Histology
Lec.4 Dr. Faraid
Small intestine:-
It is the portion of the digestive tube which extends from the pyloric
orifice to the ileocaecal junction. The small intestine is the site of
terminal food digestion, nutrient absorption & endocrine secretion. The
processes of digestion are completed in the small intestine, where the
products of digestion are absorbed by cells of the epithelial lining. The
small intestine is relatively long (5 meters) & consists of 3 segments:
Duodenum, Jejunum and Ileum.
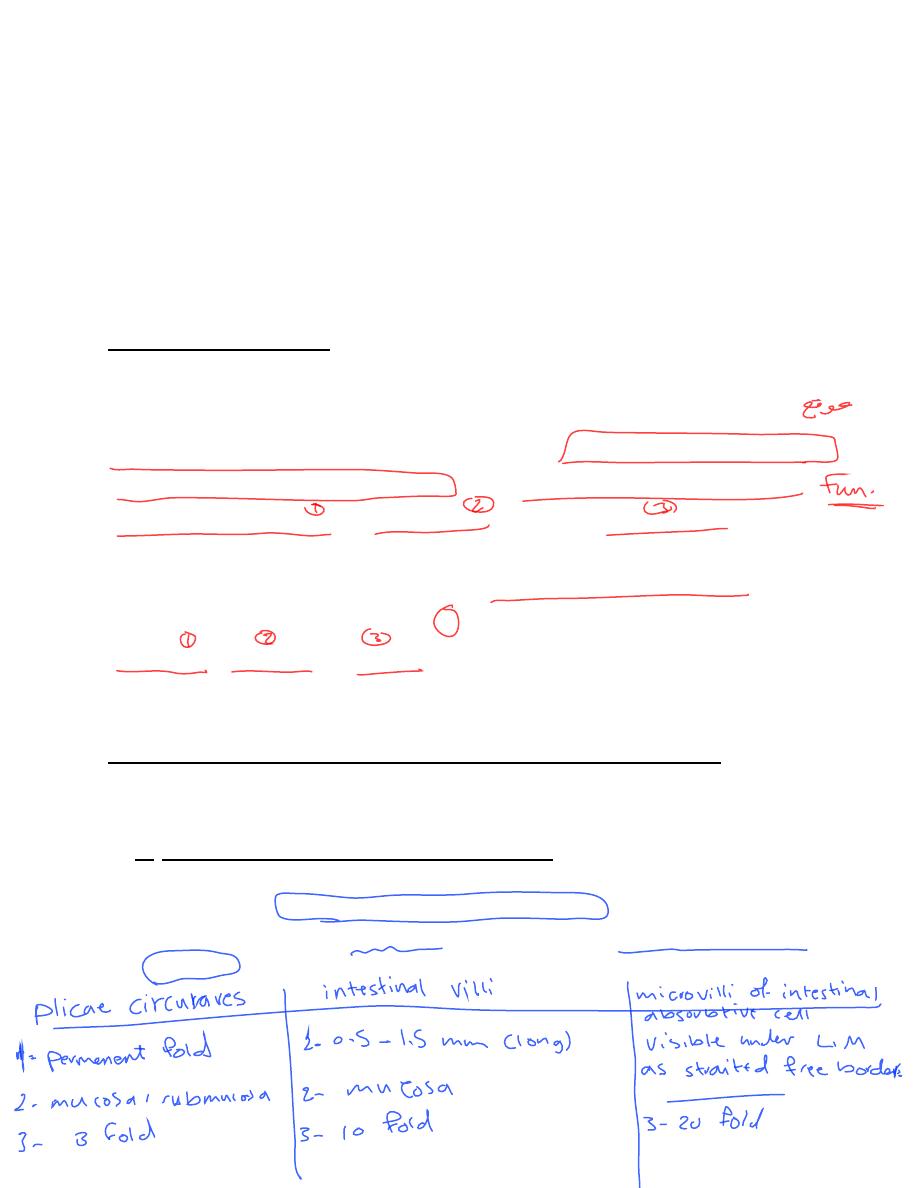
The factors that increase the surface area for absorption are:-
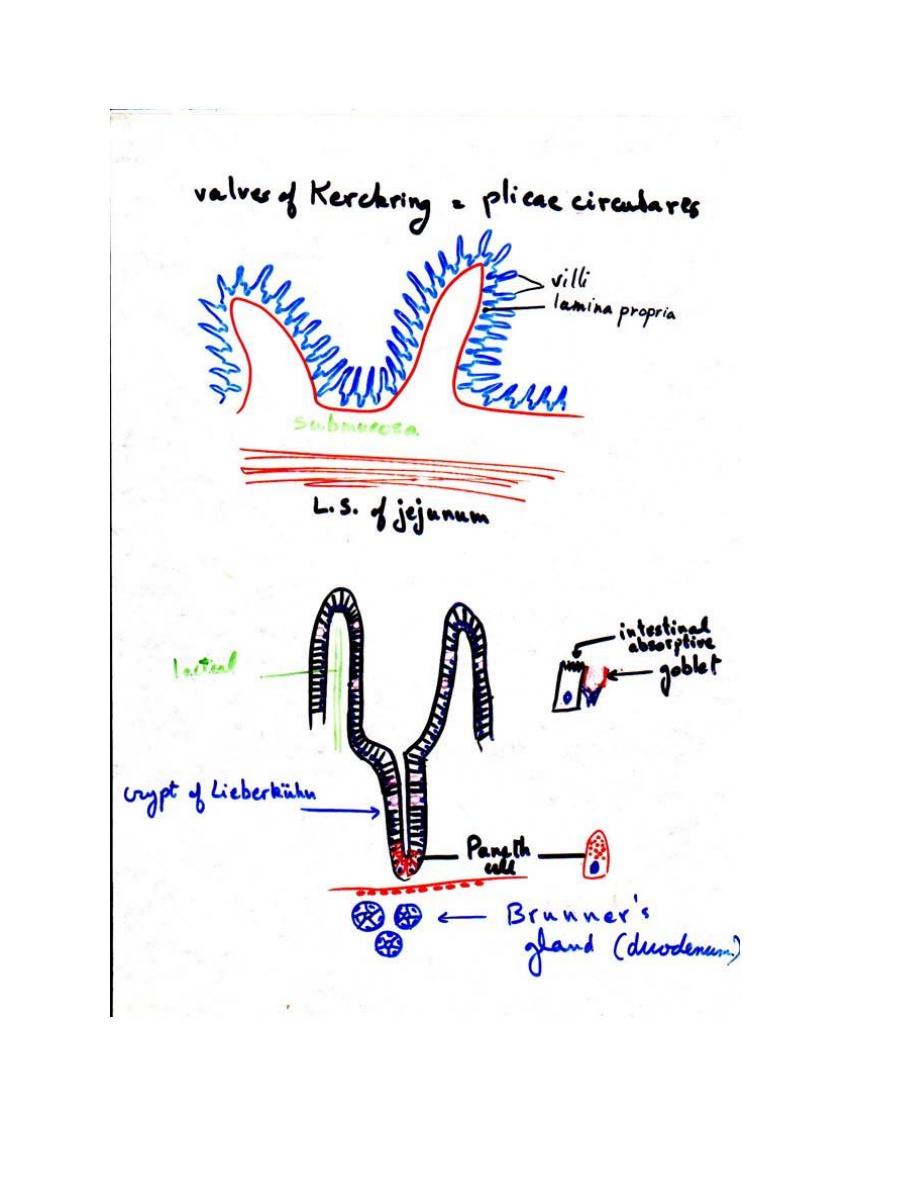
1- Plicae circulares (valves of Kerckring):- are series of permanent
folds, consisting of mucosa & submucosa, having a circular or
spiral form. The plicae are most developed in, and consequently a
characteristic of, the jejunum. They increase the intestinal surface
3-fold.
