
Gametogenesis
Prof. Dr. Malak A. Al-yawer
Objectives
At the end of this lecture, the medical student will
be able to
•
Identify the different stages of gametogenesis in
males and females
•
Name the functions of sertoli cells and
granulosa cells
•
Outline the stages of spermiogenesis
Gametogenesis
•
Is the process of formation of
gametes from germ cells in the
testes and ovaries
•
Many principles are the same
in both male and female
•
Is divided into 4 stages
1.
Extragonadal origin of
primordial germ cells
2.
Proliferation of germ cells
by mitosis
3.
Meiosis
4.
Structural and functional
maturation of ova and
spermatozoa
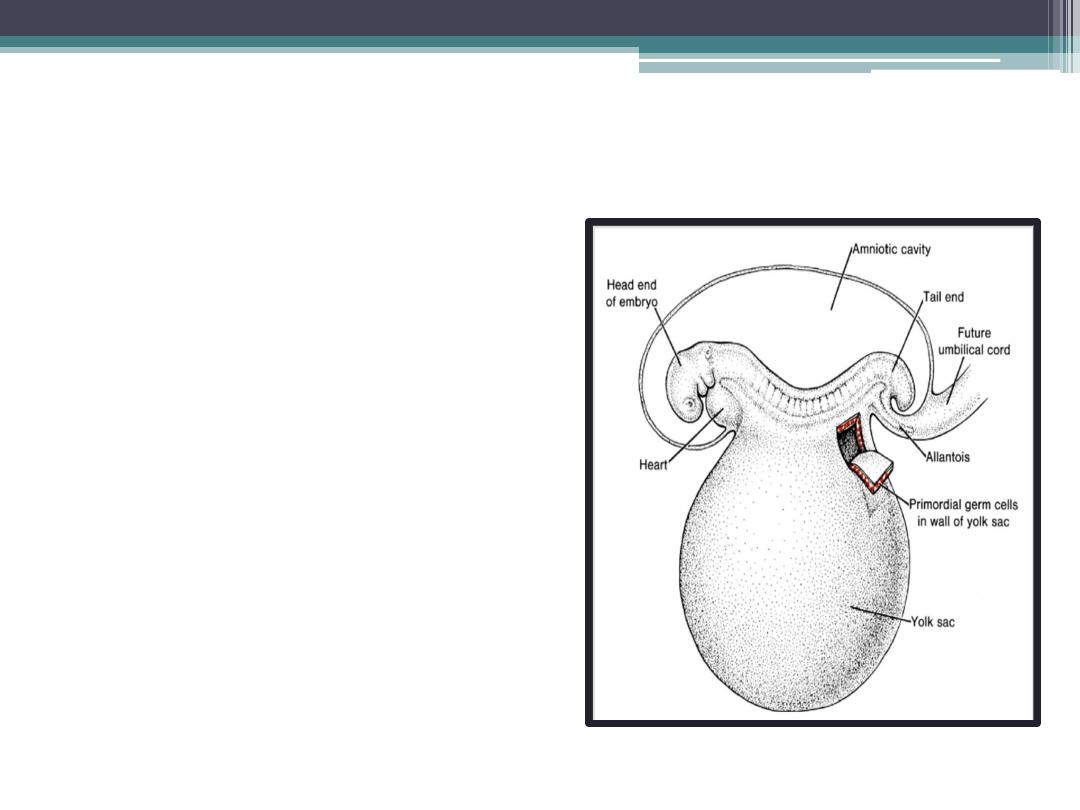
primordial germ cells
•
Gametes are derived
from
primordial germ
