1
/Immunology
_____________________________________________________
Lec. 3
د. عائدة الدرزي
Immunologic mechanisms of tissue damage
(hypersensitivity reactions)
Although the immune system generally is protective, the same
immunologic mechanisms that defend the host may at times result in
severe damage to tissues & occasionally may cause death. This
inappropriate immune response is termed hypersensitivity or allergy.
Gell & Coombs (1963) have classified hypersensitivity reactions into four
major types:
- Type I : Anaphylaxis Hypersensitivity (H.S.)
- Type II : Antibody-dependent cytotoxic H.S.
- Type III : Immune-complex mediated H.S.
- Type IV : Cell-mediated (delayed) H.S.
Type I hypersensitivity: Which is also referred to as:
- Anaphylaxis H.S. -- (A Latin- word opposite to prophylaxis).
- Immediate H.S. --( The reaction occurs within minutes after
exposure to Ag).
- Atopy -- (A hereditary predisposition to the development of
immediate hypersensitivity reaction against common environmental
antigens).
This reaction results from the release of pharmacologically active
substances from mast cells & basophils following interaction between Ag
& Ab which present on surface of these cells. The reaction may be mild
& localized one, e.g. allergic conjunctivitis, or it may be severe
generalized reaction, e.g. anaphylactic shock.
2
Requirements of anaphylaxis:
1- IgE: It is referred to as:
Reagenic Ab, Homocytotropic Ab
IgE is named so because it possesses specific receptors on
cell membrane of mast cell & basophiles.
IgE receptors:
-
Fc epsilon receptor I (FcεRI)
These are high affinity IgE receptors expressed on cell
Membrane of Basophils & mast cells (Langerhans cells).
-
Fc epsilon receptor II (FcεRII) CD23
These are low affinity IgE receptors
Expressed on: T & B lymphocytes, monocytes, eosinophil, & platelets.
2- Allergenes: These are antigens capable of stimulating type I H.S.
responses in allergic individuals, & they include:
a- Inhalants
animal danders, plant pollens, fungal spores,
houst dust, houst dust mites.
b- Ingestants
