
1
Physiology Dr Hanan Luay
Objectives :
1- Discuss the differentiation of gonads.
2- Identify the disturbance of gonads development.
3- List the effects of estrogen on female body.
The Reproductive system
There are 46 chromosomes: in males, 22 pairs of autosomes plus an X
chromosome and a Y chromosome; in females, 22 pairs of autosomes plus two
X chromosomes. As a consequence of meiosis during gametogenesis, each
normal ovum contains a single X chromosome, but half the normal sperms
contain an X chromosome and half contain a Y chromosome .When a sperm
containing a Y chromosome fertilizes an ovum, an XY pattern results and the
zygote develops into a genetic male. When fertilization occurs with an X-
containing sperm, an XX pattern and a genetic female result (so the sex of the
resulting zygot is determined by the fertilizing sperm).
The differentiation of the primitive gonads into testes or ovaries in utero is
genetically determined in humans, but the formation of male genitalia depends
upon the presence of a functional, secreting testis; in the absence of testicular
tissue, development is female. There is evidence that male sexual behavior and,
in some species, the male pattern of gonadotropin secretion are due to the action
of male hormones on the brain in early development.
Development of the Gonads
On each side of the embryo, a primitive gonad arises from the genital ridge. The
gonad develops a cortex and a medulla. Until the sixth week of development,

2
these structures are identical in both sexes i.e undifferentiated called bipotential
gonads which contains primitive germ cells and has both male and female
primordial genital ducts. After the 6
th
week the differentiation started. In genetic
males, the medulla develops during the seventh and eighth weeks into a testis,
and the cortex regresses. Leydig and Sertoli cells appear, and testosterone and
mullerian inhibiting substance are secreted. In genetic females, the cortex
develops into an ovary and the medulla regresses. It will not secret estrogen
inutero, so the secondary sex organs will develop without any hormonal
influence.
In a normal female fetus, the mullerian duct system then develops into uterine
tubes (oviducts) and a uterus. In the normal male fetus, the wolffian duct system
on each side develops into the epididymis and vas deferens. The external
genitalia
are
similarly
bipotential
until
the
eighth
week.
When there are functional testes in the embryo, male internal and external
genitalia develop. The Leydig cells of the fetal testis secrete testosterone
(androgens), and the Sertoli cells secrete mullerian inhibiting substance (MIS;
also called mullerian regression factor, or MRF). MIS causes regression of the
mullerian ducts, and testosterone fosters the development of the vas deferens and
related structures from the wolffian ducts. Also induces the formation of male
external
genitalia
and
male
secondary
sex
characteristics.
Note that the determination of the internal sex organs is not under the influence
of androgens, that’s why if we introduce androgen into a genetically female
fetus, this does not influence the female pattern of the internal sex organ, but it
will affect the external sex organ and it will show a male pattern.
ABERRANT SEXUAL DIFFERENTIATION
Chromosomal Abnormalities
Abnormalities of sexual development could be caused by genetic
(chromosomal) or hormonal abnormalities or
other teratogenic causes.
An established defect in gametogenesis is nondisjunction, a phenomenon in
which a pair of chromosomes fails to separate, so that both go to one of the
daughter cells during meiosis.
Examples of these abnormalities: 1- a syndrome called gonadal dysgenesis (or
agenesis) or, alternatively, ovarian agenesis or Turner's syndrome. In these

3
individuals there is an XO chromosomal pattern, the gonads are rudimentary or
absent, but there is female external genitalia. Stature is short, webbing of the
neck, other congenital abnormalities are often present, and no maturation occurs
at puberty.
2- A syndrome known as seminiferous tubule dysgenesis or Klinefelter's
syndrome. Individuals with the XXY pattern, the most common sex
chromosome disorder, have the genitalia of a normal male. Testosterone
secretion at puberty is often great enough for the development of male sex
characteristics. However, the seminiferous tubules are abnormal, and there is a
higher than normal incidence of mental retardation and usually these patients are
long.
