Dr. Ramez
Lec. 2
ABDOMINAL INCISIONS
WOUND HEALING
Tues. 3 / 3 / 2015
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2014 – 2015
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
2
ABDOMINAL INCISIONS
A cut produced surgically by a sharp instrument that creates an opening into the
abdomen .
When choosing an incision these three should be achieved :
Accessibility
Extensibility
Security
Re-entry into the abdominal cavity is best done through the previous laparotomy
incision. This minimizes further loss of tensile strength of the abdominal wall by
avoiding the creation of additional fascial defects
CLASSIFICATIONS :
Vertical incision
Midline incisions
Paramedian incisions
Transverse and oblique incisions
Kocher's subcostal Incision
Chevron (roof top Modification )
Mercedes Benz Modification
Mc Burney’s grid iron or muscle splitting incision.
Rutherford morison incision
Pfannenstiel incision
Maylard Transverse Muscle cutting Incision
Transverse muscle dividing incision
Thoracoabdominal incisions
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
3
MIDLINE
the most common incision
three types :
Upper Midline Incision
From xiphoid to above umbilicus.
Skin
superficial and deep fascia
linea alba
extraperitoneal fat
peritonium.
Lower Midline Incision
From the SUPERIOR umbilicus to INFERIOR pubic symphysis
Full Midline Incision
From xiphoid to pubic symphysis inferiorly
Advantages :
Adequate exposure of most if not all of the abdominal viscera
It is almost bloodless.
No muscle fibers are divided.
No nerves are injured.
It is very quick to make as well as to close.
Disadvantages :
More painful.
Chest complications.
Wound infection, Ugly scar, Incisional hernia, etc.
PARAMEDIAN
2 to 5 cm lateral to the midline.
skin
fascia
anterior rectus sheath
The posterior rectus sheath or
transversalis fascia
extraperitoneal fat and peritoneum are then excised
allowing entry to the abdominal cavity
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
4
Skin and subcutaneous fat are divided along the length of the wound. The
medial portion of the rectus sheath then is dissected from the rectus muscle,
to which the anterior sheath adheres Once the rectus muscle is free of the
anterior sheath it can be retracted laterally because the posterior sheath is
not adherent to the rectus muscle. The posterior sheath and the peritoneum
which are adherent to each other, are excised vertically in the same plane as
the anterior fascial plane
Advantages :
Provide an access to the lateral structure such as the spleen or the kidney
The closure is theoretically more secure because the rectus muscle can act
as a support between the reapproximated posterior and anterior fascial
planes so lower risk of dehiscence and hernia as compared to midline
incision
Disadvantages :
Takes longer to make and close
results in atrophy of the muscle medial to the incision
The incision is laborious and difficult to extend superiorly as is limited by
costal margin.
Risk of epigastric vessels injury
TRANSVERSE AND OBLIQUE INCISIONS
KOCHER ‘S INCISION
Incision parallel to the right costal margin. started at the midline, 2 to 5 cm
below the xiphoid and extends downwards, outwards and parallel to and
about 2.5 cm below the costal margin
It shows excellent exposure to the gallbladder and biliary tract and can be
made on the left side to show access to the spleen.
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
5
CHEVRON (ROOF TOP)MODIFICATION
The incision may be continued across the midline into a double Kocher
incision or roof top approach which provide excellent access to the upper
abdomen particularly in those with a broad costal margin
MERCEDEZ BENZ
consists of bilateral low Kocher’s incision with an upper midline incision up
to the xiphisternum.
MCBURNEY GRID IRON
Made at the junction of the middle third and outer thirds of a line running
from the umbilicus to the anterior superior iliac spine. (The McBurney
Point)
RUTHERFORD-MORRISON INCISION
This is extension of the McBurney incision by division of the oblique fossa
PFANNESTIEL INCISION
Used frequently by gynecologists and urologists for access to the pelvis
organs, bladder, prostate and for caesarean section.
Usually 12 cm long and made in a skin fold approximately 5 cm above
symphysis pubis.
skin
fascia
anterior rectus sheath
rectus muscle
transversalis
fascia
extraperitoneal fat
perineum.