(foods, drugs ... etc.) egg albumin, fish, cheese,
Nuts, milk, food additive, penicillin, aspirin.
c- Contactants
pollen, food, drugs ... ect
3- Mast cells & Basophils
They represent a major source of potent chemical mediator
implicated in a wide spectrum of inflammatory & immunological
processes.
In addition, they express membrane receptors (FcεRI) that
specifically bind the Fc portion of IgE (binding site) Ab.
Immediate H.S. reactions are mediated or initiated when allergen

3
molecule crosslink the Fab components of adjacent IgE molecule on the
surface of mast cells & basophils
degranulation of the cells & release
vasoactive amines.
Complements are not involved in this type of reaction.
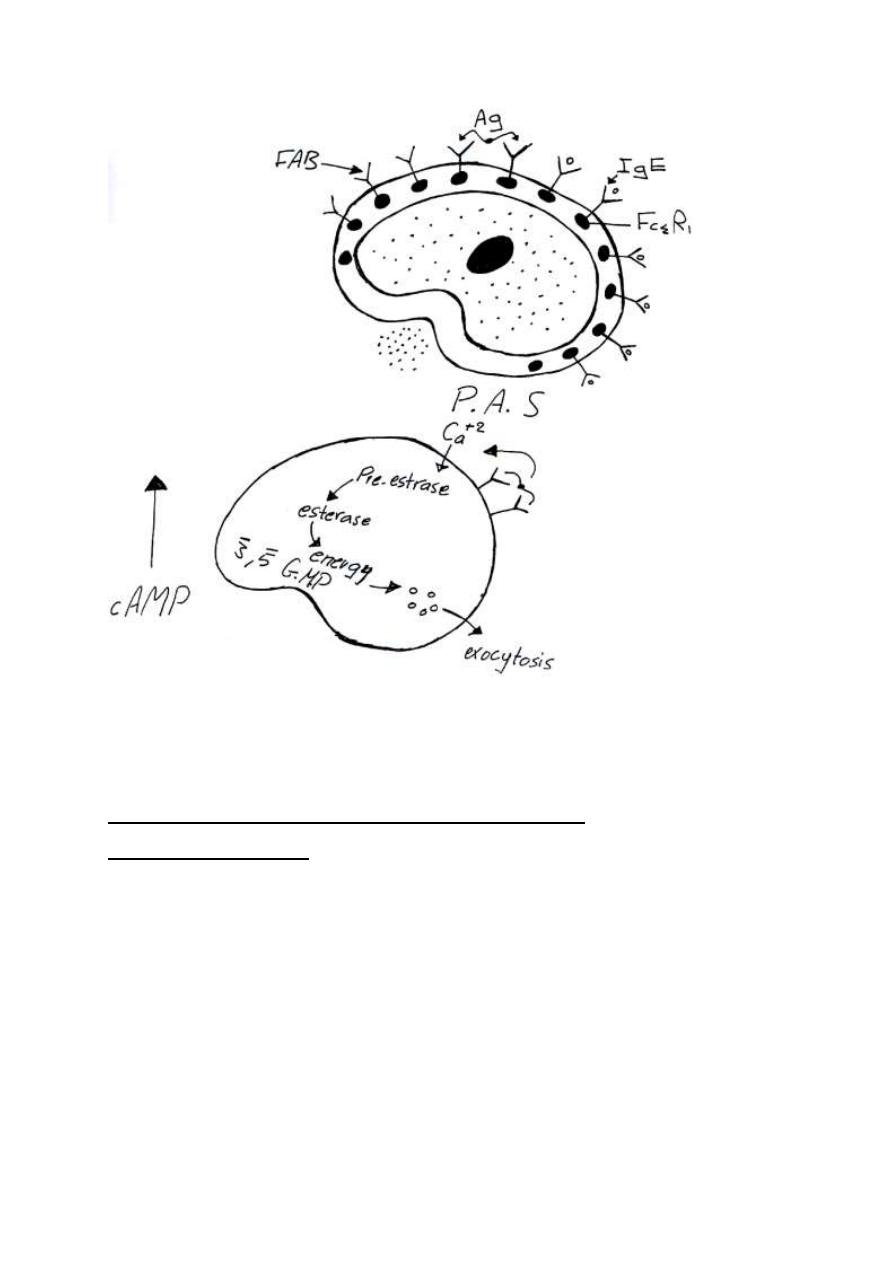
4- Intra-cellular biochemical events (mast cell degranulation):
The initial exposure to an allergen results in production of specific IgE &
its ultimate fixation to mast cells & basophils; subsequent exposure to
the allergen will trigger an Ag-Ab reaction on the cell membrane. A
critical step is the bridging of adjacent membrane-bound IgE molecules
by the allergen (one allergen molecule crosslink two adjacent FAB
components of IgE on mast cells). This is followed by:
a- Influx of calcium ions into the mast cells.
b- Cytoplasmic phosphodiesterase is activated,
c- Increase level of 3,5 GMP & decreased level of cAMP.
d- Solublization & release of mediators stored in mast cells & basophils.
4
Mast cell & basophil mediators of atopic disease
(vasoactiveamines):
1- Preformed (stored) mediators:
-Histamine
-ECF-A
Eosinophil chemotactic factor of anaphylaxis
2- Synthesized mediators
-PAF
-SRS-A
-Bradykinin

5
5- Vasoactive amines:
a- Histamine:
- It causes smooth muscle contraction of human bronchioles.
- It increases permeability of capillaries (vasodilatation).
- It increase secretions by nasal & bronchial mucous glands.
- max. Reaction 1-2 min
Duration 10 min.
- Responsible for symptoms of hay fever, angio-oedema, bronchospasm
of acute anaphylaxis.
b- ECA-A (Eosinophil Chemotactic Factor of Anaphylaxis)
- preformed in basophils & mast cells.
