Integumentary System
Prof. Dr. Malak A. Al-yawer
Learning Objectives
At the end of this lecture , the medical student will be able to
List the embryonic origin of the skin
State the embryonic origin of epidermis with its characteristic four
layers
State the embryonic origin of dermis in different parts of the body
State the embryonic origin of melanocytes
Define vernix caseosa
State the embryonic origin of different components of the hair
Define Lanugo Hair
Distinguish between the embryonic origin of different types of
glands ( eccrine, apocrine & sebaceous glands)
State the embryonic origin of mammary glands
State some clinical correlates
The skin has a dual origin
1. The epidermis develops from the surface
ectoderm
2. The dermis develops from the underlying
mesenchyme.
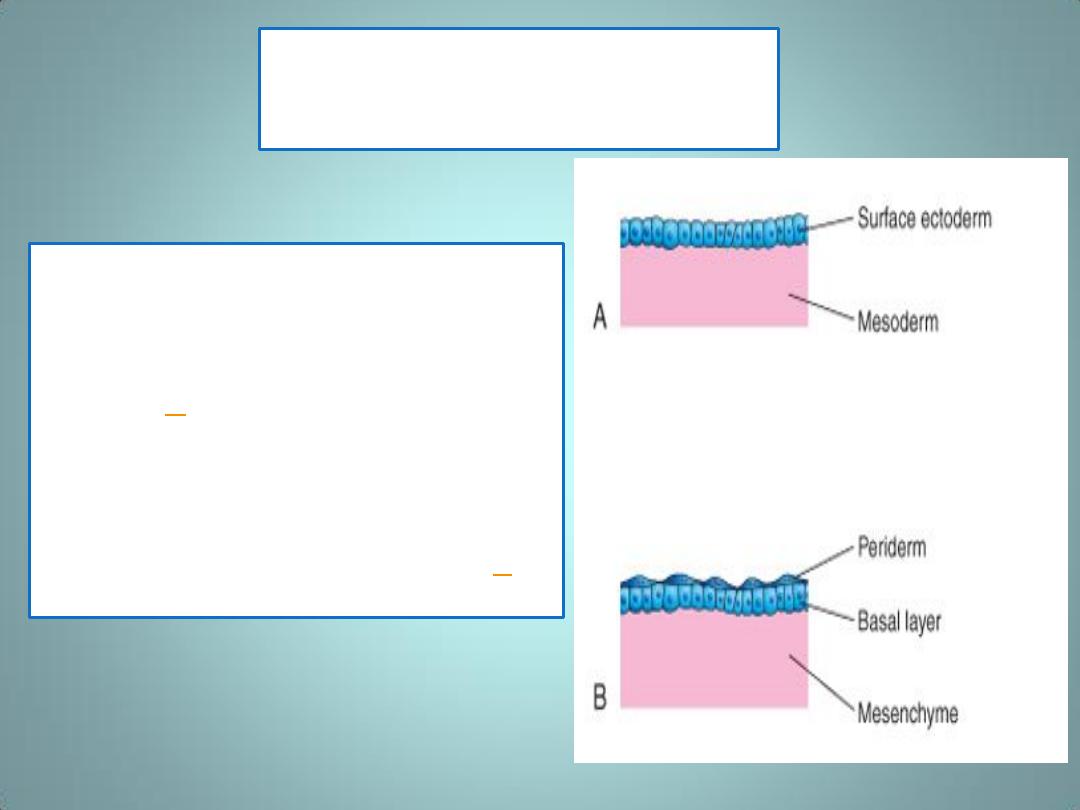
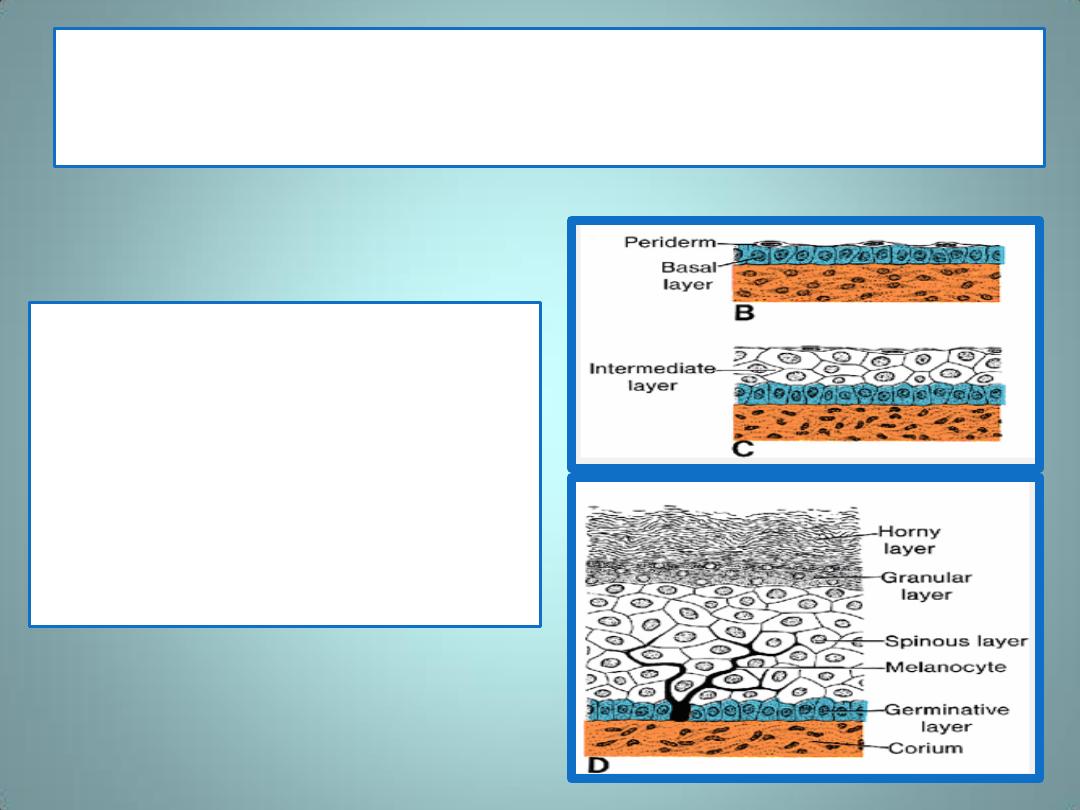
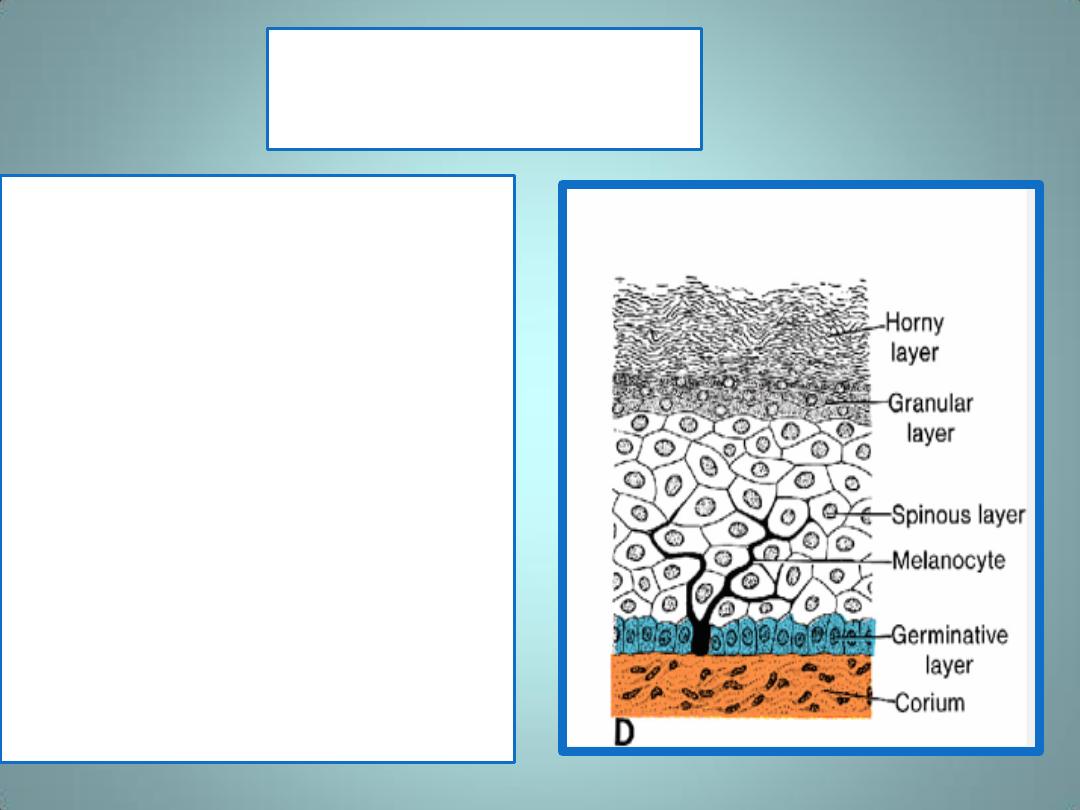
Epidermis
• Initially, the embryo is covered
by a single layer of ectodermal
cells (
A
)
• In the beginning of the 2
nd
month, this epithelium divides,
and a layer of flattened cells,
the periderm ,or epitrichium ,
is laid down on the surface (
B
(
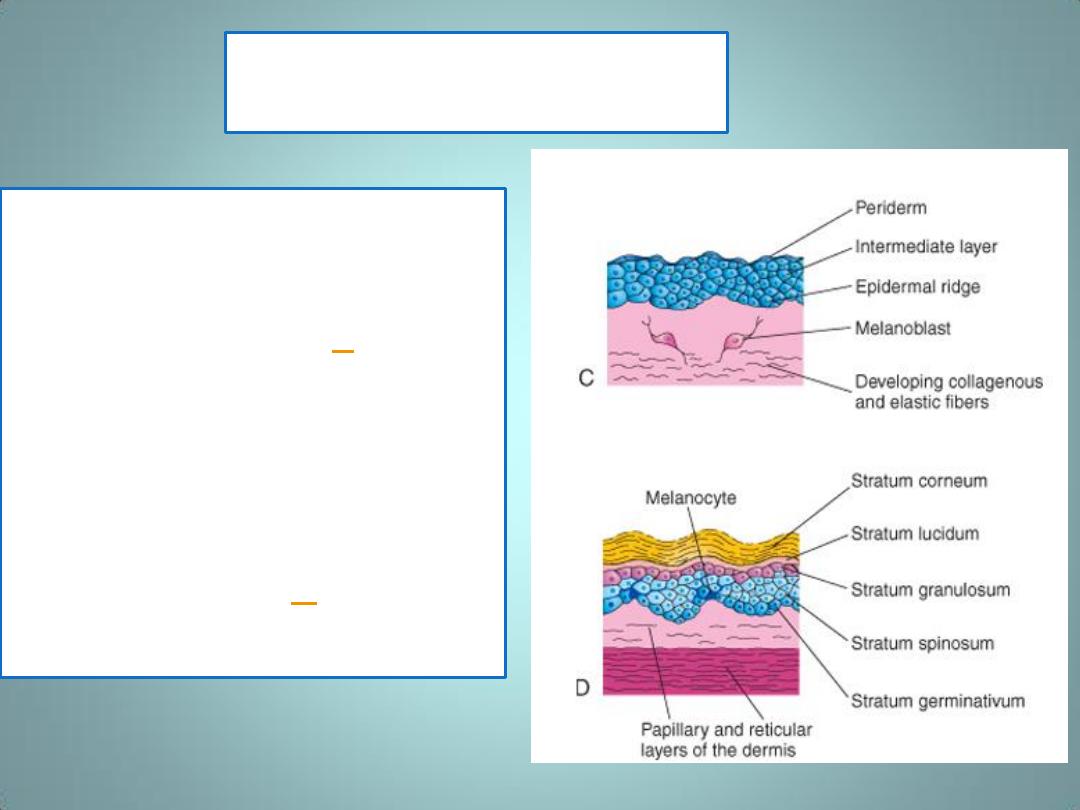
Epidermis
• With further proliferation
of cells in the basal layer,
a third, intermediate
zone is formed (
) .