2- Intestinal villi :- are 0.5 to 1.5 mm long outgrowths of the mucosa
projecting into the lumen of the small intestine. They increase the
surface 10-fold.
3- Microvilli of the intestinal absorptive cells:- increase the surface
20-fold. They are visible under light microscope as a striated free
border.
All the above three factors together, are thus responsible for
600-fold increase in the intestinal surface.
As in other parts of the digestive tube, the wall of the small intestine
is made up of 4 layers:-
1) Mucous membrane:-
the surface of the mucous membrane is
thrown up into minute projections called villi.
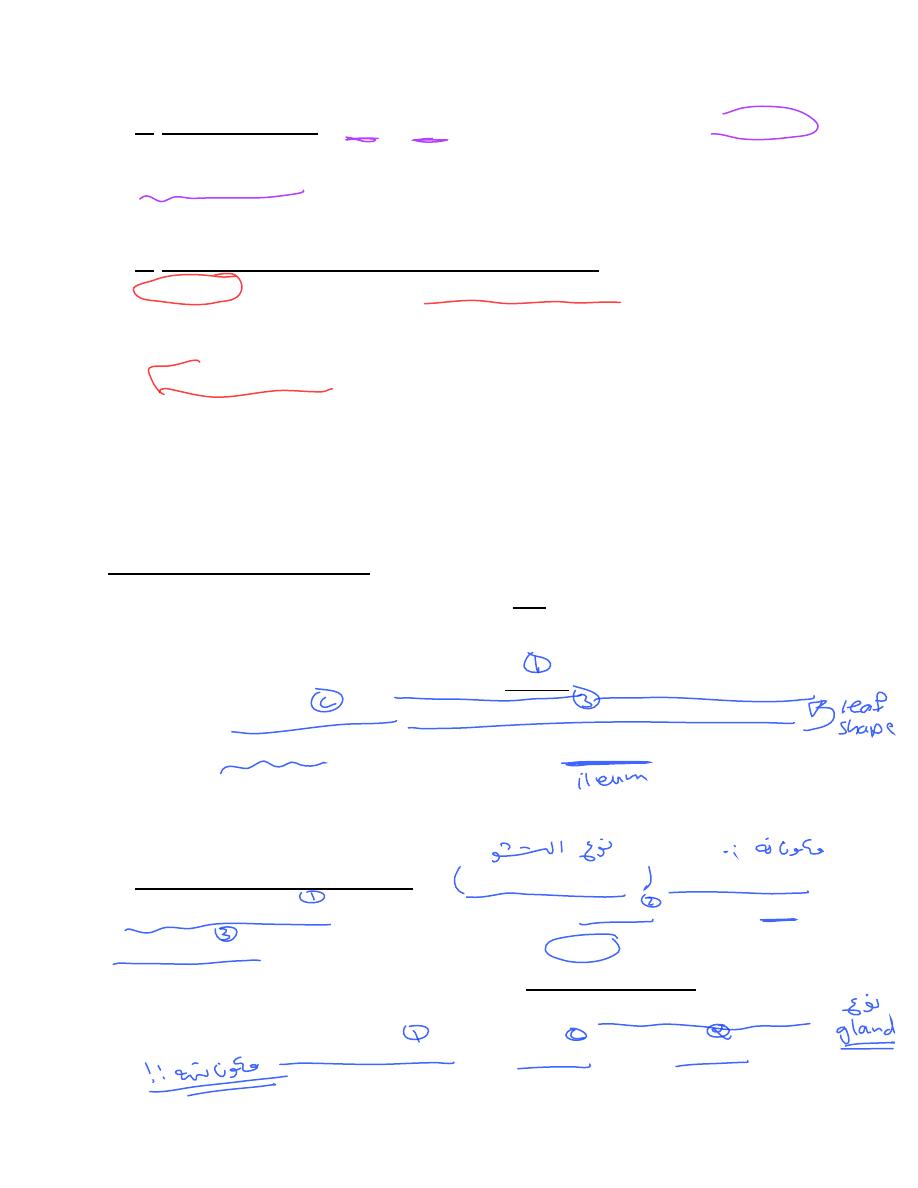
A villus consists of a core of lamina propria covered with epithelium.
The c.t. core of each villus contains a lacteal (blind-ended lymphatic
capillary), blood capillaries & strands of smooth m. In the duodenum,
the villi are leaf-shaped, gradually assuming fingerlike shapes as they
reach the ileum.
The intestinal epithelium is simple columnar, composed of
intestinal absorptive cells (enterocytes), goblet cells & some
enteroendocrine cells. In the ileum there is M-cell. The epithelium of
the villi is continuous with that of the intestinal glands [or glands
(crypts) of Lieberkühn]. The intestinal glands are simple tubular glands
contain intestinal absorptive cells, goblet cells, Paneth cells,
enteroendocrine cells& stem cells. Their secretions enter the lumen of
intestine by means of small openings between the villi.
a) The intestinal absorptive cells (enterocytes):- are tall columnar cells,
each with an oval nucleus in the basal half of the cell & striated(brush
border) at the apex of each cell. When viewed with E.M., the striated
border is seen to be a layer of densely packed microvilli. Each
absorptive cell is estimated to have an average 3000 microvilli.
