Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
1
Reproductive and Hormonal Functions of the
Male:
The reproductive functions of the male can be divided into
three major subdivisions: (1) spermatogenesis, which means
simply the formation of sperm; (2) performance of the male
sexual act; and (3) regulation of male reproductive functions by
the various hormones.
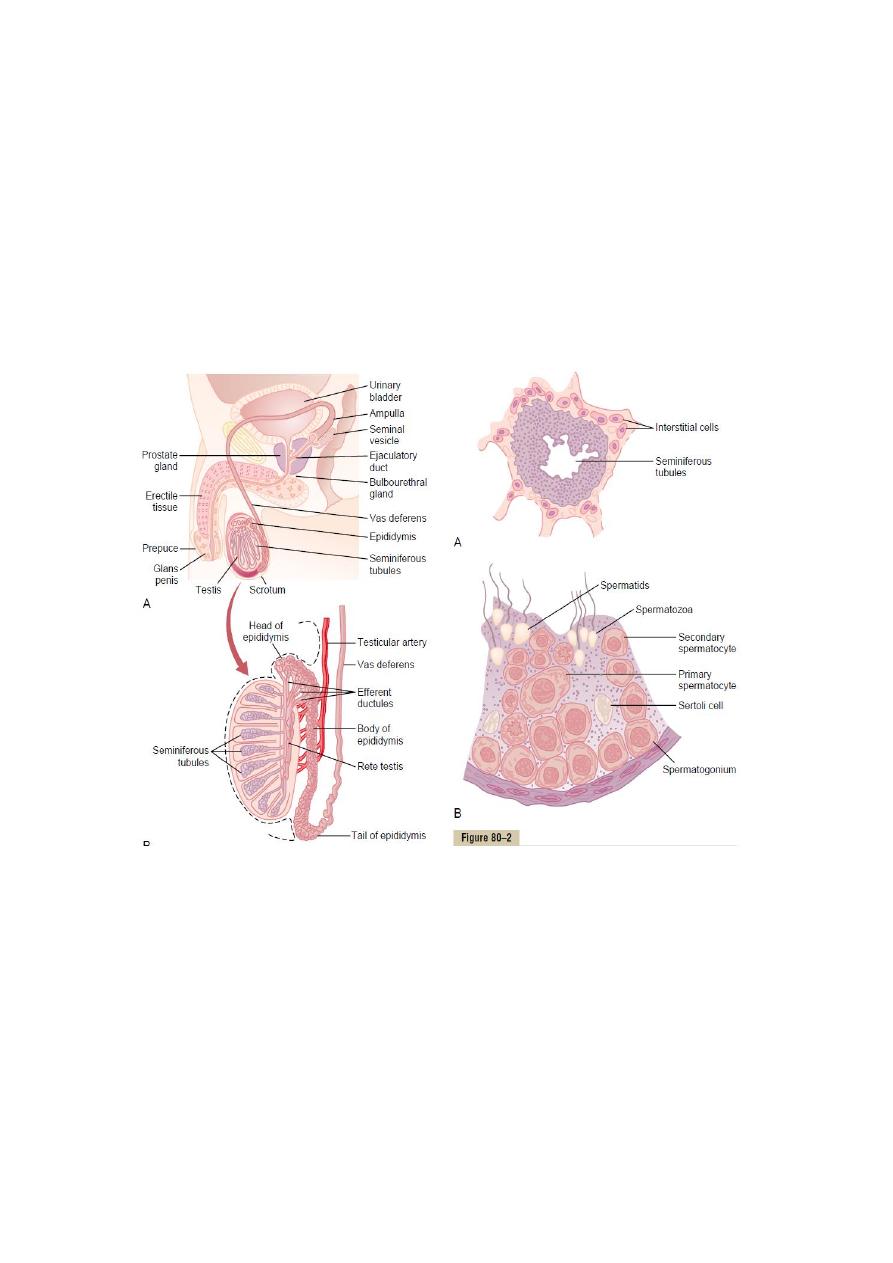
Physiologic Anatomy of the Male Sexual Organs:
Spermatogenesis
During formation of the embryo the testes contain immature
germ cells called spermatogonia which lie in two or three layers
of the inner surfaces of the seminiferous tubules. The
spermatogonia begin to undergo mitotic division, beginning at
puberty, and continually proliferate and differentiate through
definite stages of development to form sperm