• Finally, at the end of the
4
th
month, the epidermis
acquires its definitive
arrangement, and four
layers can be
distinguished)
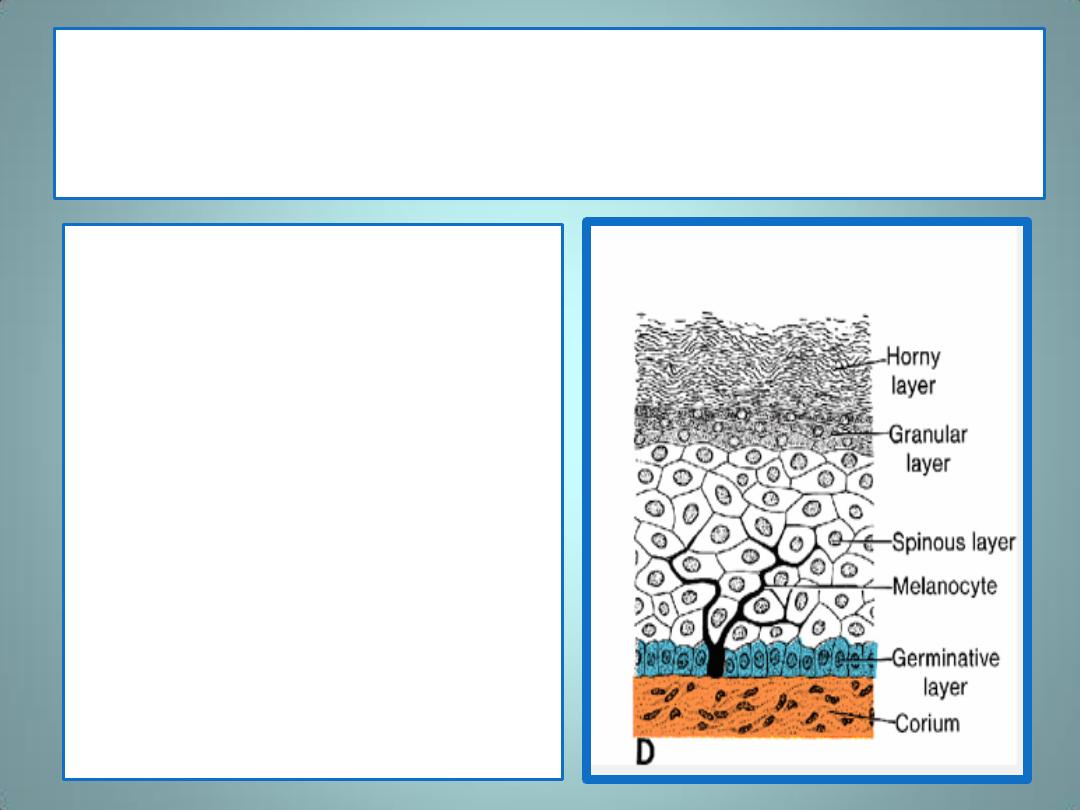
The basal layer (germinative layer)
• is responsible for
production of new cells.
• This layer later forms
ridges and hollows,
which are reflected on
the surface of the skin in
the fingerprint.
Cells of the periderm
• are usually cast off during
the 2
nd
part of
intrauterine life and can
be found in the amniotic
fluid.
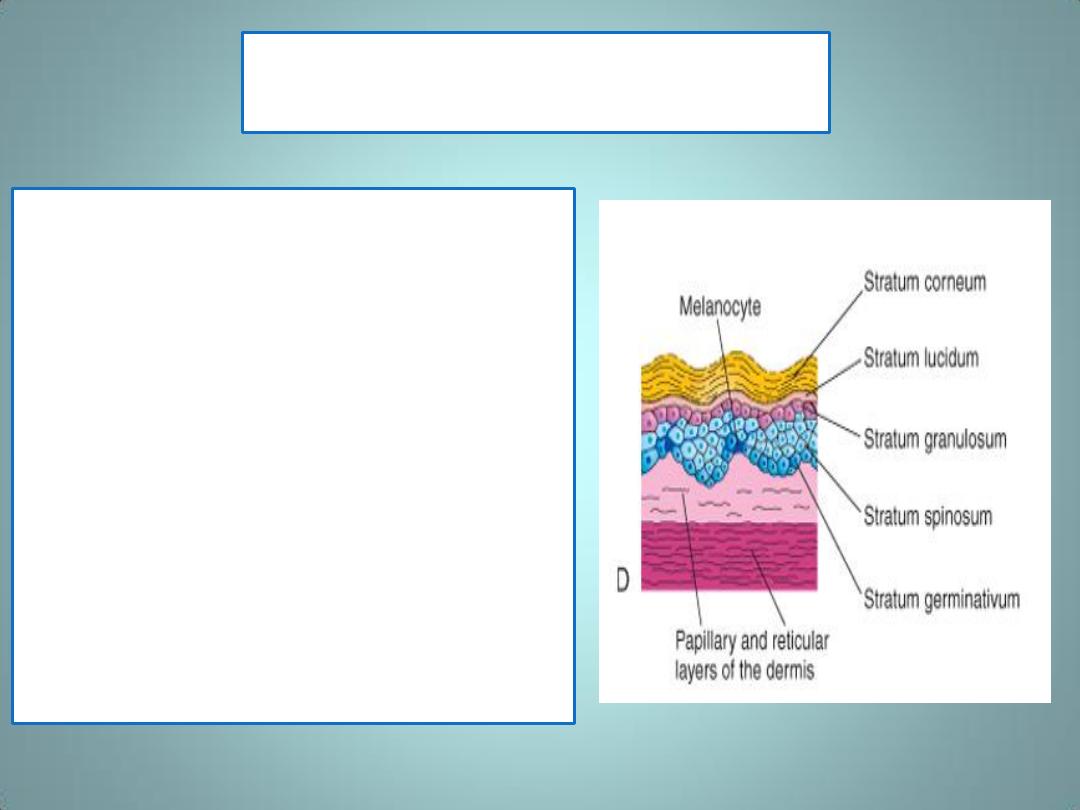
Melanocytes
• Late in the embryonic period, neural
crest cells migrate into the
mesenchyme of the developing
dermis and differentiate into
melanoblasts.
• Later these cells migrate to the
dermoepidermal junction and
differentiate into melanocytes
• The differentiation of melanoblasts
into melanocytes involves the
formation of pigment granules
• The melanocytes begin producing
melanin before birth and distribute
it to the epidermal cells.
