1
Immunology
______________________________________
Lec. 6
د. عائدة الدرزي
CANCER IMMUNOLOGY
Oncogenesis (passes through two stages):
1- Reversible change
Normal
transformed cells
2- Irreversible change
Transformed
oncogenic cells
Factors causing oncogenesis:
1 - Hereditary predisposition
2- Environmental factors: They cause mutations & have been shown to
induce transformation, they include:
a- Physical agents:
Ultraviolet light, ionizing radiation ...etc
b- Chemical agents:
Aromatic amines, Afla toxins, alcohol …..etc.
c- Viral factors:
A number of DNA & RNA have been shown to induce malignant
transformation.
e.g. herpes virus II
ca. Cervix
Cytomegalo virus (CMV)
nasopharyngeal ca.
2
3- Involvement of normal regulatory genes (cancer associated genes):
Cancer associated genes can be divided into 3 categories that reflect
their different activities:
a- The growth promoting / proto-oncogenes :
These genes encode proteins that induce cellular proliferation. Some of
these proteins function as growth factors, growth factor receptors, signal
transducers, & transcription factors. Over activities of these genes
(due to mutation, genetic rearrangement, chromosomal translocations)
results in up regulated proliferations.
b- The growth inhibiting / cancer suppressor genes :
These genes encode proteins that inhibit excessive cell proliferations.
Inactivation of these genes results in un- regulated proliferations.
Ex. P
53
: > 50% of breast & ovarian cancers have been shown to be
associated with mutation in P53.
