1
Physiology
Dr. Basim Mohamad Alwan Lecture (5)
PAIN
Pain
is an
unpleasant sensation produced by damage or impending damage
of tissues.
It is a specific sensation produced by stimulation of specific pain
receptors (nociceptors). It is not due to overstimulation of other receptors as
mechano or thermoreceptors as was believed before.
This is proved by:
1. Pain can be dissociated from other sensations; as in syringomyelia
(saccular dilation of the spinal central canal) pain and temperature sensations
disappear from the affected areas but other sensations persist.
2. Some areas do not contain pain receptors and are insensitive to pain
(the center of the cornea, the inside of the cheek opposite the second molar
tooth); these areas are sensitive to other sensations but not pain.
3. In tabes dorsalis, all sensations may disappear except pain.
4. The analgesic drugs suppress pain only but not other sensations.
CHARACTERISTICS OF PAIN SENSATION
Pain has the following characteristic:
1. Widespread distribution: Pain receptors are present almost everywhere in
the body. It is most abundant in the skin.
2. High threshold of stimulation: The stimuli used to produce pain sensation
(noxious stimuli) are of high energy that causes damage of the tissues.
3. It is produced by a variety of stimuli; mechanical, thermal or chemical.
4. It is a non-adapting sensation; pain sensation persists so long as the noxious
stimulus is applied, the sensation of pain might even increase.
2
5. It produces prepotent withdrawal reflexes; a prepotent reflex is a reflex
that takes priority over any other reflex occurring at the same time. Swinging of
the arms is an automatic reflex that occurs during walking so if during walking
a noxious stimulus is applied to the arm, swinging stops and the arm is rapidly
withdrawn away from the stimulus.
6. It is the only sensation which produces an unpleasant "affect" without
any previous learning or experience. The pleasantness or unpleasantness of
other sensations are conditioned and depend on previous learning and
experience. Only pain has a "built-in" unpleasant affect.
Prefrontal lobotomy (an operation to cut the deep connections of the frontal
lobes with the rest of the brain) abolishes this affect. After this operation, the
patient feels the pain, but it does not bother him.
7. It can be perceived at the thalamus. The cerebral cortex is not essential for
the perception of the slow type of pain.
PAIN RECEPTORS
There are three types of pain receptors:
1. Mechanosensitive pain receptors: Which are stimulated by strong
mechanical stimuli?
2. Thermosensitive pain receptors: Which are stimulated by temperatures
below 10 or above 50°C.?
3. Chemosensitive pain receptors: Which are stimulated by chemicals like P-
factor, bradykinin, lactic acid and potassium ions?
All these receptors are naked free nerve endings.
TYPES OF PAIN ACCORDING TO ITS SITE OF ORIGIN
According to the site of its origin, pain is classified into three types:
I. CUTANEOUS PAIN: Which arises from the skin and is transmitted by
cutaneous somatic nerves?
3
II. DEEP PAIN: Which arises from deep structures like muscles, tendons,
ligaments, periosteum, and is transmitted by deep somatic nerves?
III. VISCERAL PAIN: Which arises from viscera like the heart, the kidney and
the intestine, and is transmitted by the visceral afferent fibers in the
autonomic nerves?
TYPES OF PAIN ACCORDING TO THE SPEED OF ITS
CONDUCTION
Pain is conducted by either type III (A-delta) or type IV (C) sensory nerve
fibers. Accordingly, there are two types of pain; fast pain which is conducted
by type III fibers, and slow pain which is conducted by type IV fibers. They
differ widely in their properties and characteristics.
On application of a noxious mechanical stimulus to the skin (a pinprick on the
foot), one first feels a bright, sharp, localized pain of very short duration
(less than one second). This is the fast pain, which is also called "pricking
pain". This pain is produced by stimulation of the mechanosensitive pain
receptors. Shortly after feeling the pricking pain, one feels a dull, intense, burning,
diffuse pain of longer duration (few sec. - few min.). This is the slow pain,
which is also called "burning pain" or "aching pain". This pain is produced by
stimulation of the chemosensitive pain receptors.
CHARACTERISTICS OF FAST PAIN
1. It is only cutaneous.
2. It is conducted by type-Ill fibers (speed: 6-30 m/s)
3. It is felt immediately after application of the stimulus (0.1 second after
application of the stimulus).