cells (PGCs)
that are
formed in the
epiblast
during the second week
and that move to the
wall of the yolk sac.
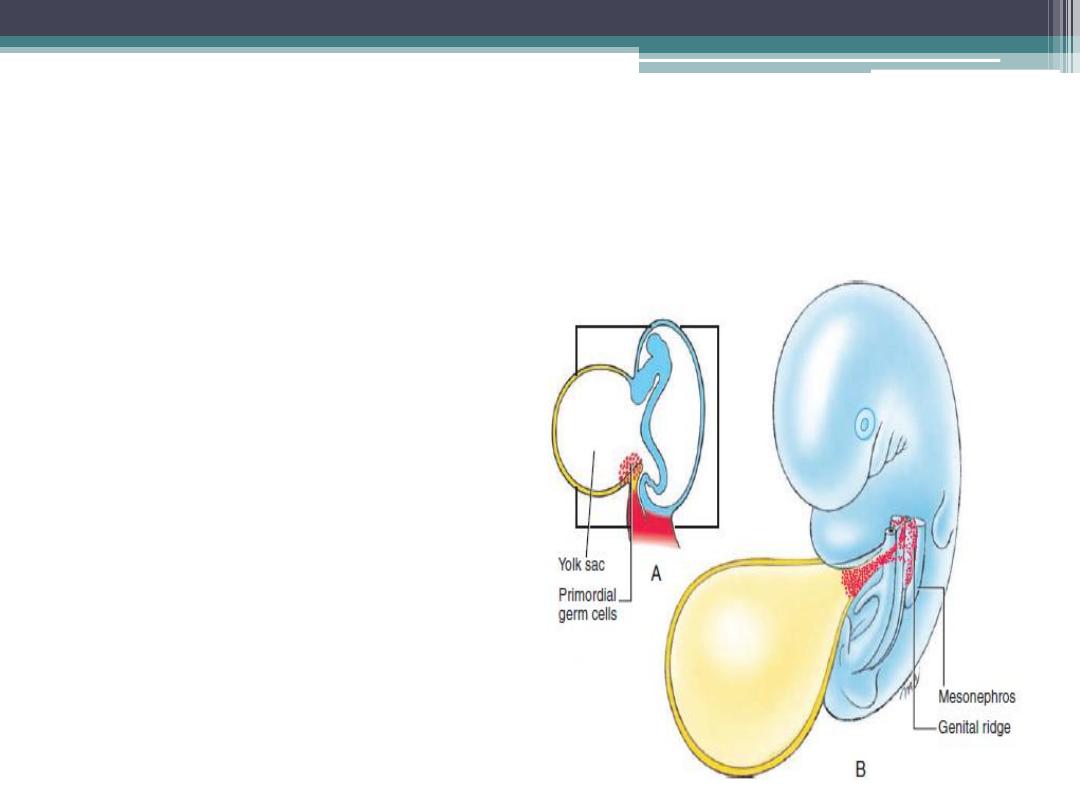
primordial germ cells
•
During the fourth week, these
cells begin to migrate ,by
ameboid movement , from the
yolk sac toward the
developing gonad
, where
they arrive by the end of the
fifth week
•
Mitotic divisions increase their
number during their migration
and also when they arrive in
the gonad.
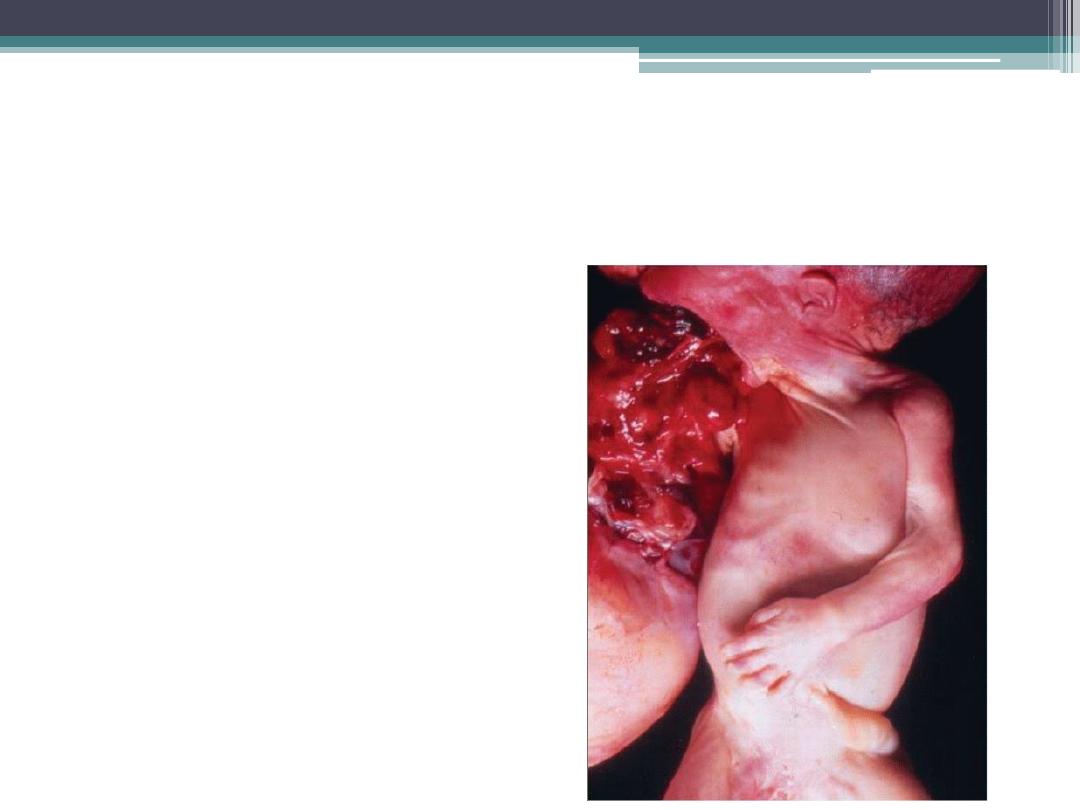
Oropharnyngeal teratoma
•
These tumors may arise from
pluripotent cells
1.
primordial germ cells or from
2.
epiblast cells
•
Tissues within the tumors
include derivatives of all
three germ layers and may
include gut, bone, skin, teeth,

