
1
Physiology
Dr. Basim Mohamad Alwan
Lecture (6)
INTERINSIC
MODIFICATION OF PAIN SENSIBILITY
Intrinsic mechanisms can modify pain sensation leading to either
exaggerated or suppressed pain sensibility.
I. EXAGGERATED PAIN SENSIBILITY
1. CUTANEOUS HYPERALGESIA
This is a pathological condition where pain sensibility from the skin is
exaggerated. It usually follows a skin injury or inflammation.
There are two types of cutaneous hyperalgesia:
A. PRIMARY HYPERALGESIA
In this case, the threshold of pain sensation from the affected area is lowered.
A stimulus which normally produces mild pain causes prolonged severe
pain. Primary hyperalgesia occurs in conditions like sunburns. It is
restricted to the affected area of skin and the area of hyperemia around it
(Spreading flare). This type of hyperalgesia is caused by facilitation of
pain receptors by substances released from the damaged or inflamed tissues
(histamine, bradykinin, substance-P, prostaglandins).
ALLODYNIA
is a severe type of primary hyperalgesia in which a gentle
stimulus like a breeze or the touch of clothes produces very severe pain.
B. SECONDARY HYPERALGESIA (HYPERPATHIA)
In this case, the threshold of pain is increased, but when the threshold is
reached it produces severe burning pain. It occurs in a normal skin area that
extends beyond the spreading flare of the injured skin. Secondary hyperalgesia
is produced by Convergence-Facilitation Mechanism (Fig. 6-1).

2
Figure 6-1: The convergence facilitation mechanism of secondary hyperalgesia.
Impulses from the injured area facilitate a central neuron. Impulses from
the hyperpathic area converge on the same central neuron. The
convergence on a central facilitated neuron explains the exaggerated pain
sensibility. The facilitator neuron which arises from the area of primary
hyperalgesia exerts lateral inhibition on the stimulator neuron which
arises from the hyperpathic area. This explains why the threshold of pain
is increased in the hyperpathic area.
2. CAUSALGIA (Complex Regional Pain Syndrom: CRPS)
Causalgia is a pathological condition in which there is hyperalgesia,
allodynia and spontaneous burning pain sensation long after a
seemingly trivial tissue injury or nerve injury. The skin in the affected
area becomes thin and shiny with increased nail and hair growth.
THE MECHANISM OF
CAUSALGIA:
Nerve injury leads to sprouting of noradrenergic sympathetic nerve fibers
into the sensory nerve track up to the dorsal root ganglia of the sensory

3
nerves of the affected area. The dorsal root ganglia cells can be stimulated
by sympathetic activity. This stimulation may facilitate the sensory neuron
leading to hyperalgesia or allodynia, or it may excite it to discharge pain
signals to the CNS leading to spontaneous pain sensation.
3. THE THALAMIC SYNDROME
Thalamic syndrome is caused by thrombosis of the thalamogeniculate
artery, a branch of the posterior cerebral artery. At first, all sensations
are lost on the opposite side. Few weeks later, pain sensibility is regained.
A noxious stimulus produces very severe, stabbing and extremely unpleasant
pain. This is due to the facilitation of the medial and laminar nuclei of the
thalamus which do not degenerate in this syndrome. They potentiate pain
conducted by the reticular activating system of the brainstem.
II. SUPPRESSED PAIN SENSIBILITY
ANALGESIA
Analgesia means suppression of pain sensation. There is an analgesia
4
system in the body which can suppress pain sensibility by activating the
spinal pain inhibitory complex in the dorsal horn peripherally or the
analgesia system centrally. The analgesia system of the body is divided
into peripheral and central analgesia systems.
THE PERIPHERAL ANALGESIA SYSTEM
The peripheral anesthesia system consists of the type-II sensory nerve
fibers which conduct mechanoreceptive sensations.
Immediately after they enter into the spinal cord, type-II fibers divide into
medial and lateral branches. The medial branch ascends to form the
gracile and cuneate tracts, and the lateral branch stimulates the PIC to
inhibit pain transmission. In this way, pain sensation can be suppressed
by scratching or rubbing of the skin.
Counterirritants which are applied to the skin to suppress pain work on
this principle. They stimulate the cutaneous receptors which send
impulses through type-II fibers that stimulate the PIC. This is also the
basis for acupuncture.
On the same principle, electrodes surgically implanted in the dorsal
column activate the PIC and suppress pain sensibility. They are
sometimes used for treatment of intractable pain.
THE CENTRAL ANALGESIA SYSTEM
This system consists of five components (Fig. 6-2)
1. THE CEREBRAL CORTEX
Many areas of the cerebral cortex, especially the limbic association area,
project corticofugal fibers to:
a. The thalamus; these fibers block pain signals at the level of the
thalamus (the second gate for pain transmission).

