Dr. Ayad Abbas
Lec. 2
ACID BASE BALANCE
Tues. 30 / 9 / 2014
Published by : Ali Kareem
مكتب اشور لالستنساخ
5102
-
5102

1
Surgery
Acid Base Balance
Lec 2:
30/9/2014
د.اياد عباس
◊ pH: is a negative logarithm of molar H
+
concentration of solution.
◊
If hydrogen ion of pure H
2
O at room temperature is equal to
1/10.000.000 mol/L → [H
+
] = 1/10.000.000 → [H
+
] = 10
-7
→ log [H
+
]
= -7 → -log [H
+
] = 7→ pH = 7.
Neutral solution → [H
+
] = [OH
-
] = 10
-7
→ pH =7
Acidic solution → [H
+
] > [OH
-
] → pH < 7
Alkaline solution → [H
+
] < [OH
-
] → pH > 7
◊
In SI system: pH unit not used now and the acid-base status measured
by direct [H
+
]/L and expressed in nanomol/L.
nano= 10
-9
, neutral solution [H
+
] = 100 nmol/L
◊ Normal blood pH = 7.4 (+ or -) 0.05 = 7.35-7.45
◊ Range of blood pH which compatible with life is only (7-7.8) which
corresponds to a range of 6 times change in hydrogen ion concentration.
◊ Acidosis : process that tend to lower pH.
◊ Alkalosis: process that tend to rise pH
◊ Acidaemia: ↓ in blood pH < 7.35
◊ Alkalaemia: ↑ in blood pH > 7.45
Compensatory Mechanism
Physiological responses to changes in [H
+
] are characterized by 3 phases:
1.Immediate chemical buffering.
2.Respiatory compensation.
3.Slower but more effective renal response that may nearly normalize
arterial pH.
2
Body buffers
Physiological important buffers are:
1.Bicarbonate (H
2
CO
3
/HCO
3
-
): is most important buffering in the
extracellular fluid.
H
2
O + CO
2
H
2
CO
3
H
+
+ HCO
3
-
Normally eliminated by lung and not ↑ PaCO
2
CO
2
+ H
2
H
2
CO
3
+ NaCl HCl + NaHCO
3
2.Haemoglobin (HbH/Hb
-
): although restricted inside RBC, but it is an
important buffer in the blood.
H
+
+ KHb HHb +K
+
3.Protein other than Hb: play a major role in buffering of intracellular
fluid.
Protein possess both acidic & alkaline groups.
.
carboxyl group
Acidic group called
.
amino group
Alkaline group called
NH
2
+
H
+
NH
3
Protein
COOH + OH
-
COO + H
2
O
3
4.Phosphate (H
2
PO
4
-
/ HPO
4
-2
): it is important urinary buffer.
↑ [H
+
] HCl + Na
2
HPO
4
NaH
2
PO
4
(kidney) +
NaCl
di (Na) phosphate mono (Na) phosphate
↑[OH
-
] NaOH + NaH
2
PO
4
NaHPO
4
+ H
2
O
excreted by kidney
5.Amonia (NH
3
/NH
4
+
): it is also important urinary buffer.
NH
3
+ H
+
NH
4
(excreted by kidney)
Respiratory compensation
↑pH → hypoventilation → ↑PaCO
2
Change in pH (sensed by
chemoreceptors
in brain stem) ↓ pH → hyperventilation → ↓PaCO
2
Renal compensation
this by the following:
1.Ability of kidney to control the amount of HCO
3
-
reabsorption.
2.Ability of kidney to form new HCO
3
-
.
3.Ability of kidney to eliminate H
+
in the form of titrable acid and
ammonium ion.
