
Lect. 8
Ccardiovascular innervations:
Cardiovascular centers
Objectives;
1. Identify
morphologically
differences
between
types
of
cardiovascular centers.
There are 2 main centers:
Vasomotor center (VMC).
Cardioinhibitory centre (CIC).
Vasomotor center:
This center located bilaterally in the reticular substance of the medulla
and lower pons. The center transmits parasympathetic impulses through
the vagus nerves to the heart and sympathetic impulses through the spinal
cord and peripheral sympathetic nerves to the heart and to the blood
vessels of the body. It includes the following areas or centers:
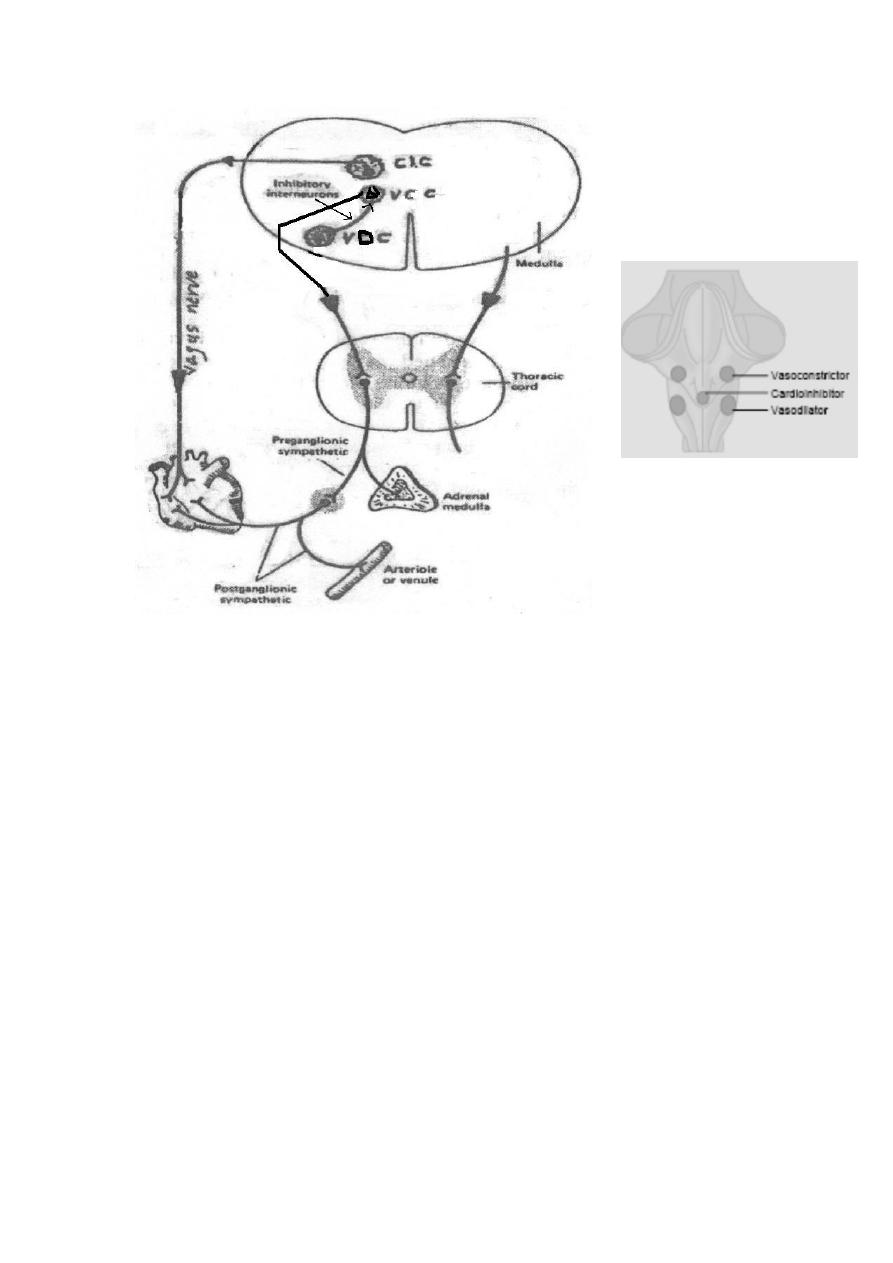
1-Vasoconstrictor center (VCC):
Its neurons secrete norepinephrine to excite the vasoconstrictor
neurons of the sympathetic system throughout the spinal cord.
Stimulation of the VCC increases the sympathetic discharge to:
The blood vessels (leading to generalized vasoconstriction (VC)).
The adrenal medullae (leading to secretion of Catecholamines).
The heart (increasing heart rate).
2-Vasodilator center (VDC):
Its fibers ascend upward to the vasoconstrictor center, inhibiting the
activity of this area (VCC), thus causing vasodilation. Stimulation of
this center leads to generalized vasodilatation (VD) by inhibiting the
activity of the VCC.