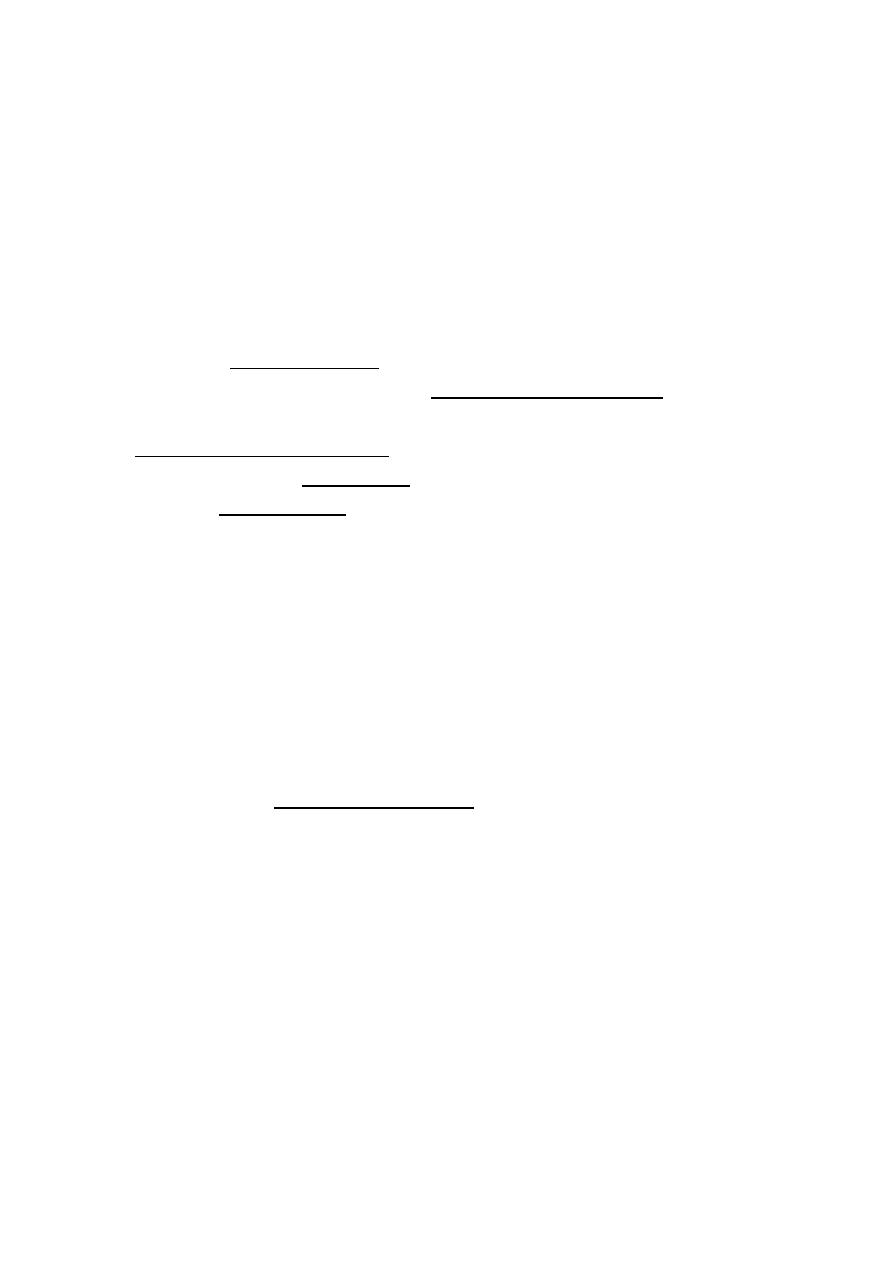
Steps of Spermatogenesis
Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
2
Spermatogenesis occurs in the seminiferous tubules during
active sexual life as the result of stimulation by anterior
pituitary gonadotropic hormones, beginning at an average age
of 13 years and continuing throughout most of the remainder
of life but decreasing markedly in old age. In the first stage of
spermatogenesis, the spermatogonia migrate among Sertoli
cells toward the central lumen of the seminiferous tubule.
Meiosis: Spermatogonia that become progressively modified
and enlarged to form large primary spermatocytes. Each of
these, in turn, undergoes meiotic division to form two
secondary spermatocytes. After another few days, these too
divide to form spermatids that are eventually modified to
become spermatozoa (sperm).
