Histology
Lec.2 Dr. Faraid
Salivary glands:-
They are exocrine glands in the mouth that produce saliva, which
has digestive, lubricating & protective functions. There are 2 groups
of the salivary glands; the major salivary glands include the parotid,
submandibular(submaxillary) & sublingual glands; and the minor
salivary glands include labial, buccal, molar, lingual & palatine
glands. Two of the major glands (parotid & submandibular) are
located outside the oral cavity, while the minor salivary glands are
chiefly in the submucosa of the different parts of the wall of the oral
cavity. The major glands secrete only in response to certain stimuli;
mechanical, chemical or olfactory. The minor salivary glands seem to
secrete continuously.
The major salivary glands are surrounded by capsule of c.t. rich in
collagen fibers. The capsule is well developed in parotid, of average
thickness in submandibular & very thin in sublingual. From the
capsule septa (trabeculae) of c.t. penetrate the gland, dividing it into
lobes & lobules. Vessels & nerves enter the gland at the hilum &
gradually branches into the lobules. A rich vascular & nervous plexus
surrounds the secretory & ductal components of each lobule. The
alveoli (acini) are surrounded by basal lamina continuous with that
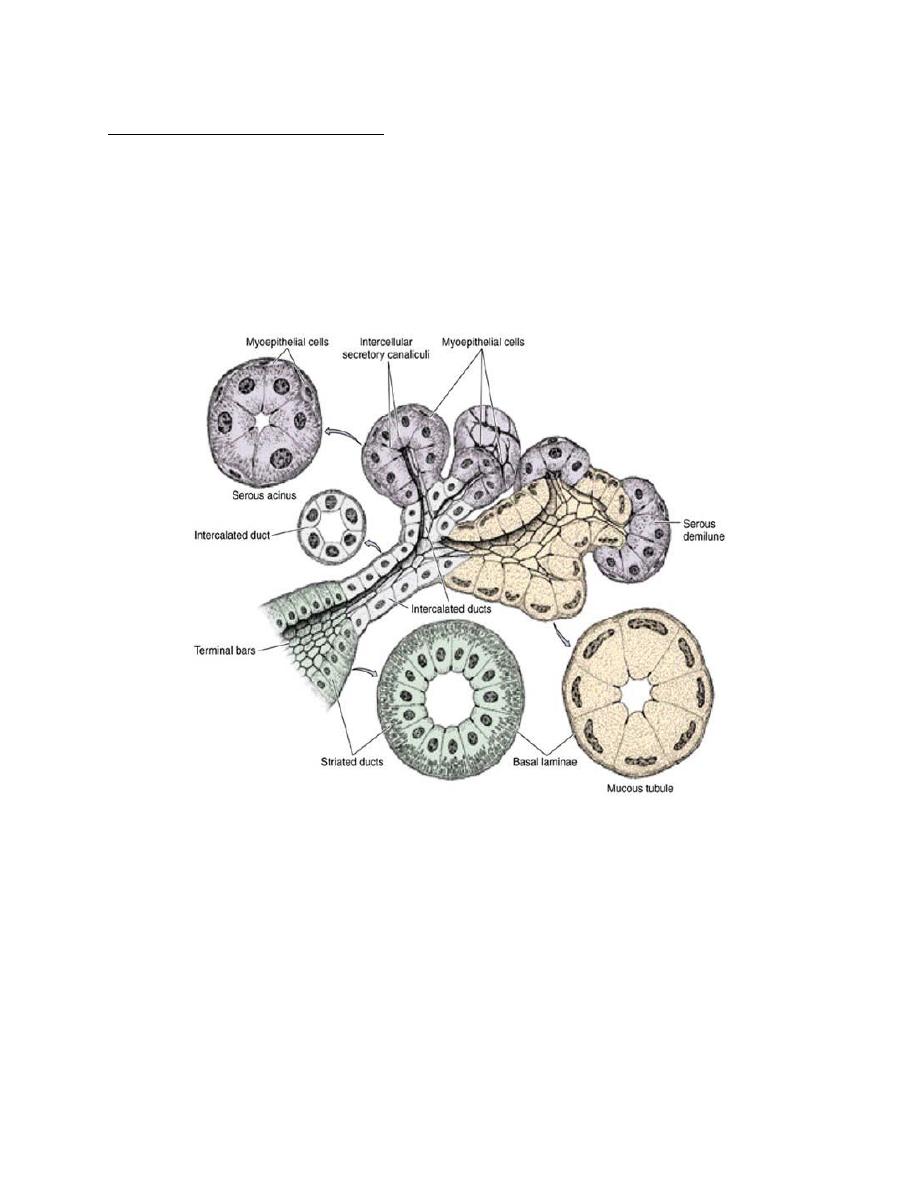
of the ducts. Myoepithelial cells lie between the basal lamina & the
epithelial cells of alveoli & also of the intercalated ducts.