3- The XXX ("superfemale") pattern, it is more common in general population,
since it does not seem to be associated with any characteristic abnormalities.
4- The YO combination is probably lethal and incompatible with life.
Nondisjunction or simple loss of a sex chromosome can occur during the early
mitotic divisions after fertilization. The result of faulty mitoses in the early
zygote is the production of a mosaic, an individual with two or more populations
of cells with different chromosome complements.
True hermaphroditism, the condition in which the individual has both ovaries
and testes, is probably due to XX/XY mosaicism and related mosaic patterns,
although
other
genetic
aberrations
are
possible.
Chromosomal abnormalities also include transposition of parts of chromosomes
to other chromosomes. Sex chromosome abnormalities are, of course, not the
only abnormalities associated with disease states; nondisjunction of several
different autosomal chromosomes is known to occur. For example,
nondisjunction of chromosome 21 produces trisomy 21, the chromosomal
abnormality associated with Down's syndrome (mongolism). The additional
chromosome 21 is normal, so Down's syndrome is a pure case of gene excess
causing abnormalities. In most instances, nondisjunction occurs in the ovary
rather than the testis and the incidence of Down's syndrome increases with
advancing age of the mother.
4
Hormonal Abnormalities
Development of the male external genitalia occurs normally in genetic males in
response to androgen secreted by the embryonic testes.
Genetic females exposed to androgens from some other source during the eighth
to the thirteenth weeks of gestation, may develop male genetalia. The syndrome
that results is female pseudohermaphroditism. A pseudohermaphrodite is an
individual with the genetic constitution and gonads of one sex and the genitalia
of the other. After the thirteenth week, the genitalia are fully formed, but
exposure to androgens can cause hypertrophy of the clitoris. Its causes either due
to congenital adrenal hyperplasia , or it may be caused by androgens
administered to the mother.
Male pseudohermaphroditism: development of female external genitalia in
genetic males. It occurs when the embryonic testes are defective. Because the
testes also secrete MIS (mullerian inhibiting substance or mullerian
regression factor), genetic males with defective testes have female internal
genitalia.
Another cause of male pseudohermaphroditism is androgen resistance, in
which, male hormones cannot exert their full effects on the tissues. One form of
androgen resistance is , in which the enzyme responsible for the formation of the
active form of testosterone is decreased.
This androgen resistance may also due to mutations in the androgen
receptor gene and the resulting defects in receptor function ranges from minor
to severe. Mild defects cause infertility with or without gynecomastia , but when
the loss of receptor function is complete, the testicular feminizing syndrome,
now known as complete androgen resistance syndrome, results. In this
condition, MIS is present and testosterone is secreted at normal or even elevated
rates. The external genitalia are female, but the vagina ends blindly because
there are no female internal genitalia. Individuals with this syndrome develop
enlarged breasts at puberty and usually are considered to be normal women until
they are diagnosed when they seek medical advice because of lack of
menstruation .i.e female external genetalia, male internal genetalia.

5
Female reproductive system
Female reproductive functions can be divided into two major phases: (1)
preparation of the female body for pregnancy, and (2) the period of pregnancy
itself.