EXAMPLES:
► H
+
+ HPO
4
-2
H
2
PO
4
(excreted by kidney)
► NH
3
+ H
+
NH
4
(excreted by kidney)
4
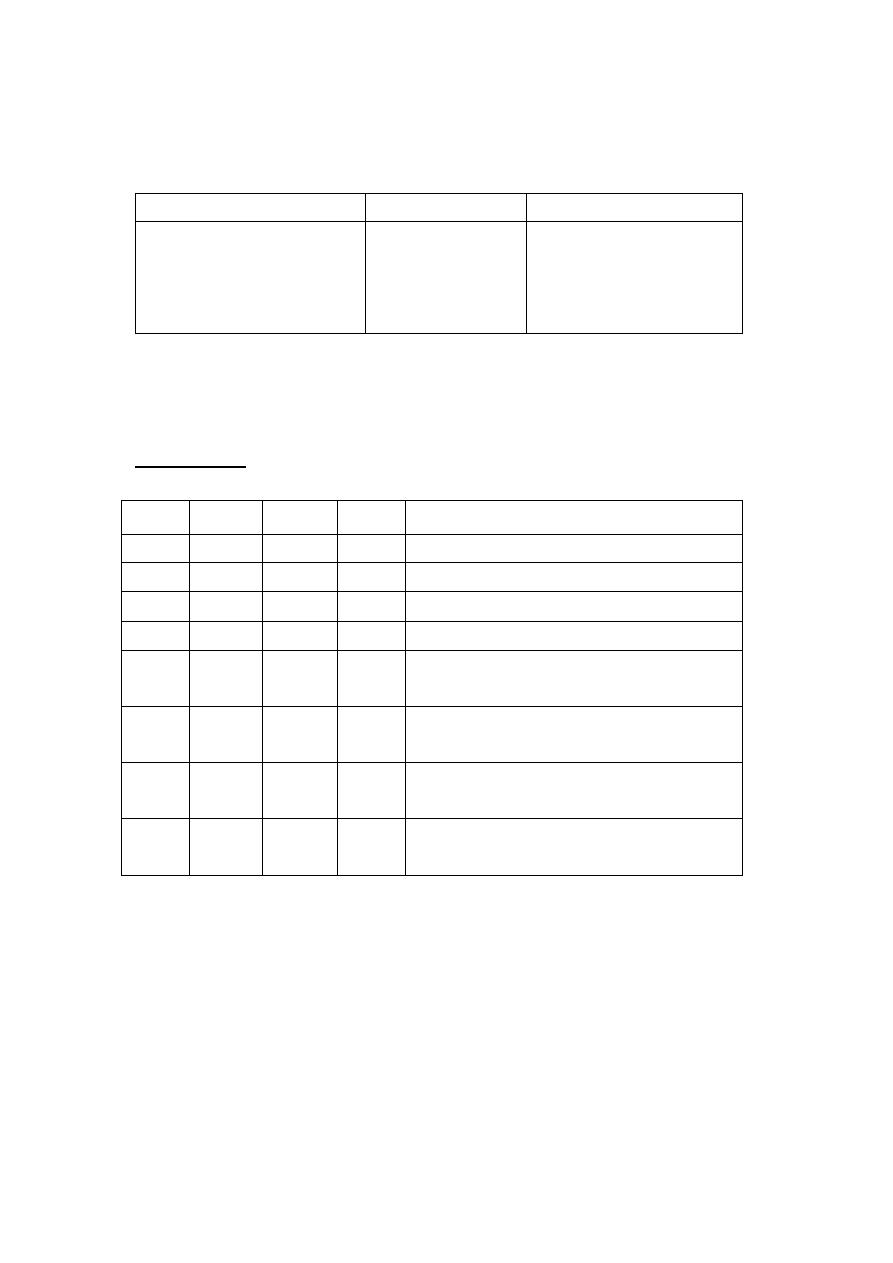
Clinical disorders
Compensatory changes
Primary changes
Disorder
↑ HCO
3
↓ HCO
3
↓ PaCO
2
↑ PaCO
2
↑ PaCO
2
↓ PaCO
2
↓ HCO
3
↑ HCO
3
Respiratory acidosis
Respiratory alkalosis
Metabolic acidosis
Metabolic alkalosis
Normally: PaCO
2
= 40
+
-
5 , HCO
3
= 22
+
-
2 , SBC
*
= 24
+
-
2, BE
**
=
+
-
3 -
zero.
EXAMPLES:
Diagnosis
BE
HCO
3
PaCO
2
pH
Uncompensated metabolic acidosis
-20
10.8
41
7.05
Uncompensated metabolic alkalosis
+16
38
42
7.59
Uncompensated respiratory acidosis
-2
22
90
7.15
Uncompensated respiratory alkalosis
Zero
24
21
7.58
Metabolic acidosis compensated by
respiratory alkalosis
-15
13.4
23
7.27
Metabolic alkalosis compensated by
respiratory acidosis
+20
42.8
55
7.55
Respiratory acidosis compensated by
metabolic alkalosis
+16
38.5
85
7.30
Respiratory alkalosis compensated by
metabolic acidosis
-10
16.5
20.5
7.46
* SBC: it is plasma [HCO
3
] from fully oxygenated (PaO
2
= 100) blood
which has been equilibrated to PCO
2
40 mmHg at 37
○
C.
** BE: Base Excess: is an amount of strong acid or base required to
titrate the pH to 7.4 at PCO
2
40 mmHg.

5
Physiological effect of acidosis
1.pH < 7.20 → direct myocardiac depression and ↓ peripheral vascular
resistance → hypotension.
2.Tissue hypoxia (although O
2
dissociation curve shift to the left)
3.Hyperkalaemia
4.CNS depression mainly in respiratory acidosis (CO
2
narcosis) → ↑
cerebral blood flow → ↑ intracranial pressure.
