
Lect. 7
Cardiac arrhythmia
Objectives:
1. List the types of arrhythmias.
2. Identify on ECG: ectopic beats, atrial & ventricular fibrillation,
heart block.
The causes of the cardiac arrhythmias are usually one or a combination of
the following abnormalities in the rhythmicity-conduction system of the
heart:
1- Abnormal rhythmicity of the pacemaker.
2- Shift of the pacemaker from the sinus node to other parts of the heart.
3- Blocks at different points in the transmission of the impulse through
the heart.
4- Abnormal pathways of impulse transmission through the heart.
5- Spontaneous generation of abnormal impulses in almost any part of the
heart.
Types of arrhythmias
1- Abnormal sinus rhythms.
2- Conduction block.
3- Premature Contractions.
4- Paroxysmal tachycardia.
1-Abnormal sinus rhythms:
Sinus Tachycardia.
Sinus Bradycardia.
Sinus Arrhythmia.
Tachycardia
The term "tachycardia" means fast heart rate, usually defined as faster
than 100 beats per minute. The electrocardiogram is normal except that
the rate of heartbeat is increased. The general causes of tachycardia are:
increased body temperature,
Stimulation of the heart by the sympathetic nerves.
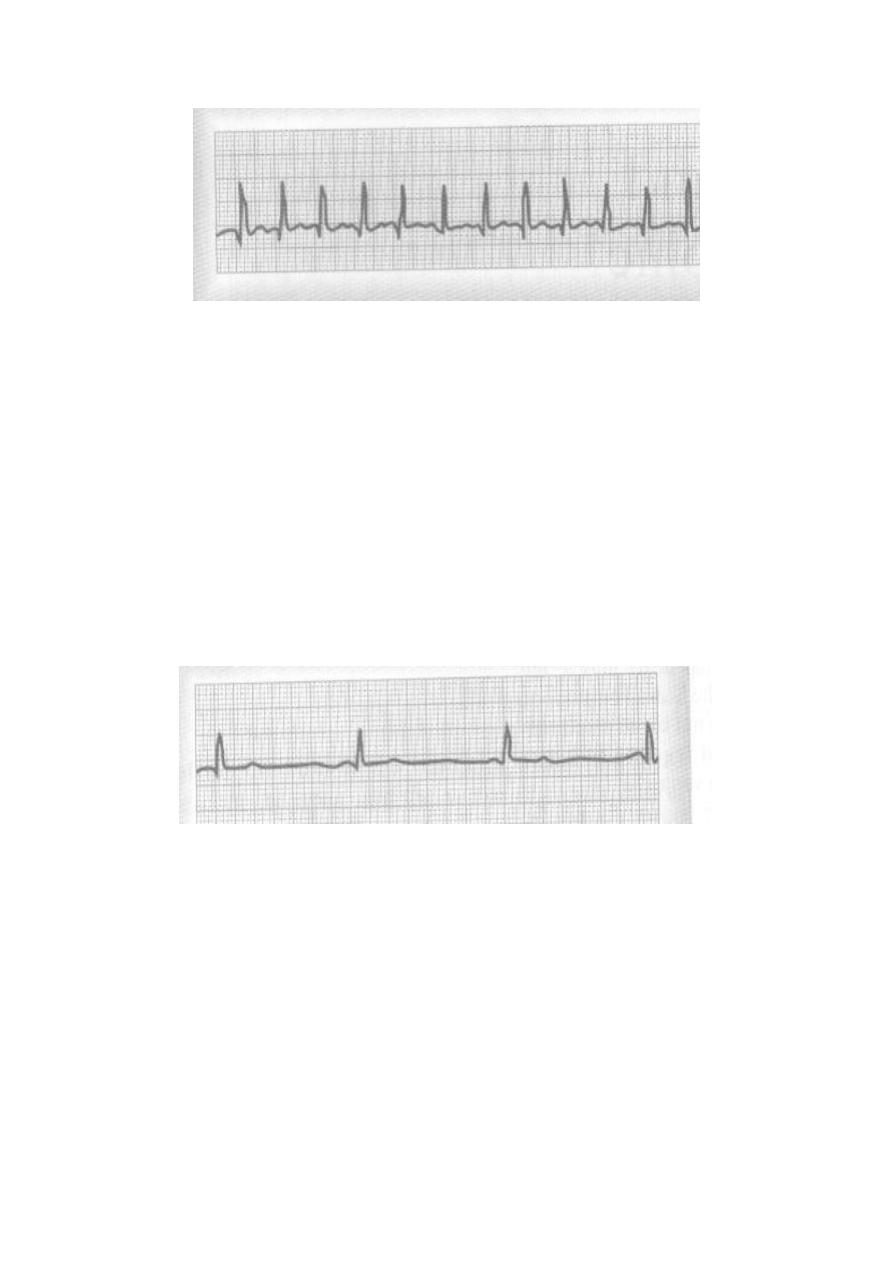
Sinus tachycardia, HR = 150 (300/2)
Bradycardia
The term "bradycardia" means a slow heart rate, usually defined as less
than 60 beats per minute. Examples:
Bradycardia in Athletes.