3-Sensory area:
Its neurons receive sensory nerve signals from the vagus and
glossopharyngeal nerves. This area controls the activities of the
vasoconstrictor and vasodilator centers, an example are the
baroreceptor reflex that controls the blood pressure.
At the same time, the vasomotor center controls the heart activity:
The lateral portion of the vasomotor center transmits excitatory
impulses through the sympathetic nerve fibers to the heart to
increase heart rate and contractility.
The medial portion of this center transmits impulses through the
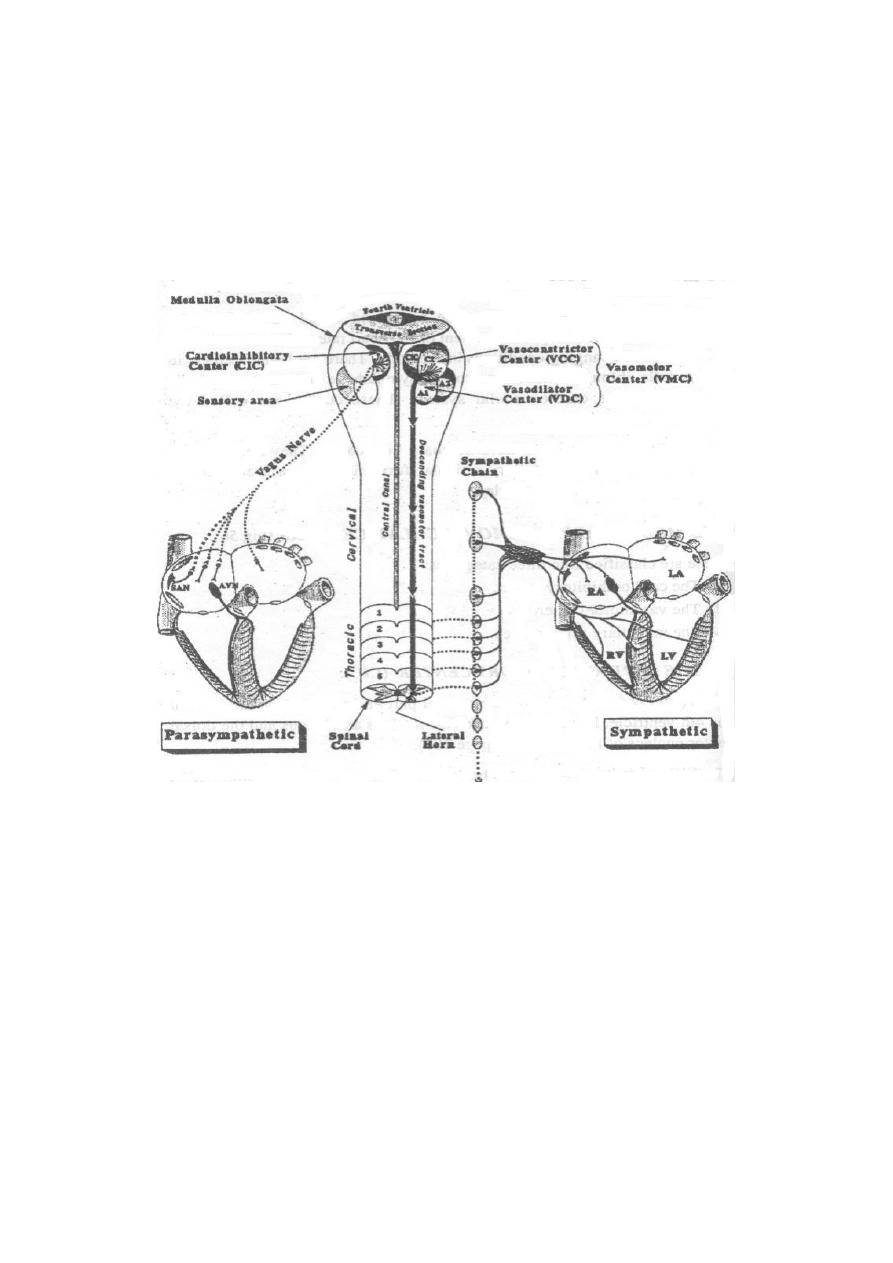
vagus nerves to the heart to decrease the heart rate.
Therefore, the vasomotor center can either increase or decrease heart
activity.
Cardioinhibitory center:
This includes mainly the dorsal motor nucleus of the vagus (plus parts of
the nucleus ambiguus and nucleus of tractus solitarius). It sends
inhibitory signals to the heart via the vagus nerve.
Innervation of the heart:
The heart receives sympathetic and parasympathetic nerve supply. The
sympathetic nerve supply to the heart is connected to, and controlled by,
the vasoconstrictor center. The parasympathetic vagal supply
to the
heart is connected to, and controlled by, the cardioinhibitory center.