Microvilli have the important physiologic function of increasing the area
of contact between the intestinal surface & the nutrients. The function
of the enterocytes is to absorb the nutrient molecules produced by
the digestive process. Disaccharidases & peptidases secreted by
absorptive cells & bound to microvilli in the brush border; hydrolyze the
disaccharides & dipeptides into monosaccharides & amino acids that
are easily absorbed. Lipid digestion occurs mainly as a result of the
action of pancreatic lipase and bile. In humans, most of the lipid
absorption takes place in the duodenum and upper jejunum.
b) Goblet cells (unicellular mucous glands):- they are present on the
villi & in the glands. They are irregularly scattered among the
absorptive cells, and resemble wine glass in shape. Their apical region is
distended with mucigen droplets, while the base of the cell forms a
slender stem or stalk. The nucleus tends to be flattened & the
surrounding cytoplasm strongly basophilic. These cells produce mucus,
whose main function is to protect & lubricate the lining of the intestine.
The frequency of goblet cell increases as the contents of the gut
become more solid towards the rectum.
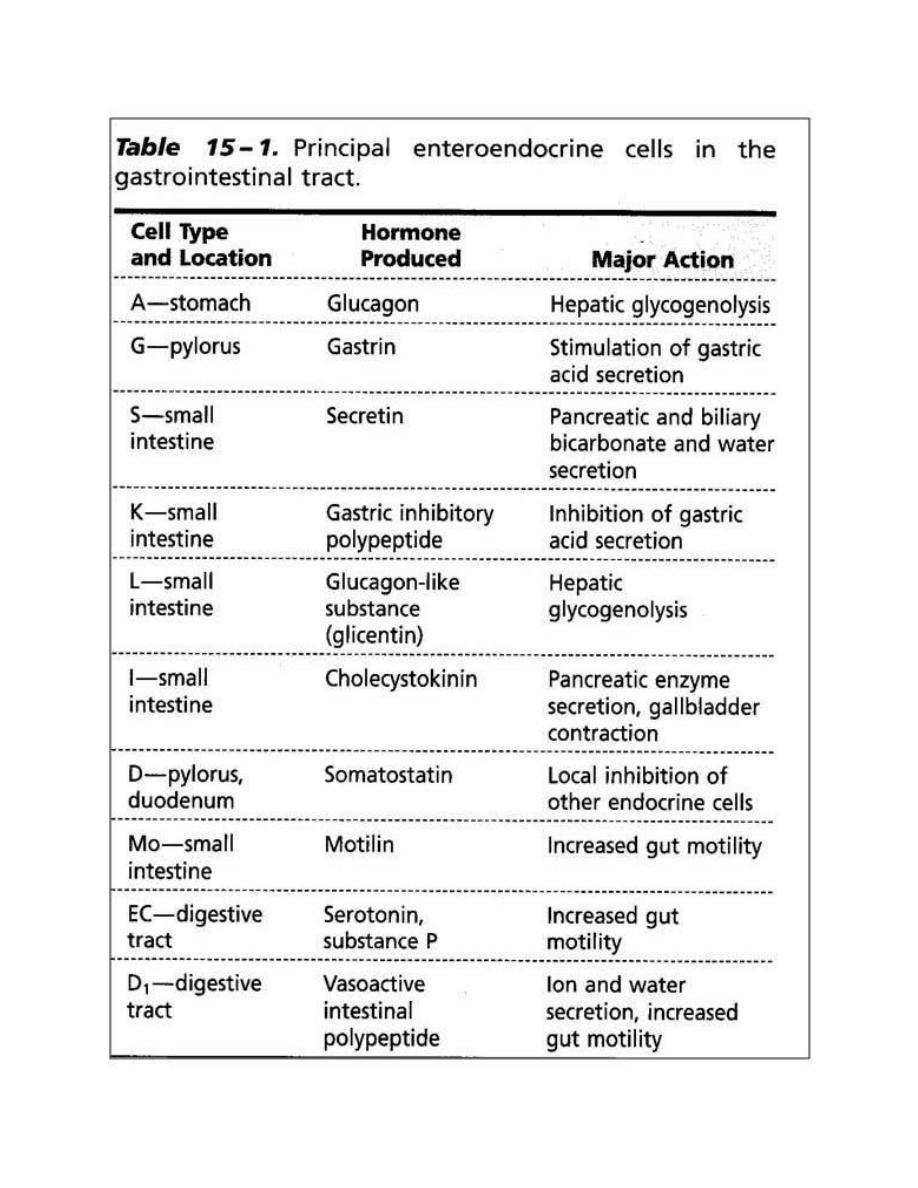
c) Enteroendocrine cells:- they are small, pyramidal cells & have
granules beneath the nucleus. Upon stimulation these cells release
their secretory granules by exocytosis, and the hormones may exert
paracrine (local) or endocrine (blood-borne) effects. They produce
hormones such as secretin, cholecystokinin, gastric inhibitory
polypeptide & motilin.
d) Paneth cells:- they are pyramidal in shape, with a round or oval
nucleus situated near the base & secretory granules in the apical
cytoplasm usually stain with acid dyes. They have the cytological
characteristics of cells actively secreting protein. Paneth cells are
located at the base of the intestinal glands of the small intestine.
Paneth cells produce lysozyme, an antibacterial enzyme whose function
is to digest the cell walls of some bacteria & may play a role in
controlling the intestinal flora. Lysozyme is present in the eosinophilic
secretory granules.
e) Stem cells (undifferentiated cells):- are located in the lower half of
the intestinal glands. In the small intestine the cells die by apoptosis in
the tip of the villi & replaced with new ones formed through mitosis of
stem cells (unidirectional cell flow).
M-cell (microfold cells, membranous epithelial cells):- are specialized
epithelial cells overlying the lymphoid follicles of Peyer's patches. They
are relatively flat cells whose apical surface is thrown into small folds
rather than microvilli. These cells are characterized by the presence of
numerous basal membrane invaginations that form pits containing
many intraepithelial lymphocytes & antigen- presenting cells
(macrophage). M cells can endocytose antigens & transport them to
the underlying macrophages & lymphoid cells, which then migrate to
the lymph nodes, where immune response to foreign antigens are
initiated. M cells represent an important link in the intestinal
immunologic system. The basement membrane under M cells is
discontinuous, facilitating transit between the lamina propria & M cells.
The lamina propria of the small intestine:- is composed of loose c.t.
with blood & lymph vessels, nerve fibers & smooth m cells. The lamina
propria constitutes the core of the intestinal villi & fills all the spaces
between the glands. The smooth m. cells are responsible for rhythmic
movements of the villi, which are important for absorption.
