INVESTIGATIONS OF GASTROINTESTINAL DISEASES
Lecture 1 and 2 د. اسماعيل
Note: 44 pictures were showed to students during power point presentation
The following are the main investigations of gastrointestinal tract:
1. Radiological test of structure (imaging): Represent the largest group and
includes (plain abdominal X-ray, barium study, ultrasonography of abdomen.
CT and MRI of abdomen with magnetic resonance choliangiopancreatography
(MRCP) of biliary and pancreatic ducts.
2. Endoscopy: Oesophagogastroduodenoscopy (OGD) for upper GIT problems
proximal to ligament of Teirtz ( oesophagus, stomach and duodenum up to
second part of duodenum) , endoscopic retrogradecholiangiopancreatography
(ERCP) sigmoidoscopy, colonoscopy, enteroscopy, and capsule endoscopy
which is especially useful for detection of obscure (not clear or hidden)
bleeding which can not detected by upper or lower endoscopy.
3. Test of infection.
4. Test of function.
5. Tests for malabsorption ( will be discussed in otherfuther lectures).
6. Radioisotop study: May be useful for detection of active bleeding.
7. Biopsy and histopathology.
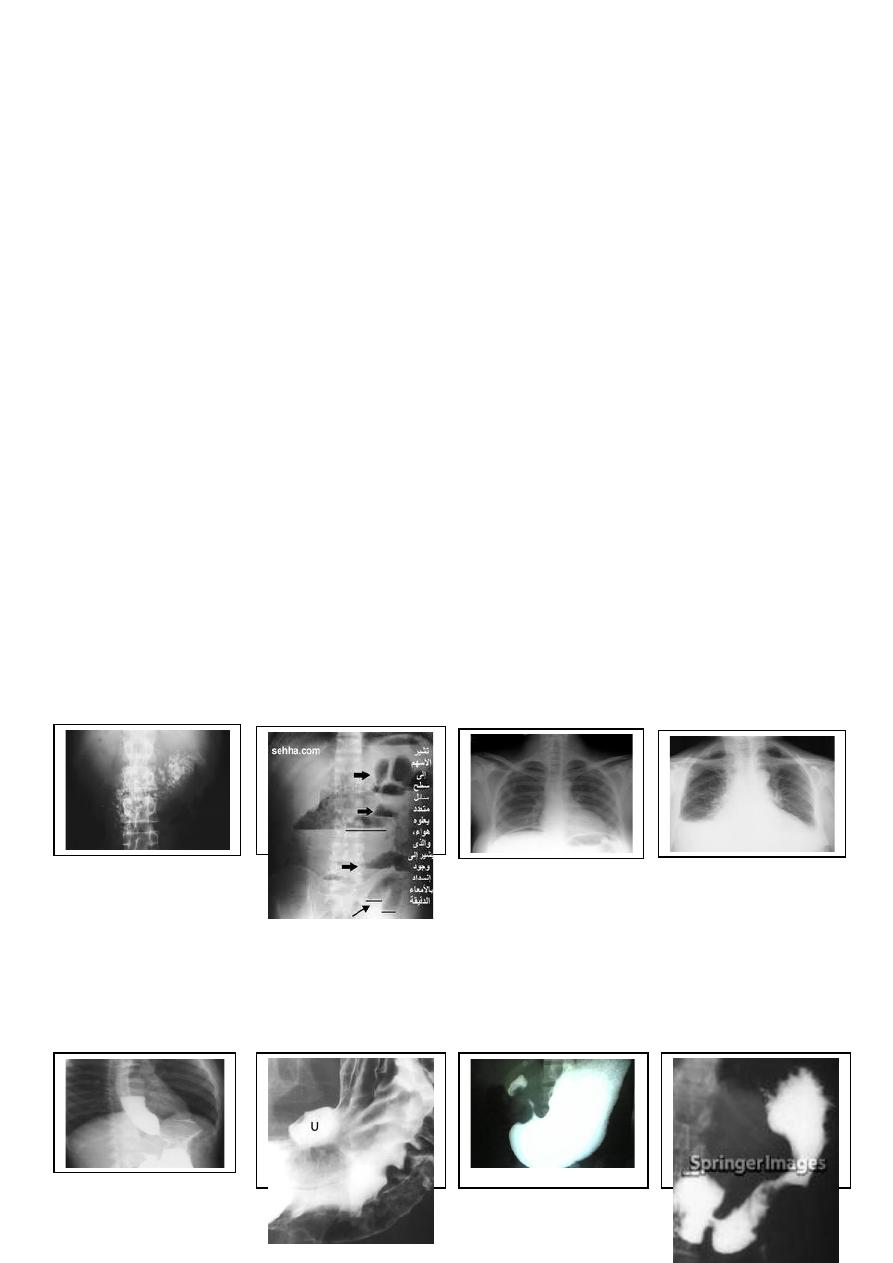
IMAGING:
Plain X-ray: May shows soft tissue outlines like liver, spleen, and kidney.