Myoepithelial cells surrounding the secretory portion are well
developed & branched (called basket cells), whereas those
associated with intercalated ducts are spindle –shaped & lie parallel
to the length of the duct.
Serous alveoli (acini):- consist of pyramid-shaped cells arranged around
a small lumen. The serous cells exhibit characteristics of polarized
protein-secreting cells. Their apical cytoplasm is crowded with
secretory granules. Serous cells have spherical nucleus & the
surrounding basal cytoplasm contains numerous profiles of rough
endoplasmic reticulum (stains deeply basophilic). Adjacent secretory
cells are joined together by junctional complexes. These junctional
complexes may be located well below the apical margin, in which case
intercellular secretory canaliculi are formed. These canaliculi increase
the area available for the discharge of serous secretions. The luminal
(apical) surface of the serous cells bears many short microvilli. Deep to
the junctional complexes, the lateral margins show folds that
interdigitate with those of adjoining cells→cell boundaries are
indistinct.
Mucous alveoli(acini):- are larger than the serous acini. Mucous cells
are usually cuboidal to the columnar in shape. Their nuclei are flattened
& pressed against the base of the cell. They exhibit the characteristics
of mucus-secreting cells, containing glycoprotein (mucins) important
for the moistening & lubricating functions of saliva. They are pale in
staining. The mucous acini have larger & more apparent lumen.
Mucous cells are most often organized as tubules. The cell boundaries
are quite distinct.
Mixed alveoli(acini):- are typically mucous alveoli surrounded or
capped by one or more groups of the serous cells, forming a crescent-
shaped serous demilune.
The parotid gland is purely serous gland. The submandibular gland is
a mixed type, being composed predominantly of serous acini. The
sublingual gland is also a mixed gland but predominantly mucous, most
of the secretory acini are mucous & mixed.
Salivary gland ducts:-
the secretory acini empty into the intercalated
ducts, lined by simple cuboidal epithelium. Several of these short ducts
join to form striated ducts, lined by simple columnar epithelium,
characterized by basal striations (radial striations) that extend from the
bases of the cells to the level of the nuclei. When viewed in the
electron microscope, the striations are seen to consist of infoldings of
the basal plasma membrane with numerous elongated mitochondria
that are aligned parallel to the infolded membranes; this structure is
characteristic of ion-transporting cells. Intercalated & striated ducts are
also called intralobular ducts because of their location within the
lobule.
The striated ducts of each lobule converge & drain into ducts located
in the c.t. septae separating the lobules, where they become
interlobular or excretory ducts. These drain into the main duct of each
gland, which empties into the oral cavity.
Saliva: -
is a hypotonic solution produced at a rate of about
1litre/day. It lubricates, moistens & cleanses the oral cavity by means of
its water or glycoprotein
(mucus) content. It acts as a solvent for
substances that stimulate the taste buds. It initiates digestion of
carbohydrates by the action of salivary amylase (produced mainly by
the serous acini) and digestion of triglycerides by lipase. It controls
bacterial flora by the action of lysozyme, lactoferrin & IgA, as well as by
its cleansing action. The salivary enzyme lysozyme secreted by the
serous cells that form the demilunes in submandibular and sublingual
glands, hydrolyzes the cell walls of certain bacteria & inhibits their
growth in the oral cavity. Lactoferrin secreted by acinar & intercalated
duct cells, binds iron, a nutrient necessary for bacterial growth &
inhibits their growth. The immunoglobulins in saliva, primarily the IgA
produced by the plasma cells in the c.t. of the glands, forms a complex
with a secretory component synthesized by the serous acinar,
intercalated & striated duct cells. The IgA-secretory piece complex
released into the saliva is resistant to enzymatic digestion & constitutes
an immunologic defense mechanism against pathogens in the oral
cavity.