The muscularis mucosae of small intestine:- consists of an inner
circular & an outer longitudinal layers of smooth muscle. The inner
circular sends bundles up to lamina propria where they are attached to
the lacteals.
The lamina propria & the submucosa of the ileum contain
aggregates of lymphoid nodules known as Peyer's patches, an
important component of the GALT (gut-associated lymphatic tissue).
Each patch consists of 10-200 nodules & is visible to the naked eye as
an oval area on the anti-mesentric side of the intestine. There are
about 30 patches in the human, most of them in the ileum. Its covering
epithelium contains M cells.
2) The submucosa:-
contains in the initial portion of the duodenum,
clusters of coiled tubular glands that open into the intestinal glands.
These are the Brunner's glands. Their cells are of the mucous type,
produce alkaline secretions. It acts to protect the duodenal mucous
membrane against the effects of the acid gastric juice & to bring the
intestinal contents to the optimum pH for pancreatic enzyme action.
They also secrete urogastrone (a polypeptide hormone that enhances
epithelial cell division & inhibits gastric HCl production).
3) Muscularis externa:-
is composed of an inner circular & an outer
longitudinal layers of smooth m. The inner layer participates in the
formation of the ileocaecal sphincter. Auerbach's plexus present
between the 2 layers.
4) Serosa:-
covers all of the jejunum & ileum & part of the duodenum.
Adventitia covers the remainder of the duodenum.
Large intestine:-
It is a tube about 5 feet (1.6 meters) in length. It extends from the
ileo-caecal valve to the anus. It consists of the caecum, colon
(ascending, transverse, descending & sigmoid), rectum, anal canal&
appendix. It converts undigested material received from the small
intestine into feces by removing water & adding mucus. The usual 4
layers are present in the wall of the large intestine. No villi are present
in the large intestine. The intestinal glands are deeper (longer)
than in the small intestine and characterized by a great abundance of
goblet and absorptive cells. The intestinal glands of the large intestine
lack Paneth cells.
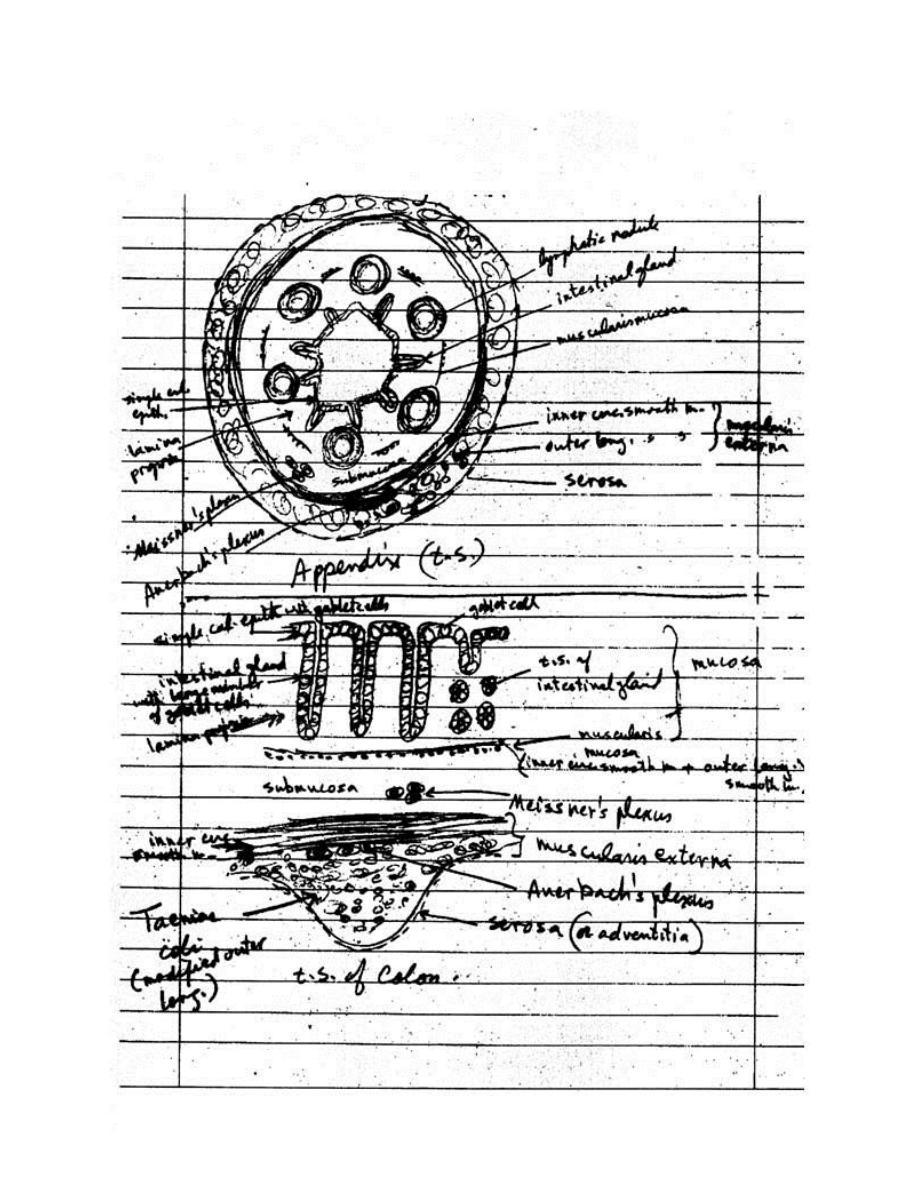
Appendix:-
is a small, slender, blind diverticulum of the caecum. It
has a narrow, stellate or irregular lumen. The villi are absent.
1. Mucosa of the appendix:-
a) Epithelium:- is simple columnar containing columnar absorptive cells
& goblet cells.
b) Lamina propria:- contains the intestinal glands(shorter & fewer) with
some goblet cells, columnar absorptive cells, stem cells & numerous
enteroendocrine cells. Lymphatic nodules with germinal centers are
very numerous & highly characteristic of the appendix. These nodules
originate in the lamina propria, because of their large size the nodules
may extend to the submucosa.
c) Muscularis mucosae:- is poorly developed.
2. Submucosa:- is relatively thick & highly vascular.
3. Muscularis externa:- is composed of an inner circular & an outer
longitudinal layers of smooth m.
4. Serosa:- completely surrounds the appendix.
Caecum & Colon:-
1-Mucosa:- is thicker than in small intestine.
a) Epithelium:- is simple columnar epithelium, containing numerous
goblet cells, absorptive cells & occasional enteroendocrine cells.
b) Lamina propria:- is similar to that of the small intestine. The
intestinal glands are longer & more closely packed, containing many
goblet cells, absorptive cells (have irregular short microvilli), stem cells
(in the lower third of the gland) and also few enteroendocrine cells.