During the change from the spermatocyte stage to the
spermatid stage, the 46 chromosomes (23 pairs of
chromosomes) of the spermatocyte are divided, so that 23
chromosomes go to one spermatid and the other 23 to the
second spermatid. This also divides the chromosomal genes so
that only one half of the genetic characteristics of the eventual
fetus are provided by the father, while the other half are
derived from the oocyte provided by the mother. The entire
period
of
spermatogenesis,
from
spermatogonia
to
spermatozoa, takes about 74 days.
Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
3
In each spermatogonium, one of the 23 pairs of chromosomes
carries the genetic information that determines the sex of each
eventual offspring. This pair is composed of one X
chromosome, which is called the female chromosome, and one
Y chromosome, the male chromosome. During meiotic division,
the male Y chromosome goes to one spermatid that then
becomes a male sperm, and the female X chromosome goes to
another spermatid that becomes a female sperm.
Formation of Sperm: When the spermatids are first formed,
they still have the usual characteristics of epithelioid cells, but
soon they begin to differentiate and elongate into
spermatozoa. The head comprises the condensed nucleus of
the cell with only a thin cytoplasmic and cell membrane layer
around its surface. On the outside of the anterior two thirds of
the head is a thick cap called the acrosome that is formed
mainly from the Golgi apparatus. This contains a number of
enzymes that play important roles in allowing the sperm to
enter the ovum and fertilize it. The tail of the sperm, called the
flagellum, which is used for sperm movement (flagellar
movement). The energy for this process is supplied in the form

Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
4
of ATP that is synthesized by the mitochondria in the body of
the tail. Normal sperm move in a fluid medium at a velocity of 1
to 4 mm/min. This allows them to move through the female
genital tract in quest of the ovum.
Hormonal Factors That Stimulate Spermatogenesis
Several hormones play essential roles in spermatogenesis.
Some of these are as follows:
1. Testosterone, secreted by the Leydig cells located in the
testis, is essential for growth and division of the testicular
germinal cells, which is the first stage in forming sperm.
2. Luteinizing hormone, secreted by the anteriorpituitary gland,
stimulates the Leydig cells to secrete testosterone.
3. Follicle-stimulating hormone FSH, also secreted by the
anterior pituitary gland, stimulates the Sertoli cells; without this
stimulation, the conversion of the spermatids to sperm (the
process of spermiogenesis) will not occur.
4. Estrogens, formed from testosterone by the Sertoli cells
when they are stimulated by FSH hormone, are probably also
essential for spermiogenesis.
5. G
rowth hormone (as well as most of the other body
hormones) is necessary for controlling background metabolic
functions of the testes. Growth hormone specifically promotes
early division of the spermtogonia themselves; in its absence,
as in pituitary dwarfs, spermatogenesis is severely deficient or
absent, thus causing infertility.

Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
5
Maturation of Sperm in the Epididymis
After formation in the seminiferous tubules, the sperm require
several days to pass through the 6-meter-long tubule of the
epididymis. Sperm removed from the seminiferous tubules and
from the early portions of the epididymis are non-motile, and
they cannot fertilize an ovum. However, after the sperm have
been in the epididymis for some 18 to 24 hours, they develop
the capability of motility. Even though several inhibitory
proteins in the epididymal fluid still prevent final motility until
after ejaculation.
Storage of Sperm: The two testes of the human adult form up
to 120 million sperm each day. A small quantity of these can be
stored in the epididymis, but most are stored in the vas
deferens. They can remain stored, maintaining their fertility, for
at least a month. During this time, they are kept in a deeply
suppressed inactive state by multiple inhibitory substances in
the secretions of the ducts. Conversely, with a high level of
sexual activity and ejaculations, storage may be no longer than
a few days.
After ejaculation, the sperm become motile, and they also
become capable of fertilizing the ovum, a process called
maturation.
Physiology of the Mature Sperm: The normal motile, fertile
sperm are capable of flagellated movement though the fluid
medium at velocities of 1 to 4 mm/min. The activity of sperm is
greatly enhanced in a neutral and slightly alkaline medium, as
exists in the ejaculated semen, but it is greatly depressed in a
mildly acidic medium. A strong acidic medium can cause rapid
death of sperm. The activity of sperm increases markedly with
increasing temperature, but so does the rate of metabolism,
causing the life of the sperm to be considerably shortened.