Human saliva consists of secretions from the parotid glands 25%, the
submandibular gland 70% & the sublingual 5%.
Parasympathetic stimulation (e.g. smell & taste of food) provokes a
copious watery secretion with little organic content.
Sympathetic stimulation (e.g. fear& stress) produces small amounts of
viscous saliva, rich in organic material.
Pharynx:-
It is the posterior continuation of the oral cavity where the
respiratory & alimentary passages fuse & cross. It extends from the
level of the base of the skull to the level of the cricoid cartilage where it
becomes continuous with the oesophagus. It is simple transport tube
through which ingested food is transmitted without undergoing
significant metabolic change. It has 3 parts:-
1. Upper part - Nasopharynx
2. Middle part- Oropharynx.
3. Lower part - Laryngeal pharynx
The wall of the pharynx is composed of the following layers :-
(starting from inside)
1. Mucous membrane
epithelium
Lamina propria
It is lined in its upper part by pseudostratified columnar ciliated
epithelium with goblet cells (respiratory epithelium). The lower two
parts are lined by stratified squamous non-keratinized epithelium
continuous with that of the oesophagus.
The lamina propria consists of c.t. containing many lymphocytes. In
its upper part there are definite lymph nodules (pharyngeal tonsil), in
the middle part there are also lymph nodules (palatine tonsils).
Numerous mucous & mixed glands are present.
2. The muscular layer:- consists of striated muscles (constrictors of the
pharynx).
3. The outer fibrous layer (adventitia):- consists of dense c.t.
continuous with surrounding structures.
General structure of digestive tract:-
The digestive tract from the oesophagus to the anus has certain
common structural characteristics. Its wall is composed of 4 principal
layers, (starting from inside):-
1.The mucosa(mucous membrane):- this consists of :-
a)The lining epithelium:- the type of epithelium varies in the relation to
the function of the part of the digestive tract. It could be protective,
absorptive or secretory. The main functions of the epithelial lining of
the digestive tract are:-
1) To provide a selectively permeable barrier between the contents of
the tract & the tissues of the body,
2) To facilitate the transport & digestion of the food,
3) To promote the absorption of the products of the digestion,
4) To produce hormones that affect the activity of the digestive system.
Cells in this layer produce mucus for lubrication & protection.
b) Lamina propria:- consists of loose c.t. rich in blood & lymph vessels
& smooth m., may also contain lymph nodules & glands(gastric glands
& intestinal glands). In the lamina propria, there is a zone rich in
macrophages & lymphoid cells located just below the epithelium. Some
of these lymphoid cells actively produce antibodies. These antibodies
are mainly IgA & are bound to a secretory protein produced by the
epithelial cells of the intestinal lining & secreted into the intestinal
lumen. This complex protects against viral & bacterial invasion (form
the first line of immunological defense against bacterial & viral
invasion).
c) Muscularis mucosae:- consists of smooth m., usually arranged in 2
layers, an inner circular & an outer longitudinal. It separates the
mucosa from the submucosa. The muscularis mucosae promotes the
movement of the mucosa independent of other movements of the
digestive tract, increasing its contact with the food.
2. The submucosa:- consists of dense c.t. with many blood & lymph
vessels. A plexus of nerve fibers with some ganglion cells are present in
the submucosa. This is called Meissner's plexus (submucous nerve
plexus). It may also contain glands (oesophageal & Brunner's gland) &
lymphoid tissue.
3.The muscularis externa:- this usually consists of an inner circular & an
outer longitudinal layer of smooth m. A plexus of nerve fibers
associated with numerous ganglion cells are situated chiefly between
the circular & longitudinal layers. This plexus is called Auerbach's plexus
or Myenteric nerve plexus. The contractions of the muscularis
generated and coordinated by nerve plexuses, propel and mix the food
in the digestive tract. These plexuses are composed mainly of nerve cell
aggregates
(multipolar
visceral
neurons)
that
form
small
parasympathetic ganglia.
