
Physiology of
Blood
ABO system
By prof. Israa f. jaafar

Learning objectives
•
To describe different types of blood
groups
•
To understand cross matching
•
To know safe blood transfusion
•
To understand transfusion reactions

Blood Typing -Surface Antigens
•
Are cell surface proteins that identify cells to
immune system
•
Normal cells are ignored and foreign cells
attacked

Figure 19–6a
4 Basic Blood Types
Blood types are genetically
determined
By presence or absence of RBC
surface antigens
A
,
B
,
Rh

4 Basic Blood Types
•
A
(surface antigen A)
•
B
(surface antigen B)
•
AB
(antigens A and B)
•
O
(neither A nor B)
Agglutinogens
•
Antigens on surface of RBCs
•
Screened by immune system
•
Plasma antibodies attack (
agglutinate
) foreign
antigens

Blood Plasma Antibodies
•
Type A: type B antibodies
•
Type B: type A antibodies
•
Type O: both A and B antibodies
•
Type AB: neither A nor B

The
Rh Factor
•
Also called
D antigen
•
Either
Rh positive
(Rh
+
) or
Rh negative
(Rh
—
)
•
Only
sensitized
Rh
—
blood has anti-Rh
antibodies
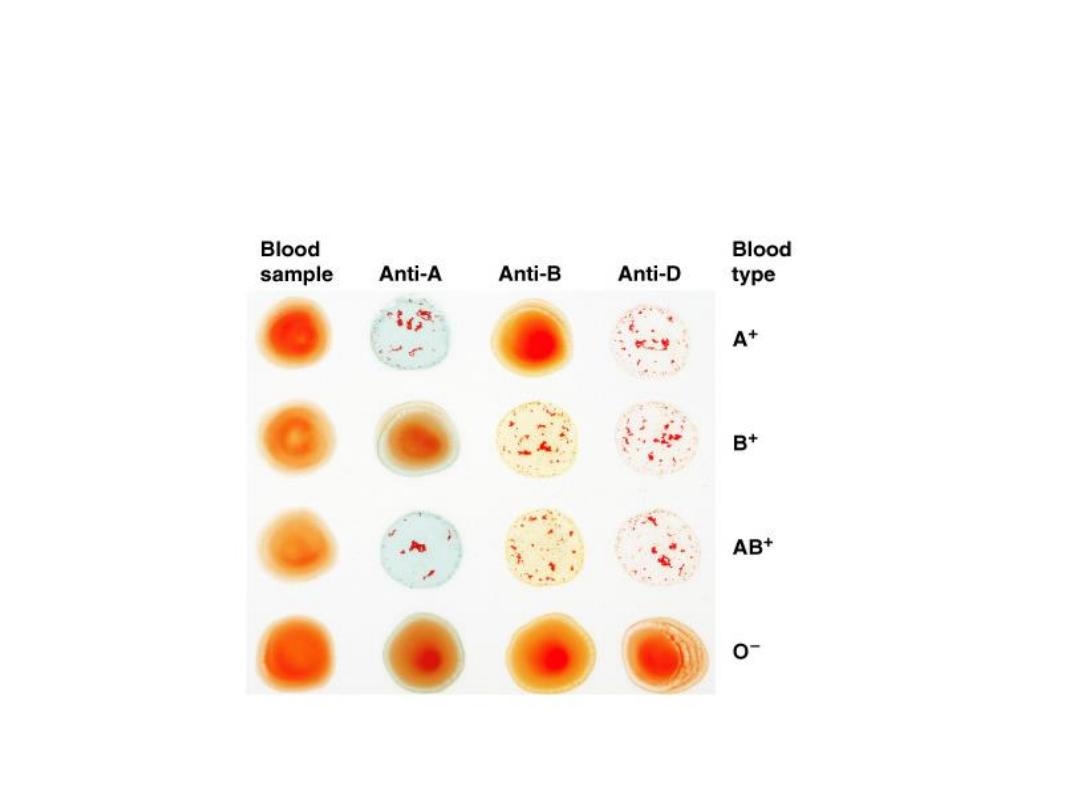
Blood Type Test
•
Determines blood type and compatibility

Cross matching
Cross-Match Test:
Performed on donor and
recipient blood for compatibility
In cross-matching, donor red cells are mixed with
recipient plasma on a slide and checked for
agglutination. It is advisable to check the action of the
donor's plasma on the recipient cells in addition, even
though, this is rarely a source of trouble.
A procedure that has recently become popular is to withdraw
the patient's own blood in advance of elective surgery and then
infuse this blood back (
autologoustransfusion
) if a transfusion
is needed during the surgery

Cross-Reaction
•
Also called
transfusion reaction
•
Plasma antibody meets its specific surface
antigen
•
Blood will agglutinate and hemolyze
•
If donor and recipient blood types not
compatible

Cross-Reaction
•
Also called
transfusion reaction
•
Plasma antibody meets its specific surface
antigen
•
Blood will agglutinate and hemolyze
•
If donor and recipient blood types not
compatible

Transfusion Reactions
Dangerous hemolytic transfusion reactions occur when blood
is transfused into an individual with an incompatible blood
type; that is, an individual who has agglutinins against the red
cells in the transfusion.
The plasma in the transfusion is usually so diluted in the
recipient that it rarely causes agglutination even when the
titer of agglutinins against the recipient's cells is high.
However, when the recipient's plasma has agglutinins against
the donor's red cells, the cells agglutinate and hemolyze. Free
hemoglobin is liberated into the plasma. The severity of the
resulting transfusion reaction may vary from an asymptomatic
minor rise in the plasma bilirubin level to severe jaundice and
renal tubular damage leading to anuria and death.

Hemolytic Disease of the Newborn
when an Rh-negative mother carries an Rh-positive fetus. Small amounts of
fetal blood leak into the maternal circulation at the time of delivery, and
some mothers develop significant titers of anti-Rh agglutinins during the
postpartum period.
During the next pregnancy, the mother's agglutinins cross the placenta to
the fetus.
In any case, when anti-Rh agglutinins cross the placenta to an Rh-positive
fetus, they can cause hemolysis and various forms of hemolytic disease of
the newborn (erythroblastosisfetalis). If hemolysis in the fetus is severe,
the infant may die in utero or may develop anemia, severe jaundice, and
edema (hydropsfetalis). Kernicterus, a neurologic syndrome in which
unconjugated bilirubin is deposited in the basal ganglia, may also develop,
especially if birth is complicated by a period of hypoxia.
Bilirubin rarely penetrates the brain in adults, but it does in infants
because
1.the
blood–brain barrier is more permeable in infancy
.
2.the bilirubin-conjugating system is not yet mature.

About 50% of Rh-negative individuals are sensitized (develop an anti-Rh
titer) by transfusion of Rh-positive blood. Because sensitization of Rh-
negative mothers by carrying an Rh-positive fetus generally occurs at
birth, the first child is usually normal. However, hemolytic disease
occurs in about 17% of the Rh-positive fetuses born to Rh-negative
mothers who have previously been pregnant one or more times with Rh-
positive fetuses. it is usually possible to prevent sensitization from
occurring the first time by administering a single dose of
anti-Rh
antibodies in the form of Rh immune globulin during the postpartum
period.
In obstetric clinics, the institution of such treatment on a routine basis to
unsensitized Rh-negative women who have delivered an Rh-positive
baby has reduced the overall incidence of hemolytic disease by more
than 90%. In addition, fetal Rh typing with material obtained by
amniocentesis or chorionic villus sampling is now possible, and
treatment with a small dose of Rh immune serum will prevent
sensitization during pregnancy.