Although sperm can live for many weeks in the suppressed
state in the genital ducts of the testes, life expectancy of
ejaculated sperm in the female genital tract is only 1 to 2 days.

Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
6
Function of the Seminal Vesicles: Each seminal vesicle is a
tortuous tube lined with a secretory epithelium that secretes a
mucous material containing an abundance of fructose, citric
acid, and other nutrient substances, as well as large quantities
of prostaglandins and fibrinogen. During the process of
emission and ejaculation, each seminal vesicle empties its
contents into the ejaculatory duct. This adds greatly to the bulk
of the ejaculated semen, and the fructose and other substances
in the seminal fluid are of considerable nutrient value for the
ejaculated sperm until one of the sperm fertilizes the ovum.
Function of the Prostate Gland: The prostate gland secretes a
thin, milky fluid that contains calcium, citrate ion, phosphate
ion, a clotting enzyme, and a profibrinolysin. During emission,
the capsule of the prostate gland contracts simultaneously with
the contractions of the vas deferens so that the thin, milky fluid
of the prostate gland adds further to the bulk of the semen. A
slightly alkaline characteristic of the prostatic fluid may be quite
important for successful fertilization of the ovum, because the
fluid of the vas deferens is relatively acidic owing to the
presence of citric acid and metabolic end products of the sperm
and, consequently, helps to inhibit sperm fertility. Also, the
vaginal secretions of the female are acidic (pH of 3.5 to 4.0).
Sperm do not become optimally motile until the pH of the
surrounding fluids rises to about 6.0 to 6.5. Consequently, it is
probable that the slightly alkaline prostatic fluid helps to
neutralize the acidity of the other seminal fluids during
ejaculation, and thus enhances the motility and fertility of the
sperm.
Semen
Semen, which is ejaculated during the male sexual act which is
about 2 to 7ml, is composed of the fluid and sperm from the
vas deferens (about 10 per cent of the total), fluid from the
seminal vesicles (almost 60 per cent), fluid from the prostate
gland (about 30 per cent), and small amounts from the mucous

Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
7
glands, especially the bulbourethral glands. Thus, the bulk of
the semen is seminal vesicle fluid, which is the last to be
ejaculated and serves to wash the sperm through the
ejaculatory duct and urethra.
The average pH of the combined semen is about 7.5, the
alkaline prostatic fluid having more than neutralized the mild
acidity of the other portions of the semen. The prostatic fluid
gives the semen a milky appearance. Also, a clotting enzyme
from the prostatic fluid causes the fibrinogen of the seminal
vesicle fluid to form a weak fibrin coagulum that holds the
semen in the deeper regions of the vagina where the uterine
cervix lies. The coagulum then dissolves during the next 15 to
30 minutes because of lysis by fibrinolysin formed from the
prostatic profibrinolysin. In the early minutes after ejaculation,
the sperm remain relatively immobile, possibly because of the
viscosity of the coagulum. As the coagulum dissolves, the
sperm simultaneously become highly motile.
Although sperm can live for many weeks in the male genital
ducts, once they are ejaculated in the semen, their maximal life
span is only 24 to 48 hours at body temperature. At lowered
temperatures, however, semen can be stored for several
weeks, and when frozen at temperatures below -100°C, sperm
have been preserved for years.