Vagal Stimulation. In patients with carotid sinus syndrome;
arteriosclerosis of the carotid sinus causes excessive sensitivity of
the baroreceptors located in the arterial wall; as a result, mild
pressure on the neck elicits a strong baroreceptor reflex, causing
intense vagal stimulation of the heart and extreme bradycardia.
Sometimes this reflex is so powerful that it stops the heart.
Sinus bradycardia of 40 beats per minute.
(300/7.5 = 40)
Sinus Arrhythmia
The heart rate is increased during inspiration and decreased during
expiration. The ECG is normal except that the number of the cycles varies
with the two phases of respiration. It is a common normal finding in young
adults and children.
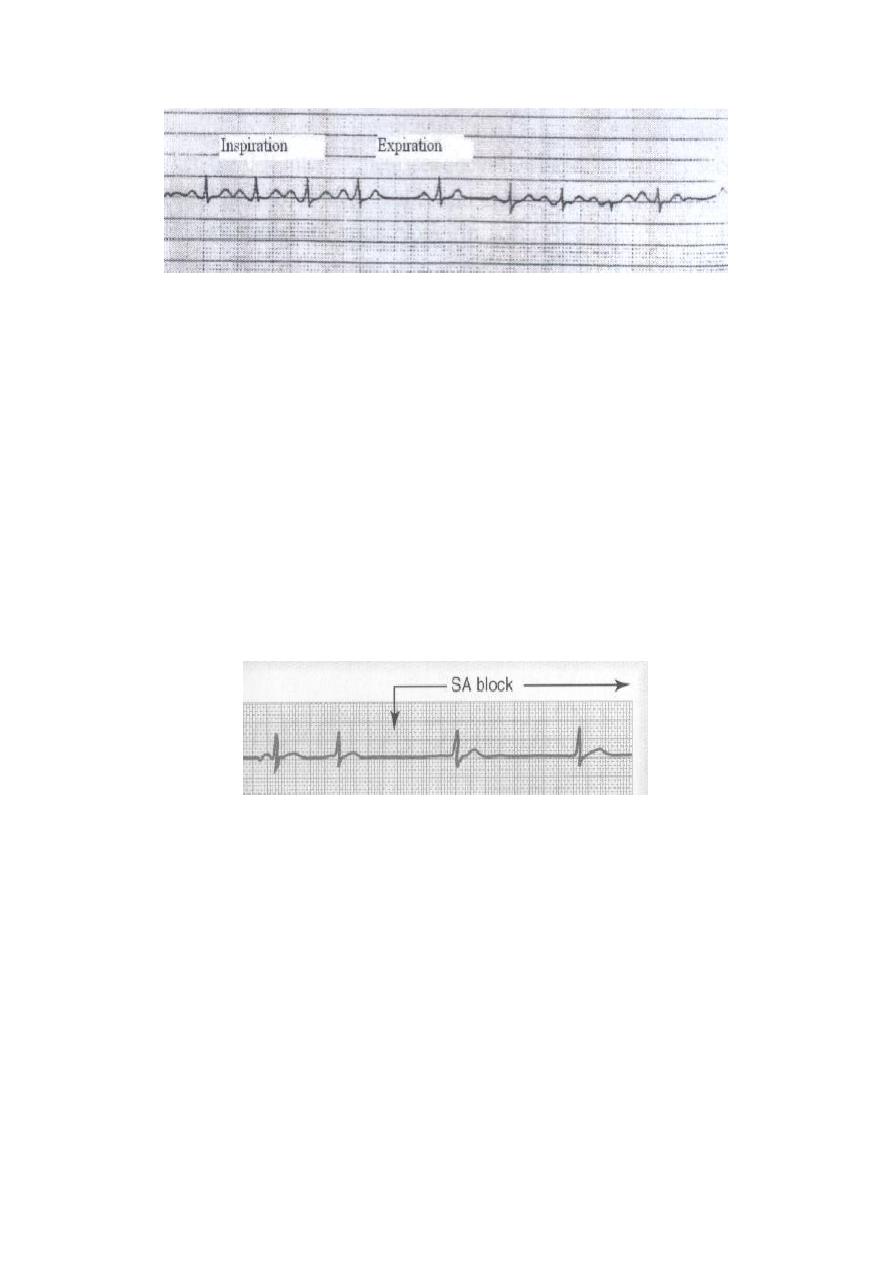
Sinus arrhythmia, acceleration of sinus rate during inspiration
and slowing during expiration.