Ovaries:
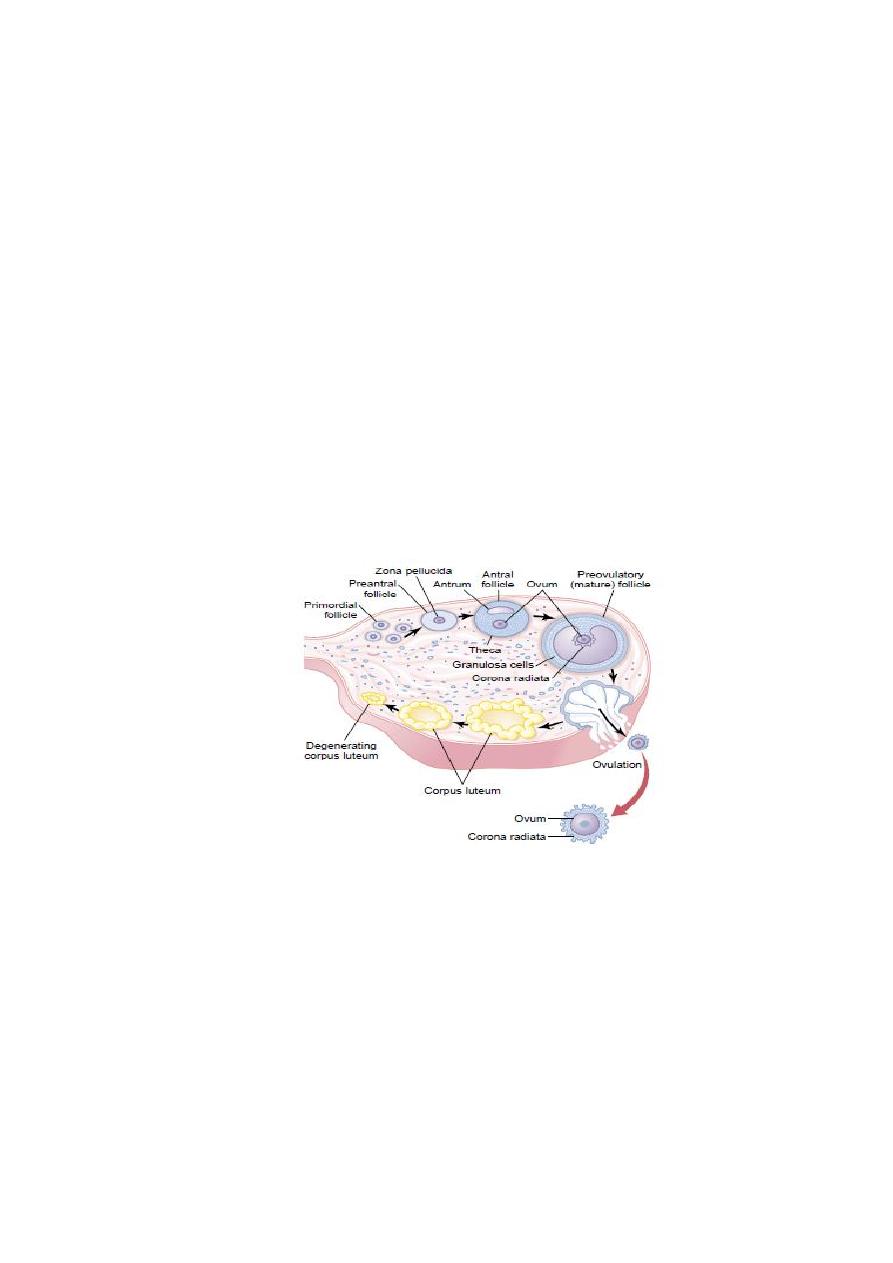
From the sixth week of intrauterine life the embryonic ovaries develop which
contain the primordial follicles which are about 7000000 follicles, then the
number regress during the next stages of life (leaving about 1 to 2 million
present at birth. At puberty, there is only about 300,000. About 400 eggs are
released during a woman's reproductive life. Only a small percentage of oocytes
mature into eggs. The many thousands of oocytes that do not mature degenerate.
.The female needs only one ovum in each menstrual cycle.
Functions of the ovarian hormones
—
the ovary secrets 3 hormones:
-Estrogens
-Progestins
-Relaxin
ESTROGENS:
It is a steroid synthesized in the ovaries mainly from cholesterol and secreted
by the ovarian theca interna cells, corpus luteum, fetoplacental units and small
amounts by the adrenal cortices and the testes,breast a,liver and fat cells.