Diseases of melanocyte function include the
various forms of albinism
• characterized by globally reduced or absence
of pigmentation in the skin, hair, and eyes.
• These cases are classified as different types of
oculocutaneous albinism (OCA)
• In most cases, abnormalities of melanin
synthesis or processing produce the
abnormalities.
Vitiligo
• results from a loss of melanocytes due to an
autoimmune disorder.
• There is patchy loss of pigment from affected
areas, including the skin and overlying hair
and the oral mucosa.
• Vitiligo is also associated with other
autoimmune diseases, particularly of the
thyroid.
Fingerprints
• The epidermal ridges that produce typical patterns
on the surface of the fingertips, palms of the hand,
and soles of the feet are genetically determined.
• They form the basis for many studies in medical
genetics and criminal investigations
)dermatoglyphics) .
• In children with chromosomal abnormalities, the
epidermal pattern on the hand and fingers is
sometimes used as a diagnostic tool.
Dermis
is derived from mesenchyme that has three
sources:
(a) lateral plate mesoderm supplying cells for
dermis in the limbs and body wall,
(b) paraxial mesoderm supplying cells for
dermis in the back, and
(c) neural crest cells supplying cells for dermis
in the face and neck .
Dermis
•
During the 3
rd
& 4
th
months,
the corium forms many
irregular papillary
structures, the dermal
papillae ,which project
upward into the epidermis.
•
Most of these papillae
contain a small capillary or
sensory nerve end organ.
•
The deeper layer of the
dermis, the subcorium ,
contains large amounts of
fatty tissue.
vernix caseosa
• At birth, the skin is covered by a whitish paste,
the vernix caseosa ,
• formed by secretions from sebaceous glands
and degenerated epidermal cells and hairs.
• It protects the skin against the macerating
action of amniotic fluid.
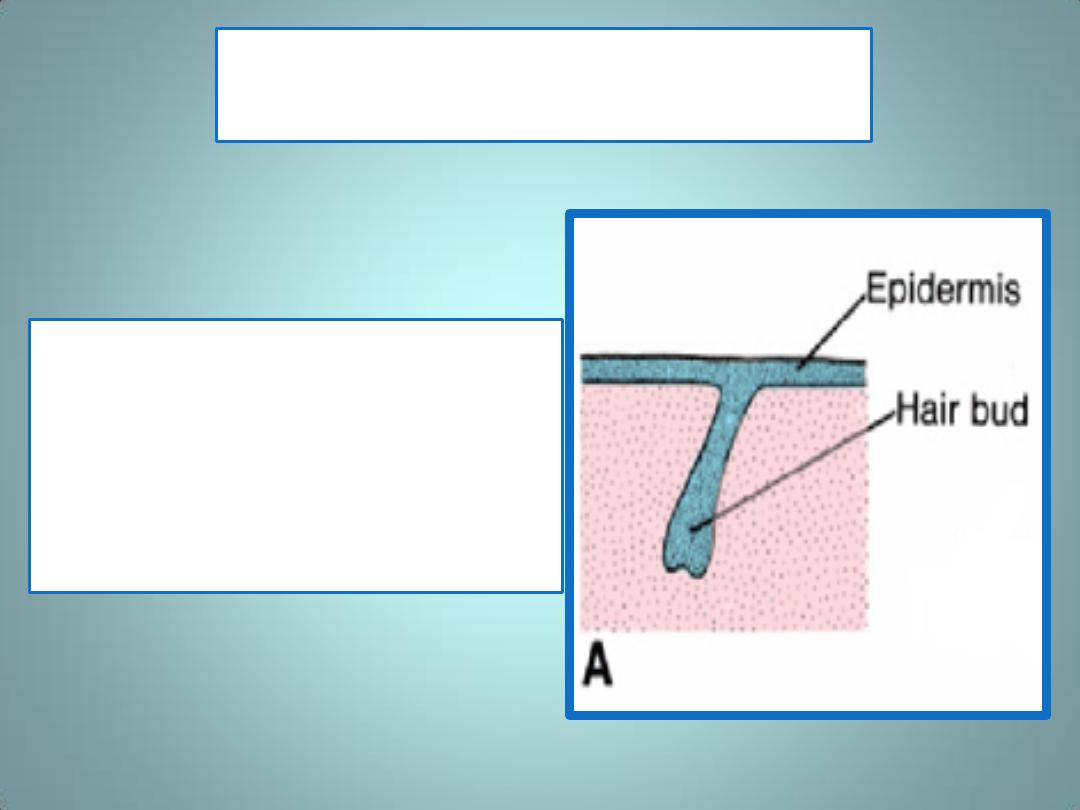
Hairs appear as
• solid epidermal
proliferations from the
germinative layer ( hair
bud) that penetrates the
underlying dermis.