2-Conduction block:
Sinoatrial Block.
Atrioventricular Block (Heart Block).
1. First Degree Heart Block.
2. Second Degree Heart Block.
3. Third Degree Heart Block.
Sinoatrial Block
The impulse from the sinus node is blocked before it enters the atrial
muscle. There is sudden cessation of P- wave with standstill of the
atrium (missed beat).
Sinoatrial nodal block (missed beat).
Atrioventricular Block (Heart Block)
Impulses pass from the atria into the ventricles is through the A-V bundle
(the bundle of His). Conditions that can either decrease or block the
impulse through this bundle are:
Ischemia of the A-V node or A-V bundle fibers by coronary
insufficiency.
Compression of the A-V bundle by scar tissue or by calcification.
Inflammation of the A-V node or A-V bundle, which can results
frequently from different types of myocarditis, such as occur in
diphtheria and rheumatic fever.
Extreme stimulation of the heart by the vagus nerves blocks
impulse conduction through the A-V node. Such vagal excitation
occasionally results from strong stimulation of the baroreceptors in
people with the carotid sinus syndrome.
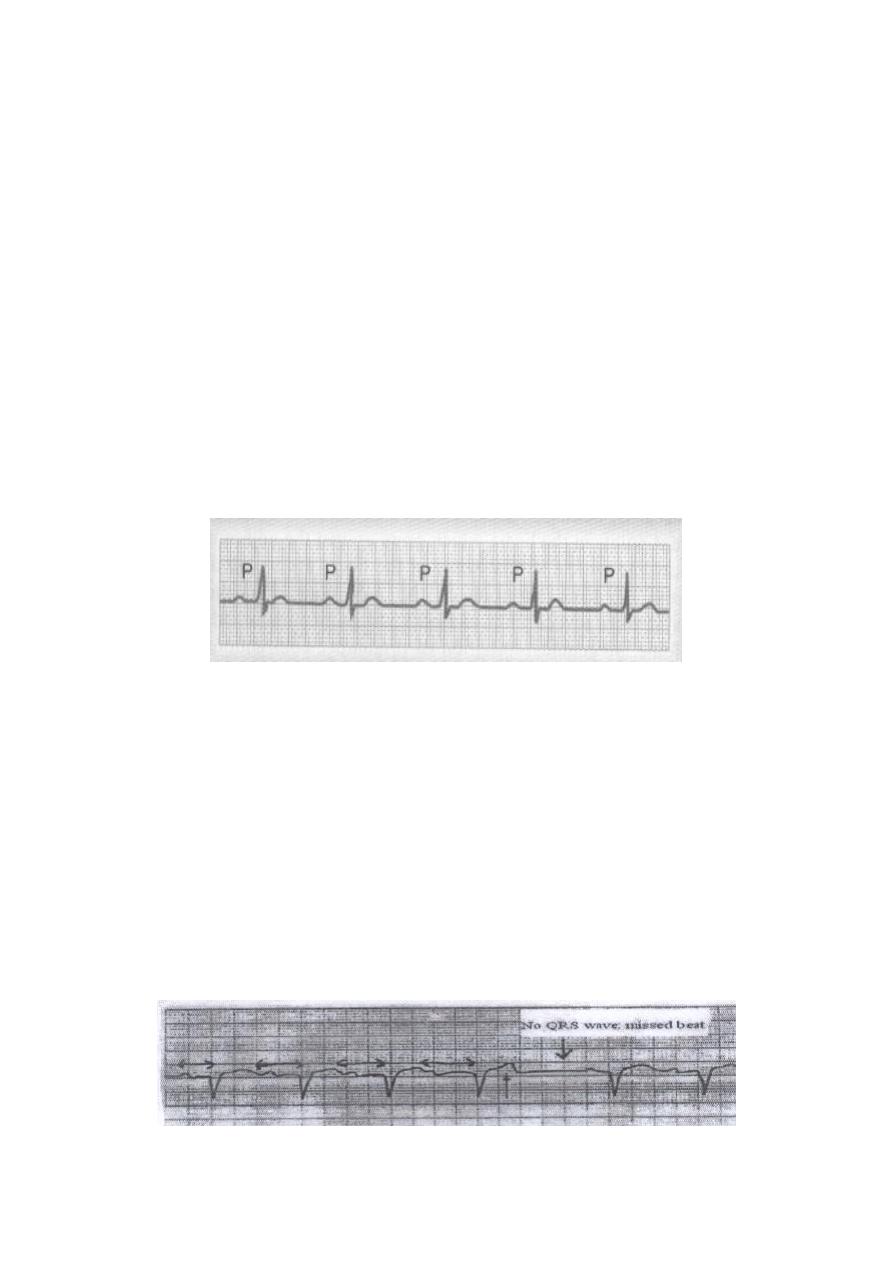
First Degree Heart Block (Prolonged P-R interval)
The normal time between the beginning of the P wave and the beginning
of the QRS complex is 0.12 – 0.21 second, when the heart is beating at a
normal rate. This P-R interval usually decreases in length with faster
heartbeat and increases with slower heartbeat. When the P-R interval
increases above a value of about 0.21 second in a heart beating at normal
rate, the P-R interval is said to be prolonged and the patient is said to
have first degree incomplete heart block (in acute rheumatic fever). The
following Figure shows an electrocardiogram with a prolonged P-R
interval. Thus, first degree heart block is defined as a delay of conduction
from the atria to the ventricles but not actual blockage of conduction.
First-degree heart block, prolonged P-R interval.
Second Degree Heart Block