There are three estrogens present in significant quantities in the plasma of the
human female: b-estradiol, estrone, and estriol, but The estrogenic potency of
b-estradiol is more than the others, it is considered the major estrogen.
They are transported in the blood bound mainly with plasma albumin and with
specific estrogen binding globulins.
The actions of estrogen are mediated by the estrogen receptor (which is
expressed in specific tissues including the ovary, uterus and breast.
Functions of the Estrogens:
A primary function of the estrogens is to cause cellular proliferation and growth
of the tissues of the sex organs and other tissues related to reproduction.
1-Effect of Estrogens on the Uterus and External Female Sex Organs.
Estrogens change the type of cervical mucosa and change the vaginal epithelium
from a cuboidal into a stratified type (more resistant to infection) and it lubricate
the internal wall of it, the external genitalia enlarge. The size of the uterus will
increase and the excitability of its muscle will increase also. It also causes
marked proliferation of the endometrial stroma (especially in the first half of the
menstrual cycle).
Estrogen makes the cervical mucosa thinner and more alkaline, these
changes promotes survival and transport of sperms
2-Effect of Estrogens on the Fallopian Tubes: it causes increase in the
mobility of the fallopian tubes (increase in the mobility and number of cilia

6
which beat toward the uterus), and helps propel the fertilized ovum in that
direction.
3-Effect of Estrogens on the Breasts.
It causes development of the stroma and the ductile tissue of the breast in
addition to that it causes breast growth and gives the external appearance of the
mature female breast. But its effect on the alveoli of the breast is to lesser extent
because their final growth is under the effect of progesterone and prolactin.
4-Effect of Estrogens on the Skeleton.
It stimulates bone growth (and causes a slight increase in total body protein).
Also it causes uniting of the epiphyses with the shafts of the long bones. This
effect of estrogen in the female is much stronger than the similar effect of
testosterone in the male. As a result, growth of the female usually ceases several
years earlier than growth of the male. A female who is devoid of estrogen
production usually grows several inches taller than a normal mature female
because her epiphyses do not unite at the normal time
.
After menopause and because of estrogen deficiency there will be decrease of
the bone matrix (increase in osteoclastic activity) and osteoporosis usually
occurs.
5-Female sexual characteristics: estrogen causes deposition of fat in the breasts
and subcutaneous tissues, also in the buttocks and thighs (broad hip), which is
characteristic of the feminine figure.
6-Effect of Estrogens on the Skin. Estrogens cause the skin to develop a
texture that is soft and usually smooth, also it causes high ratio of scalp hair to
the body hair.
7-Effect of Estrogens on Electrolyte Balance. It Causes sodium and water
retention by the kidney tubules, that’s why the female has increase in body
weight just before the menstrual cycle, also during pregnancy there is retention
of fluids because of the high estrogen.
8-Estrogen also causes decrease in the plasma cholesterol level,
Increase
, Decrease
,that’s why the incidence of ischemic heart
disease in female is higher after menopause.
10-Mental health
Estrogen is considered to play a significant role in women’s mental health.
Sudden estrogen withdrawal, fluctuating estrogen, and periods of sustained
estrogen low levels correlate with significant mood lowering..
7
Physiology
Objectives:
1- List the effects of progesterone on female body.
2- Describe the hormonal changes during the normal
menstrual cycle.
3- Discuss the uterine phases of the normal menstrual
cycle.
PROGESTINS:
The most important of the progestins is progesterone. In the normal nonpregnant
female, progesterone is secreted in significant amounts only during the latter half
of each ovarian cycle (secretory phase), when it is secreted by the corpus
luteum. Progesterone is also secreted by the placenta during pregnancy,
especially after the fourth month of gestation. Small amounts of progesterone are
excreted by the adrenal cortex and testes.
