
3
16
Lect. 9
The heart rate
Objectives:
1. Define heart rate.
2. Summarize the factors that regulate heart rate.
The heart rate refers to the ventricular rate of beating per min. It can be determined
by counting the arterial radial pulse, the heart sounds (using the stethoscope) or the
number of cycles in an ECG record /minute. Normally, it averages 72 beats/minute
(range 60-100 beats/minute) in young adult males during rest. Heart rate higher than
100 beats/minute is called tachycardia and a rate lower than 60 beats/minute is
called bradycardia. Mechanisms that affect the cardiac rate are said to have a
chronotropic effect (chrono = time). Those that increase cardiac rate have a positive
(+ve) chronotropic effect (B
2
agonists (Salbutamol;Ventolin)); those that decrease the
rate have a negative (-ve) chronotropic effect (B blockers (Propranolol; Inderal).
The heart rate is basically determined by the strength of the vagal tone, and is
normally subjected to many physiological variations such as:
It is about 120 beats/minute in newly born infants (due to absence of the vagal
tone) then it decreases to about 72 beats/minute at the age of 20 years.
It is more in females than in males (due to less vagal tone in females).
It is slowest in athletes (due to a stronger vagal tone than in sedentary persons).
It sometimes shows diurnal variations (being lowest in the early morning).
Regulation of the heart rate:
The heart rate is regulated (SA node discharge) by the following factors:
SA node activity.
Chemical.
Neural.
3
2
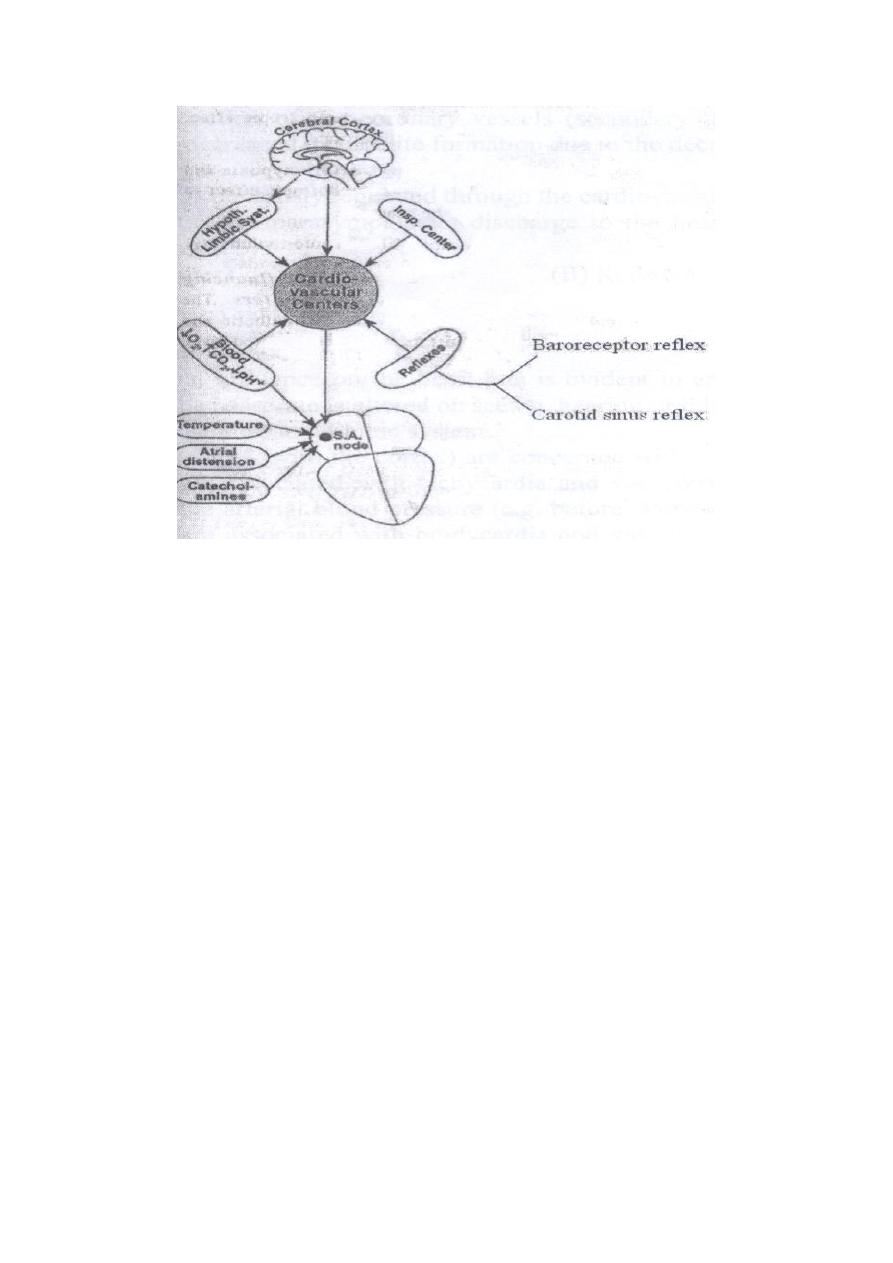
Figure: Factors that influence the heart rate.