Calcification in such organs as well as in pancreas (chronic pancreatitis) may be seen.
Fluid levels in case of paralytic ileus and intestinal obstruction, x-ray of chest may
show crescent shaped gas under right dome of diaphragm in case of perforated bowel
as well as unrecognized chest problems like pleural effusion. All pathological GIT
conditions are presented during power point presentations.
Contrast studies: Using barium sulphate and other contrast media. Double contrast
may show small mucosal lesions. Barium studies are useful for detection of filling
defects (e. g. tumor mass), strictures, erosions, ulcers, fistula (as in Crohn’s disease)
and motility disorders under screen (e. g. motility disorders of oesophagus like
achalasia). Barium sulphate is harmless inert ssubstance but may accumulate
proximal to obstruction and become more solid. Colonoscopy may postpone several
days after barium study to obtain clear view. Water soluble contrast is usually used
during CT scan and MRI examinations.

US, CT scan and MR
These non-invasive investigations are commonly used for diagnosis of many
intraabdominal diseases and can detect even very small lesions.
US: Can detect abdominal masses and cysts, tumours, abscesses, organomegaly,
ascites, biliary tract dilatation, gall stones and guides needle aspiration and biopsy of
lesion. It can not detect small lesions and gases in bowel and obesity may obscure
lesions.
CT scan: Assessment of pancreatic diseases, hepatic tumors, tumor staging. Can
detect small lesions.
MRI:
Hepatic
tumour
staging,
MRCP
(magnetic
resonance
cholangiopancreatography). It indicated in perianal and pelvic disease and for
detection of Crohn’s fistula. Contra-indicated in presence of metallic prosthesis and
cardiac pacemaker. It is expensive.