Oogenesis
Is the process whereby oogonia
differentiate into mature oocytes

Oogenesis
Maturation of Oocytes Begins before Birth
•
Once
primordial germ cells
have arrived in the
gonad of a genetic female, they differentiate
into
oogonia
.
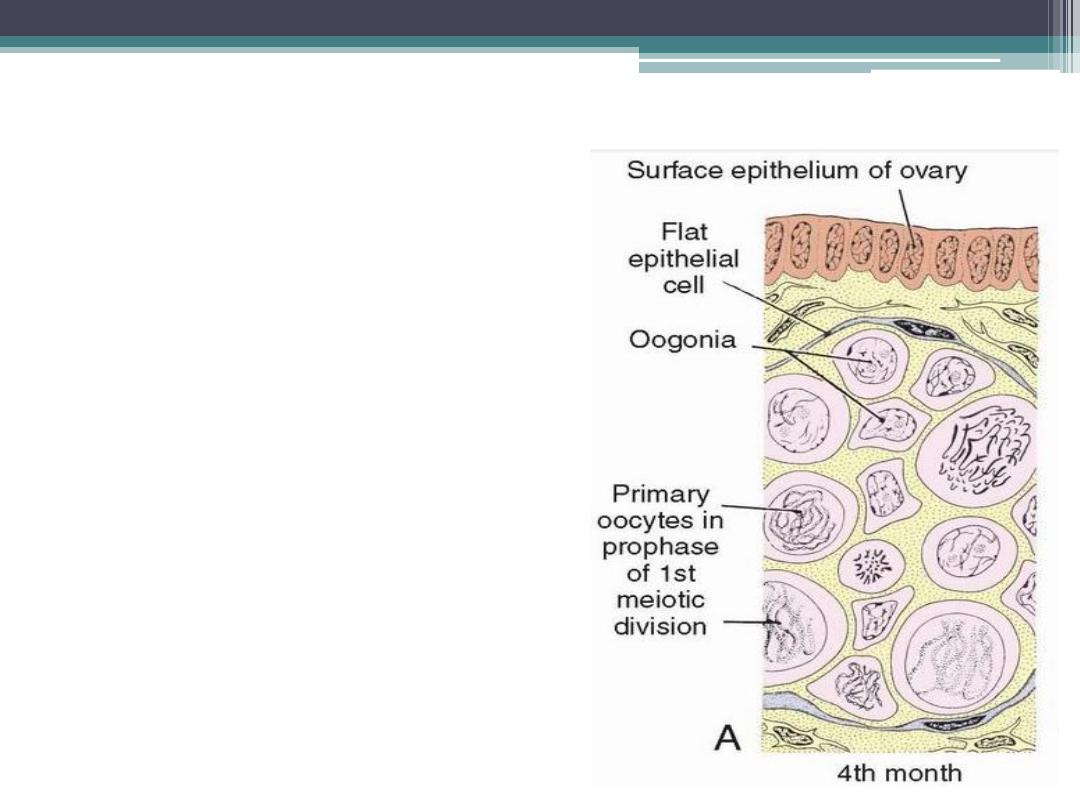
Oogonia
•
undergo a number of
mitotic divisions,
•
by the end of the third
month, they are arranged
in clusters
surrounded by
a layer of flat epithelial
cells( follicular cells),
originate from surface
epithelium covering the
ovary.
•
The majority of oogonia
continue to divide by
mitosis, but some of them
give rise to primary
oocytes that enter
prophase of the first
meiotic division.
•
By
the fifth month of
prenatal development
, the
total number of germ cells
in the ovary reaches its
maximum (7 million). At
this time, cell death begins,
and many oogonia as well
as primary oocytes become
atretic.
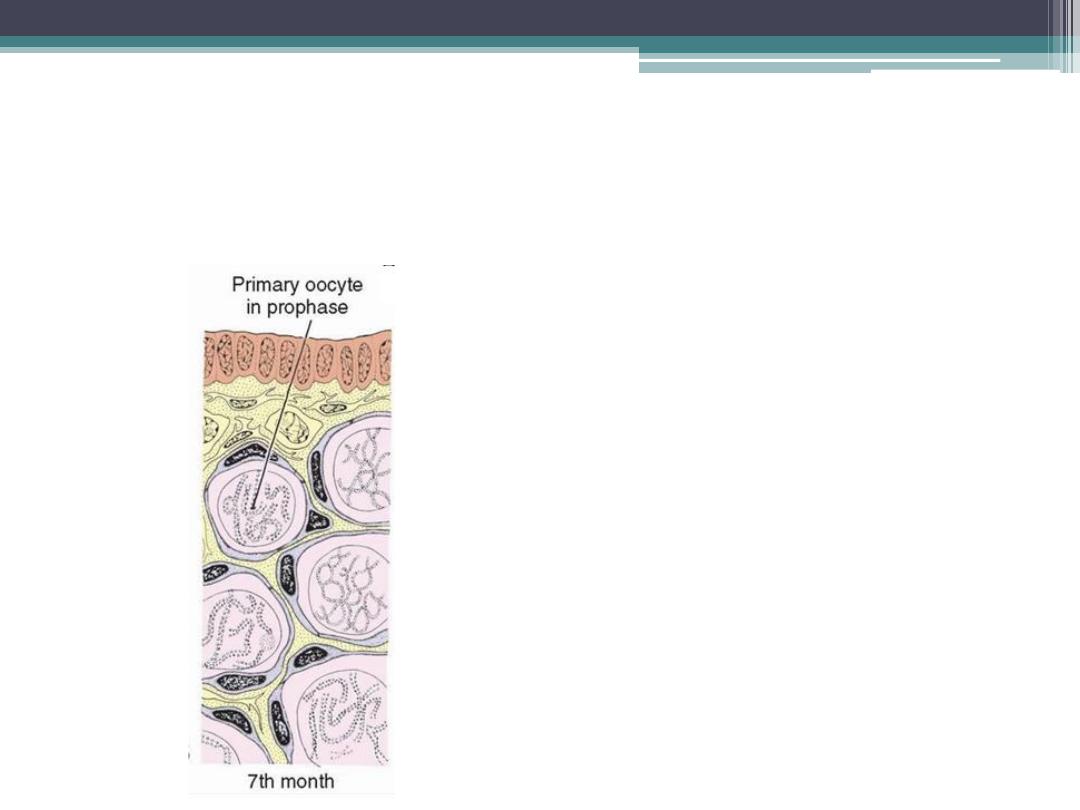
•
By the seventh month
, the
majority of oogonia have
degenerated except for a
few near the surface. All
surviving primary oocytes
have entered prophase of
meiosis I, and most of them
are individually
surrounded by a layer of
flat epithelial
cells(primordial follicle
).