4. It is of very short duration.
5. It is bright and sharp.
6. It is well localized.
4
7. It is perceived only by the sensory cerebral cortex.
8. It is conducted by the neospinothalamic sensory pathway.
CHARACTERISTICS OF SLOW PAIN
1. It can be cutaneous, deep or visceral.
2. It is transmitted by the slowly conducting type-IV fibers (speed: 0.5-2 m/s).
3. It starts about one second after application of the stimulus.
4. It lasts for a long time.
5. It is dull, aching (or burning).
6. It is diffuse and poorly localized.
7. It can be perceived at the level of the thalamus; the cerebral cortex is not
essential for its perception.
8. It is conducted by the paleospinothalamic sensory pathway.
DISSOCIATION OF FAST AND SLOW PAIN
One type of pain may disappear leaving the other intact, as in the following
conditions:
1. Compression or hypoxia of a nerve abolishes the conduction of fast pain
but leaves slow pain. This is because hypoxia affects the thick type-Ill nerve
fibers first
2. Mild local anesthesia (local low dose of cocaine) abolishes the conduction of
slow pain but leaves fast pain. This is because mild anesthesia affects the thin
type-IV nerve fibers first
I- CUTANEOUS PAIN
Cutaneous pain arises from the skin on application of a noxious stimulus. It is
conducted by somatic cutaneous nerves and is not referred to any other part. It
is usually accompanied by sympathetic reflexes (increase in heart rate and rise in
arterial blood pressure), but there is no reflex muscular rigidity. Cutaneous pain
could be of the fast "pricking" type or of the slow "burning" type.
5
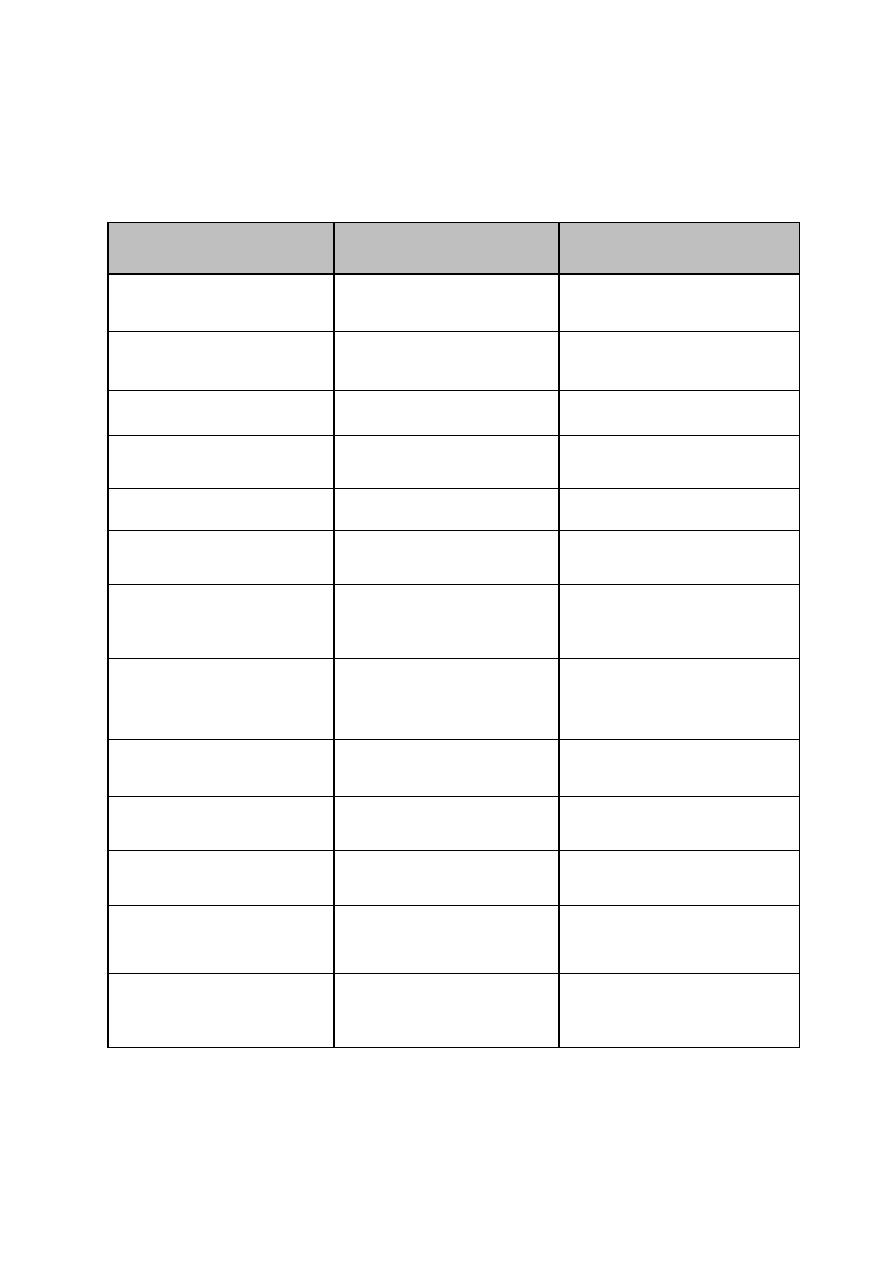
Table 8-1:
Differences between, fast and slow pain.