- causes influx of eos. to area of allergic inflammation. (eosin Phil
chemotaxis)
* role of eosinophils in allergy: They control allergic reactions by
releasing histaminase and arylsulfatase , which degrade two important
mediators, histamine and SRS-A, respectively. Eeosinophils may
therefore reduce the severity of type I response.
c- HMW-NCF (High Molecular Wt. Neutrophil Chemotactic Factor)
6
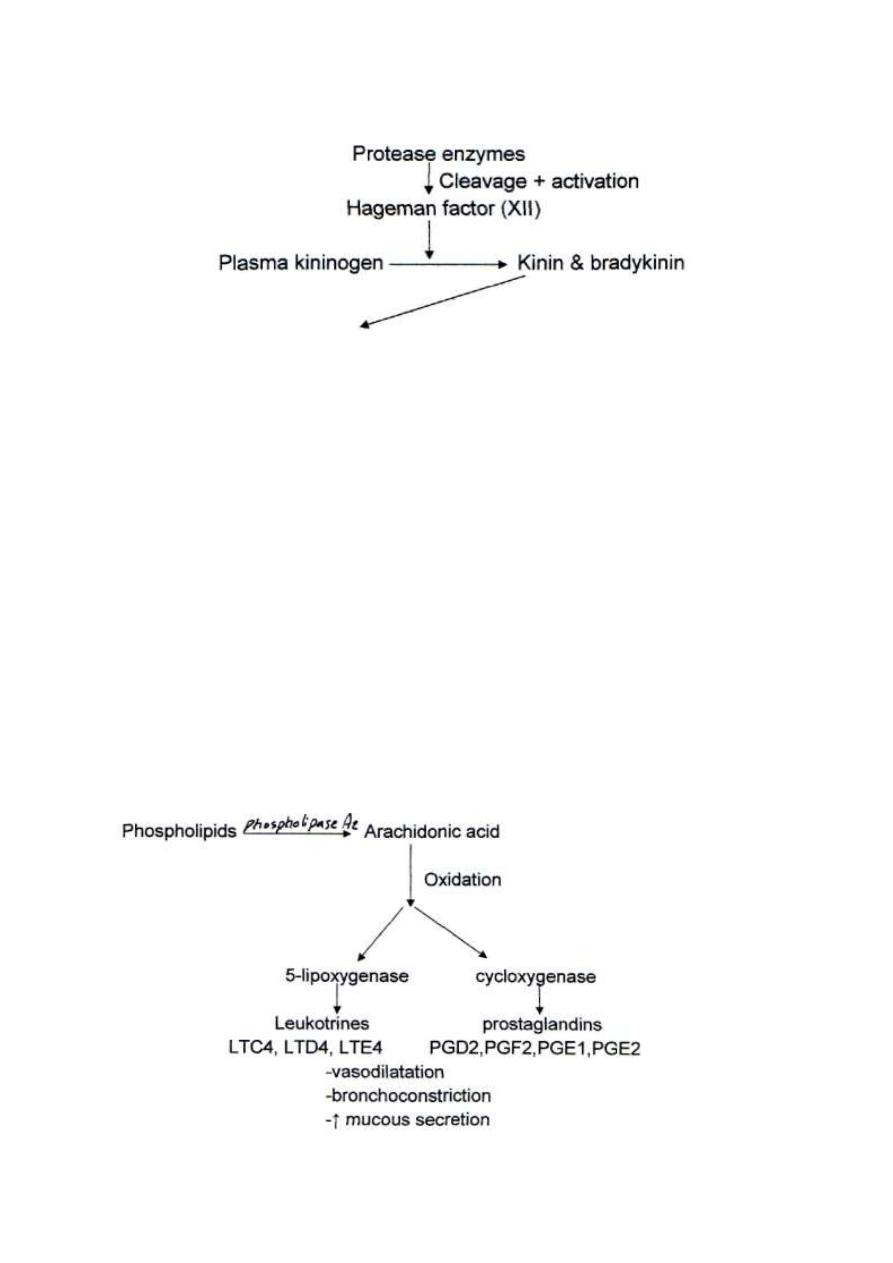
d- Kinin-Generating proteases:
- Smooth muscles contraction of bronchioles.