Within a few minutes after secretion, it binds to plasma proteins then almost all
the progesterone is degraded by the liver to other steroids that have no
progestational effect. The major end product of progesterone degradation is
pregnanediol which is excreted in urin after conversion to glucoronide. One can
estimate the rate of progesterone formation in the body from the rate of this
excretion.
Functions of Progesterone
1-Effect of Progesterone on the Uterus.
It promotes secretory changes in the uterine endometrium during the latter half
of the monthly female sexual cycle, thus preparing the uterus for implantation of
the fertilized ovum. Also it decreases the frequency and intensity of uterine
contractions, thereby helping to prevent expulsion of the implanted ovum. ( i.e
decrease the excitability of the uterine cells and their sensitivity to oxytocin.
Therefore females with low progesterone are liable for abortion so we have to
give them progestertone.
2-Effect of Progesterone on the Fallopian Tubes.
It promotes increased secretion by the mucosal lining of the fallopian tubes.
3-Effect of Progesterone on the Breasts.
Progesterone promotes development of the lobules and alveoli of the breasts,

8
causing the alveolar cells to proliferate, enlarge, and become secretory in nature
i.e causes the breasts to swell (but milk secretions will not occur until stimulated
by prolactin).
4-Progesterone is a thermogenic hormone responsible for rising
temperature at time of ovulation
.
Note: as we said Estrogen makes the cervical mucosa thinner and more alkaline,
these changes promotes survival and transport of sperms, while progesterone
makes the secretion thick and the mucosa cellular, so the mucosa is thinnest at
time of ovulation and rise in an arborizing fern like pattern when a thin layer
spread on the slide while after ovulation and during pregnancy, it become thick
and fail to form the fern like pattern.
3-Relaxin:
It is the third hormone secreted by from the corpus luteum of pregnancy .It
relaxes the symphysis pubis and causes softening and relaxation of the cervix
during pregnancy .It may also be secreted by the placenta and the uterus
.
Menstrual cycle:
Puberty and Menarche
Puberty means the onset of adult sexual life.
Menarche means the beginning of the cycle of menstruation.
The period of puberty is caused by a gradual increase in gonadotropic hormone
secretion by the pituitary, the onset of puberty and menstruation between ages 11
and 16 years in girls (average, 13 years).
Menstrual cycle is the regular cyclic changes which occur from puberty till
menopause .The cycle extends from the first day of the period to the first day of
the next.
The primordial follicles which were in the ovary from birth begin to ripe under
the effect of FSH. some 12-20 primary follicles begin to develop under the
influence of elevated levels (FSH) to form secondary follicles. After a week or
more of growth— but before ovulation occurs—one of the follicles begins to
outgrow all the others; the remaining 5 to 11 will be atretic (regression of
growth). The single follicle reaches a diameter of 1 to 1.5 centimeters at the time
of ovulation and is called the mature follicle.
As the follicle grows there will be increase in ovarian secretion of estrogen ,and
when the level of estrogen increases, it feeds back to the anterior pituitary and
stimulate the release of FSH and LH (positive feedback effect) .By the day 13 of
the cycle, the circulating level of LH increases sharply(it increases 2 days before
ovulation), this LH surge is accompanied to lesser extent by an increase of FSH
secretion also, this combination of gonadotropins bring about the final
maturation of the of the ovarian follicles and ovulation . Ovulation in a woman
who has a normal 28-day female sexual cycle occurs 14 days after the onset of
9
menstruation
.
As the follicle ruptures, the ovum expelled into the abdominal
cavity and trapped by the fimbrial ends of the fallopian tubes, where the
fertilization occurs, and the fertilized ovum will be transported to the uterus
where it becomes implanted.