The atria beat at a faster rate than the ventricles, and there are dropped
beats of the ventricles. This condition is called second degree incomplete
heart block, as shown in the following figures; a progressive prolongation
of the P-R intervals as well as one dropped beat as a result of failure of
conduction from the atria to the ventricles.
At times, every other beat of the ventricles is dropped, so that a "2:1
rhythm" develops in the heart, with the atria beating twice for every
single beat of the ventricles. Sometimes other rhythms such as 3:2 or 3:1
also develop.
Second-degree heart block, progressive PR prolongation failure of

P-wave conduction to the ventricle (missed ventricular beat).
Second-degree heart block, with missed ventricular beat.
Third Degree Heart Block (Complete heart block)
Complete block of the impulse from the atria into the ventricles. The P
waves become dissociated from the QRS-T complexes. As shown, the
rate of ventricular beat is less than 40 per minute. Furthermore, there is
no relation between the rhythm of the P waves and that of the QRS-T
complexes because the ventricles have escaped from control by the atria,
and they are beating at their own natural rate.
Complete heart block. P-waves are dissociated
from the QRS complexes.
3-Premature Contractions:
A premature contraction is a contraction of the heart before the time that
normal contraction would have been expected. This condition is also
called extrasystole, premature beat, or ectopic beat. Most premature
contractions result from ectopic foci in the heart, which emit abnormal
impulses at odd times. The possible causes:
Local areas of ischemia.
Small calcified plaques at different points in the heart, which press
against the adjacent cardiac muscle so that some of the fibers are
irritated.
Toxic irritation of the A-V node, Purkinje system, or myocardium
caused by drugs, nicotine, or caffeine. Mechanical initiation of
premature contractions is also frequent during cardiac
catheterization.