A convex incision which minimizing muscle parasthesia and paralysis post-
operatively. It also follows the cleavage lines in the skin resulting in less
scarring
The incision offers Excellent cosmetic results because the scar is almost
always hidden by the pubic hair
Limited exposure of the abdominal organs. Use of incision is therefore
restricted to the pelvic organs
High risk of injury to the bladder
Extension of the incision is difficult laterally
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
6
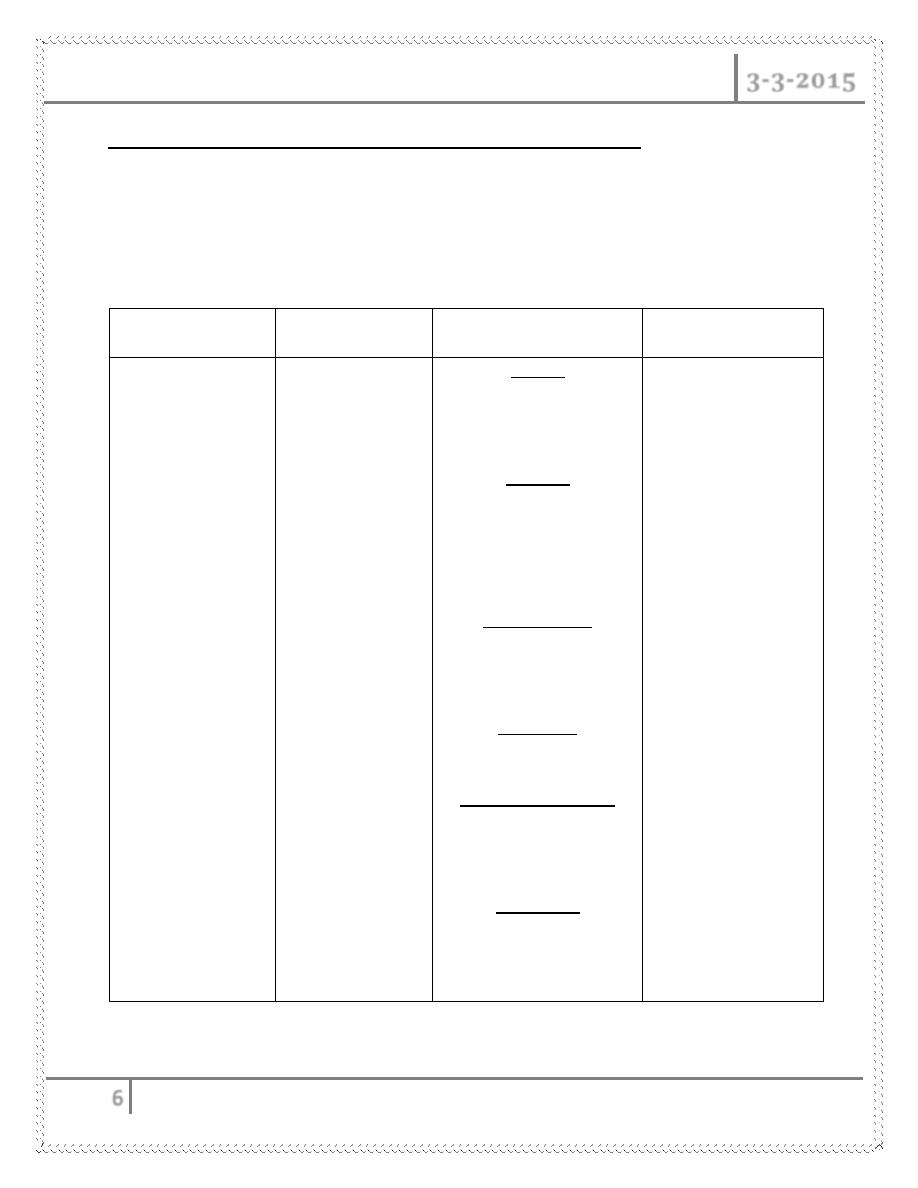
MAYLARD TRANSVERSE MUSCLE CUTTING INCISION
It is placed above but parallel to the traditional placement of Pfannenstiel
incision.
Gives excellent exposure of the pelvic organs.