At the sphincters the circular layer is greatly increased. Localized
thickenings of muscle in the bowel wall act as valves & are called
sphincters. Sphincter contraction occludes the lumen & thus prevents
the passage of the luminal contents.
The pyloric sphincter:- is the most important sphincter & is located at
the junction between the stomach & duodenum. By contracting, it
delays stomach emptying, hereby permitting continued food break
down in the stomach.
The oesophagogastric sphincter(cardiac sphincter):- is located
between the lower oesophagus & proximal stomach. It prevents reflux
of gastric contents into oesophagus.
The ileocaecal valve:- is situated between the terminal ileum &
caecum. It delays discharge of ileal contents into the caecum.
The internal anal sphincter:- is located at the upper end of the anal
canal. It retains fecal waste material in the rectum until controlled
defecation.
The pharyngoesophageal sphincter:- is a physiological sphincter (no
significant increase in the number of circular muscle fibers).
4.The serosa or adventitia:- consists of loose c.t. rich in blood & lymph
vessels, covered in those portions of the tube that are suspended by
mesentery with simple squamous epithelium (mesothelium). In other
parts, the adventitia consists only of loose c.t
.
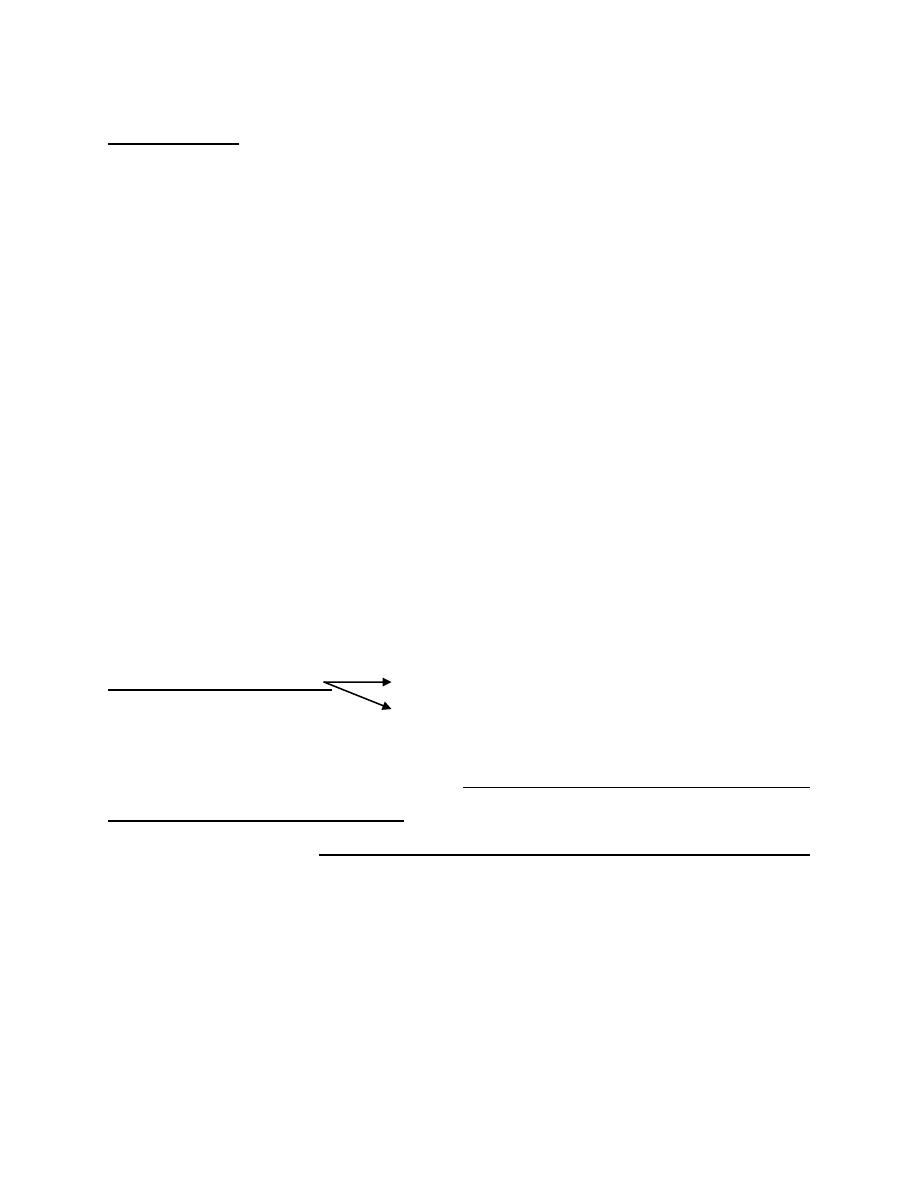
Figure1. The structure of submandibular (submaxillary) gland. The secretory portions are composed
of pyramidal serous (light blue) and mucous (light yellow) cells. Serous cells are typical protein-
secreting cells, with rounded nuclei, accumulation of rough endoplasmic reticulum in the basal third,
and an apex filled with protein-rich secretory granules. The nuclei of mucous cells, flattened with
condensed chromatin, are located near the bases of the cells. The short intercalated ducts are lined
with cuboidal epithelium. The striated ducts are composed of columnar cells with characteristics of
ion-transporting cells, such as basal membrane invaginations and mitochondrial accumulation.