Premature Atrial Contractions
The following figure shows a single premature atrial contraction, The P-
wave of this beat occurs too soon in the heart cycle, and the P-R interval
is shortened, indicating that the ectopic origin of the beat is near the A-V
node. Also, the interval between the premature contraction and the next
succeeding contraction is slightly prolonged, which is called a
compensatory pause. One of the reasons for this is that the premature
contraction originated in the atrium some distance from the sinus node,
and the impulse had to travel through a considerable amount of atrial
muscle before it discharged the sinus node. Consequently, the sinus node
discharged late in the premature cycle, and this made the succeeding
sinus node to be discharged late. Premature atrial contractions occur:
In healthy people.
In athletes.
Mild toxic conditions resulting from; excess smoking, lack of
sleep, ingestion of too much coffee, alcoholism, and the use of
various drugs.
Atrial premature beat.
Premature Ventricular Contractions
The electrocardiogram of the following figure shows a series of
premature ventricular contractions (PVCs) alternating with normal
contractions. PVCs cause specific effects in the electrocardiogram, as
follows:
The QRS complex is usually prolonged.
The QRS complex has a high voltage.
The T wave has a potential polarity opposite to that of the QRS

complex.
Some PVCs result from factors such as cigarettes, coffee, lack of sleep,
and emotional irritability. Other PVCs originate from infracted or
ischemic areas of the heart.
Ventricular ectopic beats, broad QRS complex.
4-Paroxysmal tachycardia:
Abnormalities in any portion of the heart, including the atria, the Purkinje
system, or the ventricles, can cause rapid rhythmical discharge of
impulses that spread in all directions throughout the heart. The term
"paroxysmal" means that the heart rate usually becomes rapid in
paroxysms, with the paroxysms beginning suddenly and lasting for a few
