Physiology
Smooth muscles

Objectives
1-Describe the structural morphology of the
smooth muscles and their types?
2-Explain the bases of contraction of smooth
muscles?
3-list the factors affecting the smooth muscle
contraction?
4- How does changing the length of smooth
muscle affect its tension?

Morphology
:
-Lack visible cross striations.
-Actin and myosin are present.
-There are dense bodies instead of Z lines.
-Contain tropomyosin but toponin absent.
-Poorly developed sarcoplasmic reticulum
-Few mitochondria so depend on glycolysis in
their metabolism.

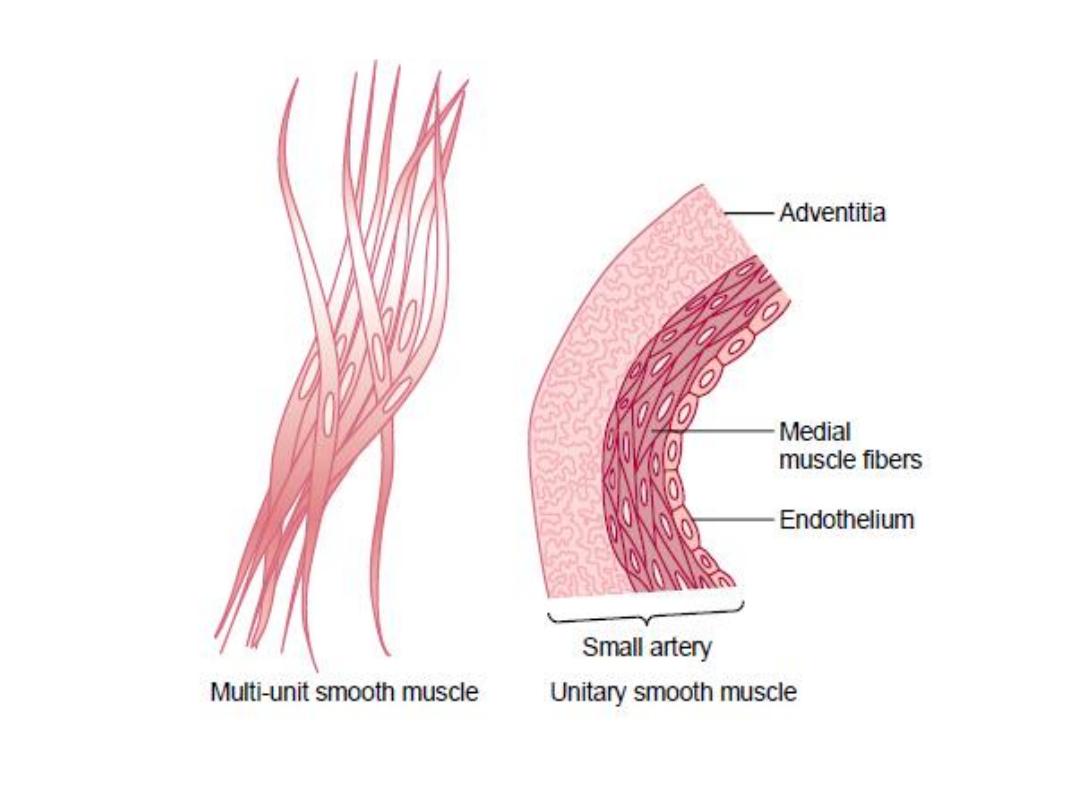
2 Types:
-Visceral smooth muscle (unitary or single unit).
-Multi-unit smooth muscle.
-Unitary or visceral smooth muscles (or syncytial smooth
muscles):
It occurs in large sheets, has low-resistance bridges between
individual muscle cells, and functions in a syncytial fashion, they
contract together as a single unit. It is found primarily in the
walls of hollow viscera.
The cell membranes are joined by gap junctions through whom
ions can flow freely from one muscle cell to another.
Multi-unit smooth muscle:
It is made up of individual units without interconnecting bridges.
It is found in structures such as the iris of the eye, in which fine,
graded contractions occur. It is not under voluntary control.
Electrical & Mechanical Activity:
Visceral smooth muscle:
It is characterized by the instability of its membrane potential
and by the fact that it shows continuous, irregular contractions
that are independent of its nerve supply.