Maturation of the oocytes
At birth and during childhood
•
Near the time of birth,
all
primary oocytes
have started
prophase of meiosis I, but instead
of proceeding into metaphase, they
enter
the diplotene stage
, a
resting stage during prophase that
is characterized by a lacy network
of chromatin .
•
Primary oocytes remain arrested in
prophase and do not finish their
first meiotic division before
puberty is reached. This arrested
state is produced by
oocyte
maturation inhibition (OMI
)
,
a small peptide secreted by
follicular cells.
•
The total number of primary
oocytes at birth is estimated to
vary from
700,000 to two million
•
During childhood, most oocytes
become atretic; only approximately
400,000
are present by the
beginning of puberty, and fewer
than 500 will be ovulated.

The diplotene stage is the most suitable phase to
protect the oocyte against environmental influences ?
•
Some oocytes that reach maturity late in life
have been dormant in the diplotene stage of the
first meiotic division for 40 years or more before
ovulation.
•
The fact that the risk of having children with
chromosomal abnormalities increases with
maternal age indicates that primary oocytes are
vulnerable to damage as they age.

Ovarian Cycle
•
At puberty, the female begins to undergo regular
monthly cycles.
•
Gonadotropin-releasing hormone (GnRH),
produced by the hypothalamus, acts on cells of
the anterior pituitary gland, which in turn
secrete gonadotropins. These hormones, follicle-
stimulating hormone (FSH) and luteinizing
hormone (LH), stimulate and control cyclic
changes in the ovary
•
Each month, 15 to 20 follicles selected from the pool
of primordial follicles begin to mature and passing
through three stages:
(1) primary,
(2) secondary or antral, and
(3) Tertiary or mature vesicular (Graafian) follicle.
•
The antral stage is the longest, whereas the mature
vesicular stage encompasses approximately 37 hours
before ovulation.
•
Under normal conditions, only one of these follicles
reaches full maturity, and the others degenerate and
become atretic.
•
corpus atreticum: When a follicle becomes atretic,
the oocyte and surrounding follicular cells
degenerate and are replaced by connective tissue
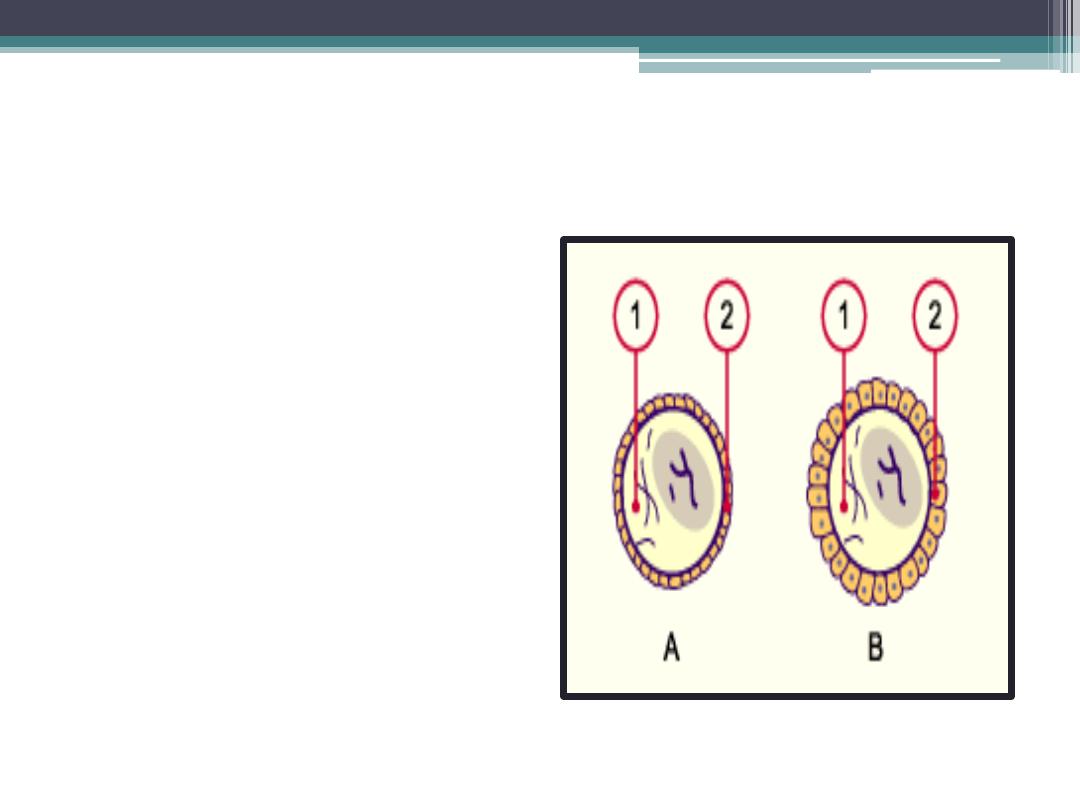
Unilaminar primary follicle
•
Primary oocyte
surrounded by a layer
of cuboidal epithelium
•
Beginning of zona
pellucida
•
A
Primordial follicle
B
Primary follicle
1
Oocyte
2
Follicular epithelium