5
b. The periaquiductal gray matter of the mesencephalon.
The corticofugal fibers are beta-endorphinergic.
2. THE HYPOTHALAMUS
Beta-endorphinergic fibers project from the periventricular nuclei and
the medial forebrain bundle of the hypothalamus to the periaquiductal
gray matter of the mesencephalon.
3.
THE PERIAQUEDUCTAL GRAY MATTER OF THE MIDBRAIN
Neurons from this area project enkephalinergic fibers to the reticular
formation of the brainstem and the raphe magnus nucleus.
4. THE RETICULAR FORMATION OF THE BRAINSTEM
This structure sends serotonergic descending fibers in the lateral
reticulospinal tract to activate the spinal PIC. It also projects fibers to the
raphe magnus nucleus.
Fig.6-2 the central analgesia system

6
5. THE RAPHE MAGNUS NUCLEUS
The raphe magnus nucleus is found in the lower pons and upper medulla.
Serotonergic nerve fibers descend from this nucleus down in the lateral
reticulospinal tract to activate the spinal PIC.
STRESS ANALGESIA
Stress analgesia is the suppression of pain sensation during stressful
conditions (fight or flight). In these conditions, pain impulses are blocked
at two levels:
A. At the first gate of pain transmission (the dorsal horn of the spinal
gray matter). The hypothalamus and other parts of the central analgesia
system activate the spinal PIC which blocks the transmission of pain
signals at the dorsal horn.
B. At the second gate of pain transmission (the thalamus).
Corticofugal fibers to the thalamus block by presynaptic inhibition the
transmission of pain signals in the thalamus before they reach the cerebral
cortex.

7
THE SOMATOSENSORY CONDUCTING SYSTEMS OF
THE SPINAL CORD
The ascending somatosensory tracts in the spinal cord are classified into
two conducting systems, the anterolateral and the dorsal column-
lemniscal systems. Each system has its own features and characteristics.
THE ANTEROLATERAL SYSTEM
The anterolateral system has two components; the ventral and the lateral
spinothalamic tracts. The fibers of the first order neurons which serve this
system are the slow, thin, myelinated type-III and the nonmyelinated
type-IV fibers.
CHARACTERISTICS OF THE ANTEROLATERAL SYSTEM
1. It is a slowly conducting system made up of thin type-III and IV fibers.
2. It has moderate degree of somatotopic lamination. This allows only
moderate degree of localization and discrimination of its sensations.
3. The intensity discrimination of its sensations is poor. Sensations of this
system can be identified in only 10-20 grades of intensity.
4. It cannot transmit rapidly repetitive signals.
5. It conducts sensations from the contralateral side of the body.
THE DORSAL COLUMN-LEMNISCAL SYSTEM
The dorsal column-lemniscal system has three components; the dorsal column
tracts (gracile and cuneate), the spinocervical tract, and the medial lemniscus.
The fibers of the first order neurons which serve this system are the rapidly
conducting, thick, myelinated, type-I and II fibers.
8
CHARACTERISTICS OF THE DORSAL COLUMN LEMNlSCAL
SYSTEM
1. It is a rapidly conducting system made up of the thick type-I and II
fibers.
2. It has a high degree of somatotopic lamination; i.e. it is arranged in
many laminae, each lamina serves a specific topic on the body surface.
This allows a high degree of localization and discrimination of its
sensations.
3. The intensity discrimination of its sensations is high. Most sensations
in this system can be identified in up to 100 grades of intensities.
4. It can conduct rapidly repetitive signals. This enables this system to
conduct vibration sense.
5. It conducts sensations from the ipsilateral side of the body.
THE ANTEROLATERAL SYSTEM
THE VENTRAL SPINOTHALAMIC PATHWAY
The ventral spinothalamic pathway (Fig. 6-3) is the sensory pathway for
crude touch and pressure, tickle and itch sensations. It has three
orders of neurons:
FIRST ORDER NEURONS:
are the dorsal root neurons. Their afferent fibers (type
III and IV) enter the spinal cord in the dorsal root of the spinal nerve then go
up or down for a few segments in the Lissaur s tract and terminate in
laminae II, III and IV of the dorsal horn of the spinal gray matter.
9
Fig. 6-3
ventral spinothalamic tract
SECOND ORDER NEURONS:
are neurons in laminae II, III and IV of the
dorsal horn. Their fibers cross to the opposite side in front of the central
canal then ascend in the ventral column of the spinal white matter as the
ventral spinothalamic tract up to the brainstem and in the brainstem, they
join the lateral spinothalamic tract to form the spinal lemniscus (nervous
tract made by union of more than one tract) which ascend up to
terminate in the ventral posterolateral nucleus of the thalamus (VPLNT).
THIRD ORDER NEURONS
: are neurons of the VPLNT. Their fibers project
through the central thalamic radiations to the final sensory neurons in the
sensory cerebral cortex.