SURGICAL PROCEDURES
Midline
Para media
Transverse & oblique
Thoracoabdominal
Vagotomy
Jejunostomy
Gastrectomy
Pancreatomy
Hysterectomy
LSCS
Cystotomy
Cystectomy
Salphingo
oopherectomy
Right
Cholecystectomy
Pyroplasty
Left
Splenectomy
pancreadectomy
Kocher
Cholecystostomy
Heptectomy
Chevron
Gastrectomy
Esophagectomy
Adrenalectomy
Mercedez benz
Liver transplant
Pancreatic transplant
McBurney
Appendectomy
Rutherford-morison
caecostomy or
sigmoid colostomy
Pfannestiel
Caesarean section
Hysterectomy
Hepatic resections
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
7
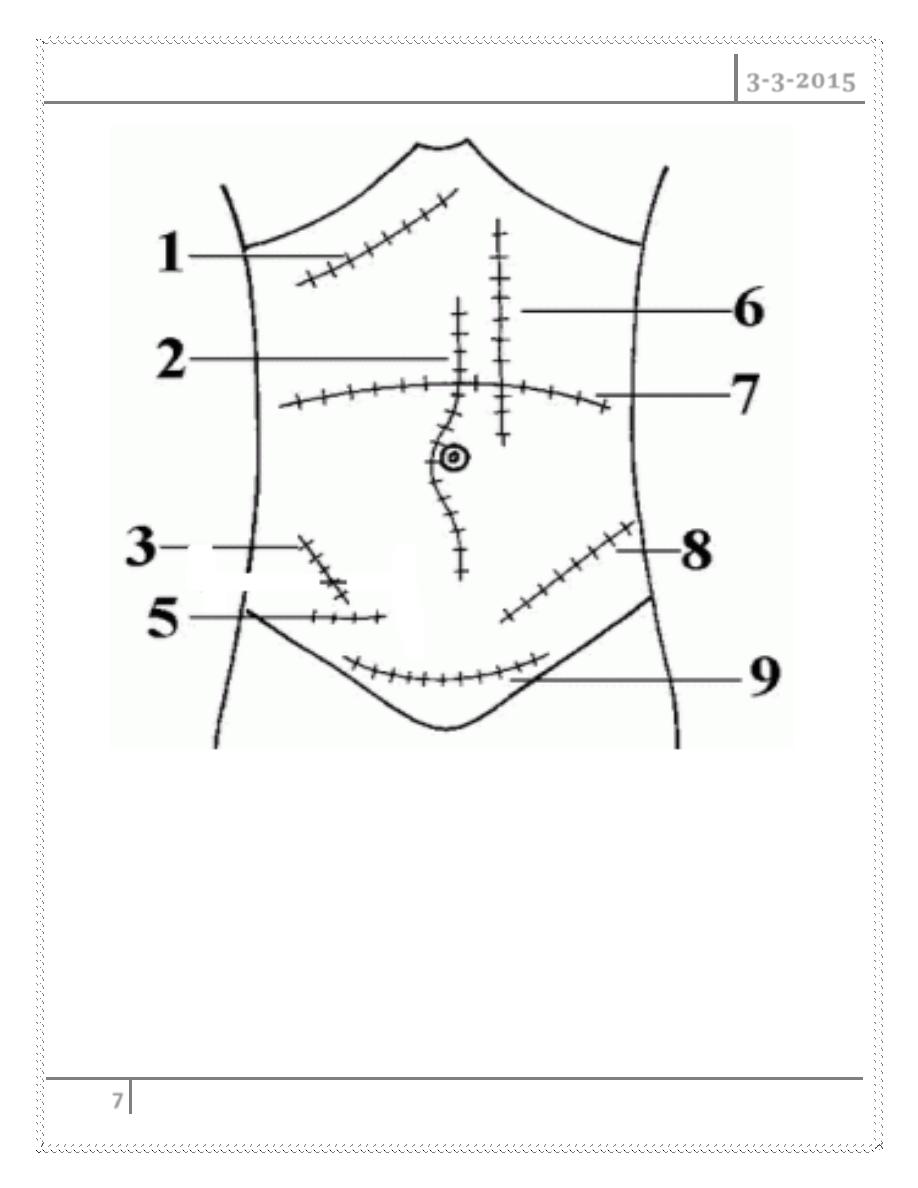
Kocher Incision: 1 Paramedian: 6
Midline: 2 Transverse: MUSCLE DIVIDING 7
McBurney: 3 Rutherford Morison: 8
Lanz: 5 Pfannenstiel 9
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
8
Wound healing
Phases of wound healing :
1. Inflammatory phase
2. Proliferative phase
3. Remodeling phase
Inflammatory phase
A. Immediate to 2-5 days
B. Hemostasis
1. Vasoconstriction – damaged blood vessels constrict
2. Platelet aggregation – primary hemostasis
3. Coagulation – fibrin – secondary hemostasis (clot – platelets + fibrin)
C. Inflammation
1. Vasodilation
2. Phagocytosis
Proliferative phase
A. 2 days to 3 weeks
B. Granulation
1. Fibroblasts lay a bed of collagen to fill the defect
C. Angiogenesis
D. Contraction
1. Wound edges pull together to reduce the defect
E. Epithelialization
1. Epithelial cells migrate across the new tissue to form a barrier between
the wound and the environment
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
9
Remodeling phase
A. 3 weeks to 2 years
B. New collagen forms which increases the tensile strength of the wound
C. Strength increases and becomes maximum but not as strong as original
tissue
D. Scar tissue is only 80% of the strength of the original tissue
Wound healing
Wound healing is accomplished in one of the following two ways :
1. Healing by first intention (primary union)
2. Healing by second intention (secondary union)
Healing of skin wounds is a classical example
Healing by first intention (primary union)
Occurs in clean, incised wounds with good apposition of the edges –
particularly planned surgical incisions
(clean wounds – no infections or foreign bodies)
The incision causes only focal disruption of epithelial basement membrane
continuity and death of a relatively few epithelial and connective tissue cells.