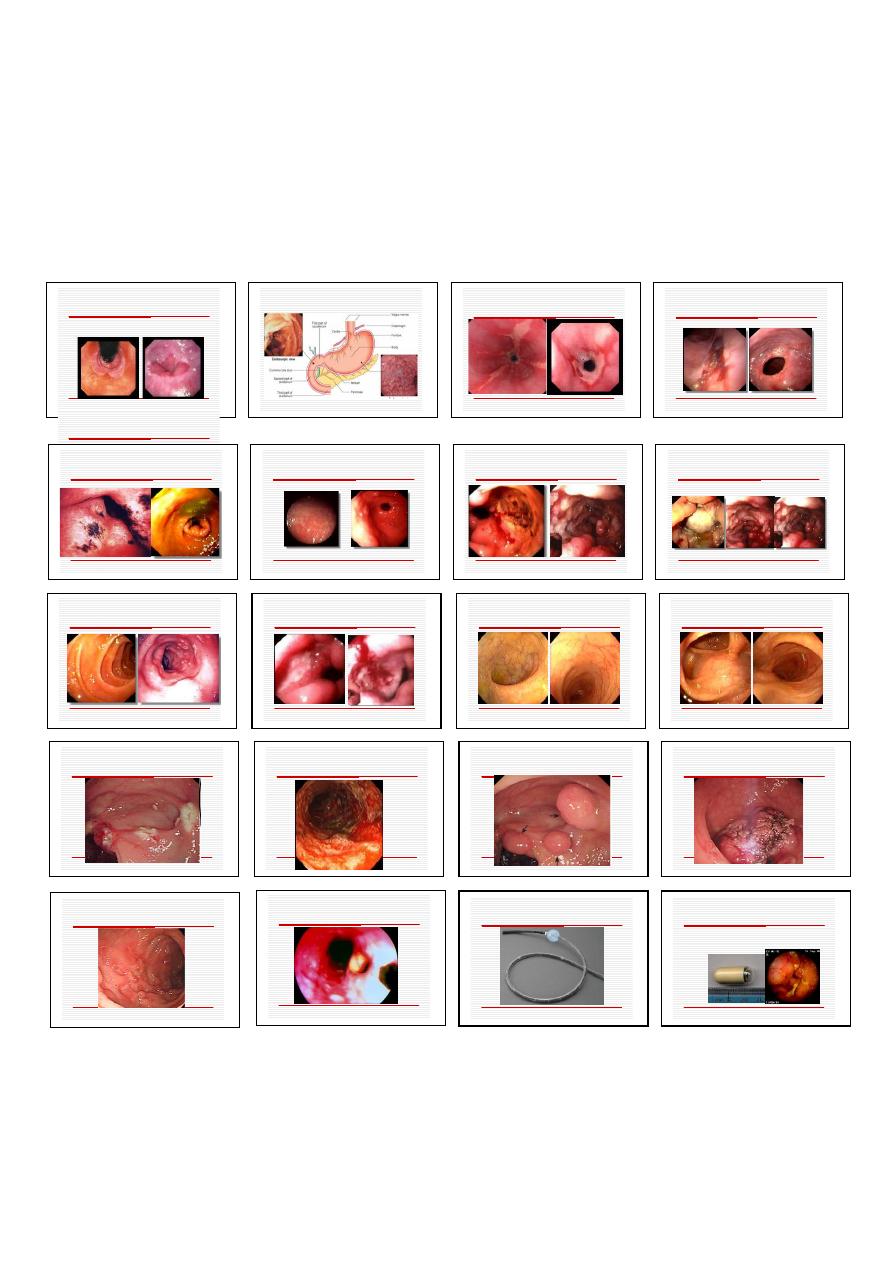
ENDOSCOPY: Two main types: 1. Old fibrooptic type. 2. New video
endoscopes.Uses: They are used for both diagnostic and therapeutic purposes.
Upper GIT endoscopy: Also called OGD which means oesophagio-gastro
duodenoscopy. The tube is 100 cm in length and reaches up to second part of
duodenum. The end-view type is used for this purpose (side-view scopes are used for
ERCP procedures).
Indications:
1. Dyspepsia in patients 55 years old or those with alarm symptoms.
2. Atypical chest pain
3. Dysphagia.
4. Vomiting (prolonged and/or severe)
5. Weight loss
6. Acute or chronic gastrointestinal bleeding.
7. Suspicious barium meal 8. Duodenal biopsy in the investigation of malabsorption.
9. Therapeutic procedures.
MRCP
Contraindication:
1.Shocked patient. 2. Recent myocardial infarction or unstable angina. 3. Severe
respiratory disease. 4. Atlantoaxial subluxation. 5. Possibility of visceral perforation.
Complications:
Cardiorespiratory depression after heavy sedation especially in elderly or shocked
patient. 2. Aspiration pneumonia. 3. Perforation and bleeding especially during
therapeutic procedures. 4. Infective endocarditis in people with valve lesions who
underwent examination without prophylaxis.