c- Genes that regulate apoptosis : They encode proteins that block or
induce apoptosis.
Ex. bcl
2
(anti-apoptosis gene)
3
Theory of oncogenesis by oncogenes:
Oncogenes were shown to cause neoplastic transformation of cell in
vitro, & were therefore regarded as the gene that causes cancer. They
occur in all eukaryotic cells including man.
More than 30 oncogens have been identified & around 28 have been
mapped. The protein of oncogen have been found to be similar to known
substances that are known to be involved in the control of the cell
division; growth factor; plasma membrane receptors; modulation of
transduction of oncogenes signals through plasma membrane. These
new discoveries changed the new concept of oncogen, i.e. they are
considered to play a vital role in the normal control of mitosis, so they
are regarded as mitogenes rather than oncogenes.
Most prominent changes associated with transformed cells:
1- Altered morphology
2- Altered pattern of growth (physiological changes)
3- Biochemical changes include:
-
↑ metabolic rate
- Changes in the composition
- Changes in the proteins of cell membrane, these changes include:
a. Loss of normal cell surface Ag
b. Gain of neoantigens & other membrane changes
Tumor immunology involves:
1- Study of antigens on tumor cells
2- Immune response to these antigens
4
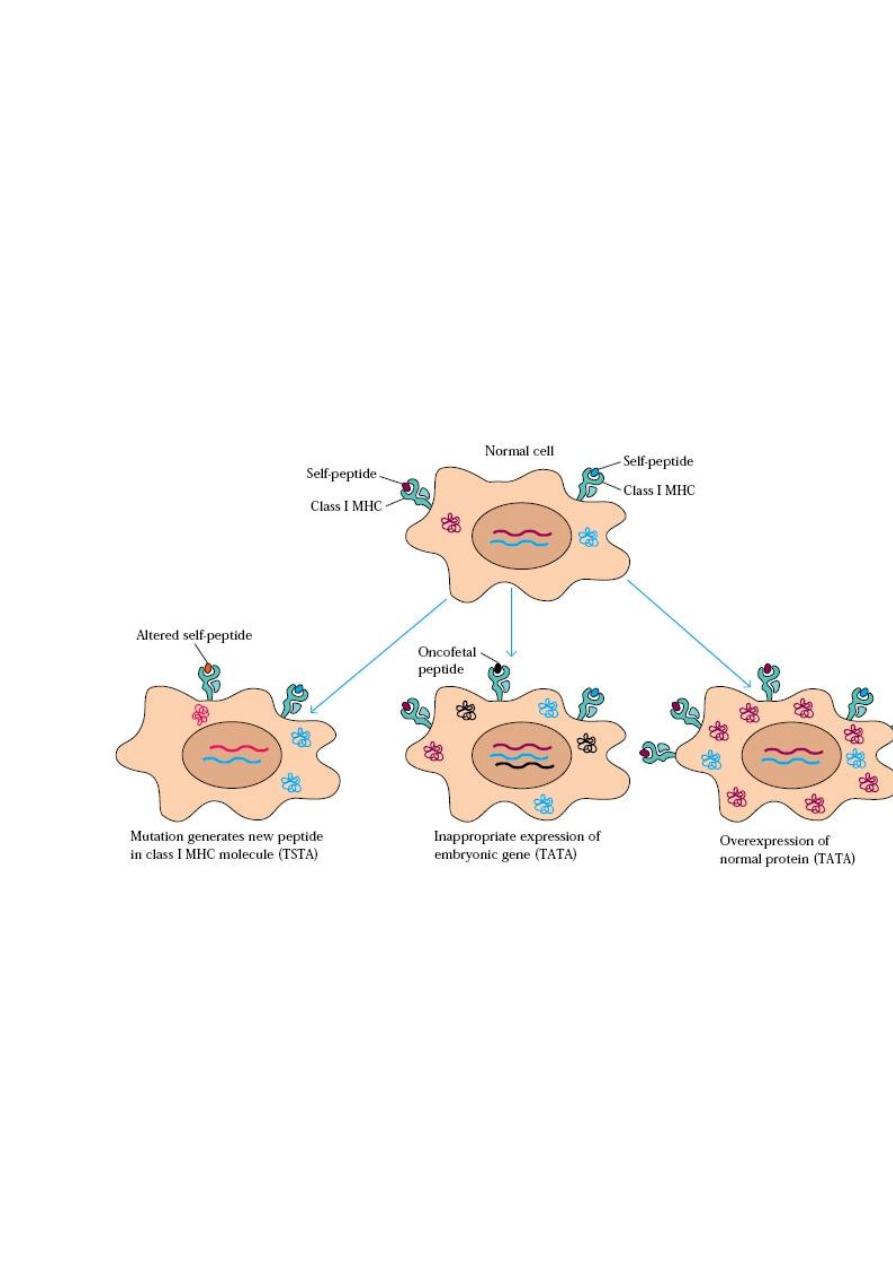
Tumor Antigens:
1- Tumor specific transplantation Ag (TSTA)
2- Oncofetal tumor antigens (Embryonic Ag)
3- Tumor associated transplantation Ag (TATA)
4- Tumor associated viral Ag

5
Tumor Antigens:
1- TSTA , these are:
