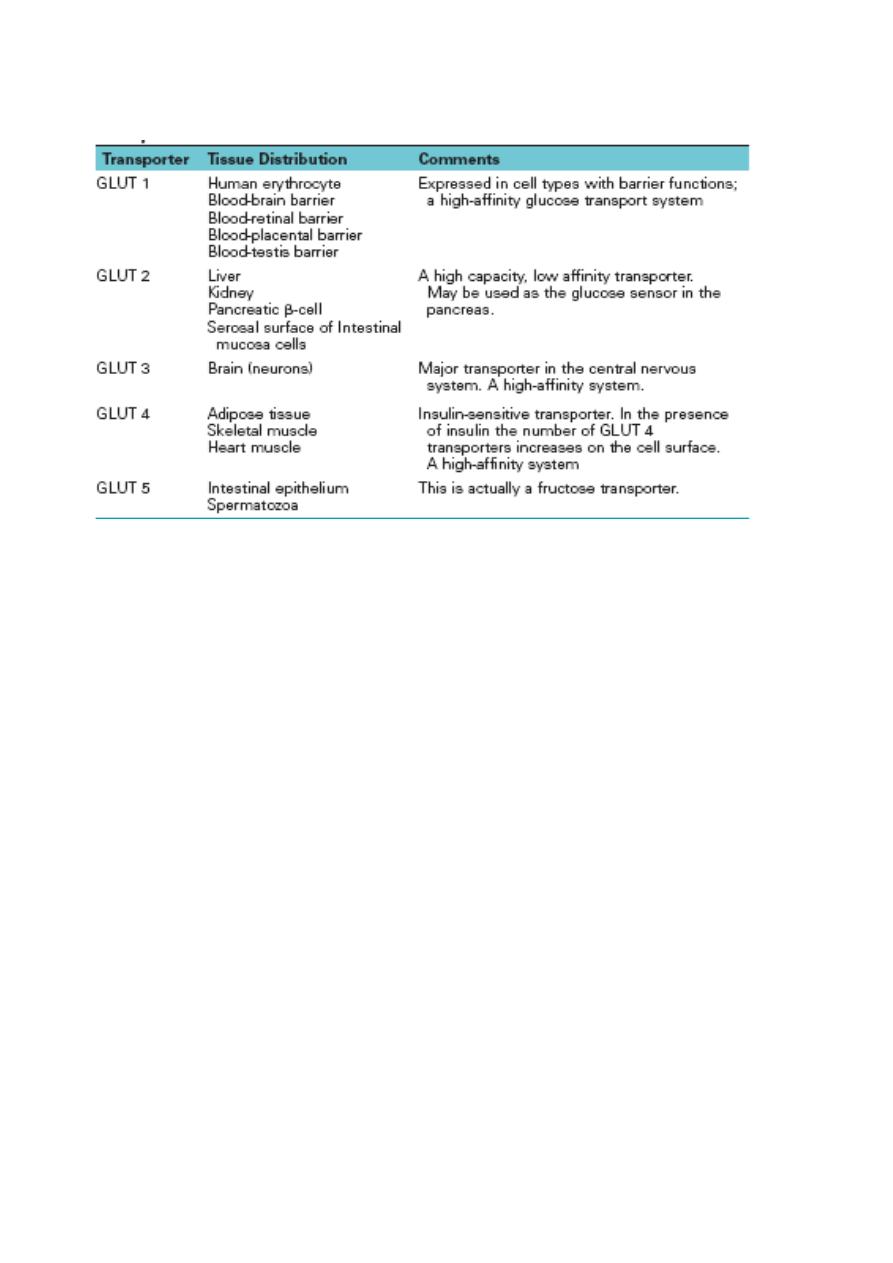
Properties of the GLUT 1-GLUT 5 Isoforms of the Glucose Transport Proteins
Genetic techniques have identified additional GLUT transporters (GLUT 7-12), but the role of these
transporters has not yet been fully described
CLINICAL CORRELATION
Disaccharidase Deficiency
Intestinal disaccharidase deficiencies are encountered relatively frequently in humans. Deficiency can
be present in one enzyme or several enzymes for a variety of reasons (genetic defect, physiological
decline with age, or the result of "injuries" to the mucosa). Of the disaccharidases, lactase is the most
common enzyme with an absolute or relative deficiency, which is experienced as milk intolerance. The
consequences of an inability to hydrolyze lactose in the upper small intestine are inability to absorb
lactose and bacterial fermentation of ingested lactose in the lower small intestine. Bacterial
fermentation results in the production of gas (distension of gut and flatulence) and osmotically active
solutes that draw water into the intestinal lumen (diarrhea). The lactose in yogurt has already been
partially hydrolyzed during the fermentation process of making yogurt. Thus individuals with lactase
deficiency can often tolerate yogurt better than unfermented dairy products. The enzyme lactase is
commercially available to pretreat milk so that the lactose is hydrolyzed
.
Conclusions
1. Large quantities of water are secreted into the lumen of the small intestine during the
digestive process water flows across the mucosa in response to osmotic gradients.
2. Glucose and galactose are taken into the enterocyte by cotransport with sodium
using the same transporter. Fructose enters the cell from the intestinal lumen via
facilitated diffusion through another transporter.
3. examples of clinical disorderes of the above mechanisms are mentioned in the text.