They lack Paneth cells.
c) Muscularis mucosae:- consists of an inner circular & an outer
longitudinal layers of smooth m.
2-Submucosa:- contains blood & lymphatic vessels, nerves & Meissner's
plexus. It has no glands.
3-Muscularis externa of the caecum & colon:- is composed of an inner
circular & a modified outer longitudinal layer of smooth m. The outer
longitudinal layer of the smooth m. is gathered into 3 thick longitudinal
bands called taeniae coli. A thin layer of longitudinal smooth m. often
exists between the bands. The parasympathetic ganglia of the
Auerbach's plexus are present between the muscle layers.
In the living, the taeniae are in a state of partial contraction which
causes the intervening portions of the wall to bulge outward, forming
sacculations of the wall.
4-Serosa:- covers the transverse & sigmoid colon & caecum; however,
the ascending & descending colon are retroperitoneal & the outer layer
on their posterior surface is the adventitia . The serosa of colon is
characterized by the presence of many fat-filled outpocketings termed
appendices epiploicae
Rectum:-
is usually divided into 2 parts. The upper part (rectum
proper) measuring 5-7 inches in length, is structurally similar to colon.
The intestinal glands are longer than in colon & are filled with goblet
cells. There is no taeniae coli, the outer longitudinal muscle is complete
layer (evenly distributed). The lower part is the upper part of the anal
canal.
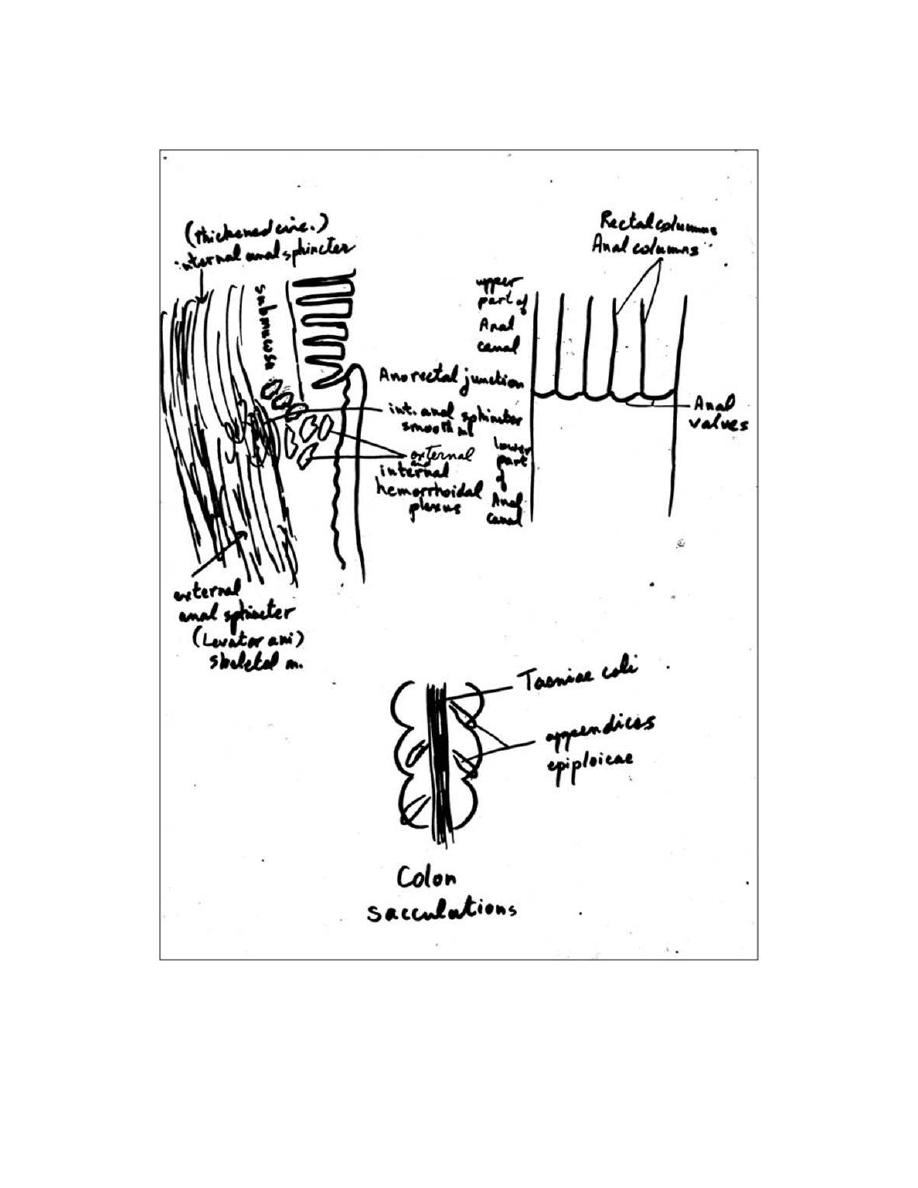
Anal canal:-
in the upper part of the anal canal, there are permanent
longitudinal folds of the mucous membrane, the rectal columns(anal
columns) of Morgagni. The bases (distal ends) of these columns are
connected by transverse folds of the mucosa, the anal valves (ano-
rectal junction). Above the anal valves, the mucosa is lined by simple
columnar epithelium, becomes stratified squamous non-keratinized
distal to the anal valves, and changes to stratified squamous keratinized
(epidermis) at the anus. The intestinal glands disappear at the ano-
rectal junction (anal valves) & also the muscularis mucosae disappear.
Two prominent venous plexuses are associated with the anal canal,
the internal & external hemorrhoidal plexuses located in the
submucosa & the lamina propria of the upper & lower part of anal
canal respectively. Hemorrhoids develop from chronic dilation of these
vessels. In the lower end of the anal canal, there are the prominent
circumanal glands (apocrine type of sweat gland) of the perianal skin.
Anal muscularis externa:- is composed of an inner circular & an outer
longitudinal layers of smooth m. The inner circular layer forms the
internal anal sphincter.
The diameter of the anal canal is controlled by two sphincters:
1. The internal anal sphincter: is composed of smooth muscle and is
under autonomic control.
2. The external anal sphincter: is composed of skeletal muscle and is
under voluntary control.
