Histology
Lec.3 Dr. Faraid
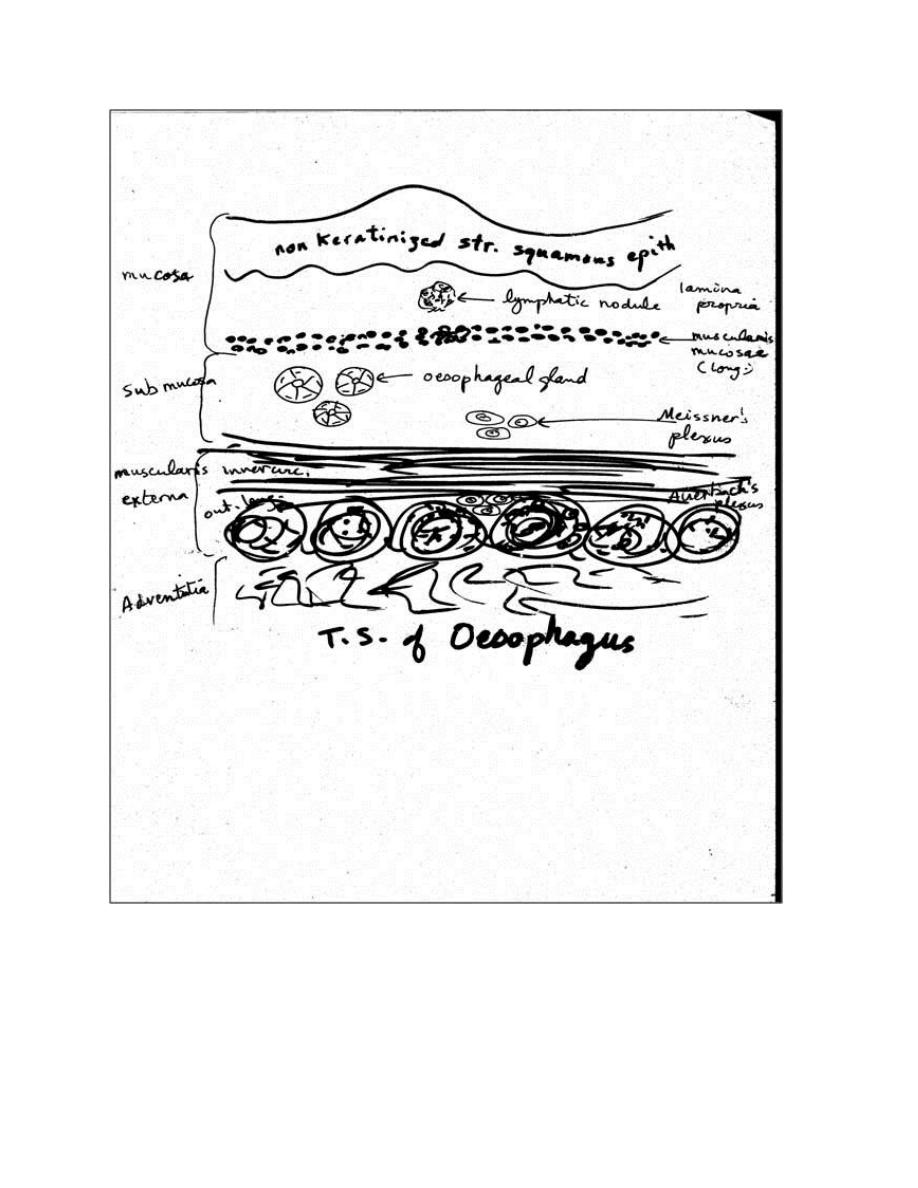
The oesophagus:-
It is a straight muscular tube that transports food from the pharynx
to the stomach. It is about 25cm long. Its wall consists of the usual 4
layers:-
1. The mucosa:-
a) It is lined by a protective, non-keratinized stratified squamous
epithelium with mitotic figures in its basal layer, indicating a constant
shedding & renewal of the cells.
b) Lamina propria :- consists of loose c.t. , in the lamina propria of the
region near the stomach are groups of glands , the oesophageal cardiac
glands ,that secrete mucus.
c) Muscularis mucosae:- it is thick & consists of longitudinal smooth
muscle fibers. In the lower part of the oesophagus, the muscularis
mucosae may be formed of inner circular & outer longitudinal muscles
fibers.