seconds, a few minutes, a few hours, or much longer. Then the paroxysms
usually end suddenly as they begun, with the pacemaker of the heart
shifting back to the sinus node.
Paroxysmal tachycardia:
Supraventricular arrhythmias:
1. Atrial tachycardia;
a- Supraventricular tachycardia (SVT).
b- Atrial fibrillation (AF).
c- Atrial flutter.
2. Junctional tachycardias (AV nodal paroxysmal tachycardia).
Ventricular paroxysmal tachycardia.
a- Ventricular tachycardia (VT).
b- Ventricular fibrillation (VF).
Supraventricular arrhythmias:
Atrial tachycardias (arising from atrial myocardium) or junctional
tachycardias (AV node tachycardia), both of which are called
Supraventricular tachycardias, usually occurs in young, otherwise healthy
people.
They are originated above the bifurcation of bundle of His. The unique
characteristics of these arrhythmias are:
1- Narrow QRS.
2- P-wave either visible, irregular in shape and with shorter duration or
invisible.
3- Variable PR interval due to variable rate of conduction at AV node.
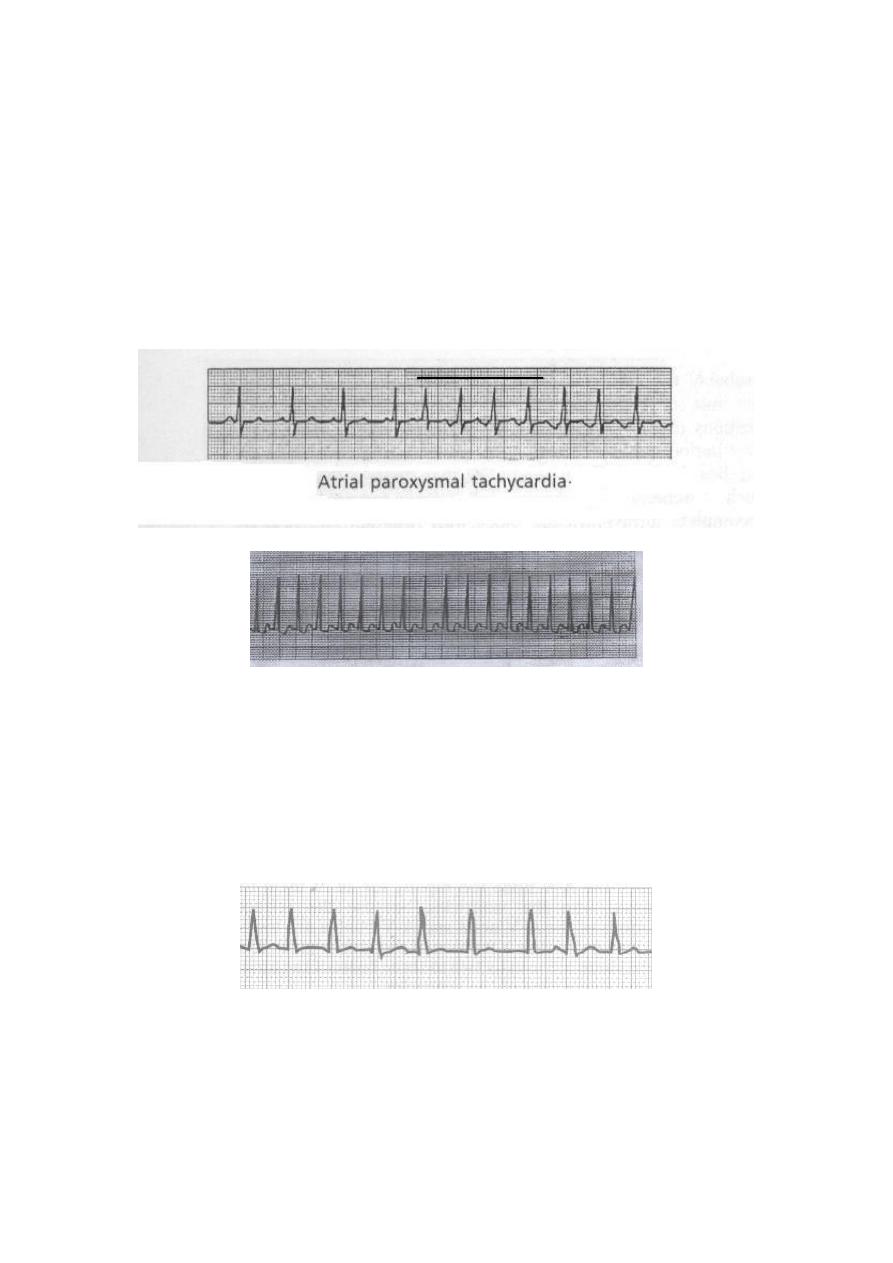
Atrial tachycardias:
a- paroxysmal Supraventricular tachycardia (SVT)
As shown in the following record, there is a sudden increase in the rate of
heartbeat from about 95 to about 150 beats per minute. It can be seen that
an inverted P-wave occurs before each of the QRS-T complexes during
the paroxysm of rapid heartbeat, and this P-wave is partially
superimposed on the normal T wave of the preceding beat. This indicates
that the origin of this paroxysmal tachycardia is in the atrium, but because
the P-wave is abnormal, the origin is not near the sinus node.
Supraventricular tachycardia, no P wave (missed) or obscured.
b- Atrial fibrillation
A frequent cause of atrial fibrillation is atrial enlargement resulting
from heart valve lesions, or from ventricular failure with excess
damming of blood in the atria. The dilated atrial walls predispose to
atrial fibrillation, which is irregular irregularity of the rhythm with no or
obscured P-wave.
Atrial fibrillation, no P wave or obscurred.