Nervous regulation of the heart rate:
The heart receives both sympathetic and parasympathetic (vagal) nerves. Activity in
the sympathetic nerves increases the heart rate, while activity in the parasympathetic
nerves decreases the heart rate.
Functions of the cardiac sympathetic nerves
The sympathetic nerves supply all parts of the heart (atria, ventricles, conduction
system and the coronary vessels). When activated, they lead to the following:
A- An increase in:
1. Heart rate (+ve chronotropic effect).
2. Contractility (+ve inotropic effect).
3. Excitability (causing extrasystole or paroxysmal tachycardia)
4. Conductivity (thus decreasing the AV nodal delay).
B- An increase of the cardiac output.
C- Vasodilation of the coronary vessels (by the effect of the metabolites formed as
a result of the increased myocardial activity).
Functions of the cardiac parasympathetic nerves
They supply atria, SA & AV nodes and coronary vessels but not the ventricles. When
activated, they lead to depression of all cardiac properties, resulting in a decrease of:
- Rhythmicity i.e. the heart rate (-ve chronotropic effect).
- Atrial contractility (-ve inotropic effect).
- Atrial excitability (terminate an attacks of atrial tachycardia or extrasystole).
- Conductivity (prolongs AV nodal delay).
2- A decrease of the cardiac output.
3- Vasoconstriction of the coronary vessels (secondary to decreased metabolite
formation due to the decreased cardiac activity).

3
3
The heart rate is nervously regulated through the cardiovascular centers which control
the sympathetic and parasympathetic discharge to the heart. The activity of these
centers is affected by:
A- Higher centers.
B- Reflexes.
3
2
Higher centers:
(1) The cerebral cortex. Cortical influence on heart rate is evident in
emotions (the heart rate is altered on seeing, hearing or thinking of a
certain event).
(2) The hypothalamus and limbic system. These structures (with the
cortex) are concerned with emotional reactions. Most emotions are
associated with tachycardia and vasoconstriction which increases the
arterial blood pressure (ABP), (e.g. before starting a race, or examination)
but some are associated with bradycardia and vasodilation which
decreases the ABP (e.g. when hearing shocking news).
(3) The respiratory center. Respiratory sinus arrhythmia; this term refers
to the increase of the heart rate during inspiration and to the decrease of
heart rate during expiration that occurs normally in young subjects and
children. The tachycardia that occurs during inspiration is due to;
excitation of the vasoconstrictor center (VCC) by the inspiratory center,
and Bainbridge reflex which is initiated during inspiration by rise of the
right atrial pressure as a result of increase of the venous return.
Reflexes:
Bainbridge reflex (atrial stretch reflex)
An increase in the right atrial pressure or increased distention of the right
atrium leads to heart acceleration. Impulses are discharged mostly from
atrial receptors via afferent nerve fibers to the medullary VCC leading to
reflex increase in sympathetic tone to the heart, increasing the heart rate.
Baroreceptor reflex
This reflex is initiated by stretch receptors, which are located in the
carotid sinus and aortic arch. They are stimulated when stretched; signals
from the carotid arteries are transmitted through the glossopharyngeal
nerves while signals from the arch of aorta are transmitted through the
vagus nerves into; the cardiovascular centers.