10
THE LATERAL SPINOTHALAMIC PATHWAYS
There are two lateral spinothalamic pathways; the paleospinothalamic and
the neospinothalamic pathways.
1. THE PALEOSPINOTHALAMIC PATHWAY
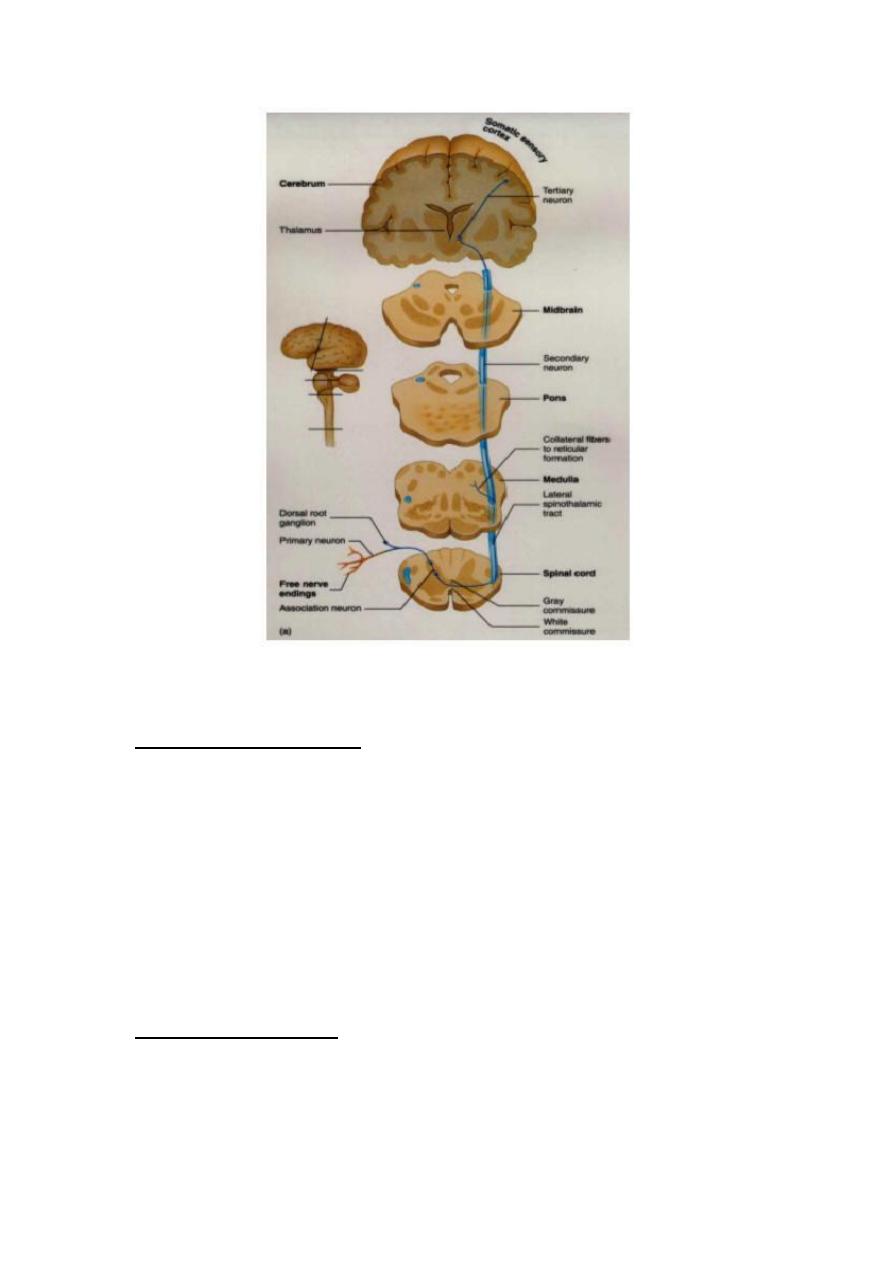
Fig. 6-4 the paleospinothalamic pathway
The paleospinothalamic pathway (fig. 6-4) is the sensory pathway for slow
pain, and temperature sensations (heat).
FIRST ORDER NEURONS:
are the dorsal root neurons. Their afferent fibers (type
IV) enter the spinal cord in the dorsal root of the spinal nerve then go up or
down for a few segments in the Lissaurs tract and terminate in the
substantia gelatinosa of Rolandi (laminae II, III) of the dorsal horn of the
spinal gray matter.
11
SECOND ORDER NEURONS:
are neurons in the substantia gelatenosa of
Rolandi. Their fibers cross in front of the central canal to the opposite
side. Fibers ascend in the anterolateral column of the spinal white matter
as the lateral spinothalamic tract. In the brainstem the lateral
spinothalamic tract joins the ventral spinothalamic tract to form the
spinal lemniscus. Fibers terminate in the nonspecific intralaminar
nuclei of the thalamus (ILNT).
During their course in the brainstem, some fibers deviate and make a
separate tract called "the spinoreticular tract". The fibers of this tract
terminate in the reticular formation of the brainstem. Multiple, short fiber
neurons conduct the signals from the reticular formation onto the
intralaminar nuclei of the thalamus (ILNT).
THIRD ORDER NEURONS
: are neurons of the ILNT. Their fibers project
through the anterior, central and posterior thalamic radiations to the final
sensory neurons in all parts of the cerebral cortex.
2. THE NEOSPINOTHALAMlC PATHWAY
The neospinothalamic pathway (fig. 6-5) is the sensory pathway for fast
pain and temperature (cold).
FIRST ORDER NEURONS:
are the dorsal root neurons. Their afferent fibers
(type III) enter the spinal cord in the dorsal root of the spinal nerve and go
up or down for a few segments in the Lissaur tract then terminate in laminae
II and V of the dorsal horn of the spinal gray matter.
SECOND ORDER NEURONS:
are neurons in laminae, II and V. Their fibers
cross in front of the central canal to the opposite side, and then ascend in