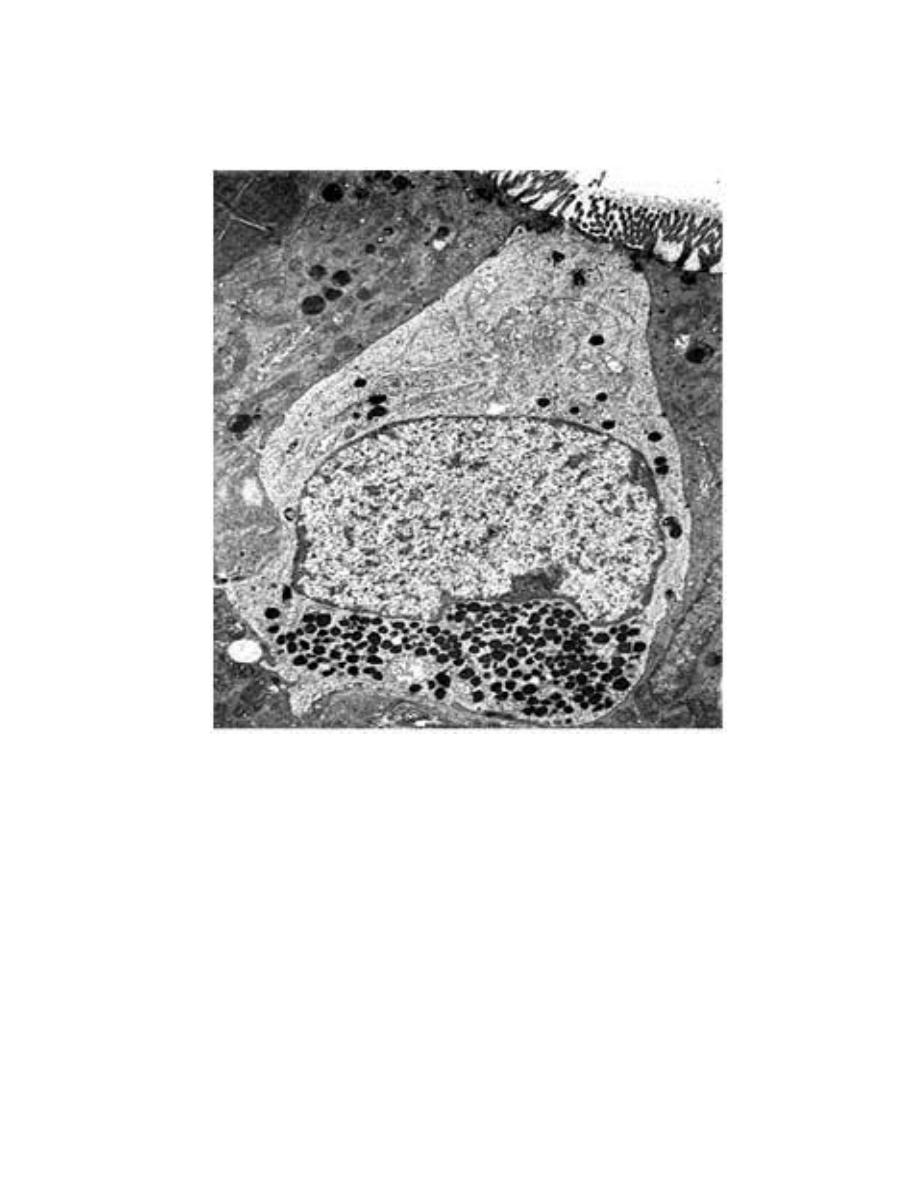
Electron micrograph of an enteroendocrine cell (open type) of the
human duodenum. Note the microvilli in its apex. x6900. (Courtesy of
AGE Pearse.)
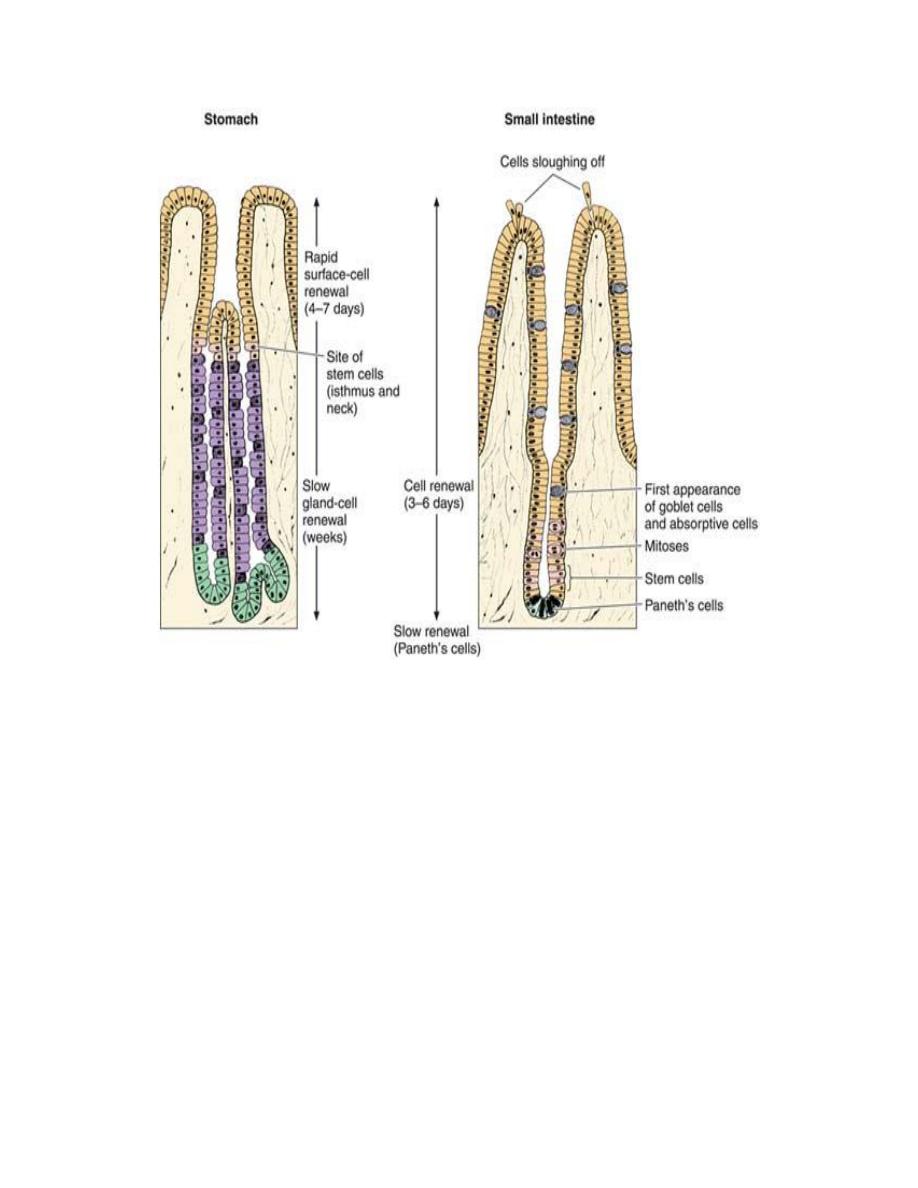
Regeneration of the epithelial lining of the stomach and small
intestine. Note differences in the location of stem cells.