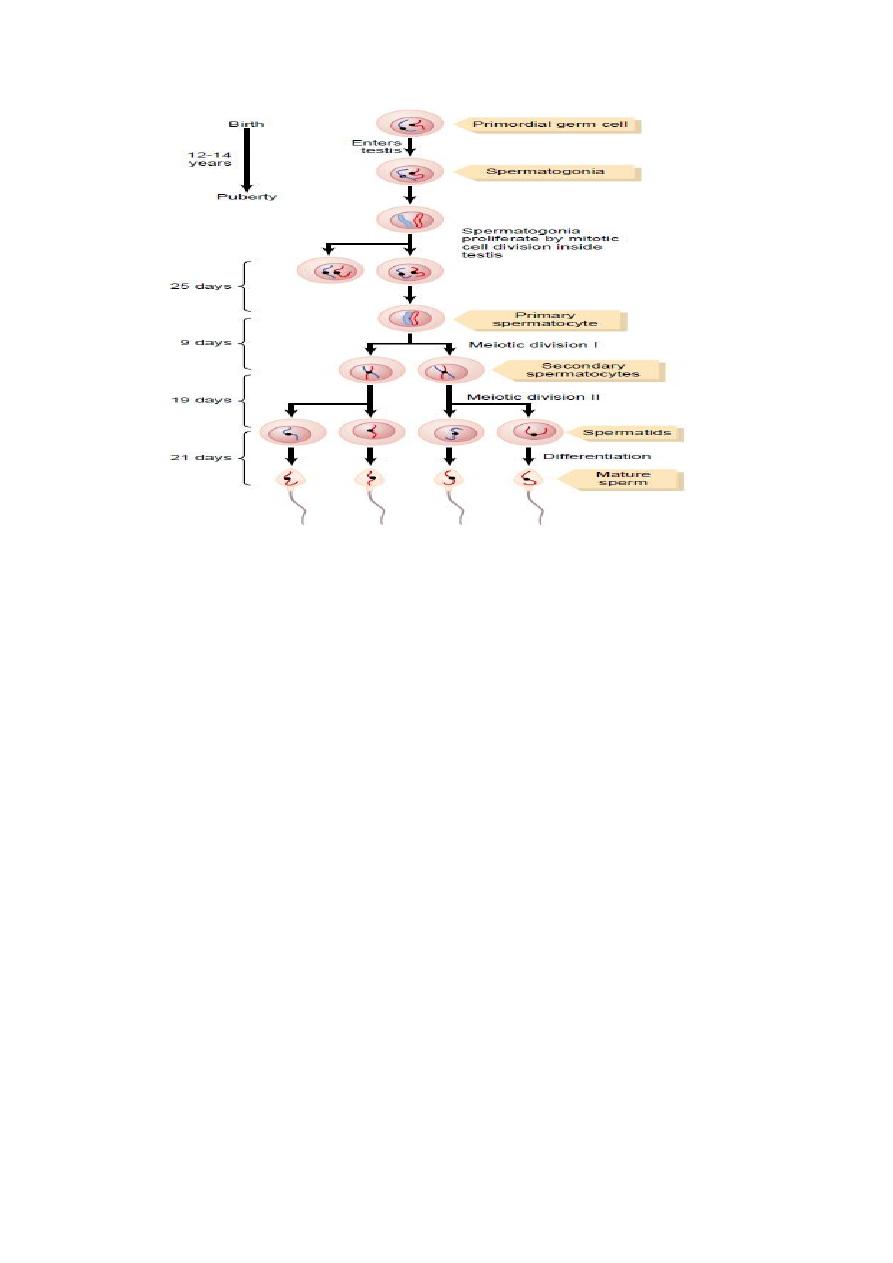
Erection, Emission, and Ejaculation: The Male Sexual Act:
Erection, accompanied by increases in the length and width of
the penis, is achieved as a result of blood flow into the “erectile
tissues” of the penis. These erectile tissues include two paired
structures—the corpora cavernosa—located on the dorsal side
of the penis, and one unpaired corpus spongiosum on the
ventralside. The urethra runs through the center of the corpus
spongiosum. The erectile tissue forms columns that extend the
length of the penis.
Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
8
Erection is achieved by parasympathetic nerve-induced
vasodilation of arterioles that allows blood to flow into the
corpora cavernosa of the penis. The neurotransmitter that
mediates this increased blood flow is now believed to be nitric
oxide. As the erectile tissues become engorged with blood and
the penis becomes turgid, venous outflow of blood is partially
occluded, thus aiding erection.
The term emission refers to the movement of semen into the
urethra, and ejaculation refers to the forcible expulsion of
semen from the urethra out of the penis. Emission and
ejaculation are stimulated by sympathetic nerves, which cause
peristaltic contractions of the tubular system, contractions of
the seminal vesicles and prostate, and contractions of muscles
at the base of the penis. Sexual function in the male thus
requires the synergistic action (rather than antagonistic action)
of the parasympathetic and sympathetic systems.
Erection is controlled by two portions of the central nervous
system—the hypothalamus in the brain and the sacral portion
of the spinal cord. Conscious sexual thoughts originating in the
cerebral cortex act via the hypothalamus to control the sacral
region, which in turn increases parasympathetic nerve activity
to promote vasodilatation and erection of the penis.