Colonoscopy:
Indications: 1. Suspected inflammatory bowel disease. 2. Chronic diarrhea. 3.
Altered bowel habit. 4. Rectal bleeding or anaemia. 5. Assessment of abnormal
barium enema. 6. Colorectal cancer screening. 7. Colorectal adenoma follow-up. 8.
Therapeutic procedures.
Contraindications: 1. Severe acute ulcerative colitis. 2. Severe shock 3. Perforation.
4. Recent ischemic heart disease 5. Severe acute infections.
Complications: 1. cardiopulmonary depression due to excessive sedation 2. Bleeding
and perforation 3. Infective endocarditis in susceptible patient when antibiotic
prophylaxis was not given.
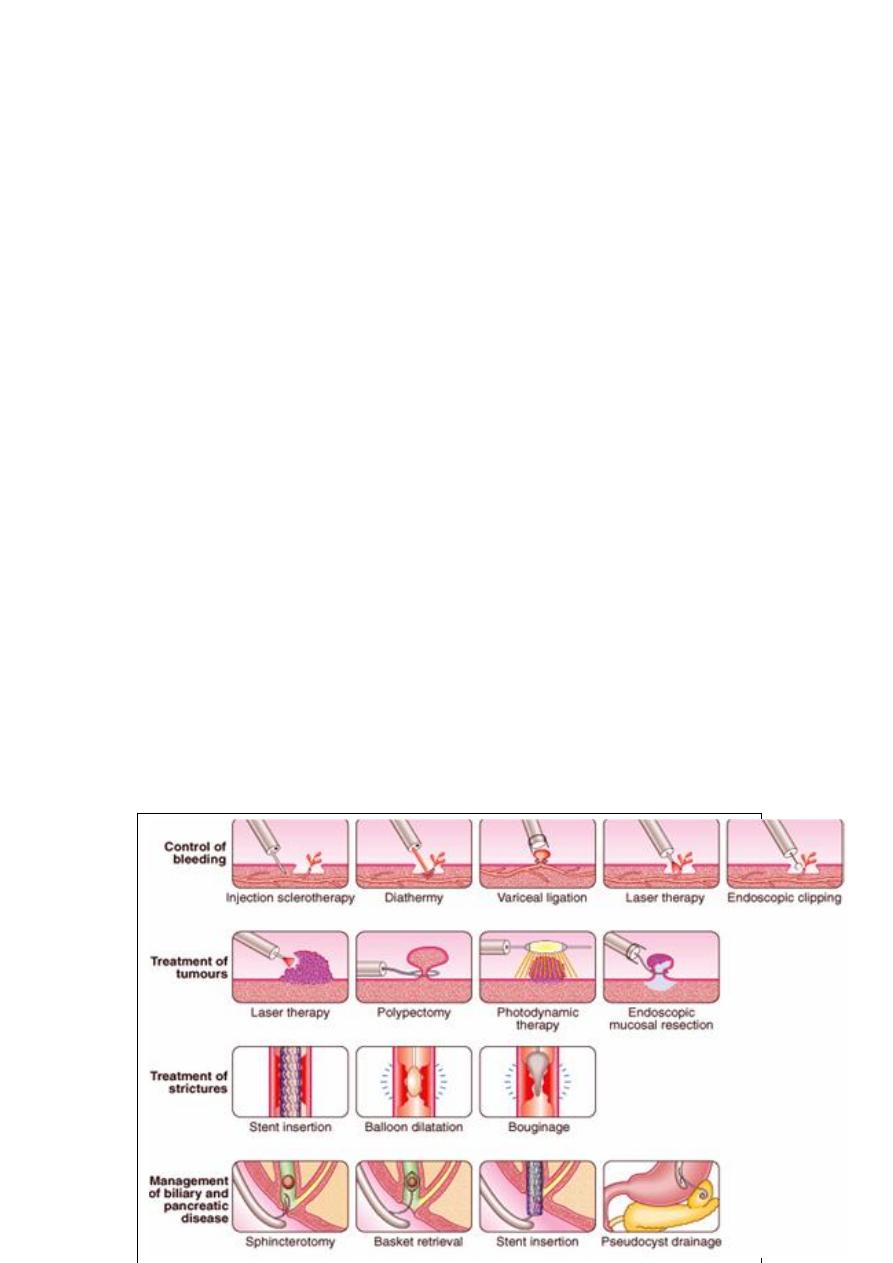
Therapeutic procedures which can be done through endoscopy: لالطالع فقط
1. Control of bleeding by using: injection sclerotherapy (for varices), variceal ligation
(for varices), diathermy, lasser therapy, endoscopic clipping and injection of diluted
adrenaline into the lesion.