The baroreceptor signals inhibit the vasoconstrictor center and excite the
vagal center (CIC) resulting in vasodilation, decreased heart rate. In other
words, a rise in arterial blood pressure produces reflex decrease in heart
rate whereas a fall in arterial blood pressure produces reflex increase in
heart rate.
The carotid sinus reflex
An external pressure on the carotid sinus area (behind the angle of the
mandible) produces reflex slowing of the heart rate and peripheral
vasodilation. The applied external pressure stimulate the baroreceptors in
the carotid sinus which leads to reflex increase in the vagal tone to the
heart (bradycardia) and decrease in the sympathetic vasoconstrictor tone
(vasodilation). On the same basis, an attack of paroxysmal atrial (but not
ventricular) tachycardia can be terminated by initiating a carotid sinus

3
3
reflex, through external massaging of the carotid sinus. A strong blow on
the carotid sinus area could lead to complete cardiac arrest. Some
individuals pathologically have an abnormal hypersensitivity of the
carotid sinus. Thus, mild pressure on the carotid sinus area e.g. during
shaving or by a tight collar, produces bradycardia and generalized
vasodilation, which may markedly decrease the cardiac output and
arterial blood pressure resulting in brain ischemia and fainting. Such
cases can be treated by anticholinergic drugs (Atropine) to block the
vagal discharge to the heart.
Chemical regulation of the heart rate:
A- Effect of changes in blood gases.
Hypoxia.
Hypercapnia and acidosis.
Hypoxia:
Moderate hypoxia (O
2
lack) increases the heart rate by 3 mechanisms:
Direct mechanism (by stimulating the SA node pacemaker cells).
Central mechanism (by inhibiting the CIC).
Reflex mechanism (by stimulating the VCC through exciting the
peripheral chemoreceptors in the carotid and aortic bodies.
On the other hand, severe hypoxia causes reduction of the heart rate due
to inhibition of the SA node activity and paralysis of the medullary
cardiovascular centers.
Hypercapnia and acidosis:
A moderate hypercapnia (CO
2
excess) and acidosis (increased H
+
ion
concentration) increase the heart rate by the following mechanisms:
Inhibition of the CIC.
Stimulation of the VCC through exciting the peripheral chemo-
receptors.
Stimulation of the VCC through exciting the central
chemoreceptors.
On the other hand, severe hypercapnia or acidosis decreases the heart rate
due to inhibition of SA node activity and paralysis of medullary
cardiovascular centers.
B- Effects of hormones, drugs and chemicals:
Adrenaline; Small doses increase the heart rate by a direct action
on the beta one (B
1
) receptors in the SA node.
Thyroxine: This increases the heart rate by direct stimulation of the
SA node and increasing its sensitivity to catecholamines.
Atropine: This accelerates the heart by blocking parasympathetic
3
4
activity.
Histamine: This is a potent vasodilator (VD) substance which leads
to marked drop of the ABP, resulting in heart acceleration.
Bile salts: inhibit SA node activity & stimulate the CIC leading to
bradycardia.
Autonomic drugs: Sympathomimetic drugs (amphetamine) cause
tachycardia while parasympathomimetic drugs (acetylcholine)
cause bradycardia.
SA node activity:
Factors that directly affect the SA node activity:
Body temperature; (physical factors) An increase of the body
temperature by 1 °C increases the heart rate by 10-20 beats/minute
and vice versa.
Mechanical factors; Right atrial distension may directly excite the
SA node leading to tachycardia.
Chemical factors; The SA node is directly excited by mild
hypoxia, Catecholamines, thyroxine, while it is directly inhibited
by severe hypoxia and hypercapnia, bile salts, and cholinergic
drugs.
Thyroid hormones (T
3
, T
4
) again have direct action on SA node.
Increases in the level of circulating thyroid hormones increases the
rate at which SA node beats e.g., in case of Thyroitoxicosis
disease, there is an increase in heart rate, (resting tachycardia; HR
> 100 beats/minute).
>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>>
>>>>>>>>