2. The submucosa:- contains the oesophageal glands. These are
branched tubulo-alveolar glands which are mucous in nature, their
ducts open on the epithelial surface.
3. The muscularis externa:- consists of 2 layers, of which the outer is
mainly longitudinal & the inner mainly circular. In the upper part of the
oesophagus, the muscle fibers are striated, in the middle are mixed
(striated & smooth) & in the lower part all the muscle fibers are
smooth. In the region of the cardiac sphincter the circular muscle is
greatly thickened. Between the 2 muscle layers there is Auerbach's
plexus.
4. The adventitia:- consists of loose c.t. continuous with that of the
surrounding structures. There is a serous layer only on the abdominal
part of the oesophagus.
Oesophago-gastric junction:-
At this junction the stratified squamous epithelium of the
oesophagus ends abruptly to be replaced by the simple columnar
epithelium of the stomach. The oesophageal glands stop & the gastric
glands appear in the lamina propria. Lymph nodules are frequent
around the junction. The oesophago-gastric junction is an important
site of the pathologic abnormality. Lower oesophagus is an important
site of common diseases, particularly ulceration, stricture & cancer.
The epithelium of the oesophagus is protected from exposure to the
gastric acid by:-
1. The anatomical arrangement of the oesophago-gastric junction.
2. The cardiac sphincter which prevents reflux of the gastric contents
into the lower oesophagus.
Reflux of acid gastric secretions may occur into the lower esophagus
causing inflammation & pain. Under the constant irritating effect of
reflux of acidic gastric secretions, the epithelium in the lower
esophagus changes to a gastric type.
Stratified squamous non-keratinized epithelium→ simple columnar
The columnar epith
prone to
ulceration & inflammation
and predispose to the development of one type of oesophageal cancer.
Healing of such ulcers can lead to scarring of the lower end of the
oesophagus & thereby narrowing of its lumen (i.e oesophageal
stricture) → difficulty of swallowing.
Stomach:-
It is both exocrine & endocrine organ that digests food & secretes
hormones. It is a dilated segment of the digestive tract.
The main functions of the stomach:-
1. Continuation of digestion of carbohydrates initiated in the oral
cavity (mouth) by salivary amylase which starts the digestion of
carbohydrates & this process will continue in the stomach.
2. Secretion of acids (HCl) together with the muscular activity of the
muscles of the stomach will transform the digested food into a
viscous mass known as chyme.
3. The stomach initiates the digestion of proteins by the enzyme
pepsin so the stomach secretes pepsinogen which is converted into
pepsin which initiates the digestion of proteins.
4. The stomach secretes or produces gastric lipase. Gastric lipase
starts the digestion of triglycerides together with the help of lingual
lipase (Von Ebner's gland).
For descriptive purpose or anatomically the stomach can be
divided into 4 divisions:-
1. Cardia
2. Fundus
3. Body
4. Pylorus or pyloric region
Because the fundus & body are identical in microscopic structure,
only 3 histologic regions are recognized. In empty, contracted
stomach, the mucosa & submucosa form numerous longitudinal
folds known as rugae. When the stomach is filld with food, these
folds flatten out.
The wall of the stomach consists of the usual 4 layers of digestive
tract:-
1. The mucosa:-
consists of :
A) Surface epithelium (simple columnar epithelium):- their cells
secrete mucin (mucus) & they are known as surface mucous cells.
The mucus forms a thick layer that protects these cells from the
effects of the strong acid secreted by the stomach. The surface
epithelium invaginates to various extents into the lamina propria,
forming gastric pits (lined by the same epithelium). Emptying into
the gastric pits are branched tubular glands (cardiac, fundic &
pyloric) characteristic of each region of the stomach. The surface
mucous cells are thought to produce blood group substances. Tight
junctions present around surface & pits cells also form part of the
barrier to acid. Stress & other psychosomatic factor; ingested
substances such as aspirin or ethanol & some microorganisms (e.g.
Helicobacter pylori) can disrupt this epithelial layer & lead to
ulceration.
B) The lamina propria:- is occupied by the gastric glands. These are
branched tubular glands, separated by little amount of c.t. They
open into the bases of the gastric pits.