There are also afferent nerve fibers from the heart join the sympathetic
and parasympathetic nerves to the CNS.
The sympathetic cardiac nerves
The preganglionic fibers arise from the lateral horn cells of the upper
five thoracic spinal segments. They relay in the three cervical and upper
five thoracic sympathetic ganglia. Postganglionic fibers arise from the
cervical and thoracic ganglia and proceed to supply the atria, ventricles,
and the conducting system of the heart.
The parasympathetic cardiac nerves
The preganglionic fibers arise from the cardioinhibitory center in the
medulla. The fibers proceed as vagal fibers to relay in terminal ganglia
in the wall of the atria. Short postganglionic fibers arise from terminal
ganglia & proceed to supply the atria, SA node, & AV node, but the
ventricles are not supplied by vagus nerve.

Innervation of the blood vessels:
The vessels which are most affected by the vasoconstrictor nerve fibers
are:
The high resistance vessels (the arterioles).
The capacitance vessels (mainly the big veins).
The vessels constrict when the sympathetic discharge to them increases
and dilate when the sympathetic discharge decreases.
The vasoconstrictor nerves
All the blood vessels of the body except the capillaries are supplied with
sympathetic vasoconstrictor fibers. These fibers are connected with, and
under control of, the medullary vasoconstrictor center. The chemical
transmitter of all the sympathetic vasoconstrictor fibers is noradrenaline.
It acts on the (alpha);
α
-adrenergic receptors on the smooth muscles of
the blood vessels leading to their constriction.
The vasodilator nerves
The vasodilator nerves include sympathetic, parasympathetic, and
somatic nerves. None of them is under the control of the vasomotor
center.
A- The sympathetic vasodilator system
These are sympathetic vasodilator cholinergic nerves which supply the
blood vessels of skeletal muscle. The activity of this system is
centrally controlled by the motor cerebral cortex in the frontal lobe of
the brain. Descending fibers from the motor cortex proceed
downwards, relay in the anterior hypothalamus and midbrain. Fibers
from the hypothalamus and midbrain descend through the brainstem
without relay, to end on specific lateral horn cells in the spinal cord.
These lateral horn cells send preganglionic fibers which activate the
postganglionic sympathetic vasodilator fibers. Thus, this sympathetic
vasodilator system is not under the control of the vasomotor center. It
helps to increase the blood flow through skeletal muscles during
exercise.
In addition, this system is activated by sudden strong emotions which
may lead to widespread vasodilation → severe hypotension → brain
ischemia → syncope (transient loss of consciousness).
Other sympathetic cholinergic vasodilator fibers are those which
supply sweat glands. Their activity is controlled by the heat loss center
in the anterior hypothalamus. Another example of sympathetic
cholinergic fibers is those which supply piloerector muscles of the
hairs.
B- The parasympathetic vasodilator system
All parasympathetic nerves contain vasodilator fibers except the
oculomotor nerve. The vasodilator fibers in the vagus are generally
weak, but parasympathetic stimulation has almost no effects on most
blood vessels.
C- The somatic vasodilator fibers
These are fibers of the cutaneous pain-conducting nerves. They are
short branches which emerge from the main-stem nerve fibers near
their termination in the skin. They supply the cutaneous blood vessels.
Their chemical transmitter is substance P which is a strong
vasodilator.
The resting tones to the heart:
The VCC and CIC are normally continuously active during rest leading to
tonic discharge to the heart known as the sympathetic and vagal tones
respectively.
*
The resting sympathetic tone to the heart
This is positively inotropic (increasing the ventricular pumping power 20-
25 %) and positively chronotropic (tending to increase the heart rate to
about 120 beats /minute). However, the chronotropic effect is
antagonized by the stronger vagal tone. So blocking the sympathetic
activity reduces the ventricular pumping power only but doesn't decrease
the normal heart rate.
*
The resting parasympathetic tone to the heart (vagal tone)
The inhibitory vagal tone is the continuous discharge of impulses in the
vagus nerves at the SA node during rest, reducing its rhythmicity;
decreasing the heart rate to about 72 beats/min. which is well below the
inherent rate of SA node rate that is of 100 beats/minute. It doesn't affect
the ventricular pumping power (because the vagi don't supply the
ventricles). Thus, vagotomy increases the heart rate to about 120 beats
per minute (because of the dominance of sympathetic tone). In other
words, in resting state, there is more parasympathetic activity (vagal tone)
to the heart than sympathetic, so the normal resting heart rate is of 72
beats/minute.
Vasomotor tone: (the resting tone to the blood vessel)
Under normal conditions, the vasoconstrictor area of the vasomotor
center transmits a continuous discharge of impulses to the vasoconstrictor
neurons in the lateral horn of the spinal cord and in turn to the
sympathetic vasoconstrictor nerve fibers, maintaining a partial state of
contraction in the blood vessels, keeping the normal level of arterial
pressure.

>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>
>>>>>>>>>