2. Treatment of tumours and polyps.
3. Therapeutic procedures during ERCP (Endoscopic retrograde
cholangiopancreatography) for biliary and pancreatic disorders like stone removal.
4. Treatment of strictures by using of ballons and by dilators e. g. oesophageal
strictures.
Enteroscopy:
This is another type of endoscopy of different subtypes used for diagnosis of small
bowel lesions. It needs special experience by examiner for its use.
Capsule endoscopy:
Especially useful in cases of small bowel pathology as in cases of obscure GIT
bleeding.
Endoscopic view of normal lower
oesophagus
Endoscopic view of normal lower
oesophagus
Normal endoscopy (stomach and
duodenum
ESOPHAGITIS
Reflux esophagitis with ulcer
hemorrhage
Erosive and bile induced gastritis
Other types of gastritis
Antral gastric carcinoma
GASTRIC CARINOMA BODY,
ANTRUM
A. Normal duodenum. B. Duodenitis
DU and bleeding DU
Normal rectum and sigmoid
Normal splenic flexure and
transverse colon
Colonic ulceration. Malignant?
Colonoscopy: Ulcerative colitis
Colonic polyps
Colonic carcinoma
Colonoscopy: Crohn’s colitis
Colonoscopy: Crohn’s disease
CAPSULE ENDOSCOPY
Especially useful in cases of small bowel
pathology as in cases of obscure GIT
bleeding.
ENTEROSCOPE

Tests of infection:
e. g. stool cultures in cases of dirrhea, Three noninvasive tests for H. pylori detection:
serological tests for detection of anti-H. Pylori antibodies, stool antigen detection and
breath test for H. pylori. The latter is considered the best practical test.
Note: Others (invasive tests) for H. pylori detection (Urease test and histopathology
with special staining ) are not used routinely in practice.
Tests of function:
for study of motility disorders of oesophagus, intestine and colon. It also uses for
gastric emptying disorders e. g. gastro-paresis when no structures defects are detected
by usual investigation. The tests also use for small intestine transit time (lactulose-
hydrogen breath test).
Radioisotope tests:
e. g. in diagnosis of MECKEL’S DIVERTICULUM (an abnormal gastric mucosa
presents in a diverculum in upper part of intestine and may lead to GIT bleeding
undetected by usual investigation). Also used for detection of bacterial overgrowth in
intestine and active intestinal bleeding.
Biopsy and pathology:
1. study of duodenal and jejunal biopsy material for diagnosis of celiac disease
(mucosal abnormalities). 2. To diagnose lesions like: e. g. inflammatory bowel
disease (e.g. cryptic anbscess in UC and granuloma in Crohn’s disease) and tumors. 3.
Also used for diagnosis of infection like Giardiasis, H. pylori and fungal infection. 4.
Some time enzyme study is done from biopsy material.
Breath test for H. pylori
Breath test for H. pylori
H. Pylori: Rapid serological test
Small bowel
bleeding demonstrated
by Tc-99m erythrocyte
Histopathology: Ulcerative colitis
(cryptic abscess)
Histopathology: Celiac disease
Granuloma formation: Crohn’s disease