Multilaminar primary follicle
•
Follicular cells proliferate
under the influence of FSH
and produce a stratified
epithelium of granulosa cells
•
Zona pellucida a layer of
glycoproteins on the surface
of the oocytes secreted by the
Granulosa cells and the
oocytes.
•
A basement membrane
separating the granulosa cells
from the theca folliculi

Secondary ( vesicular , antral )
•
fluid –filled spaces appear between the granulosa cells .coalescence of
these spaces form the antrum which is crescent shaped, but with time,
it enlarges . Granulosa cells surrounding the oocyte remain intact and
form the cumulus oophorus.
•
The follicle is surrounded by the theca interna, which is composed of
cells having characteristics of steroid secretion, rich in blood vessels,
and the theca externa, which gradually merges with the ovarian
connective tissue

Tertiary follicle
•
there is an abrupt increase in
LH that causes the primary
oocyte to complete meiosis I
and the follicle to enter the
preovulatory stage.

Maturation of the oocyte.
•
Meiosis I is completed, resulting in formation of two
daughter cells of unequal size, each with 23 double-
structured chromosomes . One cell, the secondary oocyte,
receives most of the cytoplasm; the other, the first polar
body, receives practically none. The first polar body lies
between the zona pellucida and the cell membrane of the
secondary oocyte in the perivitelline space.
•
The cell then enters meiosis II but arrests in metaphase
approximately 3 hours before ovulation.
•
Meiosis II is completed only if the oocyte is
fertilized; otherwise, the cell degenerates
approximately 24 hours after ovulation.
•
The first polar body may undergo a second
division

Ovulation
•
The oocyte, in metaphase of
meiosis II, is discharged from
the ovary together with a
large number of cumulus
oophorus cells.
•
Some of the cumulus
oophorus cells then rearrange
themselves around the zona
pellucida to form the corona
radiata
•
Follicular cells remaining
inside the collapsed follicle
differentiate into lutean cells.