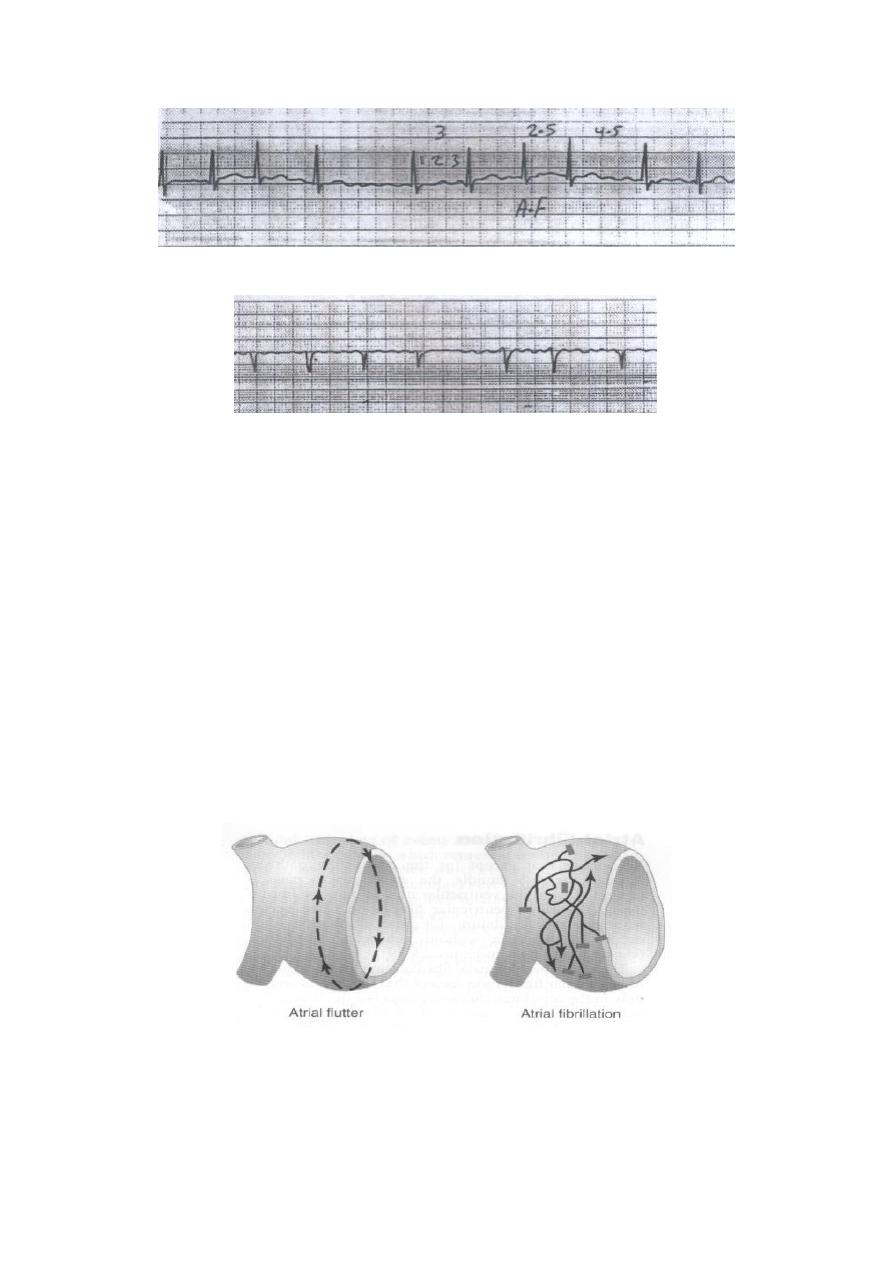
Atrial fibrillation; irregular rhythm (irregular irregularity).
Atrial fibrillation; Fine, high frequency, and very low voltage P- wave.
c- Atrial Flutter
In Atrial flutter, the electrical signal travels as a single large wave front
always in one direction around and around the atrial muscle mass. As
shown in the following Figure, this wave travels from top to bottom to
top around the openings of the superior and inferior venae cavae. Atrial
Flutter causes a rapid rate of contraction of the atria, usually between 200
and 350 beats per minute. But not all can stimulate the ventricles, there-
fore, there are usually two to three beats of the atria for every single beat
of the ventricles.
In the Atrial flutter ECG trace, the P waves are strong (saw-teeth
appearance), the QRS-T complex follows an atrial P wave only once for
every two to three beats of the atria, giving a 2:1 and a 3: 1 rhythm.
Pathways of impulses in atrial flutter and atrial fibrillation.

Atrial flutter; saw-teeth appearance of the P-wave.
Junctional tachycardias (AV nodal paroxysmal tachycardia)
Paroxysmal tachycardia often results from an aberrant rhythm that in-
volves the AV node. This usually causes normal QRST complexes but
missing or obscured P-waves.
Ventricular Paroxysmal Tachycardia (VT):
The electrocardiogram of ventricular paroxysmal tachycardia has the
appearance of a series of ventricular premature beats occurring one after
another without any normal beats inbetween. Ventricular tachycardia
frequently initiates the lethal condition of ventricular fibrillation because
of rapid stimulation of the ventricular muscle.
Ventricular paroxysmal tachycardia.