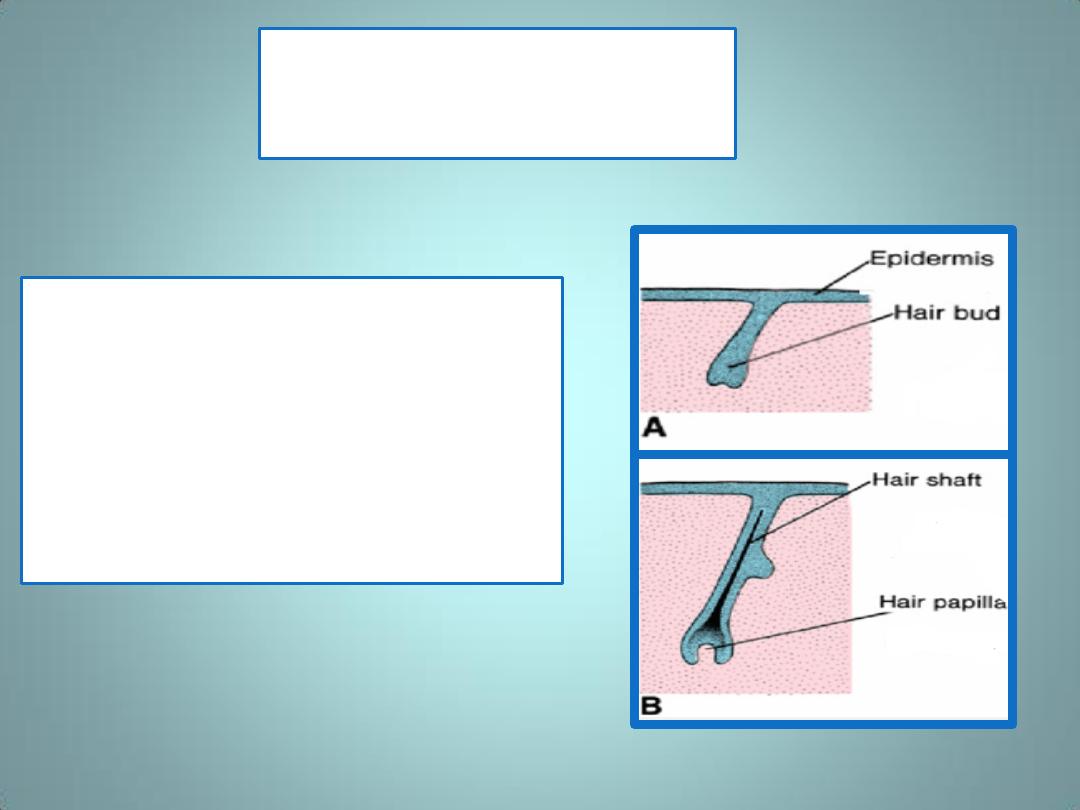
Hair papillae
• At their terminal ends, hair buds
invaginate. The invaginations,
the hair papillae ,are rapidly
filled with mesoderm in which
vessels and nerve endings
develop
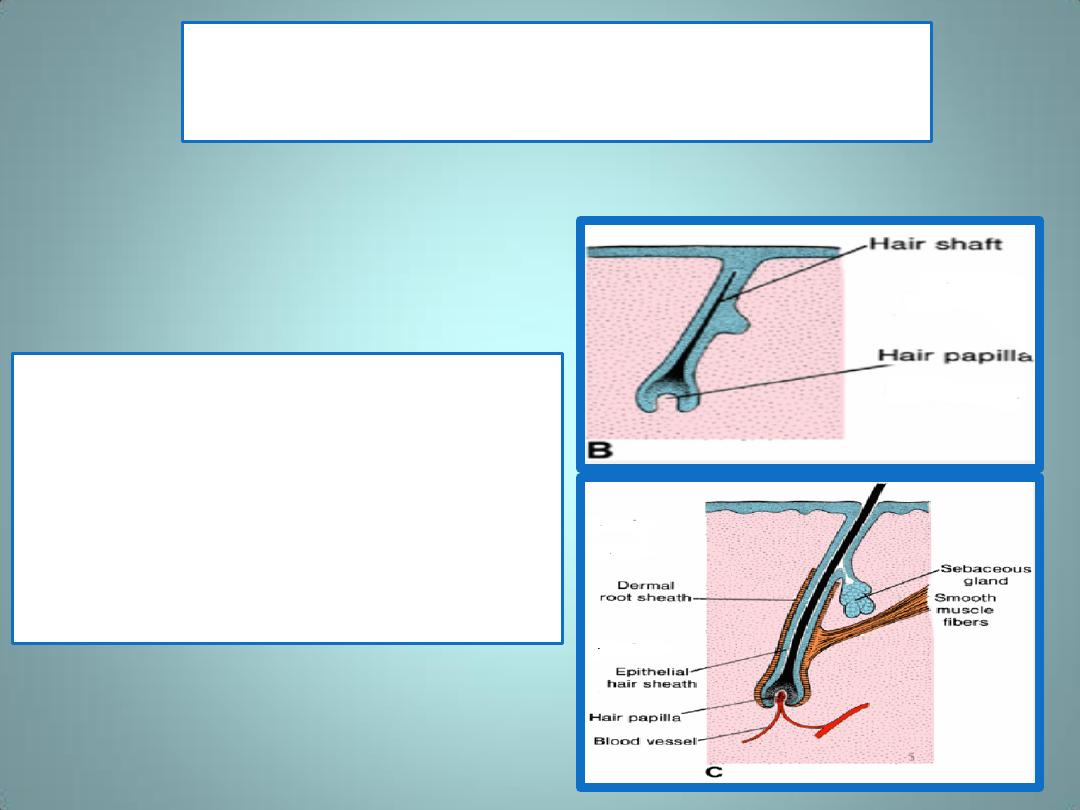
The hair shaft & the hair sheath
• Cells in the center of the hair
buds become spindle-shaped
and keratinized, forming the hair
shaft ,while peripheral cells
become cuboidal, giving rise to
the epithelial hair sheath
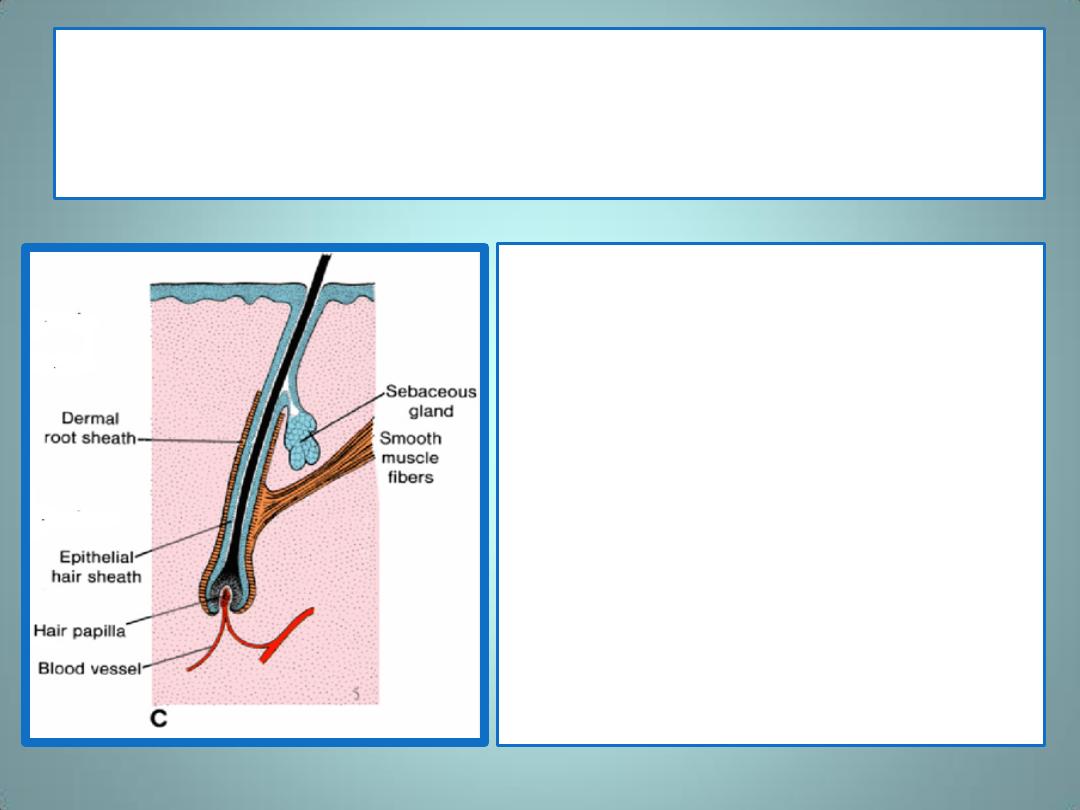
The dermal root sheath & arrector pili
muscle
• The dermal root sheath is
formed by the surrounding
mesenchyme.