Types of gastric glands:-
1) The cardiac glands:- are present in the cardiac region. They are
simple or branched tubular glands, lined by mucus secreting
columnar cells similar to the mucous neck cells of the gastric gland
proper. They secrete mucus & lysozyme.
2) Fundic glands (gastric gland proper):- are present in the lamina
propria of the fundus & body of the stomach. They are branched,
tubular glands, 3 to 7 of which open into the bottom of each gastric
pit. The glands are composed of the following cells:-
a) Mucous neck cells:- are located between the parietal cells in
the neck of the gland. The cells are large irregular in shape, with
clear cytoplasm & the nucleus is flattened at the base of the cell.
They secrete mucus which protects the stomach wall from the
action of the HCl & proteolytic enzymes.
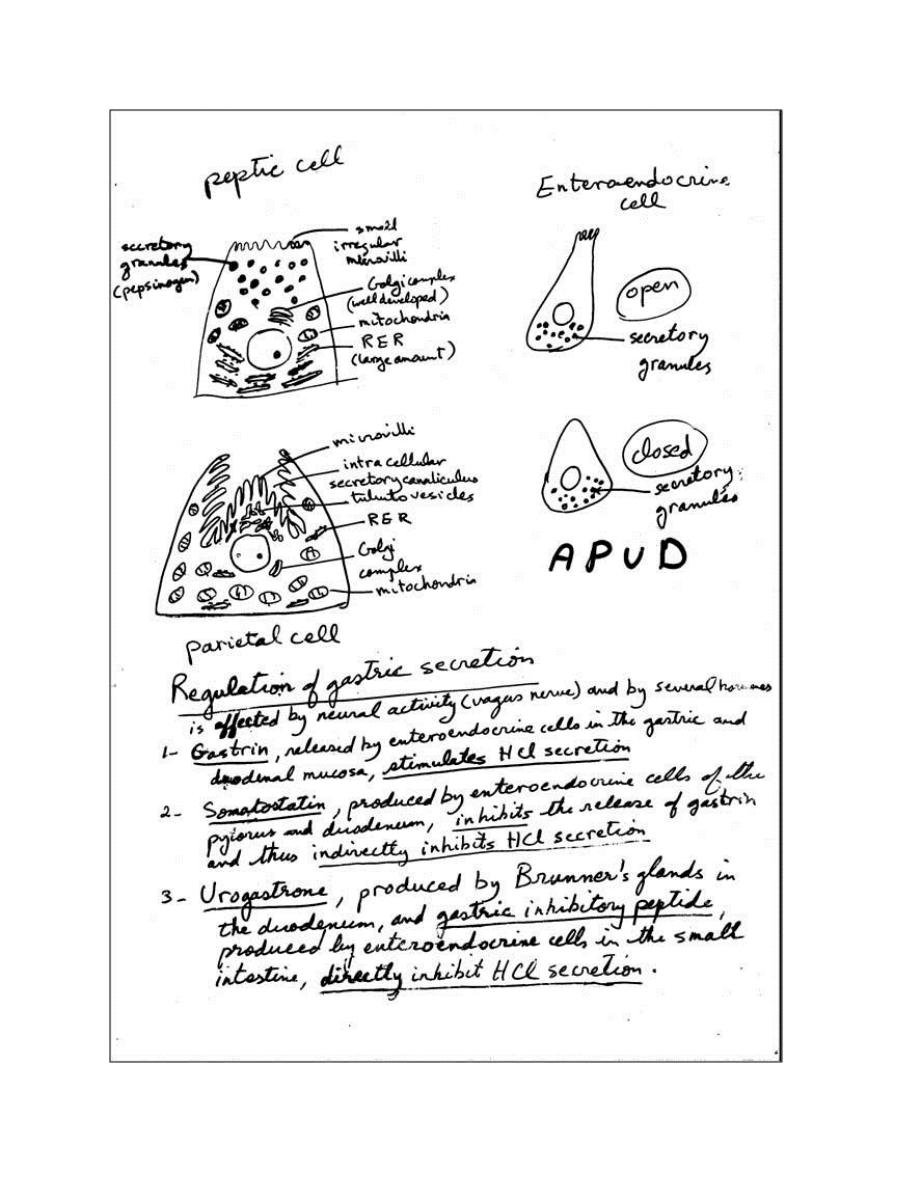
b) Peptic (chief or zymogenic) cells:- they predominate in the
lower part of the gland & have all the characteristics of the
protein synthesizing & exporting cells. Their basophilia is due to
the abundant RER (rough endoplasmic reticulum). The granules in
their cytoplasm contain the inactive enzyme pepsinogen, the
precursor of pepsin. In human, chief cells also produce the
enzymes, lipase & rennin. The E.M shows the presence of small
irregular microvilli on their free surfaces, a well developed Golgi
apparatus (complex) located in the supranuclear region, large
amount of basally located RER & many apical secretory granules.