12
the anterolateral column of the spinal white matter as the lateral
spinothalamic tract. In the brainstem, the lateral spinothalamic tract
joins the ventral spinothalamic tract to form the spinal lemniscus. The
fibers of the neospinothalamic tract terminate in the ventral
posterolateral nuclei of the thalamus (VPLNT).
Fig. 6-5 the neospinothalamic pathway
THIRD ORDER NEURONS:
are the neurons of the VPLNT. Their fibers project
through the central thalamic radiations to the final sensory neurons in the
sensory cerebral cortex.
THE DORSAL COLUMN PATHWAY
The dorsal column pathway (the gracile and cuneate pathway) (Fig. 6-6) is the
sensory pathway for fine touch, fine pressure, vibration, stereognosis,
muscle tension and proprioceptive sensations.

13
FIRST ORDER NEURONS:
are the dorsal root neurons. Their afferent fibers
(type II) enter the spinal cord in the dorsal root of the spinal nerve then
branch into medial and lateral branches. The medial branches ascend without
relay up in the ipsilateral dorsal column of the spinal white matter where they
are called "the dorsal column tracts" or "the gracile and cuneate
tracts". They terminate in the dorsal column nuclei (the gracile and
cuneate nuclei) in the medulla.
Fig. 6-6 the dorsal column pathway
SECOND ORDER NEURONS:
are the neurons of the dorsal column nuclei in
the medulla. Their fibers cross to the opposite side in the sensory
decussation and ascend in the brainstem as the medial lemniscus. They
terminate in the ventral posterolateral nucleus of the thalamus
(VPLNT). .