After ovulation, the granulose and theca interna cells lining the follicles
proliferate and replaced by luteal cells (filled with lipids which give the
yellowish color) forming what is called corpus luteum which secrets estrogen
and progesterone. So in the second half of the menstrual cycle the rise in
estrogen is from the corpus luteum .This high level of estrogen and progesterone
will feedback to the anterior pituitary and inhibit the release of FSH and LH
(negative feedback effect), and loss of these hormones finally causes the corpus
luteum to degenerate completely, So no more maintenance of the corpus luteum
and no more maintenance of the lining endometrium, so shedding of the
endometrium with drops of blood sudden cessation of secretion of estrogen,
progesterone, by the corpus luteum removes the feedback inhibition of the
anterior pituitary gland, allowing it to begin secreting increasing amounts of
FSH and LH again. FSH and LH initiate the growth of new follicles, beginning a
new ovarian cycle.
The period between the ovulation and the next cycle is usually 14 days, so any
change in the period occurs in the first half of the cycle (i.e. the time between the
start of the cycle and the ovulation is variable between women).
If the pregnancy occurs the corpus luteum persists (it persists because of the
action of human chorionic gonadotrophin hCG secreted by the embryonic
tissues) and continue to secret estrogen and progesterone, but after the 12
th
week
the fetoplacental unit takes the function.
After fertilization the fertilized ovum reaches the uterine cavity in 3-4 days
.During this time many or several mitotic divisions occur
(it becomes what is
called blastocyt about 100 cells), but not reach very large size because the
opening of the fallopian tube is small but if it enlarges in the tube for any reason
there will be ectopic pregnancy.
But in normal conditions the fertilized ovum

11
implanted in the uterine cavity in the 7
th
or 8
th
day after fertilization.
Implantation results from the action of trophoblast cells that secrete proteolytic
enzymes that digest the adjacent cells of the uterine endometrium.
After implantation the ovulation and menstruation is prevented by the secretion
of human chorionic gonadotropin by the newly developing embryonic tissues,
the secretion of this hormone can first be measured in the blood 8 to 9 days after
ovulation
or 6 days after fertilization (or in urine 14 days after fertilization)
,
shortly after the blastocyst implants in the endometrium. Then the rate of
secretion rises rapidly to reach a maximum at about 10 to 12 weeks of pregnancy
and decreases back to a lower value by 16 to 20 weeks. It continues at this level
for the remainder of pregnancy
.
The function of human Chorionic Gonadotropin (hCG) is to prevent
involution of the corpus luteum at the end of the monthly female sexual cycle.
Instead, it causes the corpus luteum to secrete even larger quantities of its sex
hormones—progesterone and estrogens—for the next few months.
Regarding the lining of the uterus (Uterine cycle), it passes through the
following stages: (1) proliferation of the uterine endometrium; (2) development
of secretory changes in the endometrium; and (3) desquamation of the
endometrium, which is known as menstruation.
1-Proliferative Phase (Estrogen Phase) of the Endometrial Cycle, Occurring
Before Ovulation
Under the influence of estrogens, secreted in increasing quantities by the ovary
during the first part of the monthly ovarian cycle, the stromal cells and the
epithelial cells proliferate rapidly the endometrium increases greatly in
thickness, owing to increasing numbers of stromal cells and to progressive
growth of the endometrial glands and new blood vessels into the endometrium.
The cervical canal has glands that secrete a thin mucous that helps deposited
sperm.
2-Secretory Phase (Progestational Phase) of the Endometrial Cycle,
Occurring After Ovulation
Progesterone causes marked swelling and secretory development of the
endometrium. The glands increase in tortuosity. Also, the cytoplasm of the
stromal cells increases; lipid and glycogen deposits increase greatly in the
stromal cells; and the blood supply to the endometrium further increases
with
the blood vessels becoming highly tortuous.
The whole purpose of these
endometrial changes is to prepare large amounts of stored nutrients to provide
appropriate conditions for implantation of a fertilized ovum.