• Arrector pili muscle,
1. derived from mesenchyme,
2. is usually attached to the
dermal root sheath.
• Continuous proliferation of
epithelial cells at the base of the
shaft pushes the hair upward
Lanugo hair
• by the end of the 3
rd
month, the first hairs
appear on the surface in the region of the
eyebrow and upper lip.
• The first hair that appears ,lanugo hair ,is
shed at about the time of birth and is later
replaced by coarser hairs arising from new
hair follicles.
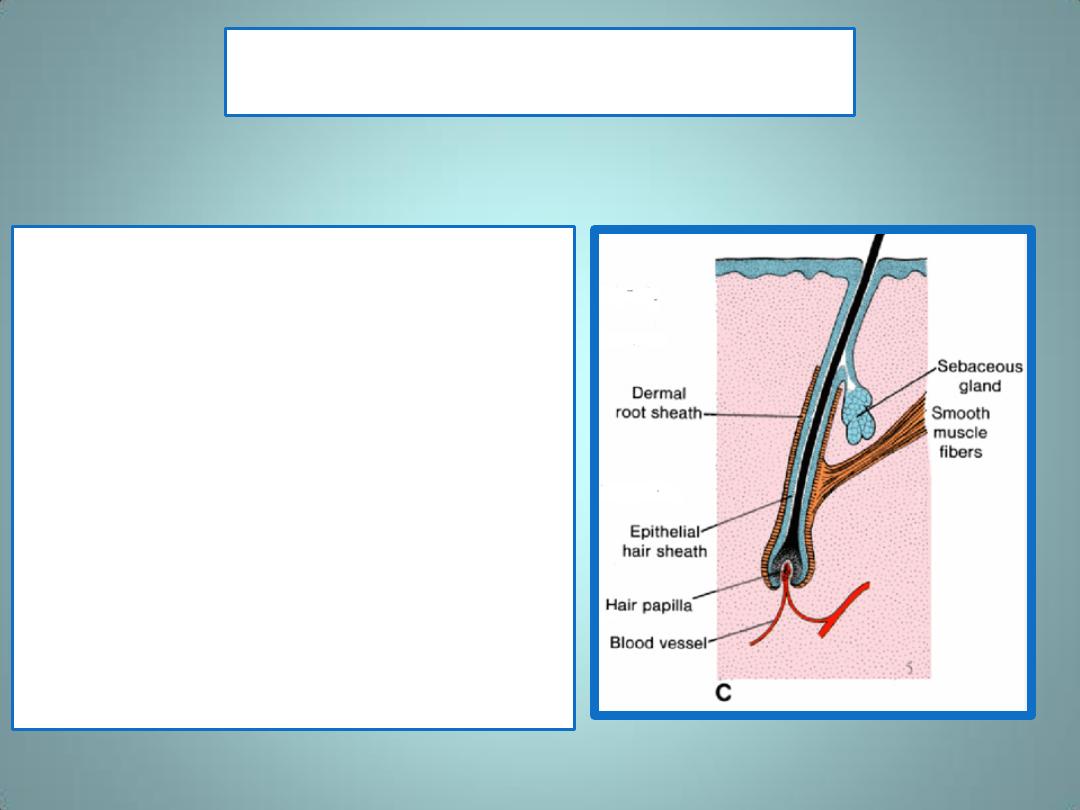
Sebaceous glands
• develop as buds from the sides of
developing epithelial root sheaths of
hair follicles
• The glandular buds grow into the
surrounding connective tissue and
branch to form the primordia of several
alveoli and their associated ducts.
• The central cells of the alveoli break
down, forming an oily secretion-sebum-
that is released into the hair follicle and
passes to the surface of the skin, where
it mixes with desquamated peridermal
cells to form vernix caseosa.
• Sebaceous glands independent of hair
follicles (e.g., in the glans penis and labia
minora) develop in a similar manner to
buds from the epidermis.