14
THIRD ORDER NEURONS:
are those of the VPLNT. Their fibers project
through the central thalamic radiations to the final sensory neurons in the
sensory cortex.
* The gracile is the medial tract. It is formed in the lower part of the
spinal cord and carries sensations from the lower part of the body. The
cuneate is the lateral tract. It is formed in the upper part of the spinal
cord at the level of the 6th thoracic spinal segment, and carries
sensations from the upper part of the body.
THE SPINOCERVICAL PATHWAY
The spinocervical pathway (Fig. 6-7) is an accessory pathway for the dorsal
column pathway. It conducts impulses at a faster rate. So, impulses in this
pathway reach the cerebral cortex before those conducted by the dorsal
column pathway.
FIRST ORDER NEURONS:
are the dorsal root neurons. Their afferent fibers
(type I and II) enter the spinal cord in the dorsal root of the spinal nerve and
terminate in lamina IV" of the dorsal horn of the spinal gray matter.
SECOND ORDER NEURONS:
are neurons in lamina IV. Their fibers ascend in the
ipsilateral posterolateral column of the spinal white matter as the
spinocervical tract. The fibers terminate in the lateral cervical nucleus
(a longitudinal cell column lateral to the tip of the dorsal horn of the
upper 2-3 cervical segments)
of the same side.
THIRD ORDER NEURONS:
are those of the lateral cervical nucleus. Their
fibers cross to the opposite side and ascend in the brainstem as part of the
medial lemniscus to terminate in the VPLNT.
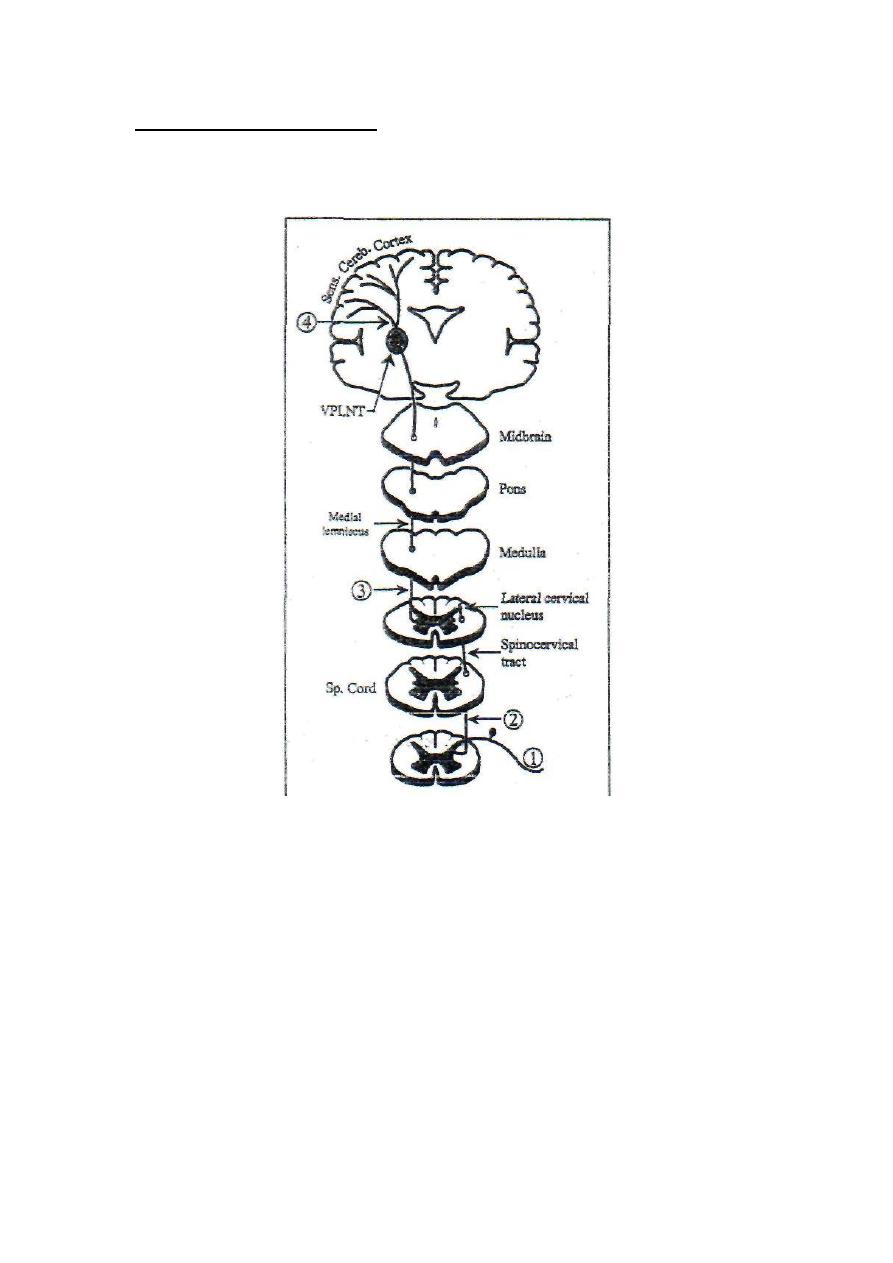
15
FOURTH ORDER NEURONS
: are neurons of the VPLNT. Their fibers
project through the central thalamic radiations to the final sensory
neurons in the sensory cerebral cortex.
Fig. 6-7 the spinocervical pathway