3-Menstruation phase; If the ovum is not fertilized, about 2 days before the end
of the monthly cycle, the corpus luteum in the ovary suddenly involutes, and the
ovarian hormones (estrogens and progesterone) decrease to low levels of
secretion, Menstruation follows which lasts usually from 4-7 days (necrosis in
the endometrium, especially of the blood vessels → bleeding about 40 ml of
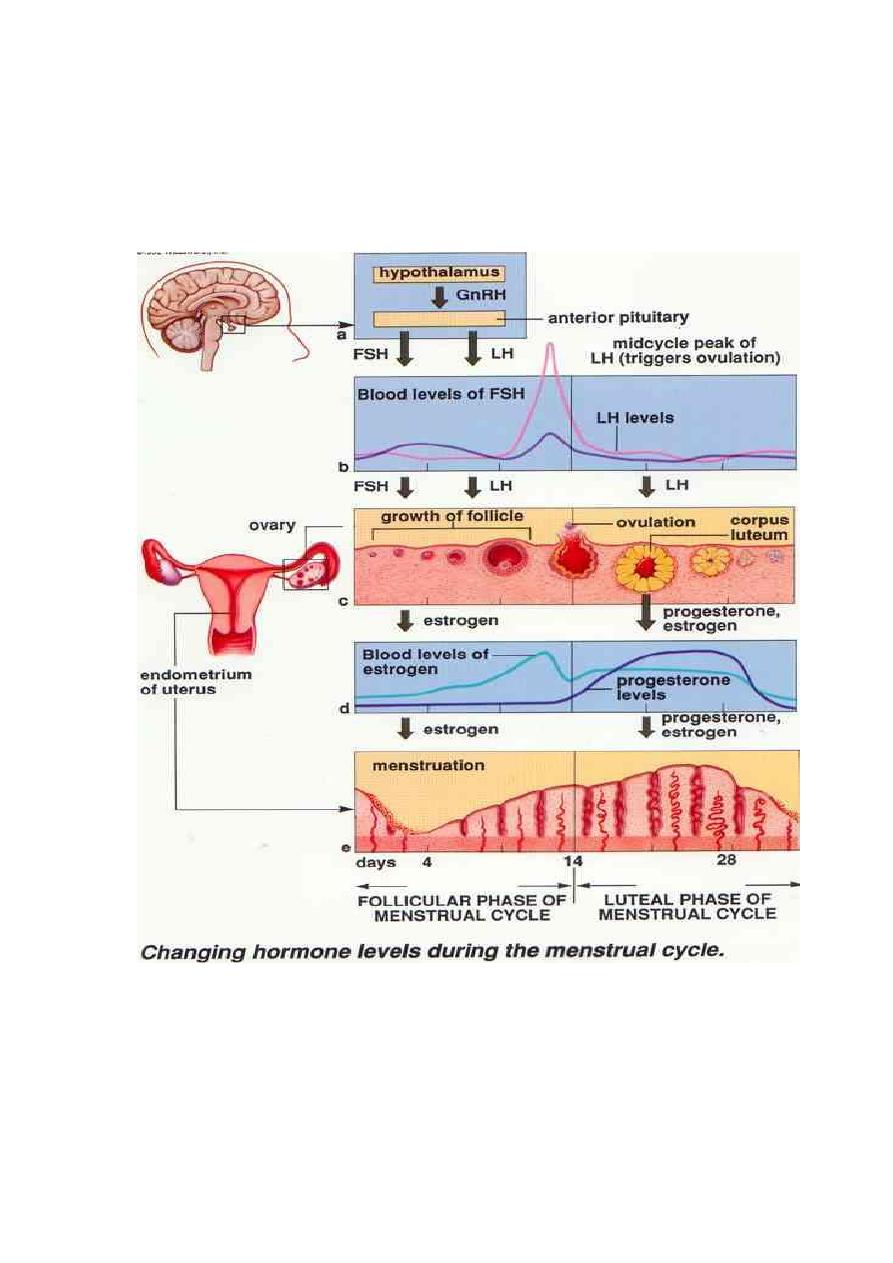
11
blood).

12