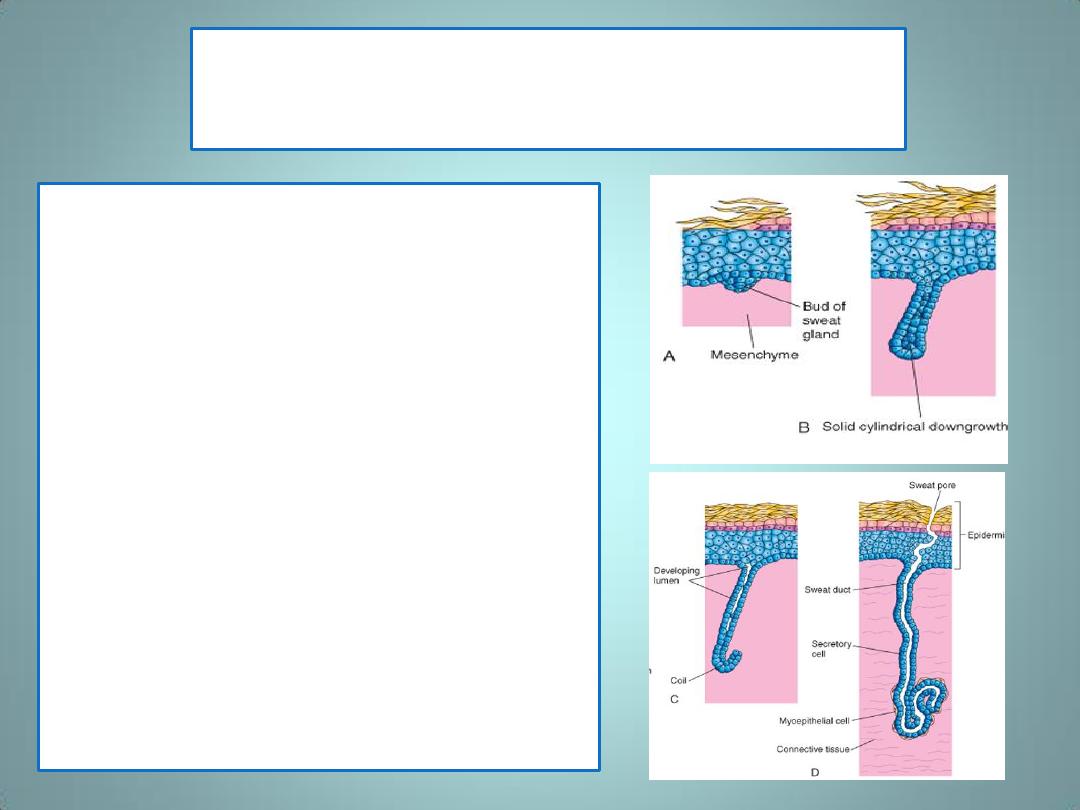
Eccrine sweat glands
• develop as epidermal
downgrowths (cellular
buds) into the underlying
mesenchyme
• As the buds elongate,
their ends coil to form the
primordium of the
secretory part of the gland
• The central cells of the
primordial ducts
degenerate, forming a
lumen.
apocrine sweat glands
• develop from downgrowths of the stratum
germinativum of the epidermis that give rise
to hair follicles.
• As a result, the ducts of these glands open,
not onto the skin surface as do eccrine sweat
glands, but into the upper part of hair follicles
superficial to the openings of the sebaceous
glands. They begin to secrete during puberty.
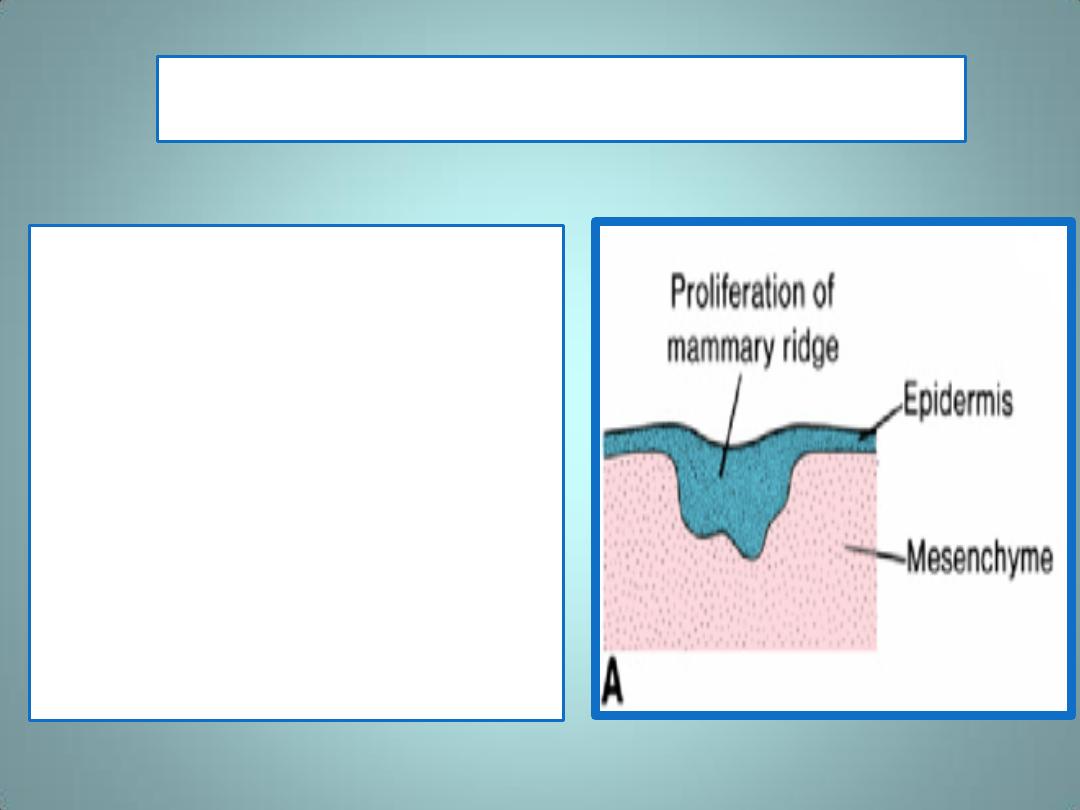
The mammary line or mammary ridge
• is the first indication of
mammary glands
• is a band-like thickening of the
epidermis
•
In a 7-week embryo, this line
extends on each side of the
body from the base of the
forelimb to the region of the
hindlimb
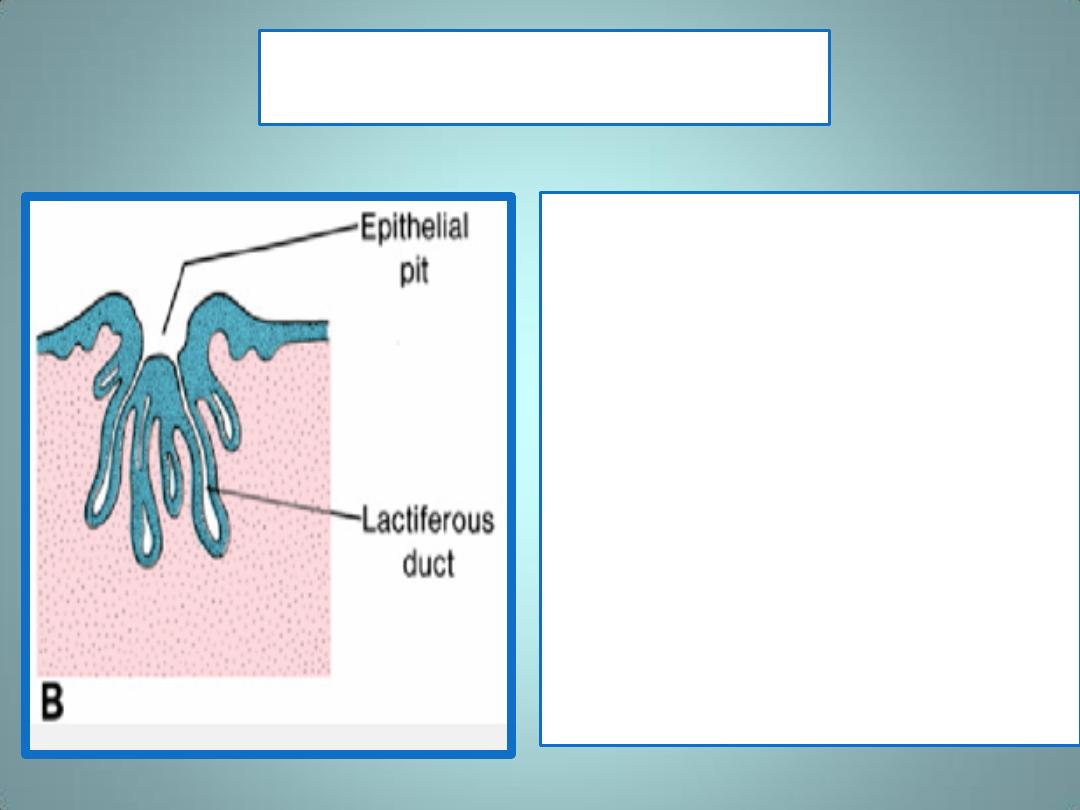
Sprouts & Buds
• Although the major part of the
mammary line disappears
shortly after it forms, a small
portion in the thoracic region
persists and penetrates the
underlying mesenchyme
• Here it forms 16 to 24 sprouts,
which in turn give rise to small,
solid buds.
• By the end of prenatal life,