Myoepithelial cells are shown in the serous secretory endpieces.
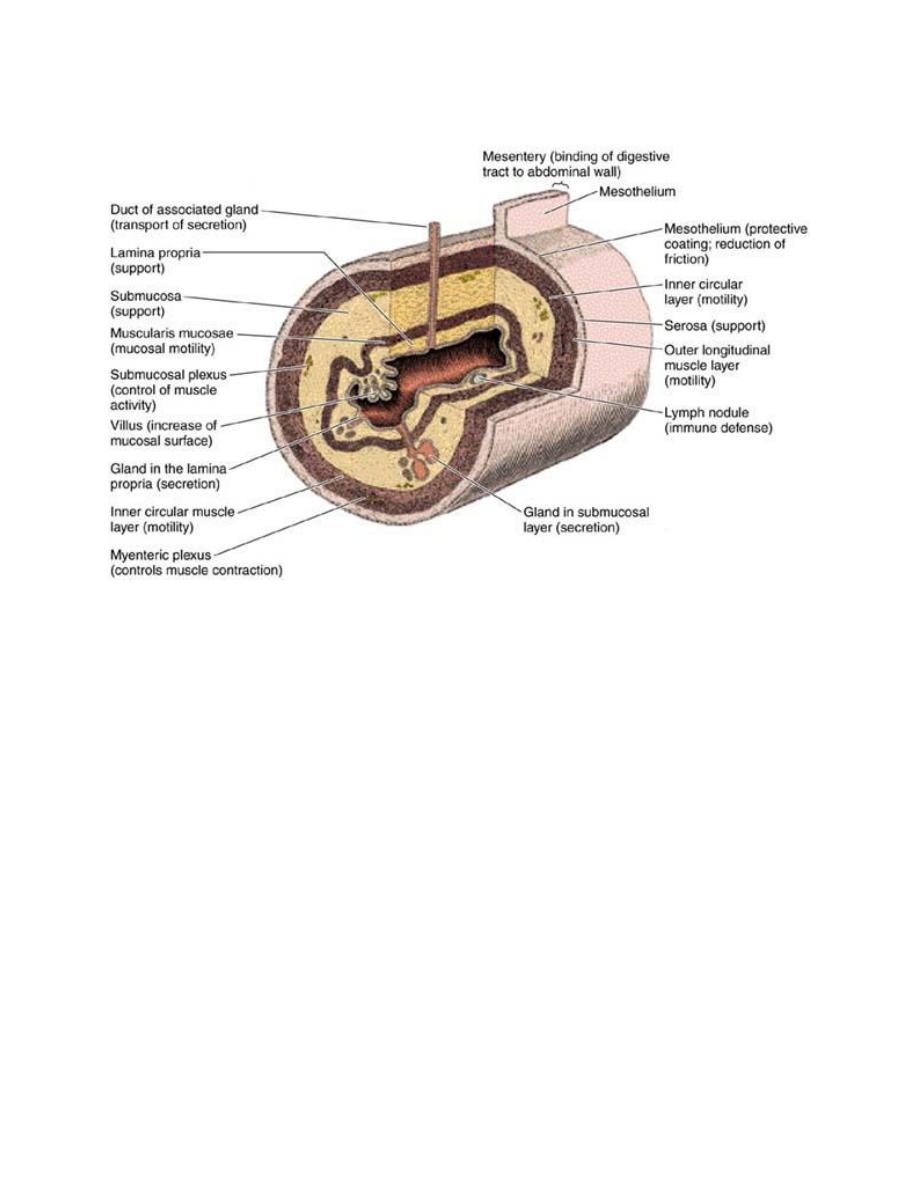
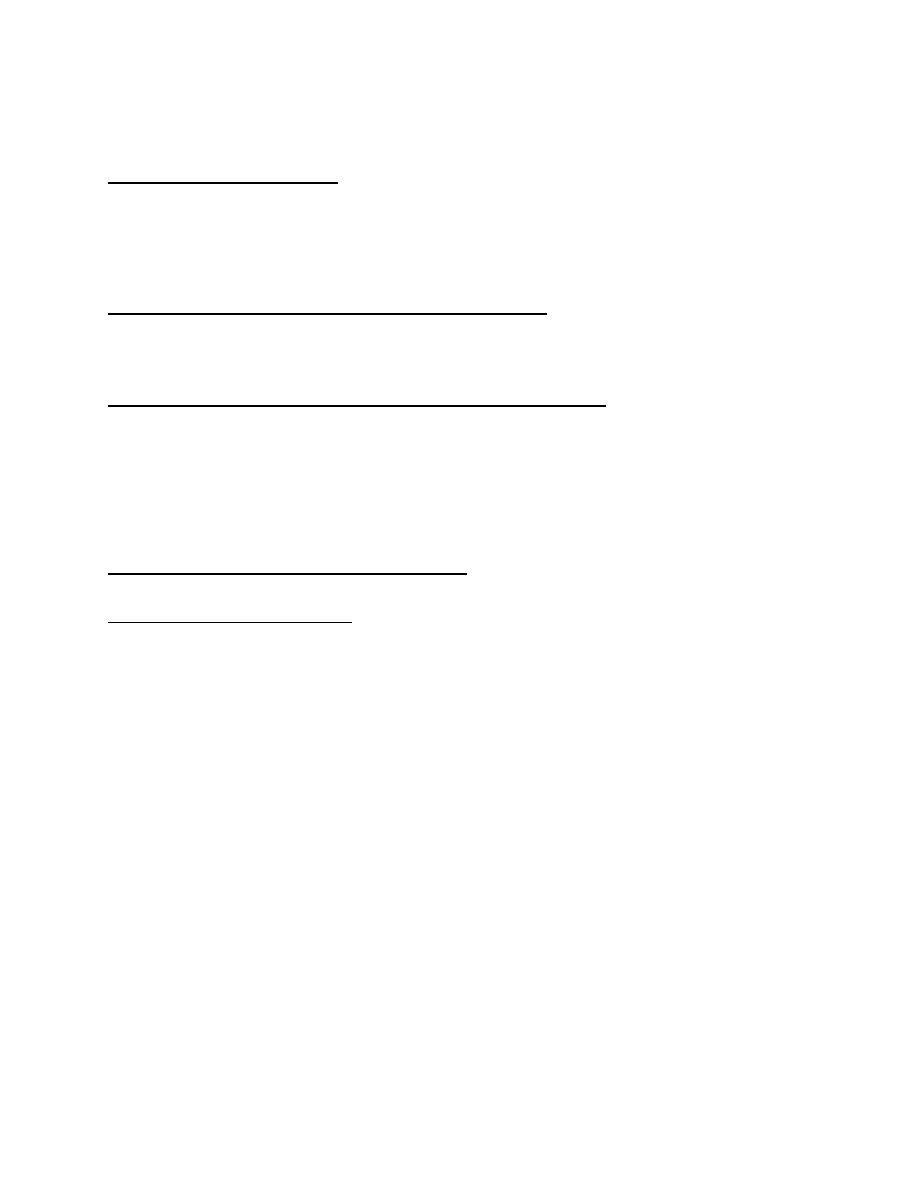
Figure 2. Schematic structure of a portion of the digestive tract with
various components and their functions. (Redrawn and reproduced, with
permission, from Bevelander G: Outline of Histology, 7
th
ed. Mosby , 1971.)