-
↑ vascular permeability
-
↑ secretion of mucous glands
- Stimulate pain fibers
-
e- PAF (Platelet Activating Factor) - This factor enhances platelet
aggregation & release vasoactive amines----increase vascular
permeability
---- contraction of smooth muscles
---- bronchoconstriction
f- Arachidonic acid metabolites (slow reacting substances of
anaphylaxis SRS-A)
7
Clinical manifestations:
Clinical manifestations of immediate H.S. reaction begin very shortly (10-
20 minutes) after allergen exposure, & vary greatly in severity &
depending on the target organ or tissue:
- Skin
urticaria , angioneurotic oedema , atopic dermatitis
- Respiratory system
Hay fever, asthma , allergic conjunctivitis
- Gastro-intestinal tract
Vomiting , abdominal pain , diarrhoea
- Urinary tract
Frequency , dysuria , hematuria
- Vascular involvement
CNS
headache , personality disorder
Factors predisposing to type I H.S.:
- Genetic factors (atopic allergies -hay fever, asthma, food allergy)
Atopic individuals have IL4-gene coding for high level for IL4
a- IL4 gene ---- IL4
↑ no. Th2
↑isotype switching
↑IgE level
b- HLA allele at (maternal & paternal) DR loci
e.g. allergy to grass pollen
HLA-DR3
allergy to rag pollen
HLA-DR2 , HLA-DR5
8
- Environmental Factors
Air pollutants (S02, car exhaust, fumes, passive cigarette smoking)
increase permeability of epithelial cells of respiratory tract for allergens.
Diagnosis:
- In Vitro
PRIST (Paper Radio Immunosorbent Test)
RAST (Radio Allergosorbent Test)
These are radioimmunoassay tests to measure total IgE in serum &
specific serum IgE respectively
- In vivo (skin test)
A series of potential allergens are administered via a scratch test or
intradermal, & the injection sites are examined within 15-20 min. for the
appearance of wheal (edema) & flare (erythema) reaction.
Treatment & Prevention:
1-
Avoidance of responsible allergens.
This
can
be
accomplished easily with food allergies, however it may be difficult with
inhalant allergens.
2- Immunotherapy
a- Desensitization , Hyposensitization (IgG-blocking Abs)
This involves injecting the patient, over time, with gradually increasing
doses of responsible allergens. This stimulates Th1 subsets rather than
Th2, cytokines secreted by Thl including y-INF causing class switch in B
-cell to produce allergen specific IgG-blocking Abs, these Abs diffuse in
9
tissues, bind to allergen molecules & the IgG-allergen complex is
removed by opsonisation , & no further allergen molecules bind IgE on
mast cells.
b- Immunotolerance
By injecting the patient with synthetic peptides which bind T cell receptors
directly & causing T cell anergy (T cell unresponsiveness). So T cell
cannot produce help to B cells for further activation.
3
- Drugs
a- Anti-histamins
Tavist-D (clemastin fumerate)
b- Mast cell & basophil stabilizing drugs:
1- Adrenaline
increase intracellular level of cAMP
2- Theophylline
inhibits brake down of cAMP by phosphodiesterase
3-Sodium chromoglycate
inhibits calcium influx
c- General anti-inflammatory agents
corticosteroids
Anaphylactoid reactions:
The clinical manifestations of anaphylaxis can occur in the absence
of any evidence for an allergen-lgE antibody event.
These reactions are believed to arise through the non-immunologic
release of vasoactive & inflammatory mediators from mast cells and
basophils in certain susceptible individuals. The inciting agents are:
- I.V. radiographic contrast media
- Aspirin
- Venom
- Exercise induce anaphylaxis
- Other causes
idiopathic
B
rought
t
o
y
ou
b
y :
A
li
K
areem