CRITERION
FAST PAIN
SLOW PAIN
1. Site of origin
only cutaneous
cutaneous, deep or visceral
2. Time of perception
0.1 sec. after the stimulus
1 sec. after the stimulus
3. Characteristics
bright, sharp & localized
dull, intense and diffuse
4. Duration
Very short (less than 1
sec.)
Longer (few sec – few
min.)
5. Conducting nerves
type-III fibers
type-IV fibers
6. Sensory pathway
neospinothalamic
pathway
paleospinothalamic
pathway
7. Associated reflexes
rapid, protective
withdrawal reflexes
slower autonomic
reflexes (e.g. increase in
heart rate & ABP)
8. Abolished by
hypoxia or pressure on
the nerve
mild local anesthesia
(low dose of local cocaine)
9. Center of perception
cerebral cortex
thalamus
10. Relay in dorsal horn
laminae II & V
laminae II & III
11.Relay nuclei in the
thalamus
VPLN
ILN
12.Relay in reticular
formation
no relay
relay
13.Final destination in
CNS
sensory cerebral cortex
all areas of the cerebral
cortex.
6
11 - DEEP PAIN
Deep pain is a slow type of pain which arises from deep structures; i.e. muscles,
tendons, ligaments and periosteum. It is conducted by deep somatic nerves and
is referred to any other part.
CHARACTERISTICS OF DEEP PAIN
1. It is dull, aching, diffuse and poorly localized.
2. Usually associated with nausea, sweating and hypotension.
3. Pain from tendons, ligaments and periosteum initiates reflex muscular
spasm in the nearby muscles.
4. It is conducted by the slowly conducting type-IV fibers.
5. It may be referred to the skin of the same dermatome.
CAUSES OF DEEP PAIN
1. Ischemia of skeletal muscles: This leads to the release and accumulation of
P-factor (Lewis pain-producing factor). The nature of this factor is not
exactly known, but it could be bradykinin, histamine, proteolytic enzymes,
lactic acid or potassium ions or a collection of all these substances.
P-factor directly stimulates the chemosensitive pain receptors, but it also
facilitates the mechanosensitive and thermosensitive pain receptors.
Prostaglandins are released from damaged and inflamed tissues. They facilitate
but do not stimulate pain receptors. So they produce tenderness of the affected
area.
INTERMITTENT CLAUDICATIONS (LAMENESS OR LIMPING):
This disease is an example where there is severe ischemic pain in the muscles of
the lower limb. In this condition, there is narrowing of blood vessels of the lower
limbs (following vascular inflammation or severe atherosclerosis). The slightest
exercise leads to accumulation of the P-factor and pain sensation then limping. . During
rest", there is no. pain as there is no accumulation of the P-factor.
2. Muscular spasm (cramp): In tetany or when one loses a lot of salt in sweating
7
(muscular exercise in hot weather or miner's disease) muscle spasm (cramp)
occurs and stimulation of mechanosensitive pain receptors then pain sensation.
Ischemia also contributes to the production of pain in this condition.
3. Bone injury: It is painful because of the chemical and mechanical irritation of
the overlying periosteum. Bone itself is insensitive to pain.