As a result, epithelial regeneration predominates over fibrosis
Sequence of events
Immediate
The narrow incisional space rapidly fills
with fibrin clotted blood
Dehydration at the surface produces a scab
to cover and protect the healing repair site

ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
10
Within 24 hrs
Movement and proliferation of epithelial cells
across the wound resulting in a thin, but
continuous epithelial layer
Early inflammation close to the edges (neutrophils)
2-3 days
Neutrophils replaced by macrophages
Macrophages remove the blood clot
Proliferation of epithelial cells
Fibroblastic activity
10-14 days
Scab loose (aka dry clot)
Epithelial covering complete
Fibrous union of edges
Wound still weak
vascularization
By the end of the first month
Scar comprises of a cellular connective tissue
devoid of inflammatory infiltrate, covered by
intact epidermis
Dermal appendages destroyed in the line of
incision are permanently lost
Tensile strength of the wound increases and
reaches maximum
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
11
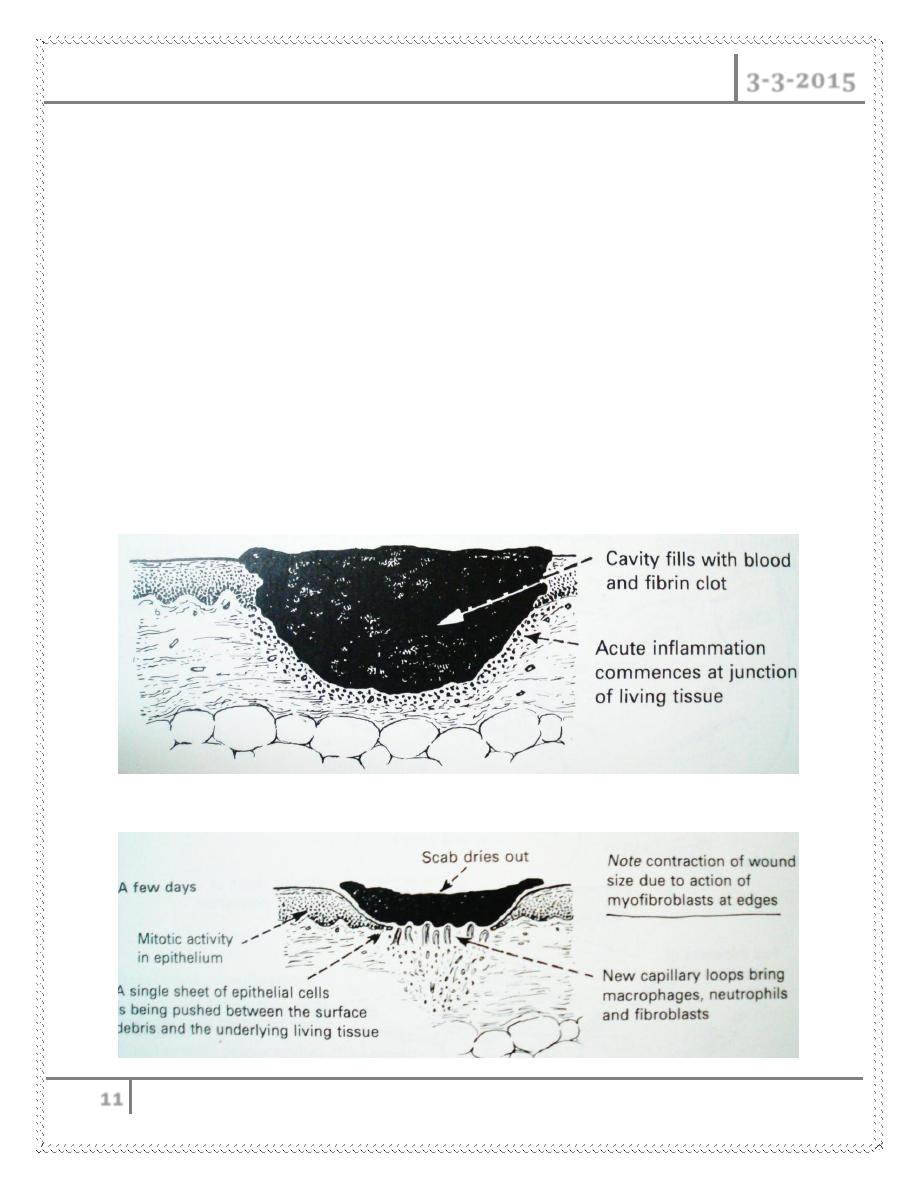
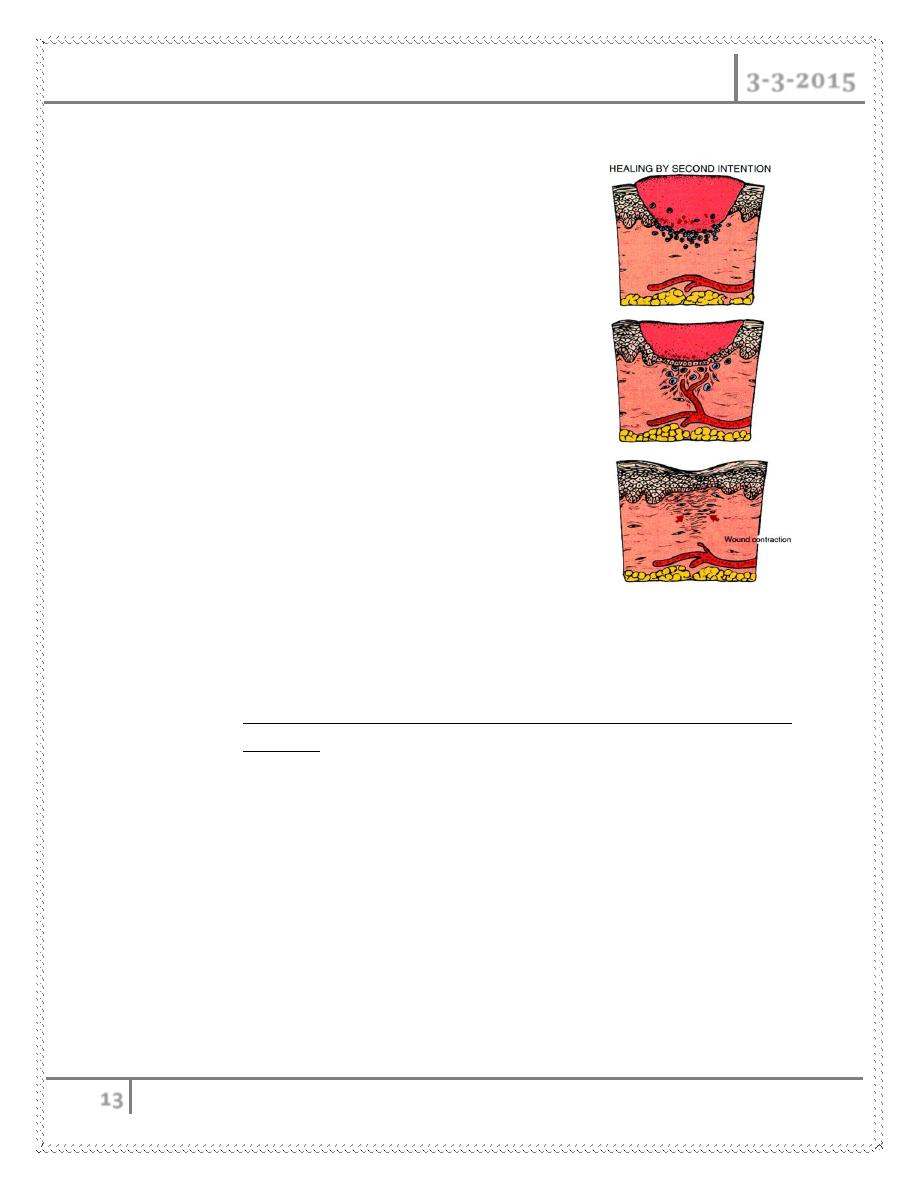
Healing by second intention (secondary union)
This occurs in open wounds, particularly when there has been significant
loss of tissue, necrosis or large wounds with irregular margins
Regeneration of parenchymal cells cannot completely reconstitute the
original architecture
Abundant granulation tissue grows in from the margin to complete the
repair
Granulation tissues consists of :
o ECM fibroblasts
o Macrophages, neutrophils
o New blood vessels
Sequence of events
Early
A few days
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
12
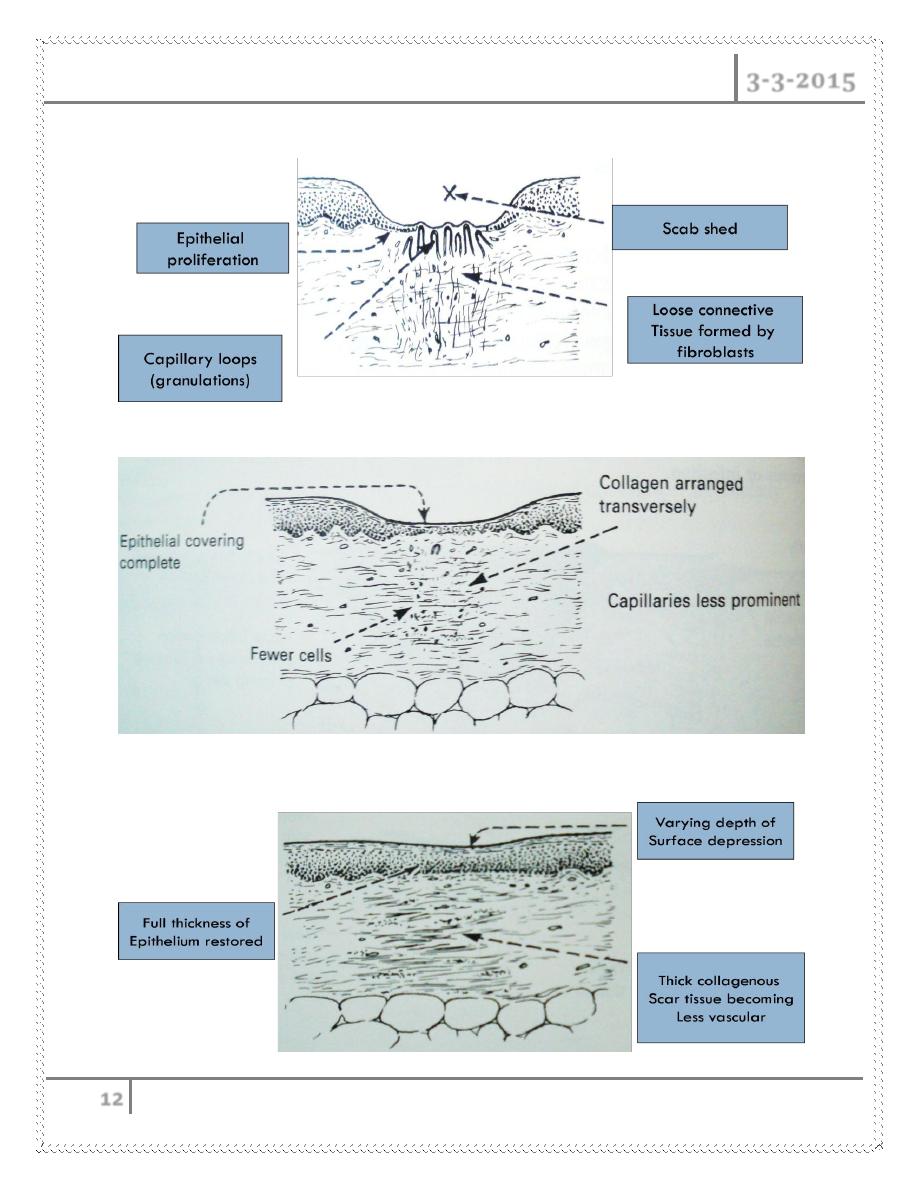
1 week
2 weeks onwards
Months
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
13
Secondary union differs from primary union in several respects
1. Inflammatory reaction is more intense
2. Larger amounts of granulation tissue
formation
3. Larger scar
4. ***ound contraction
- Myofibroblasts: modified fibroblasts with
feature of SMC
- defect significantly decreases in size as
wound heals.
Wound Strength
Skin wounds
- 1 week old; 10% of unwounded skin
o rapid increase in tensile strength as scar tissue accumulates over
2 months
- Completely healed; 70-80% of unwounded skin
- Scar tissue is never as strong as the original tissue !!
Factors that influence healing
Classified as :
A. Systemic
B. Local
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
14
Systemic Factors that Delay/Retard Wound Healing
Nutrition
Protein deficiency, Vitamin C deficiency
o Inhibit collagen synthesis
Zn deficiency (cofactor in type III collagenase)
Metabolic status
Diabetes mellitus :
o Susceptibility to infection caused by impaired circulation and
increased glucose.