c) Parietal (oxyntic) cells:- are present mainly in the upper half of
the gland. They are large rounded or pyramidal cells with one
centrally placed spherical nucleus & intensely eosinophilic
cytoplasm. The most striking features of the active secreting cell
seen in the electron microscope are an abundance of
mitochondria (eosinophilic) & a deep circular invagination of the
apical plasma membrane, forming the intracellular secretory
canaliculus lined with abundant microvilli. In the resting cell, a
number of tubulovesicular structures can be seen in the apical
region of the cell. At this stage, the cell has few microvilli. When
stimulated to produce HCl, tubulovesicles fuse with the cell
membrane to form the canaliculus & more microvilli, suggesting
that tubulovesicles are involved in secretion. The parietal cells
secrete the HCl & gastric intrinsic factor (a glycoprotein that binds
to vitamin B12 & facilitate its absorption by the intestine). Lack of
the intrinsic factor can lead to vitamin B12 deficiency →pernicious
anaemia. In cases of atrophic gastritis, both parietal and peptic
cells are much less numerous, and the gastric juice has little or no
acid or pepsin activity, and no intrinsic factor → pernicious
anaemia.
Parietal cells have abundant carbonic anhydrase, which is thought
to play a vital role in generating H
+
ions for the production of HCl.
d) Enteroendocrine cells:- were formerly called argentaffin &
enterochromaffin cells, owing to their affinity for silver &
chromium stains. Most of the cells have the characteristics of the
so-called APUD cells (amine precursor uptake & decarboxylation),
which are wide spread in the body (found in the epithelium of
GIT, respiratory tract, in the pancreas & thyroid gland). Their
cytoplasm either contains polypeptide hormones or the biogenic
amines epinephrine, norepinephrine, or 5-hydroxytryptamine
(serotonin). These cells have characteristics of diffuse
neuroendocrine system (DNES).These cells can be identified &
localized by immunocytochemical methods or other cytochemical
techniques for specific amines. The enteroendocrine cells are
small pyramidal cells found near the bases of gastric glands. They
are characterized by the presence of abundant dense secretory
granules, always located at the base of the cell between the
nucleus & basal lamina. This suggests that they are endocrine cells
that liberate their secretion into the blood vessels in the lamina
propria rather than into lumen of the gland. Some of these cells
are known as paracrine because they produce hormones that
diffuse into the surrounding extracellular fluid to regulate the
function of neighboring cells without passing through the vascular
system.
Polypeptide-secreting cells of the digestive tract fall into 2
classes:-
1) The open type:- in which the apex of the cell presents microvilli
& contacts the lumen of the organ.
2) The closed type:- in which the cellular apex is covered by other
epithelial cells.
In the fundus of the stomach, serotonin is one of the principal
secretory products. Tumors arising from these cells are called
carcinoids, are responsible for the clinical symptoms caused by
overproduction of the serotonin.
e) Stem cells (undifferentiated cells):- are found in the neck
region of all gastric glands (cardiac, fundic & pyloric). These cells
have a high rate of mitosis; some of them move upward to
replace the pit & surface mucous cells, which have a turnover
time of 4-7 days. Other daughter cells migrate more deeply into
the glands & differentiate into the different types of cells of the
glands. These cells are replaced much more slowly than are
surface mucous cells.
3) Pyloric glands:-
are present in the pyloric region of the stomach
& are similar to the cardiac glands. However, the pits are longer &
the glands are shorter & coiled, opposite to that of cardiac glands.
The pyloric glands secrete mucus as well as appreciable amounts of
the enzyme lysozyme. These glands also have enteroendocrine cells
as follows:-
1. G cells release gastrin which stimulates the secretion of the acid
by the parietal cells.