4. Inflammation of joints: It is painful due to chemical and mechanical irritation
of the surrounding tendons and ligaments.
III - VISCERAL PAIN
Visceral pain is a slow type of pain that arises from the viscera. It is carried by
the visceral afferent type-IV slow conducting nerve fibers. Some regions are
insensitive to pain as the liver parenchyma and lung alveoli.
CHARACTERISTICS OF VISCERAL PAIN
1. It is diffuse, dull or colicky.
2. It is a slow pain, carried by the slowly conducting type-IV fibers.
3. It is poorly localized.
4. It may be referred to the skin or other deep structures.
5. It is associated with:
(a) Autonomic reflexes: Nausea; vomiting, sweating and bradycardia. That is why
visceral pain is said to be "sickening".
(b) Somatic reflexes: Rigidity of the overlying skeletal muscles; e.g. the rigidity
of muscles over the inflamed appendix (guarding rigidity).
(c) Cutaneous hyperalgesia: Increased pain sensibility in the skin of the same
dermatome.
(d) Strong emotional affect: With depression, malaise and bad mood.
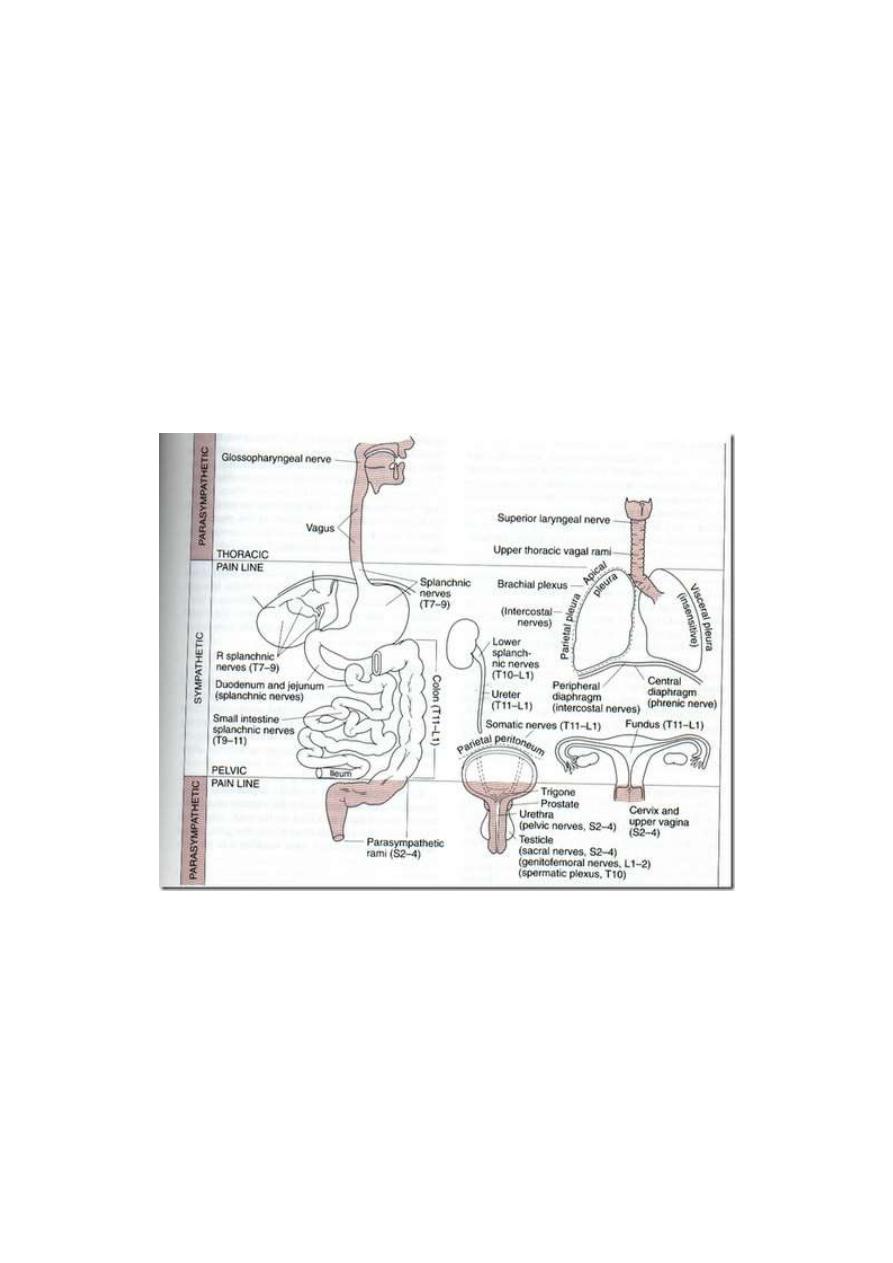
NERVES CONDUCTING VISCERAL PAIN
Visceral pain is conducted via afferent visceral fibers in the autonomic nerves
(fig. 8-1). Somatic nerves conduct pain from some parts of the viscera.