Testosterone:
The testes secrete several male sex hormones, which are
collectively called androgens. Testosterone is eventually
converted into the more active hormone dihydrotestosterone
in the target tissues.
Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
9
Testosterone is formed by the interstitial cells of Leydig, which
lie in the interstices between the seminiferous tubules and
constitute about 20 per cent of the mass of the adult testes.
Leydig cells are almost nonexistent in the testes during
childhood when the testes secrete almost no testosterone, but
they are numerous in the newborn male infant for the first few
months of life and in the adult male any time after puberty; at
both these times the testes secrete large quantities of
testosterone.
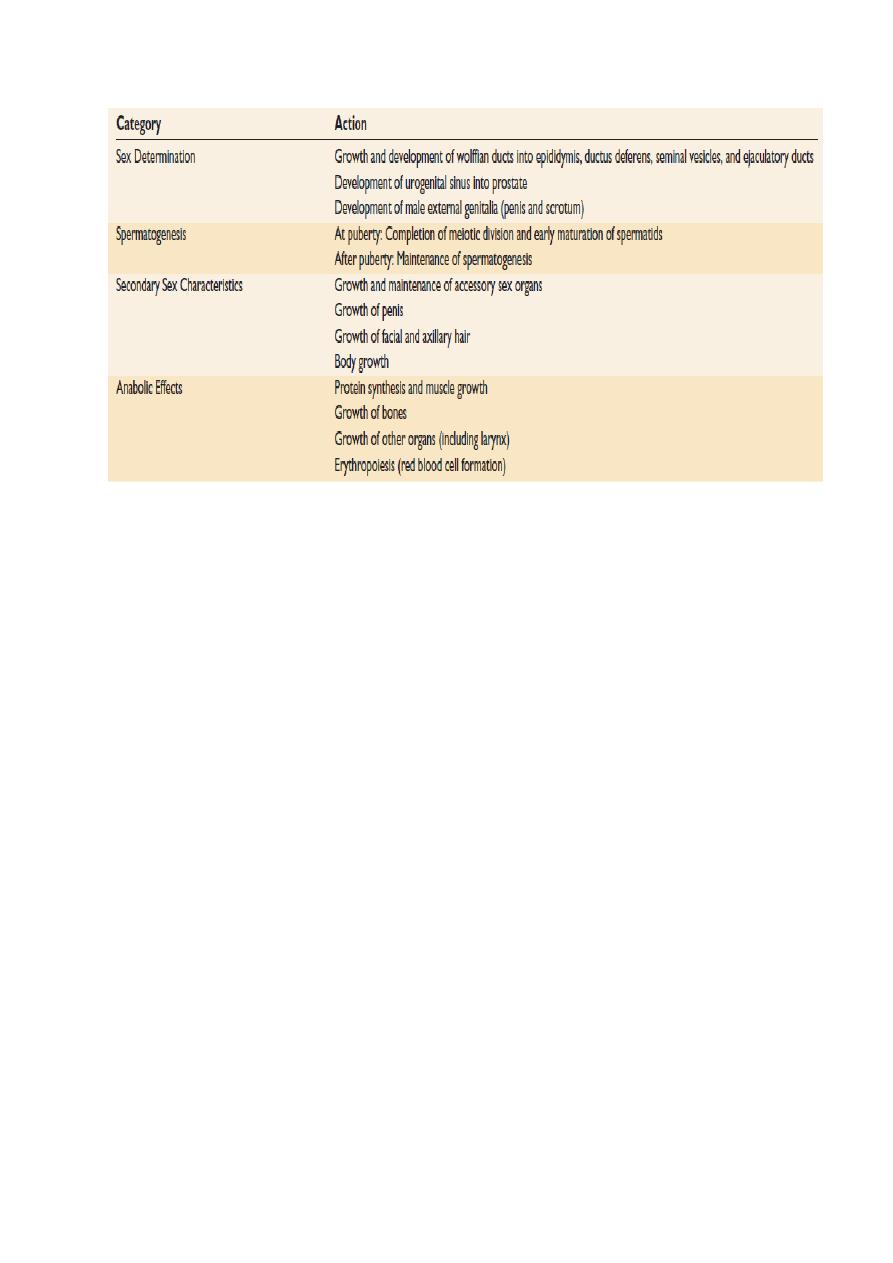
Functions of Testosterone:
A- Functions of Testosterone during Fetal Development:
Testosterone secreted first by the genital ridges and later by
the fetal testes is responsible for the development of the male
body characteristics, including the formation of a penis and a
scrotum rather than formation of a clitoris and a vagina. Also, it
causes formation of the prostate gland, seminal vesicles, and
male genital ducts, while at the same time suppressing the
formation of female genital organs.