1. the epithelial sprouts are
canalized and form the
lactiferous ducts
2. the buds form small ducts and
alveoli of the gland.

• Initially, the lactiferous
ducts open into a small
epithelial pit
• Shortly after birth, this
pit is transformed into
the nipple by
proliferation of the
underlying
mesenchyme
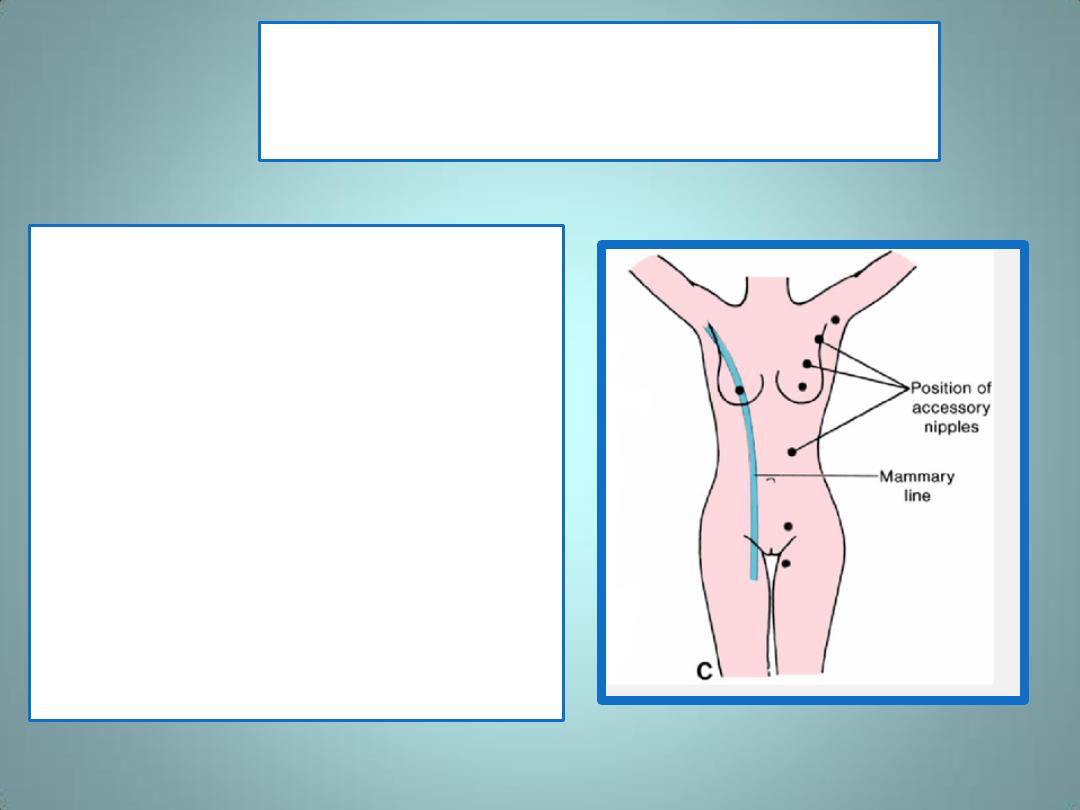
Polythelia
• is a condition where accessory
nipples have formed due to the
persistence of fragments of the
mammary line
.
• Accessory nipples may develop
anywhere
along the original
mammary line, but usually
appear in the axillary region.
Mammary Gland Abnormalities
• Polymastia occurs when
a remnant of the
mammary line develops
into a complete breast.
• Inverted nipple is a
condition in which the
lactiferous ducts open
into the original
epithelial pit that has
failed to evert.
Summary
• The epidermis of the skin and its associated
structures, hair, nails, and glands, are derived
from surface ectoderm.
• The dermis of the skin is derived from lateral
plate mesoderm, dermatomes of the somites and
neural crest cells
• Melanocytes are derived from neural crest cells
• Hairs develop from downgrowth of epidermal
cells into the underlying dermis.
• Sebaceous glands, sweat glands, and mammary
glands all develop from epidermal proliferations