8
VISCERAL PAIN CONDUCTED BY SYMPATHETIC NERVES
Afferent fibers that run with sympathetic nerves conduct pain from the thoracic and
abdominal viscera, the urinary bladder, uterus and uterine tubes.
VISCERAL PAIN CONDUCTED BY PARASYMPATHETIC NERVES
• With glossopharyngeal and vagus nerves (Cr. IX and X nerves):
Pain from pharynx, trachea and upper part of the esophagus
• With the pelvic nerve (S 2, 3 & 4): Pain from sigmoid colon,
rectum, the trigone of the bladder and the genital organs.
Figure 8 -1: The areas from which pain is conducted by somatic and by autonomic nerves.
VISCERAL PAIN CONDUCTED BY SOMATIC NERVES
Thoracic intercostal nerves carry pain sensations from parietal pleura, parietal
pericardium and parietal peritoneum. This pain is called "parietal pain". It is
well localized.
9
CAUSES OF VISCERAL PAIN
1. Ischemia: Ischemic pain is due to accumulation of the P-factor which
stimulates the chemosensitive pain receptors, e.g. anginal pain.
2. Spasm of a hollow viscus: Spasmodic pain is colicky pain caused mainly by
stimulation of the mechanosensitive pain receptors. Ischemia due to squeezing
of blood vessels may contribute to pain production, e.g. intestinal, renal or
biliary colic.
3. Over distention of a hollow viscus: Overstretch of the tissues stimulates
mechanosensitive pain receptors. Ischemia may contribute, e.g. over distention
of the intestine by large volumes of gases.
4. Chemical irritation: Chemical irritants produce pain by stimulating chemo
sensitive pain receptors as in rupture of a peptic ulcer could lead to leak of the
highly acidic gastric juice into the peritoneum leading to severe abdominal pain.
5. Traction on the mesentery: E.g. by an abdominal tumor. This cause is rare
and of little clinical significance.
REFERRED PAIN
Referred pain is pain felt away from its site of origin.
Examples:
1. Ischemia of the heart causes pain that may be referred and felt in the left
shoulder and the inside of the left arm.