1. D cells secrete somatostatin, which inhibits the release of some
other hormones, including gastrin.
C) The muscularis mucosae:- consists of smooth m. arranged as an
inner circular & an outer longitudinal layer, in some parts there is a
third outer layer of circular fibers. Strands of muscle extend from the
inner layer into the lamina propria between the glands; their
contraction helps to empty the glands.
2. Submucosa:-
is composed of dense c.t. containing blood & lymph
vessels & Meissner's plexus.
3. Muscularis externa:-
consists of 3 illdefined layers of smooth m.,
an inner oblique, a middle circular & an outer longitudinal. At the
pylorus, the middle layer is greatly thickened to form the pyloric
sphincter. Auerbach's plexus is found between the muscles.
4. Serosa:-
derived from the visceral peritoneum consists of a thin
layer of loose c.t. covered by mesothelium (simple squamous
epithelium).
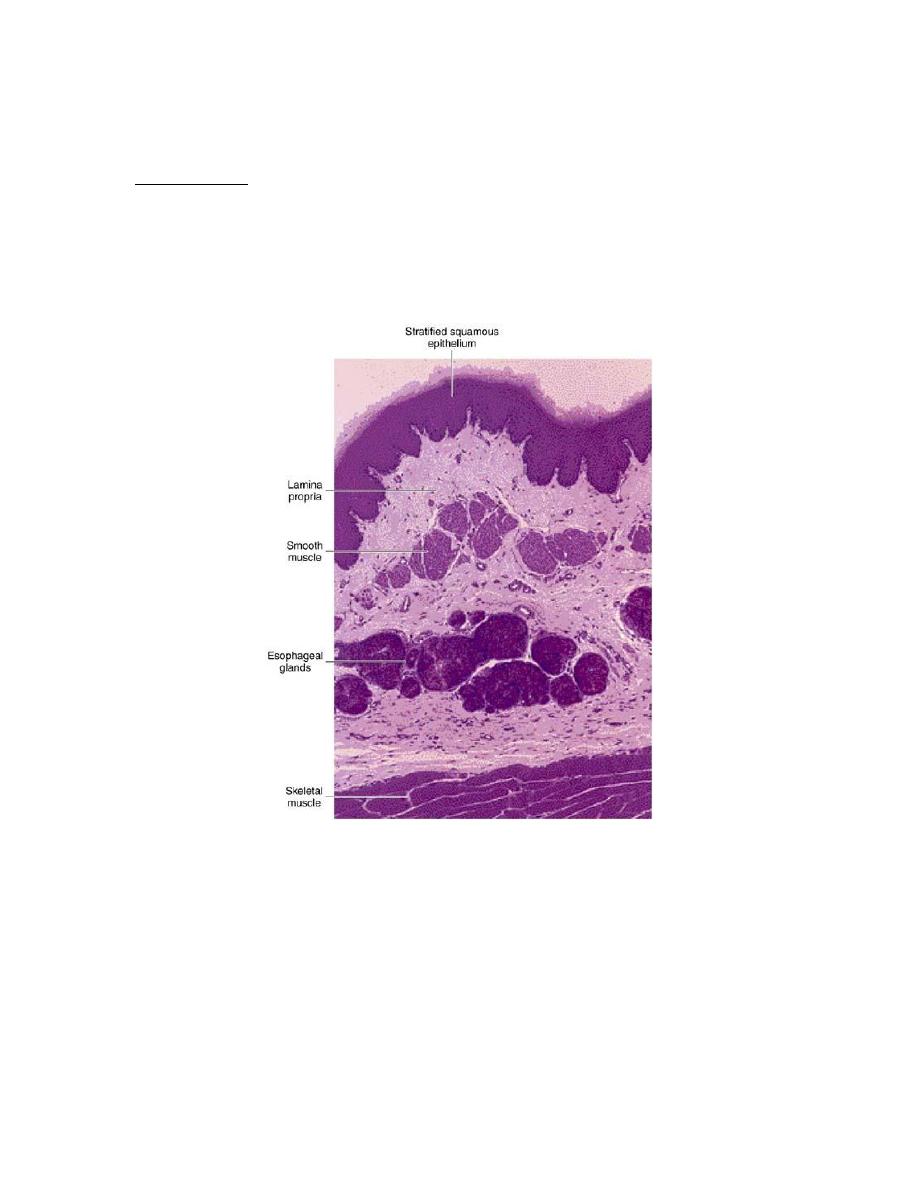
Photomicrograph of a section of the upper region of the esophagus.