Ovulation
•
is generally accompanied by a
rise in basal temperature &
•
there is middle pain
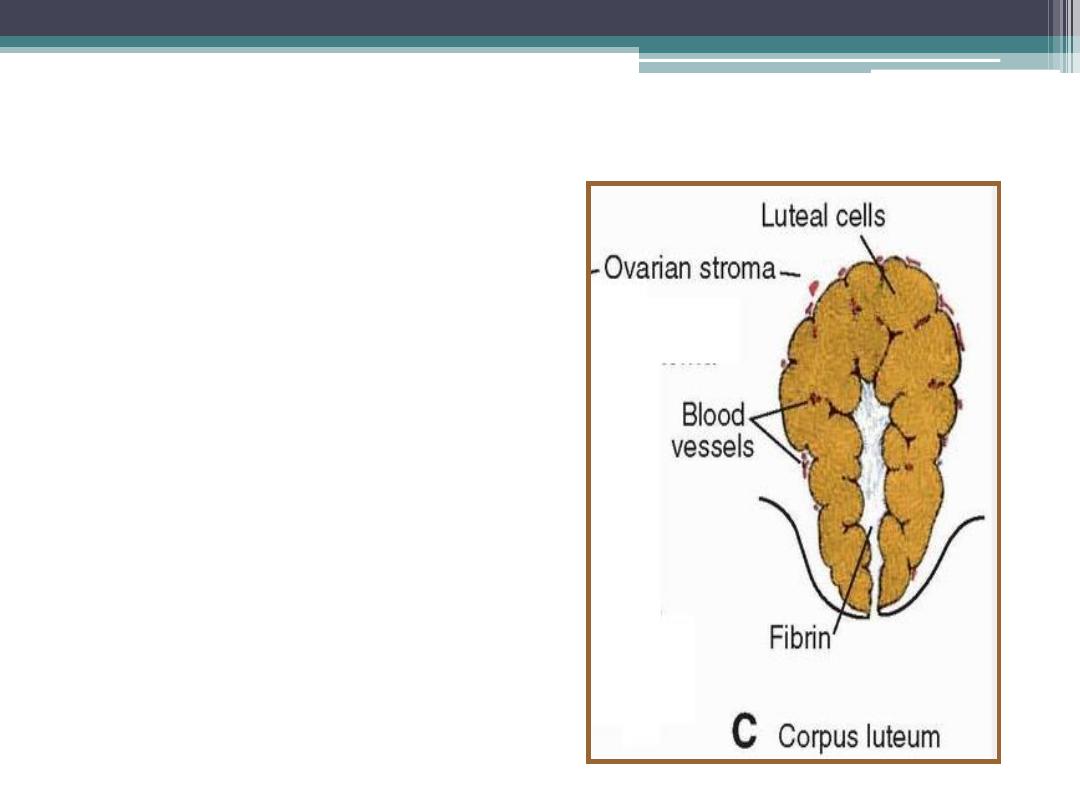
Corpus Luteum
•
After ovulation,
granulosa
cells
remaining in the wall of the
ruptured follicle, together with
cells from the theca interna
,
are vascularized by surrounding
vessels.
•
Under the influence of LH
,
these cells develop a yellowish
pigment and change into lutean
cells, which form the corpus
luteum and secrete the hormone
progesterone .
•
Progesterone, together with
estrogenic hormones, causes the
uterine mucosa to enter the
progestational or secretory stage
in preparation for implantation
of the embryo.

Fate of the corpus luteum
•
If fertilization does not
occur
, the corpus luteum
reaches maximum
development approximately 9
days after ovulation.
•
Subsequently, the corpus
luteum shrinks because of
degeneration of lutean cells
and forms a mass of fibrotic
scar tissue, the
corpus
albicans.
•
If the oocyte is fertilized
, the
corpus luteum continues to grow and
forms the
corpus luteum of
pregnancy
(corpus luteum
graviditatis).
•
By the end of the third month, this
structure may be one third to one
half of the total size of the ovary.
•
Yellowish luteal cells continue to
secrete progesterone until the end of
the fourth month; thereafter, they
regress slowly as secretion of
progesterone by the trophoblastic
component of the placenta becomes
adequate for maintenance of
pregnancy.
•
Removal of the corpus luteum of
pregnancy before the fourth month
usually leads to abortion
.

Three moments in the life of a woman are apparent in which atresia
takes place more rapidly
.
•
The largest decrease
occurs in the
20th week after the maximum
number of 7 million germ cells (per
ovary) is reached, thus still in the
fetal period.
•
Immediately following birth a
further,
short period of
accelerated decline happens
.
•
The third,
temporally longest
period, of increased decline
takes place during puberty.