2. Pain from the gall bladder may be referred and felt in the right shoulder.
3. Pain of appendicitis may be referred to the umbilical area.
4. Pain from the ureter may be referred to the testis.
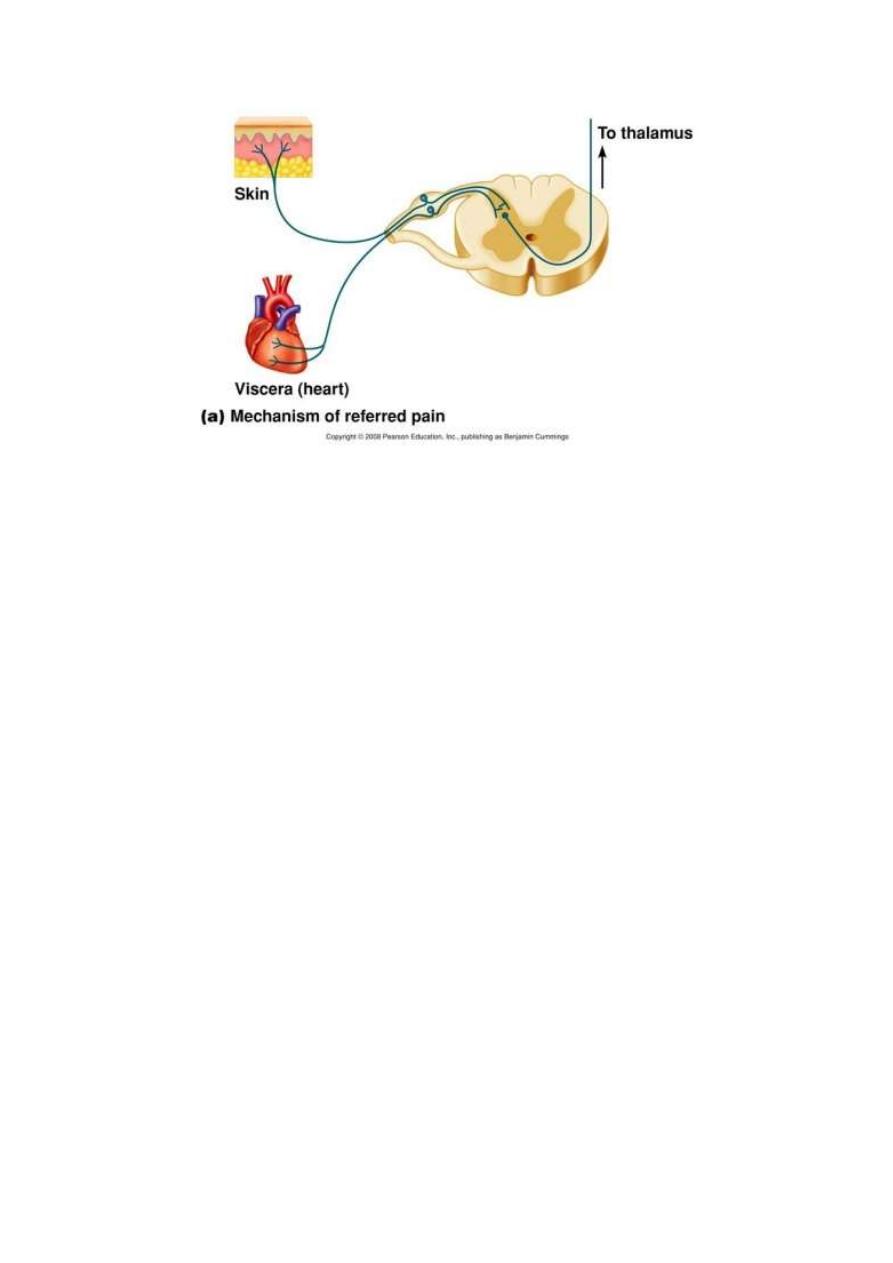
MECHANISM OF REFERRED PAIN (Convergence Projection mechanism):
Afferent pain-conducting fibers from viscera converge with afferent pain-
conducting fibers from skin on one central neuron of the paleospinothalamic
tract.
10
Figure 5-2: The convergence projection mechanism of referred pain.
In this way, pain impulses from the viscera travel in the same central pathway
as pain impulses from the skin to reach the same final sensory neuron in the
brain. The final sensory neuron projects pain sensation to the skin, as the skin is
the place from which it usually receives pain signals (fig. 5-2).
This means that the pain signals from the viscera converge to the same final
sensory neuron as the signals from the skin, the brain projects any pain
sensation from the viscera to the skin. This mechanism is known as "the
convergence projection mechanism".
Accordingly, if pain arises from a certain viscera from which impulses
converge with impulses coming from a certain area of skin, one would feel pain
as if it is coming from the skin not from the viscera.
Reference of pain occurs from viscera to deep structures or the skin and from
deep structures to the skin, but not the opposite way.
DERMATOMAL RULE OF REFERRED PAIN
Visceral or deep pain is referred to the dermatome which has the same nerve
supply as the site of pain, as the heart, the left shoulder and the inside of the left
arm have the same nerve supply.