I.Respiratory acidosis
1
○
↑ in PaCO
2
. It is of two types:
1.Acute respiratory acidosis: the compensatory mechanism to acute (6-12
hr) is limited.
2.Chronic respiratory acidosis: renal compensation characterizes chronic
respiratory acidosis, it is appreciable after (12-24 hr) and may not peak
until 3-5 days. Plasma HCO
3
↑ ~ 4mmol/L for each 10 mmHg ↑ PaCO
2
above 40 mmHg.
Causes of respiratory acidosis:
1.Alveolar hyperventilation
● CNS depression e.g: 1.cerebral ischemia 2.cerebral trauma 3.drug
induced
● Neuromuscular disorder: myopathy, neuropathy
● Chest wall abnormality e.g kyphoscoliosis
● Pleural abnormality e.g pneumothorax, pleural effusion
● Airway obstruction: foreign body, tumor → upper airway
asthma, COPD → lower airway
● Paranchymal lung disease:1.Pulmonary Oedema 2.Pulmonary Emboli
3.Pneumonia 4.Aspiration 5.Interstitial lung disease
2.↑ CO
2
production
● ↑ in enteral or paraentral nutrition of carbohydrate
● Intense shivering
● Prolong seizure activity
● Thyroid storm
● Excessive thermal injury

6
Treatment:
● Treatment of the cause
● May → respiratory depression → mechanical ventilation
● I.V NaHCO
3
is rarely necessary (i.e not used)
II.Metabolic acidosis
1
○
↓ in HCO
3
, pulmonary compensation by marked hyperventilation to ↓
PaCO
2
does not completely normalize pH.
Anion Gap: defined as the difference between major measured cations
and major measured anions.
Anion gap = [Na
+
] -([Cl
-
] + [HCO
3
-
]) normally (9-15).
Causes:
Those with ↑ anion gap, with normal anion gap (hyperchloraemic).
1.Incresed anion gap
● ↑
production of non volatile acids e.g renal failure, DKA (diabetic
ketoacidosis), lactic acidosis.
● Ingestion of toxins e.g salicylatye, methanol, sulfer
●
Rhabdomyositis
2.Normal anion gap
● ↑ GIT loss of HCO
3
: diarrhoea, ingestion of CaCl
2
/MgCl
2
, fistula
(pancreatic, biliary, small bowel)
● ↑ renal loss of HCO
3
: renal tubular acidosis, hypoaldosteronism
● Dilutional: large amount of HCO
3
free fluid
● Total paraenteral nutrition
● ↑ intake of chloride containing acid e.g ammonium chloride
Treatment:
● ph < 7.2 → Na HCO
3
(8.4 %) should be given
NaHCO
3
= BE X 30% X body weight (giving 1/2 the dose and reassess
the values).
● Treatment of the cause
7
Alkalosis (physiological effect)
1.Hypokalaemia
2.Difficult to give up O
2
to tissue → hypoxia.
3.↓ ionized Ca
+2
→ circulatory depression and neuromuscular irritability.
4.Respiratory alkalosis → ↓ cerebral blood flow, ↑ systemic vascular
resistance and may → coronary vasospasm.
I.Respiratory alkalosis
1
○
↓ in PaCO
2
, by inappropriate ↑ in alveolar ventilation relative to CO
2
product.
It is compensated by ↓ [HCO
3
] in plasma.
Causes:
● Central stimulation: 1.pain 2.anxiety (hystria) 3.stroke 4.ischemia
5.fever 6.infection 7.drug induced e.g salicylate
● Peripheral stimulation: 1.hypoxia 2.high altitude 3.pulmonary disease
(CHF, pulmonary oedema, pulmonary emboli, asthma (severe))
● Iatrogenic: ventilator induced
Treatment:
● Treatment of the cause is enough
● For severe (pH > 7.6) i.v HCl or NH
4
Cl
4
(ammonium chloride) my be
indicated
II.Metabolic alkalosis
1
○
↑ in HCO
3
Causes:
1. Chloride sensitive: those causes associated with ↓ NaCl and ECF
depletion
● GIT: vomiting, gastric drainage, chloride diarrhoea
● renal: diuretic
● sweat: cystic fibrosis
2.Chloride resistance: those associated with enhanced mineralocorticoid
activity
● ↑ mineralocorticoid activity: hyperaldosteronism, cushing syndrome
3.Miscellanous
8
● massive blood transfusion
● alkaline treatment with renal insufficiency
● hyper Ca
+2
e.g metastasis
Treatment:
● Treatment of underlying cause
● For chloride sensitive causes i.v normal saline and K
+
replacement
● when pH > 7.6 i.v : 1.HCl 2.ammonium chloride 3.Vit.C (5-10 g/day)
4.haemodialysis may be considered
Done By:
Ali Malik