This maintained state of partial contraction is called tonus or
tone.
There is no true "resting" value for the membrane potential, but
it averages about -50 mV, when the muscle active it becomes
low and high during inhibition.
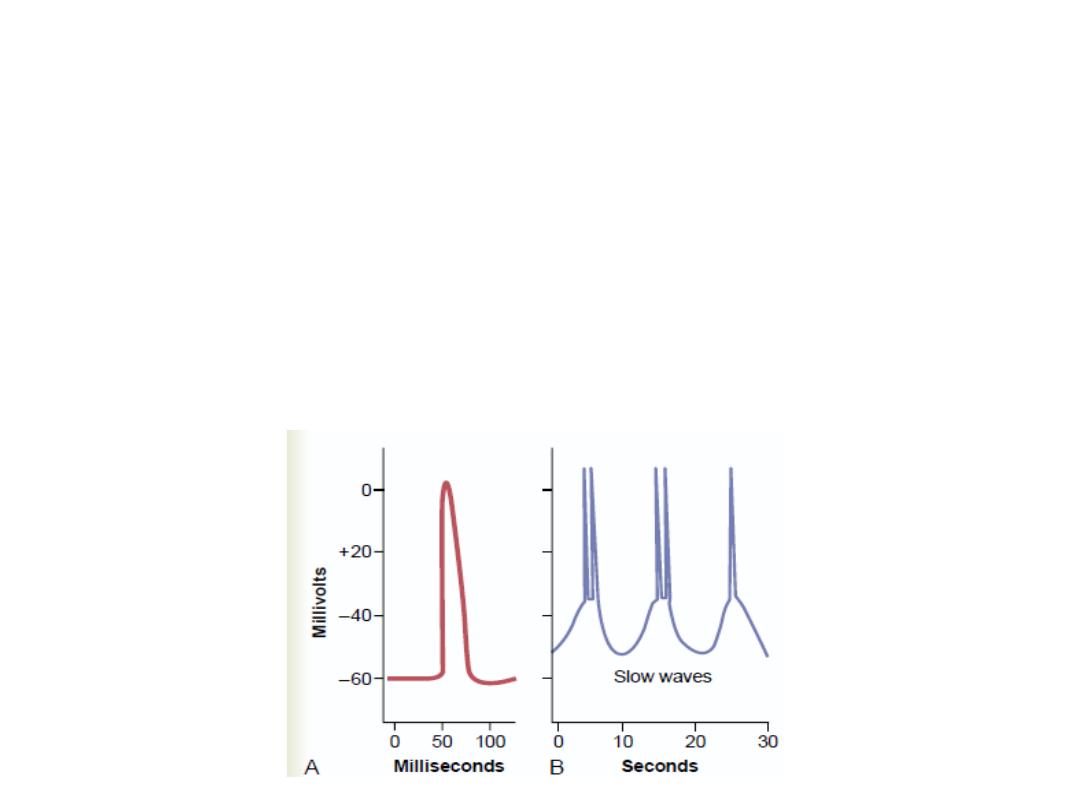
Superimposed on the membrane potential are waves of various types:
There are
-Slow sine wave-like.
Sharp spikes.
Pacemaker potentials.
Thus, the excitation-contraction coupling in visceral smooth muscle is a very
slow process compared with that in skeletal and cardiac muscle, in which the
time from initial depolarization to initiation of contraction is less than 10 ms.
Molecular Basis of Contraction
;
1-Binding of Ach to Muscarinic reseptors.
2-Ca
2+
influx from the ECF via Ca
2+
channels.
3-Ca
2+
binds to calmodulin, and the resulting complex activates
calmodulin-dependent myosin light chain kinase. This enzyme
catalyzes the phosphorylation of the myosin light chain.
4-The phosphorylation allows the myosin ATPase to be activated, and
actin slides on myosin, producing contraction.
5-Myosin is dephosphorylated by myosin light chain phosphatase in
the cell.
6-Relaxation of the smooth muscle.
Dephosphorylation of myosin light chain kinase does not necessarily
lead to relaxation of the smooth muscle. a latch bridge mechanism
by which myosin cross-bridges remain attached to actin for some
time after the cytoplasmic Ca
2+
concentration falls. This produces
sustained contraction with little expenditure of energy, which is
especially important in vascular smooth muscle.