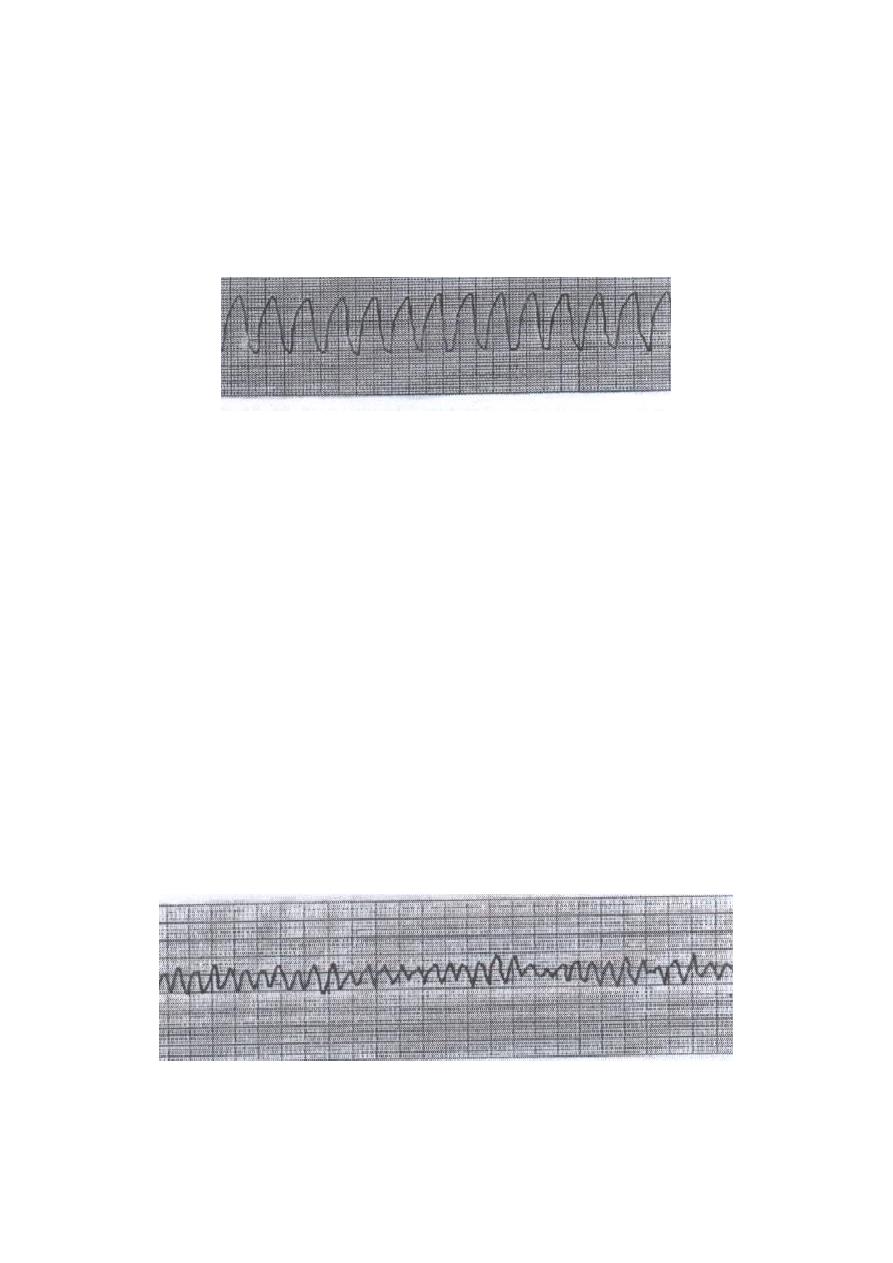
a- Ventricular tachycardia (VT)
VT refers to a rhythm originating from a ventricular ectopic focus at a
rate greater than 100 beats per minute. The ECG shows a wide-complex
tachycardia with no associated P-wave.
Ventricular tachycardia, regular wide QRS tachycardia
at a rate of 170 / min.
b- Ventricular fibrillation (VF)
Ventricular fibrillation results from cardiac impulses that have gone here
and there within the ventricular muscle mass. Stimulating first, one
portion of the ventricular muscle, then another portion, then another, and
eventually feeding back onto itself to re-excite the same ventricular
muscle over and over. Multiple factors can spark the beginning of
ventricular fibrillation:
(1) Sudden electrical shock of the heart.
(2) Ischemia of the heart muscle, of its specialized conducting system, or
both.
Ventricular fibrillation.