- Specific Ags
- Unique to tumor cells, & do not occur on normal cells
- result from mutation ,& tumor cells generate altered cellular peptides
e.g. PSA (prostate specific antigen)
2- Oncofetal tumor antigens:
a- Alpha fetoprotein (AFP) - These are associated with:
- Primary liver cancer
- Testicular & ovarian cancer
- Gastric & pancreatic cancer
- Liver cirrhosis & hepatitis
b- Carcinoembryonic Ag (CEA)- These are associated with:
- Colorectal cancer
- Pancreatic cancer
- Liver cirrhosis, chronic lung disease
3- TATAs
e.g. myeloma pr. , CALLA
4- Tumor associated viral Ags
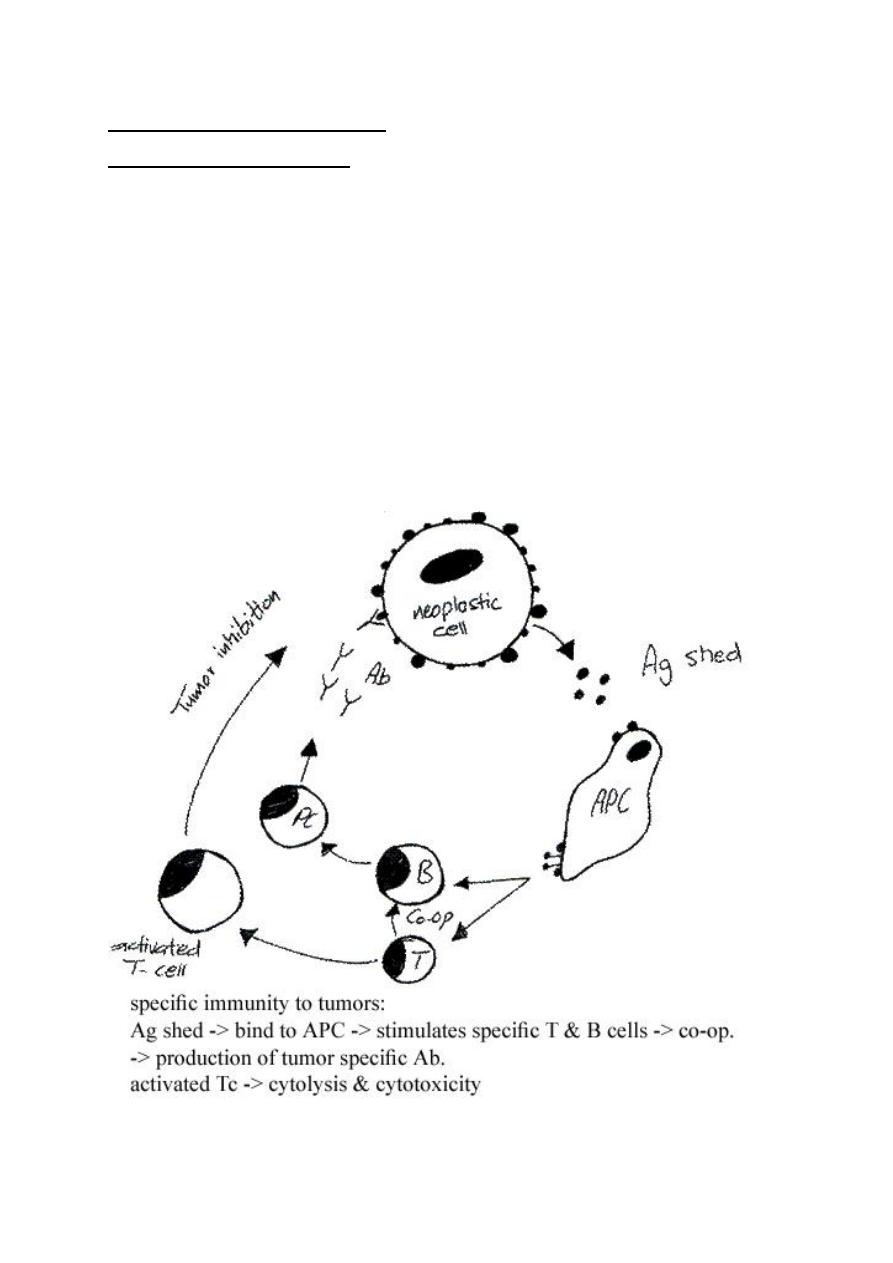
Immune response to tumor:
I- Non-specific immunity:
a- Macrophages: not MHC restricted, so it kills tumor cells in-
specifically
- Activated macrophages express Fc-receptors that bind Ab on tumor
cells
kill the target cells by ADCC
- Anti-tumor activity of macrophages is mediated by:
Hydrolytic enzymes, cytokines, INF-
ү, TNF-α, oxidative products (H
2
O
2
),
nitric oxide
directly kill tumor cells
6
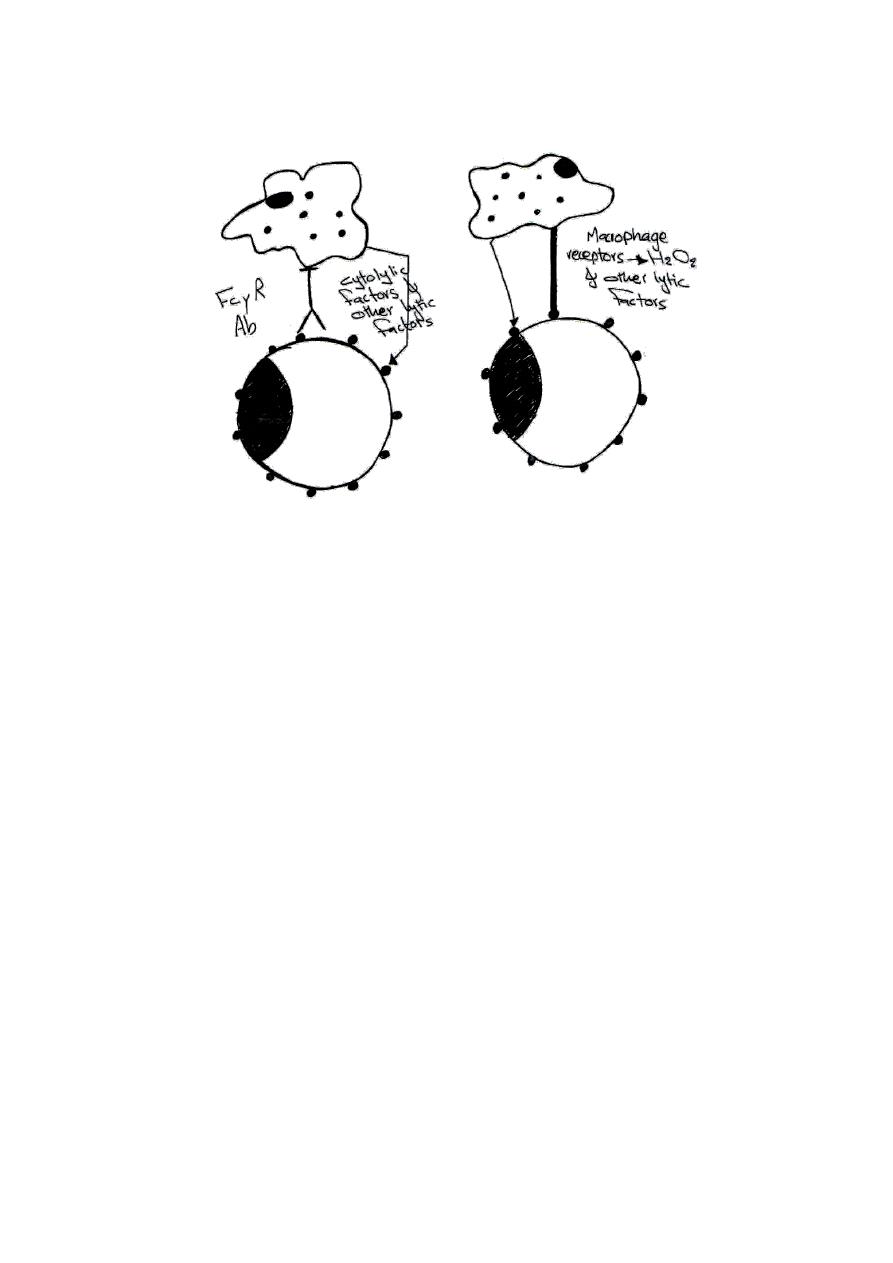
Macrophage act against tumor in two ways:
1- Antibody binds to tumor cell Ag & FcyR on macrophage
2- Direct contact of new surface determinants on tumor cell &
macrophage receptors
b- Natural killer cells: not MHC restricted
- NK cells express Fc-receptors that bind Ab on tumor cells
kill the
target cell by ADCC through releasing of Perforine, granzymes, &
proteases
-Direct contact
• INF-
Ү
- Activates non active NK
- Hyper activates the already active NK
- Makes NK resistant to PGE