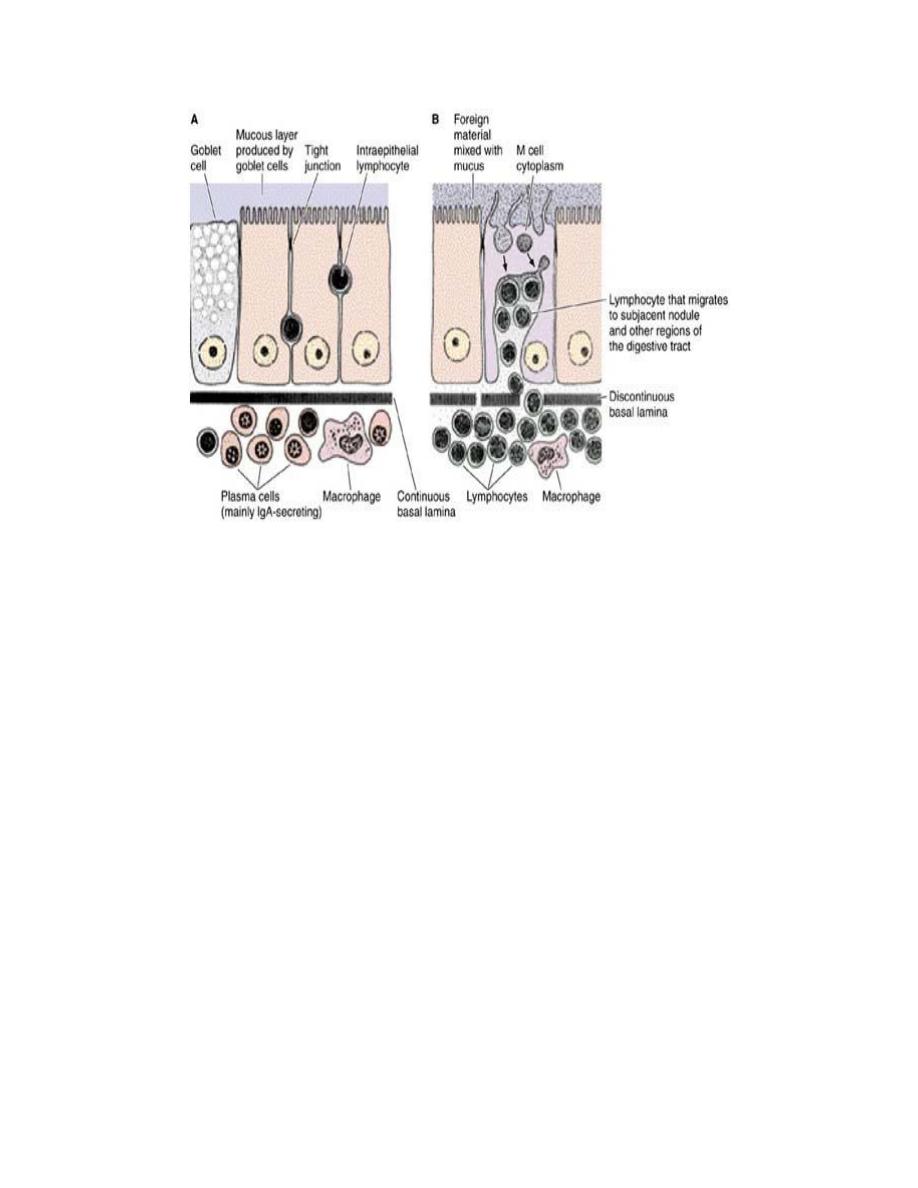
Some aspects of immunologic protection of the intestine. A: A
condition that is more frequent in the upper tract, such as in the
jejunum. There are many IgA-secreting plasma cells, scattered
lymphocytes, and some macrophages. Note that the lymphocytes in
the epithelial lining are located outside the epithelial cells, and below
the tight junctions. B: A condition that is more frequent in the ileum,
where aggregates of lymphocytes are located under M cells. The M
cells transfer foreign material (microorganisms and macromolecules)
to lymphocytes located deep in the cavities of the M cells.
Lymphocytes spread the information received from this foreign
material to other regions of the digestive tract, and probably to other
organs, through blood and lymph.