Mucous oesophageal glands are in the submucosa; striated skeletal
muscle is in the muscularis. PAS and PT stain. Low magnification.

Regions of the stomach and their histological structure
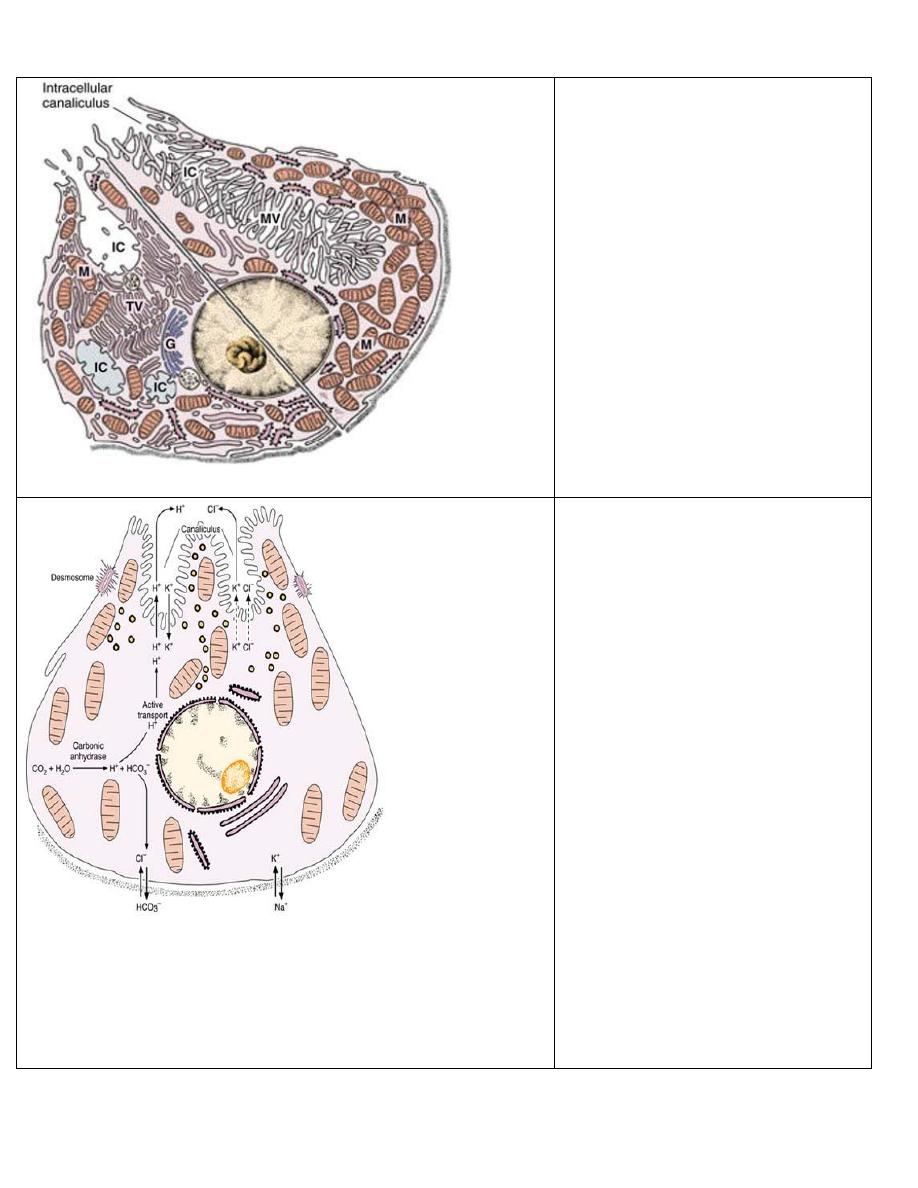
Composite diagram of a parietal cell,
showing the ultrastructural differences
between a resting cell (left) and an
active cell (right). Note that the
tubulovesicles (TV) in the cytoplasm of
the resting cell fuse to form microvilli
(MV) that fill up the intracellular
canaliculi (IC). G, Golgi complex; M,
mitochondria. (Based on the work of Ito
S, Schofield GC. J Cell Biol 1974;
63:364.)