Circulatory status
Inadequate blood supply
o atherosclerosis, vascular defects
Hormones
Glucocorticoids inhibit collagen synthesis, decrease inflammation
Local Factors that Delay/Retard Wound Healing
Infection
Most important cause of delayed wound healing
Persistent injury and inflammation
Mechanical factors
Motion early in healing
Foreign material - like suture material and foreign bodies
Size, location & type of wound
Wounds in ↑ vascularized areas (face) heal faster than in poorly vasc
areas (tendon, feet)
Small wounds heal faster than larger
Incisions faster than blunt trauma (contusions)
Complications of wound healing
1. Deficient scar formation ( most important)

ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
15
2. Excessive formation of repair components
3. Exaggerated contraction
Deficient scar formation
Can lead to two types of complications :
A. Wound Dehiscence (rupture of wound)
most common after abdominal surgery
o coughing, vomiting
B. Ulceration - defect in the continuity
Wound Dehiscence
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
16
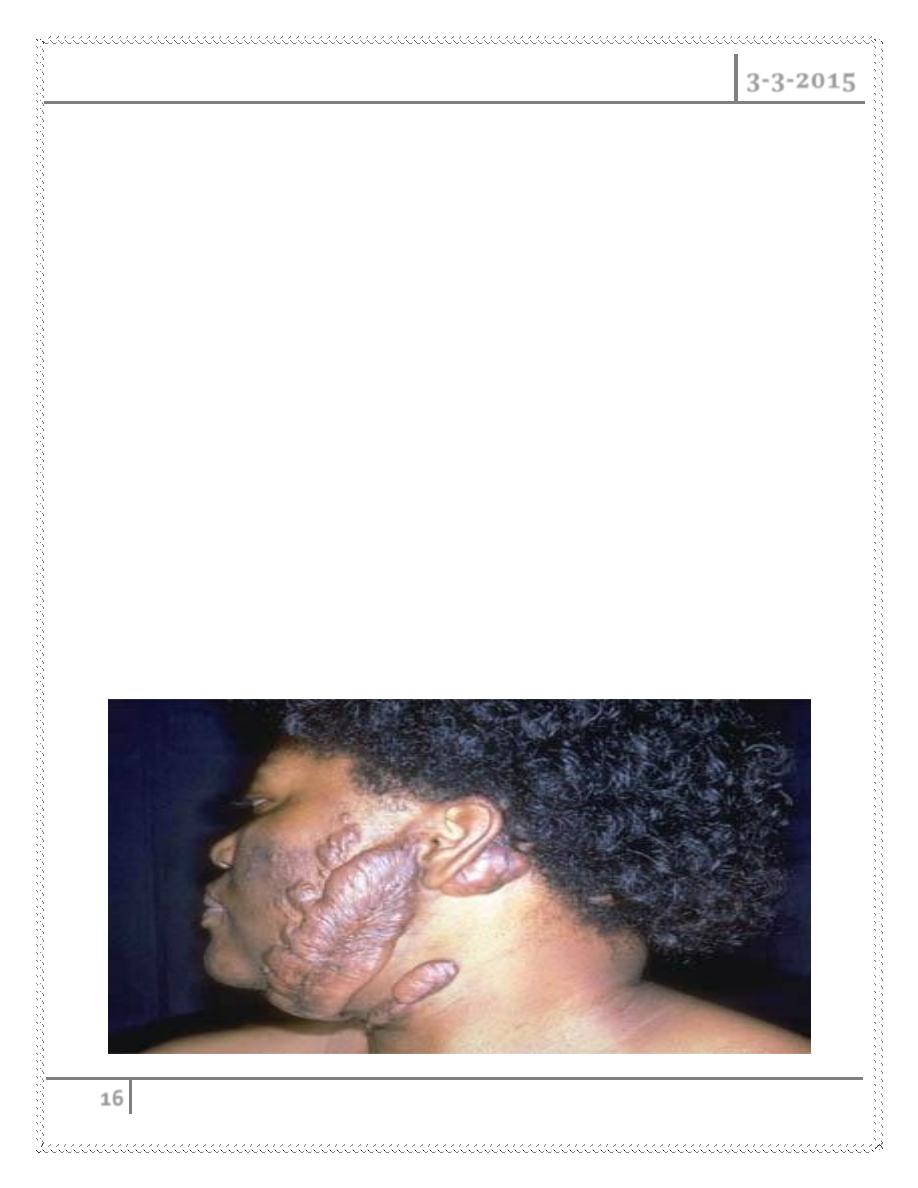
Excessive formation of repair components
1. Keloid / hypertrophic scar (excess collagen)
2. Exuberant granulation or proud flesh(excessive granulation tissue that
protrudes above the level of the surrounding skin and impairs the growth of
epithelium)
Keloid / hypertrophic scar
Raised scars due to accumulation of excess amounts of collagen ( type III