2
7
Immune response to tumor:
II- Specific immunity by:
a- Cell mediated immunity:
- CD8
+
cell (Tc)
direct hit & run phenomenon
perforine & granzymes
granules
- CD4
+
cell (T
DTH
)
indirectly by cytokines (MIF, MAF, MCF , IL
2
, TNF-
β)
b- Humoral immune response
- Complement fixation
- Opsonization
- ADCC
8
Modes of escape from host defence mechanisms:
1- Tumor is non-immunogenic
2- Tumor modulates it's surface Ag
avoid immune destruction
3- Loss of class I MHC molecules
Tu. cannot be destroyed by MHC-
restricted cytotoxic T-cell
4- Immune enhancement (blocking factors): Tumor-growth-enhancing
Abs protect tumor cells & prevent their interaction with protective
immune factors
5- Ag shedding: continuous shedding of Ag
local & systemic
tolerance
6- Lack of co-stimulatory signal (B
7
)
no immune response
7- Tumor secrets immune-suppressive molecules (immune-kinetics) e.g.
PGE
2
immune response is down regulated
8- Ag masking: tumor products mask the antigenic determinant area
hidden
9
Cancer immunotherapy:
a- Immunotoxines:
Tumor specific monoclonal Abs conjugated to tumoricidal substances.
e.g. cytotoxic drugs, diphtheria toxin... etc. (Magic bullet)
b- Macrophage activating compounds:
- Bacille Calmette-Guerin (BCG)
- Cytokine therapy:
1- INF-
ү.β.α- ↑ class I MHC on T-cell
2- INF-y
↑ class II MHC especially on macrophage
Inhibits cell division & proliferation
↑ Activity of NK, Tc
3- TNF-
α & β
direct anti-tumor activity
4- IL
2
T & NK activation
c- Cytokine genes (genetic engineering)
1- GM-CSF gene
2- IL
12
gene