of the smooth muscles:
Stimulation
1- Stretch:
It contracts when stretched in the absence of
any extrinsic innervations. Stretch is followed
by a decline in membrane potential, an
increase in the frequency of spikes and a
general increase in tone.

Chemical mediators
:
1-epinephrine or norepinephrine
:
The membrane potential usually becomes larger, the spikes decrease in frequency,
and the muscle relaxes.
Norepinephrine exerts both α and β actions on the muscle.
The β action, reduced muscle tension in response to excitation, is mediated via cyclic
AMP and is due to increased intracellular binding of Ca
2+
.
The α action, which is also inhibition of contraction, is associated with increased Ca
2+
efflux from the muscle cells.
2- Acetylcholin:
Has an effect opposite to that of norepinephrine on the membrane potential
acetylcholine causes the membrane potential to decrease and the spikes become
more frequent , with an increase in tonic tension and the number of rhythmic
contractions.
Released by stimulation of cholinergic nerves (similar to cold and stretch in vitro).
Other chemicals: like progesterone which decreases the activity and estrogen which
increase it (in uterine smooth muscles).
-Thermal stimuli : like cold which causes spasm.
Function of the Nerve Supply to Smooth Muscle:
It has two important properties: (1) its spontaneous activity in
the absence of nervous stimulation, and
(2) Its sensitivity to chemical agents released from nerves locally
or brought to it in the circulation.
The function of the nerve supply is not to initiate activity in the
muscle but rather to modify it (control).
It has dual nerve supply from 2 divisions of the autonomic
nervous system. Stimulation of one division usually increases
smooth muscle activity, whereas stimulation of the other
decreases it.
(i.e if noradrenergic increase ,the Acetylcholine decrease and
visa versa).

Relation of Length to Tension; Plasticity
:
It is the variability of the tension it exerts at any given length. If a
piece of visceral smooth muscle is stretched, it first exerts increased
tension, if the muscle is held at the greater length after stretching,
the tension gradually decreases. It is consequently impossible to
correlate length and developed tension accurately.
In intact humans, For example, the tension exerted by the smooth
muscle walls of the bladder can be measured at different degrees of
distention as fluid is infused into the bladder via a catheter Initially
there is relatively little increase in tension as volume is increased,
because of the plasticity of the bladder wall. However, a point is
eventually reached at which the bladder contracts forcefully. This
phenomenon is called stressrelaxation and reverse stress-relaxation.
Its importance is that its ability to return to nearly its original force
of contraction seconds or minutes after it has
been elongated or shortened
MULTI-UNIT SMOOTH MUSCLE:
-It is nonsyncytial .
-Contractions do not spread widely through it (discrete, fine and more
localized).
- Very sensitive to circulating chemical substances and is normally activated
by chemical mediators (acetylcholine and norepinephrine).
- Norepinephrine tends to persist in the muscle and to cause repeated firing
of the muscle after a single stimulus rather than a single action potential.
Therefore, the contractile response produced is usually an irregular
tetanus rather than a single twitch.
The simple muscle twitch resembles the twitch contraction of skeletal muscle
except that its duration is ten times longer.