Diagram of a parietal cell, showing the
main steps in the synthesis of
hydrochloric acid. Active transport by
ATPase is indicated by arrows and
diffusion is indicated by dotted arrows.
Under the action of carbonic anhydrase,
blood CO2 produces carbonic acid.
Carbonic acid dissociates into a
bicarbonate ion and a proton H+, which
is pumped into the stomach lumen in
exchange for K+. A high concentration
of intracellular K+ is maintained by the
Na+,K+ ATPase, while HCO3— is
exchanged for Cl— by an antiport. The
tubulovesicles of the cell apex are seen
to be related to hydrochloric acid
secretion,
because
their
number
decreases
after
parietal
cell
stimulation.
The
bicarbonate
ion
returns to the blood and is responsible
for a measurable increase in blood pH
during digestion.
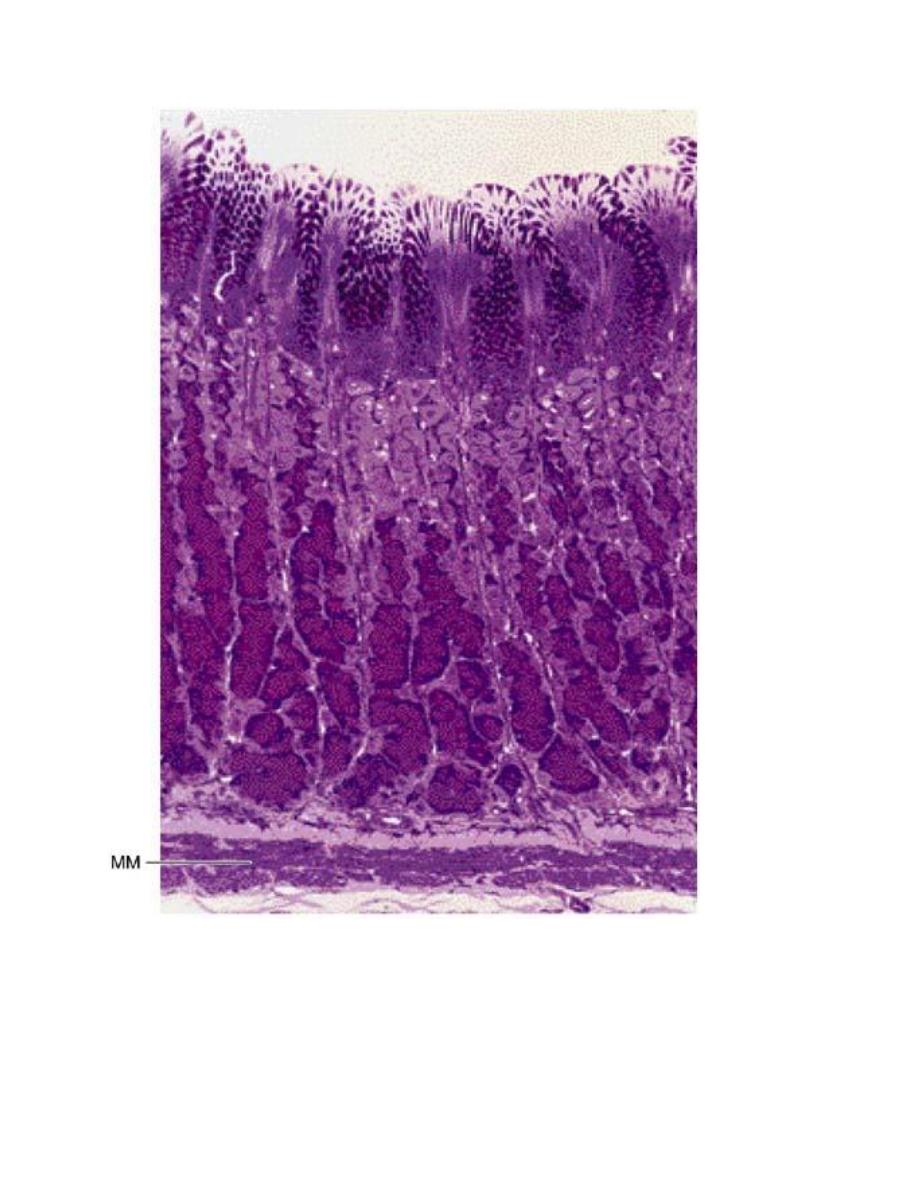
Photomicrograph of a section of the gastric glands in the fundus of the stomach. Note the superficial mucus-
secreting epithelium. Parietal cells (light-stained) predominate in the mid and upper regions of the glands; chief
(zymogenic) cells (dark-stained) predominate in the lower region of the gland. MM, muscularis mucosae. PT
stain. Low magnification.