Spermatogenesis
Is a complex series of changes by
which spermatogonia are
transferred into spermatozoa .
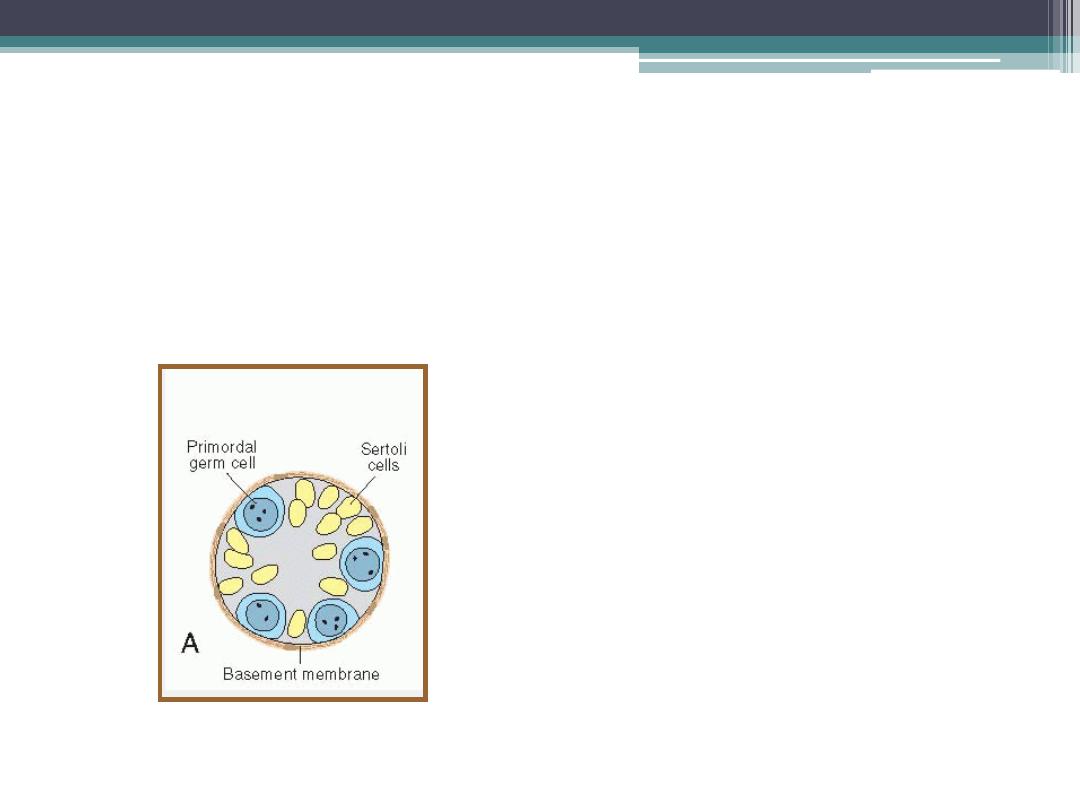
In the male infant
•
Germ cells
can be
recognized in the
sex
cords of the testis
as large,
pale cells surrounded by
supporting cells .
•
Supporting cells
, which are
derived from the surface
epithelium of the gland in the
same manner as follicular
cells, become
sustentacular
cells, or Sertoli cells
.

Shortly before puberty,
•
the sex cords acquire a lumen
and become the seminiferous
tubules.
•
Maturation of Sperm Begins at
Puberty
•
At about the same time,
primordial germ cells give rise
to spermatogonial stem cells.
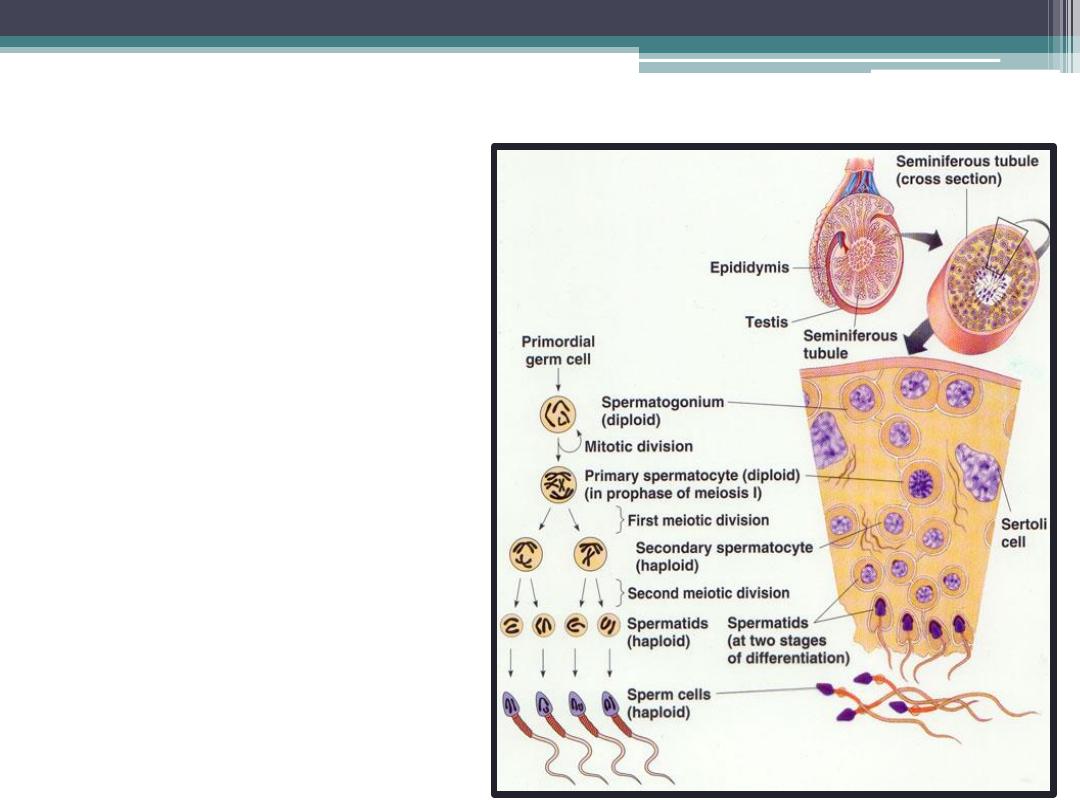
Spermatogenesis
can be divided into 3 phases :
•
a. spermatocytosis
•
b. meiosis
•
C. spermiogenesis
spermatocytosis
•
Spermatogonia proliferate by mitotic division to
replace themselves and to produce primary
spermatocytes

Meiosis
•
2 successive
divisions
•
Meiosis I produce
secondary
spermatocytes
•
Meiosis II produce
spermatids

The progeny of a single spermatogonium form a clone of
germ cells that maintain contact throughout differentiation
•
Spermatogonia and
spermatids remain
embedded in deep
recesses of Sertoli cells
throughout their
development.