Testosterone begins to be elaborated by the male fetal testes
at about the seventh week of embryonic life.
Also Testosterone causes descent of the testes. The testes
usually descend into the scrotum during the last 2 to 3 months
of gestation when the testes begin secreting reasonable
quantities of testosterone. The process of tsetse decent needs
normal amount of testosterone.
B- Effect of Testosterone on Development of Adult Primary
and Secondary Sexual Characteristics
After puberty, the increasing amounts of testosterone
secretion cause the penis, scrotum, and testes to enlarge about
eightfold before the age of 20 years. In addition, testosterone
causes the secondary sexual characteristics of the male to
develop, beginning at puberty and ending at maturity. These
secondary sexual characteristics, in addition to the sexual
organs themselves, distinguish the male from the female.
Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
11
*Effect on the Distribution of Body Hair: Testosterone
decreases the growth of hair on the top of the head; a man
who does not have functional testes does not become bald.
However, many virile men never become bald because
baldness is a result of two factors: first, a genetic background
for the development of baldness and, second, superimposed on
this genetic background, large quantities of androgenic
hormones.
*Effect on the Voice: Testosterone causes hypertrophy of the
laryngeal
mucosa
and
enlargement
of
the
larynx.
*Testosterone Increases Thickness of the Skin and Can
Contribute to Development of Acne: Testosterone increases
the thickness of the skin over the entire body and increases the
ruggedness of the subcutaneous tissues. Testosterone also
increases the rate of secretion of all the body’s sebaceous
glands. Especially important is excessive secretion by the
sebaceous glands of the face, because this can result in acne.
*Testosterone Increases Protein Formation and Muscle
Development: One of the most important male characteristics
is development of increasing musculature after puberty,
averaging about a 50 per cent increase in muscle mass over
that in the female. This is associated with increased protein in

Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
11
the non-muscle parts of the body as well. Many of the changes
in the skin are due to deposition of proteins in the skin, and the
changes in the voice also result partly from this protein
anabolic function of testosterone.
*Testosterone Increases Bone Matrix and Causes Calcium
Retention: After the great increase in circulating testosterone
that occurs at puberty the bones grow considerably thicker and
deposit
considerable
additional
calcium
salts.
Thus,
testosterone increases the total quantity of bone matrix and
causes calcium retention. The increase in bone matrix is
believed to result from the general protein anabolic function of
testosterone plus deposition of calcium salts in response to the
increased protein.
Testosterone has a specific effect on the pelvis to narrow its
outlet and lengthen it. In the absence of testosterone, the male
pelvis develops into a pelvis that is similar to that of the female.
The testosterone also causes the epiphyses of the long bones
to unite with the shafts of the bones at an early age. Therefore,
despite the rapidity of growth, this early uniting of the
epiphyses prevents the person from growing tall.
*Testosterone Increases Basal Metabolism: the usual quantity
of testosterone secreted by the testes during adolescence and
early adult life increases the rate of metabolism some 5 to 10
per cent above the value that it would be were the testes not
active.
*Effect on Red Blood Cells: the average man has about 700,000
more red blood cells per cubic millimeter than the average
woman so the level of Hb is higher. This difference may be due
partly to the increased metabolic rate by testosterone and may
be from the direct effect of testosterone on red blood cell
production.