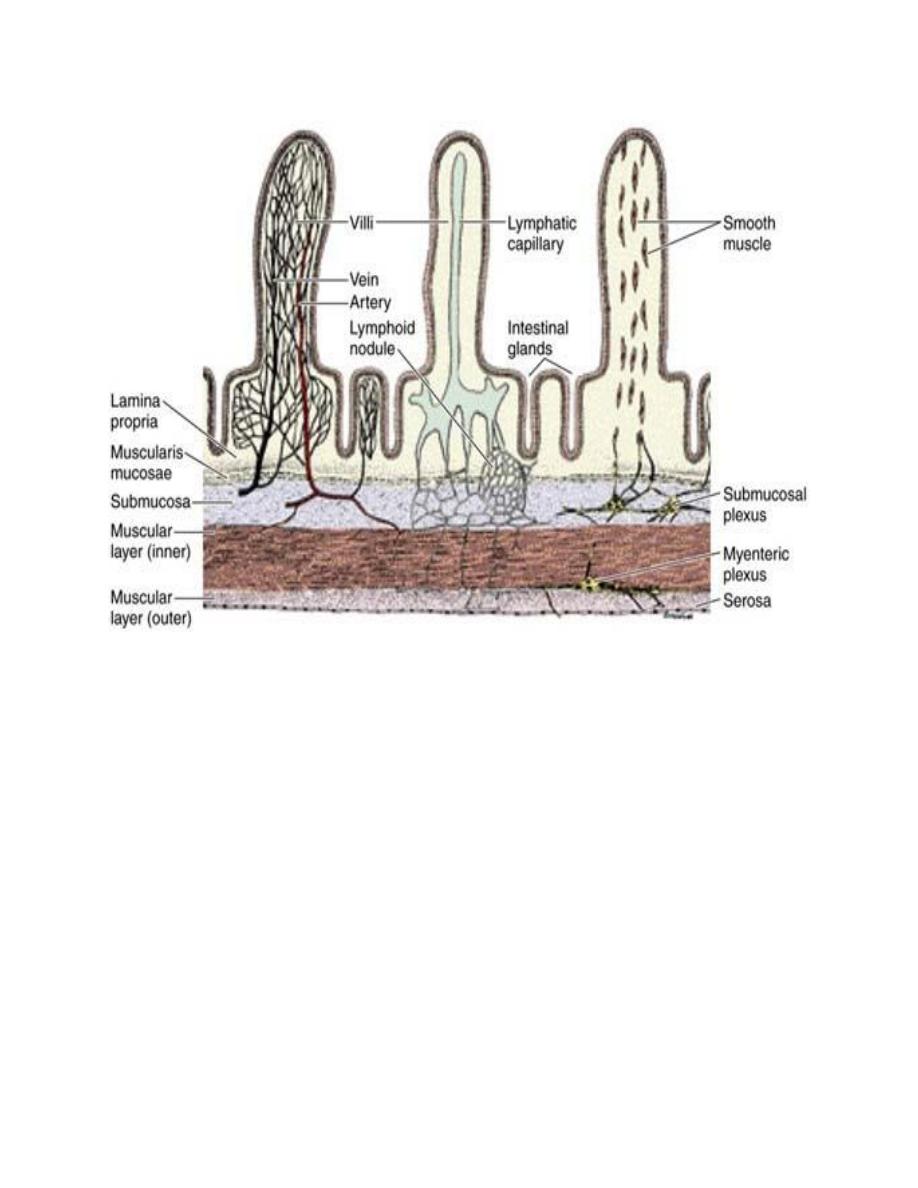
Blood circulation (left), lymphatic circulation (center), and innervation
(right) of the small intestine. The smooth muscle system for
contracting the villi is illustrated in the villus on the right.
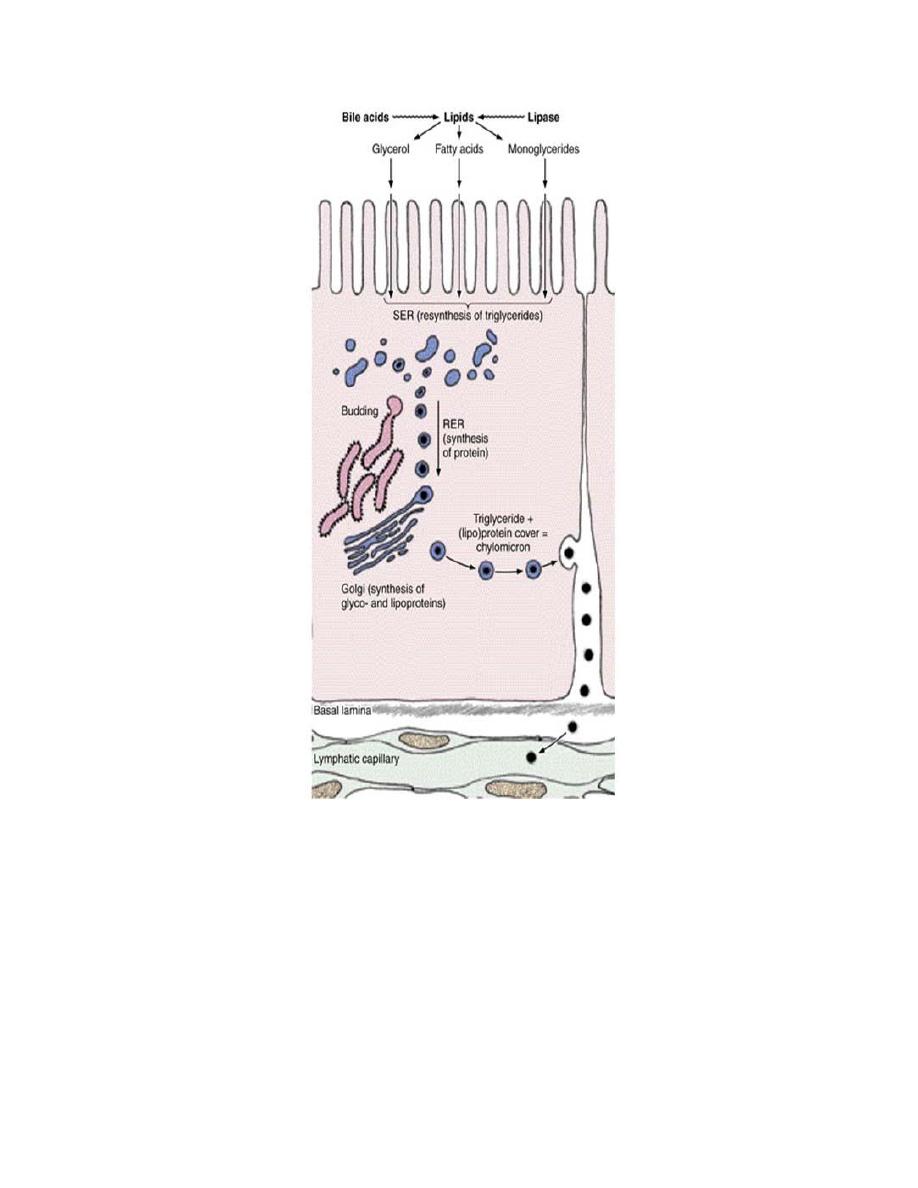
Lipid absorption in the small intestine. Lipase promotes the hydrolysis of lipids to monoglycerides and fatty
acids in the intestinal lumen. These compounds are stabilized in an emulsion by the action of bile acids. The
products of hydrolysis cross the microvilli membranes passively and are collected in the cisternae of the
smooth endoplasmic reticulum (SER), where they are resynthesized to triglycerides. These triglycerides are
surrounded by a thin layer of proteins that form particles called chylomicrons (0.2—1 micrometers in
diameter). Chylomicrons are transferred to the Golgi complex and then migrate to the lateral membrane,
cross it by a process of membrane fusion (exocytosis), and flow into the extracellular space in the direction of
the blood and lymphatic vessels. Most chylomicrons go to the lymph; a few go to the blood vessels. The long-
chain lipids (>C12) go mainly to the lymphatic vessels. Fatty acids of fewer than 10—12 carbon atoms are not
reesterified to triglycerides but leave the cell directly and enter the blood vessels. RER, rough endoplasmic
reticulum. (Based on results of Friedman HI, Cardell RR Jr: Anat Rec 1977;188:77.)