11
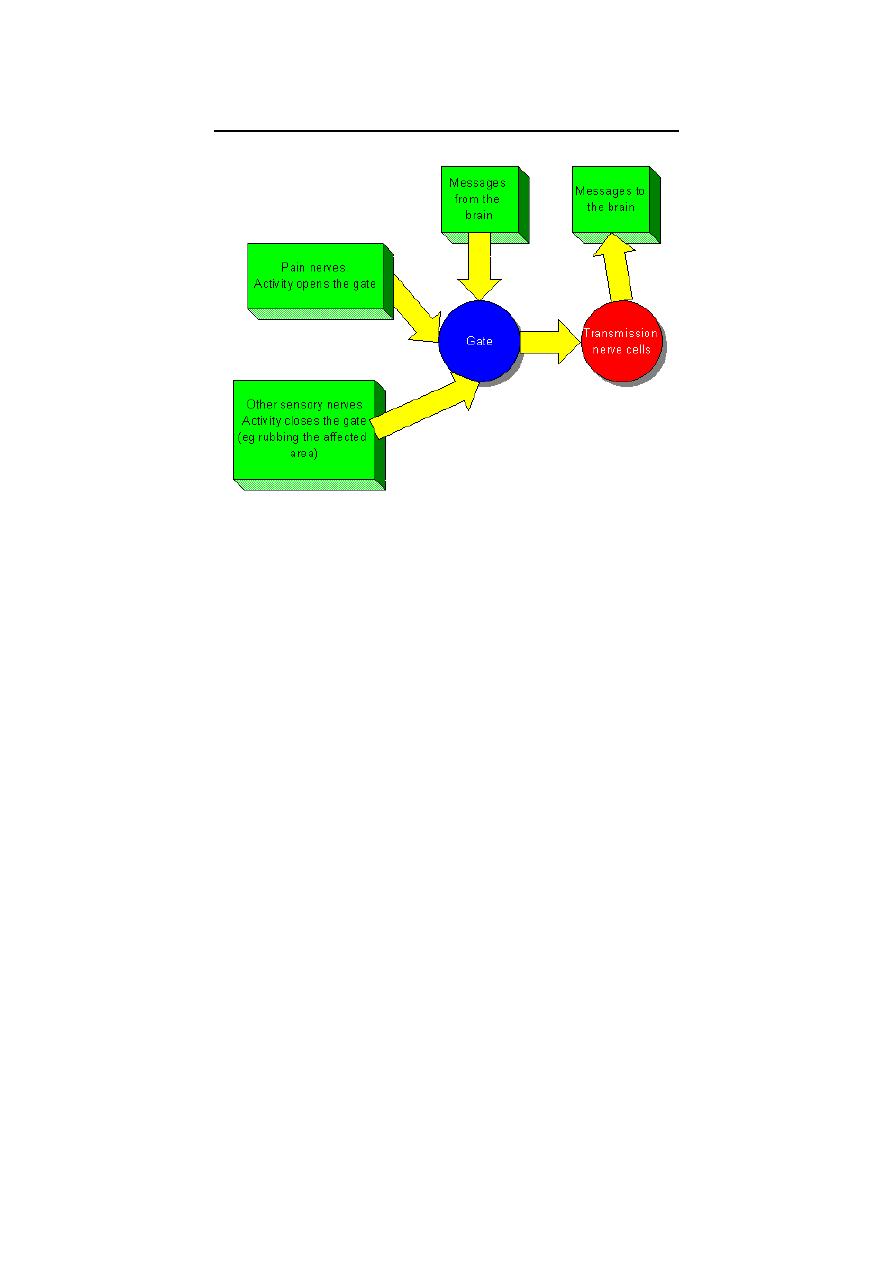
THE GATE THEORY OF PAIN TRANSMISSION
This theory proposed by Melzack and Wall in the 1960's. This theory states that
the dorsal horn of the spinal gray matter at the substantia gelatinosa of Rolandi
is the site of first relay in the sensory pathway of pain. At this level, there is a
group of inhibitory, enkephalinergic interneurons which form the "Pain.
Inhibitory Complex, (PIC). When stimulated, these interneuron's block the
transmission of pain sensation by presynaptic inhibition of the primary pain-
conducting fibers. At the dorsal horn also, transmission of pain sensation could
be facilitated in cases of secondary hyperalgesia. In this way, the dorsal horn
acts as a "gate" that may pass, facilitate or block pain transmission.
Accordingly, the dorsal horn of the spinal gray matter is sometimes referred to
as the "gate" for pain transmission.
The same "gating" mechanism for pain is found also at the thalamus where
pain signals could be blocked by corticofugal fibers or facilitated by
intralaminar thalamic nuclei. In this way, the thalamus acts as a secondary gate
for pain transmission.
A 3
rd
gate may also be located in the reticular formation which can be
considered as tertiary gate.

12