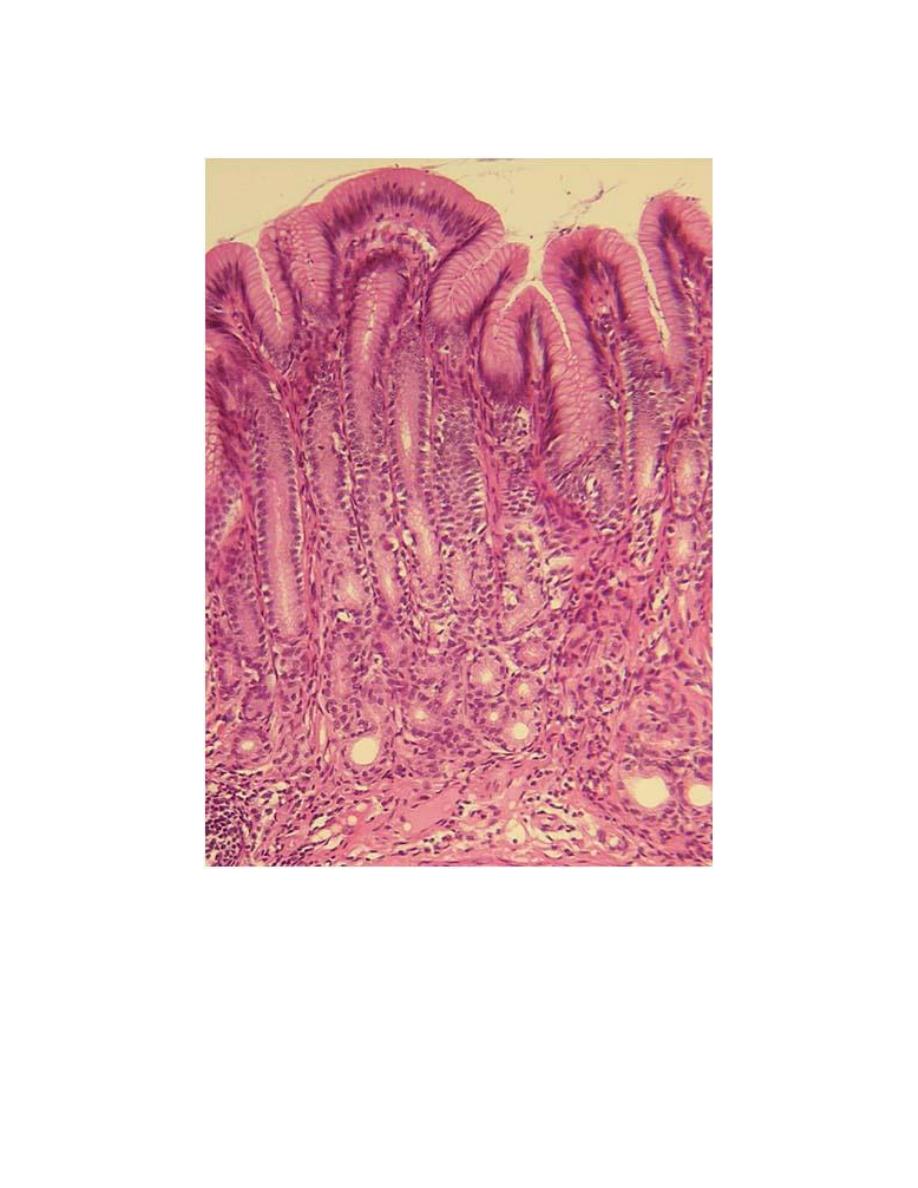
Photomicrograph of a section of the pyloric region of the stomach.
Note the deep gastric pits with short pyloric glands in the lamina
propria. H&E stain. Low magnification. (Courtesy of MF Santos.)