Control of Male Sexual Functions by Hormones from the
Hypothalamus and Anterior Pituitary Gland: A major share of
the control of sexual functions in both the male and the female
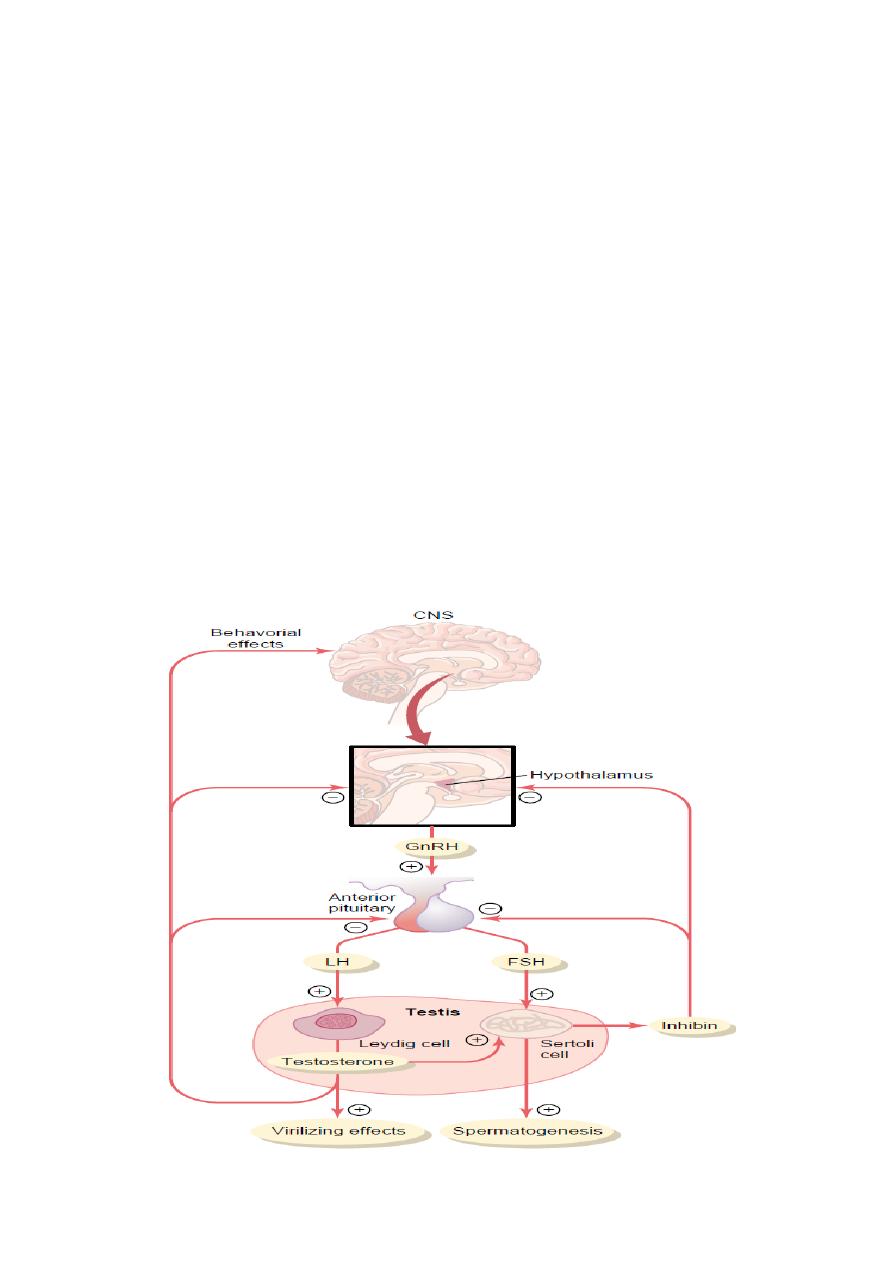
Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
12
begins with secretion of gonadotropin-releasing hormone
(GnRH) by the hypothalamus. This hormone in turn stimulates
the anterior pituitary gland to secrete two other hormones
called gonadotropic hormones: (1) luteinizing hormone (LH) and
(2) follicle-stimulating hormone (FSH). In turn, LH is the primary
stimulus for the secretion of testosterone by the testes, and
FSH mainly stimulates spermatogenesis.
Gonadotropic Hormones: LH and FSH
Both of the gonadotropic hormones, LH and FSH, are secreted
by the same cells, called gonadotropes, in the anterior pituitary
gland. In the absence of GnRH secretion from the
hypothalamus, the gonadotropes in the pituitary gland secrete
almost no LH or FSH. LH and FSH are glycoproteins. They exert
their effects on their target tissues in the testes mainly by
activating the cyclic adenosine monophosphate second
messenger system, which in turn activates specific enzyme
systems in the respective target cells.
Endocrine physiology - Reproductive physiology Dr. Ghassan lec. 2
13
