Assistant Professor
Dr. Shamil AL-NeaimyMBchB MSc Ph D
Antiarrhythmic drugs
The student should make knowledge about:
Drugs for cardiac arrhythmiasPrincipal drugs by class
Objectives:The pathophysiology of cardiac arrhythmias is complex and the actions of drugs that are useful in stopping or controlling them may seem equally so.
Drug therapy for arrhythmias has a place beside radiofrequency ablation or the use of implanted devices
Overview:
OBJECTIVES OF TREATMENT
In almost no other set of conditions is it so clearly obvious to remember the dual objectives, which are to reduce morbidity and mortality.
DRUGS FOR CARDIAC ARRHYTHMIAS
Cardiac muscles are of 2 types:The first type is ordinary myocardial (atrial and ventricular) muscle, responsible for the pumping action of the heart.
The second type is specialized conducting tissue that initiates the cardiac electrical impulse and determines the order in which the muscle cells contract e.g. the SA and AV nodes
SOME PHYSIOLOGY
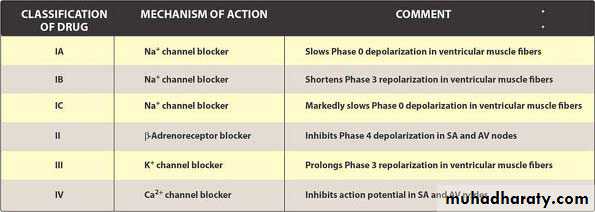
This partially relates to the phases of the cardiac cycle:CLASSIFICATION OF ANTIARRHYTHMIC DRUGS
These drugs restrict the rapid inflow of sodium during phase 0 and thus slow the maximum rate of depolarization (membrane stabilising activity)Class I: sodium channel blockade
A. lengthen action potential duration and refractoriness (adjunctive class III action), e.g. quinidine, disopyramide, procainamide
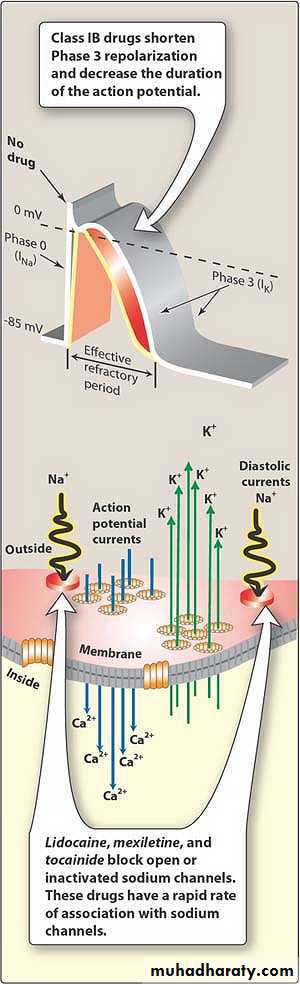
B. shorten action potential duration and refractoriness, e.g. lidocaine and mexiletine
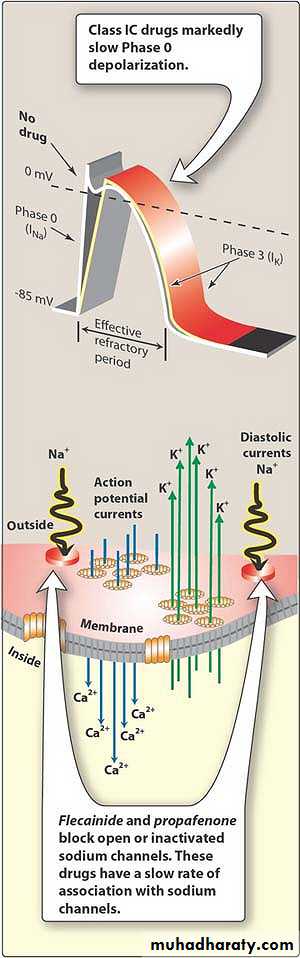
C. have negligible effect on action potential duration and refractoriness, e.g. flecainide, propafenone
The class subdivides into drugs that:
Propranolol and other β-adrenoceptor antagonists reduce background sympathetic tone in the heart,reduce automatic discharge (phase 4) and
protect against adrenergically stimulated ectopic pacemakersClass II: catecholamine blockade
These drugs depress the slow inward calcium current (phase 2) andprolong conduction and refractoriness particularly in the SA and AV nodes,
which helps to explain their effectiveness in terminating paroxysmal supraventricular tachycardia,e.g. verapamil.
Class IV: calcium channel blockade
Quinidine is considered the prototype class I drug.
In addition to its class IA activity:Quinidine has positive inotropic effect
Reduces vagus nerve activity (antimuscarinic effect).Quinidine
1. Antimuscarinic effect2. Serious ventricular tachyarrhythmias
3. Non-cardiac effects, called 'cinchonism', include:diarrhea
gastrointestinal symptoms,
rashes,
thromobocytopenia and fever.
Adverse reactions:
1.They counteract the arrhythmogenic effect of catecholamines.
2.Abolishe rate of automatic firing of the SA node3.β-Blockers prolong the refractoriness of the AV node
4.Many β-blocking drugs also possess membrane stabilizing (class I) propertiesCLASS II (CATECHOLAMINE BLOCKADE):
In patients with depressed myocardial contractility,
the combination of oral or intravenous β-blockade and calcium channel blockade (nifedipine, verapamil)
may cause hypotension or heart failure
Interactions
Amiodarone:Amiodarone is the most powerful antiarrhythmic drug available for the treatment and prevention of both atrial and ventricular arrhythmias
CLASS III POTASSIUM CHANNEL BLOCKADE)
1. Chronic ventricular arrhythmias2. To maintain sinus rhythm after cardioversion for atrial fibrillation or flutter.
3.Amiodarone was used for the management of re-entrant supraventricular tachycardias.USES:
1.Cardiovascular effects include bradycardia, heart block and induction of ventricular arrhythmia.
2.Others : nausea, vomiting, taste disturbances and the development of corneal microdeposits.
3.Plasma transaminase levels may rise.
4. hyperthyroidism and hypothyroidismAdverse reactions:
5.Photosensitivity reactions are common.6.Amiodarone may cause a bluish discoloration on exposed areas of the skin.
7. Less commonly, pneumonitis and pulmonary fibrosis occur.8.Peripheral neuropathy and myopathy occur.
Adverse reactions1.With digoxin & with warfarin increases the effect of both these drugs.
2.β-Blockers and calcium channel antagonists augment the depressant effect of amiodarone on SA and AV node function.Interaction
Calcium channel blockers inhibit the passage of calcium through the membrane channels;
the result in myocardial cells is to depress contractility, and in pacemaker cells to suppress their automatic activity.Members of the group therefore may have negative cardiac inotropic and chronotropic actions,
CLASS IV (CALCIUM CHANNEL BLOCKADE)
A 57-year-old man is being treated for an atrial arrhythmia. He complains of headache, dizziness, and tinnitus. Which one of the following antiarrhythmic drugs is the most likely cause?
A. Amiodarone.
B. Procainamide.
C. Propranolol.
D. Quinidin
E. Verapamil.