– type I)
Hypertrophic scars do not grow beyond the boundaries of the original
wound
Keloids grow beyond the boundaries of the original wound (more
serious)
o Can result from a surgery, an accident, body piercing or can be
spontaneous
o Genetic predisposition
o More common in African – Americans
o Commonly seen over face, shoulders and chest
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
17
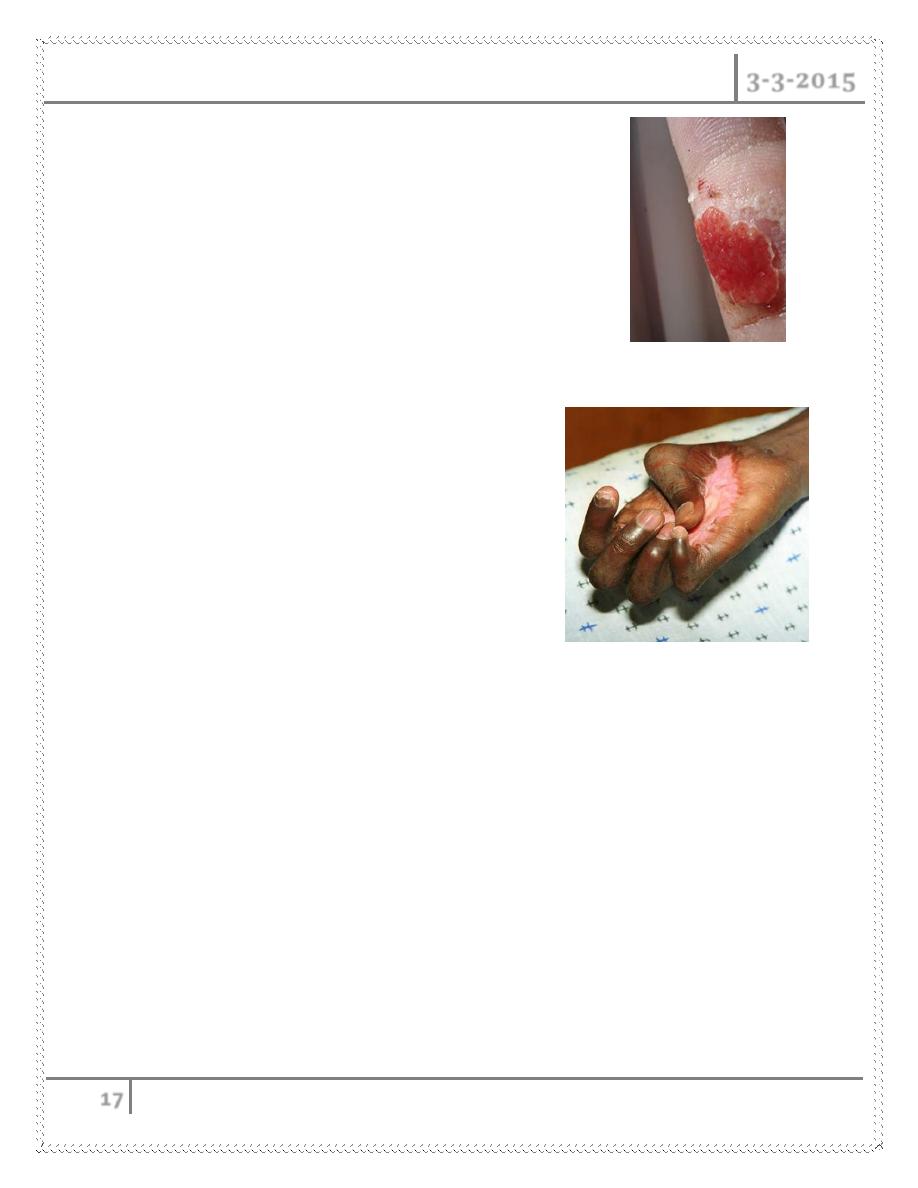
Exuberant granulation (proud flesh)
Excessive granulation tissue
Protrudes above surrounding skin
Prevents re -epithelialization
Exaggerated contraction
deformation of surrounding tissue or wound
Can compromise the movement of joints.
most common on
- palms, soles, anterior thorax following
severe burns
Important Growth factors responsible for wound healing
Platelet derived growth factor:
o Promotes migration and proliferation of fibroblasts
o Is chemotactic for monocytes
Epidermal growth factor
o Promotes growth of endothelial, epithelial cells and fibroblasts
Growth factors in wound healing
Fibroblast growth factor:
o Promotes synthesis of ECM proteins including fibronectin.
ABDOMINAL INCISIONS Dr. Ramez
3-3-2015
18
o Chemotactic for fibroblasts and endothelial cells
o Promotes angiogenesis
Vascular Endothelial Growth Factor (VEGF)
o Angiogenesis
Macrophage derived growth factors
o IL-1 and TNF
Promote proliferation of fibroblasts and endothelial cells.
#END
Done by
Ali Kareem