The sertoli cells are supporting cells that
have several functions
.
•
They form the blood-testes
barrier: nutrients, and
circulating substances do
not directly reach the germ
cells
•
They form invaginations
surrounding the
spermatocytes, spermatids
and developing
spermatozoa and are
nutritive to them.
•
They also produce
antigen-binding proteins,
which are necessay for
spermiogenesis.

Spermiogenesis
•
The series of changes resulting in the transformation of spermatids into
spermatozoa include
(a) formation of the acrosome, which covers half of the nuclear surface and
contains enzymes to assist in penetration of the egg and its surrounding
layers during fertilization ;
(b) condensation of the nucleus;
(c) formation of neck, middle piece, and tail; and
(d) shedding of most of the cytoplasm.
•
In humans, the time required
for a spermatogonium to
develop into a mature
spermatozoon is
approximately 74 days, and
approximately 300 million
sperm cells are produced daily.
•
When fully formed,
spermatozoa enter the lumen
of seminiferous tubules. From
there, they are pushed toward
the epididymis by contractile
elements in the wall of the
seminiferous tubules.
•
Although initially only slightly
motile, spermatozoa obtain
full motility in the epididymis.

Clinical Correlates
Abnormal Gametes
•
A. Primordial follicle with two oocytes.
•
B. Trinucleated oocyte.
•
C. Various types of abnormal spermatozoa.
Thank you
Next Lecture:
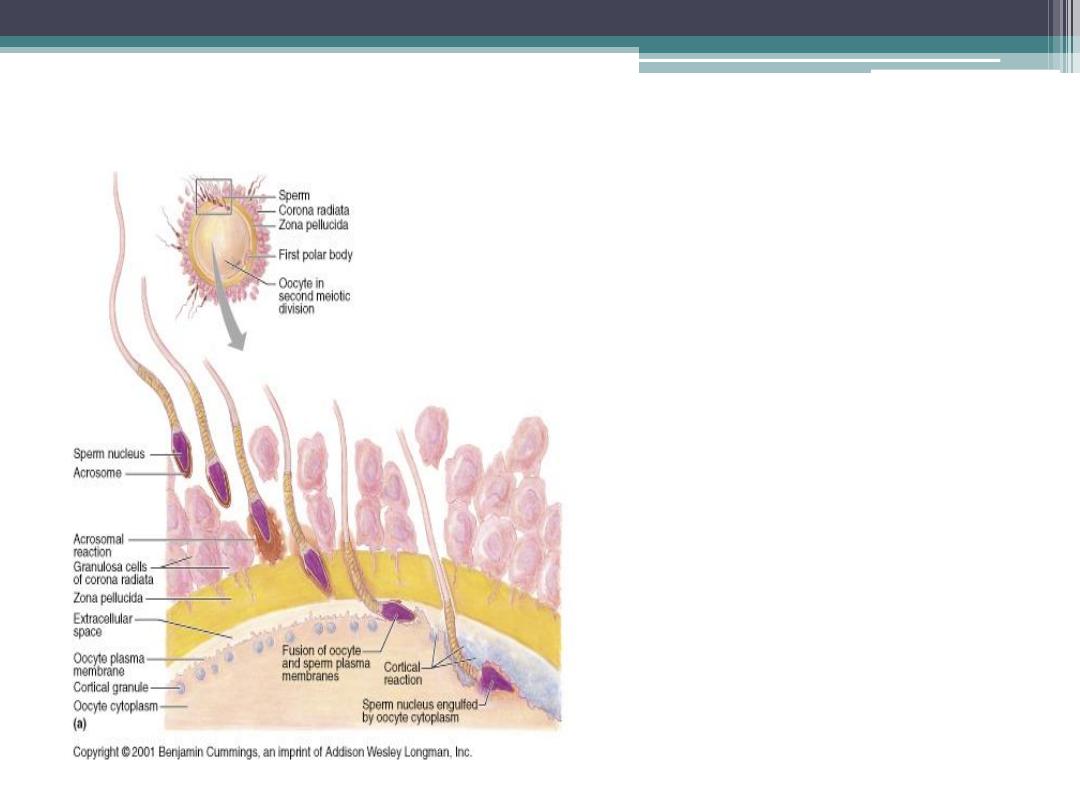
Fertilization

Key words of Fertilization
•
Capacitation
•
acrosome reaction
•
Fast block to polyspermy
•
Slow block to poly spermy
•
Contraceptive Methods
•
Infertility
•
In vitro Fertilization ( IVF )
•
Intracytoplasmic sperm injection
