
Immunological Tolerance
and
Autoimmune Diseases
Immunological Tolerance
a state of specific immunological
unresponsiveness to a particular
antigen in a fully immunocompetent
person
- Immunogen
- Tolerogen
Immunological Tolerance
Types of tolerance:
– Naturally acquired
(Neonatal, self ,auto
tolerance)
Tolerance to self is initially induced
during embryonic life, and is maintained
by antigen , continues to occur at some
level throughout life (as new
lymphocytes are produced from bone
marrow stem cells)
– Specifically Induced
Induced Tolerance
–Therapeutic
Inducing tolerance may be exploited
to prevent graft rejection, treat autoimmune and
allergic diseases
-
T cells
becomes tolerance quicker & last longer
than B cells
-
The simpler the Ag
gets Better Tolerance
because has less epitopes
Can be achieved by
•Low Zone Tolerance
•High Zone Tolerance

Mechanisms of Immunological
Tolerance - Overview
• Central Tolerance
Through Clonal Deletion
–Clones of cells that have receptors for
self-antigens are deleted during
development (negative selection)
• Peripheral tolerance

Peripheral Tolerance
1-
Immunological ignorance
to some self
antigens (anatomical barrier)
2- T-cell anergy
a-
signal block: failure of APC to deliver a
second signal during antigen presentation
(example: B7-CD28 interaction)
b-
engagement of inhibitory receptors
(CTLA-4)

Peripheral Tolerance
3- Suppression of responses
by regulatory
T- cells (CD4+ CD25+) :
secretion of immunosuppressive cytokines
(IL-10 & TGF-B)
4- Deletion
(activation-induced cell death):
T- cell apoptosis by engagement of death
receptors (Fas-Fas L)
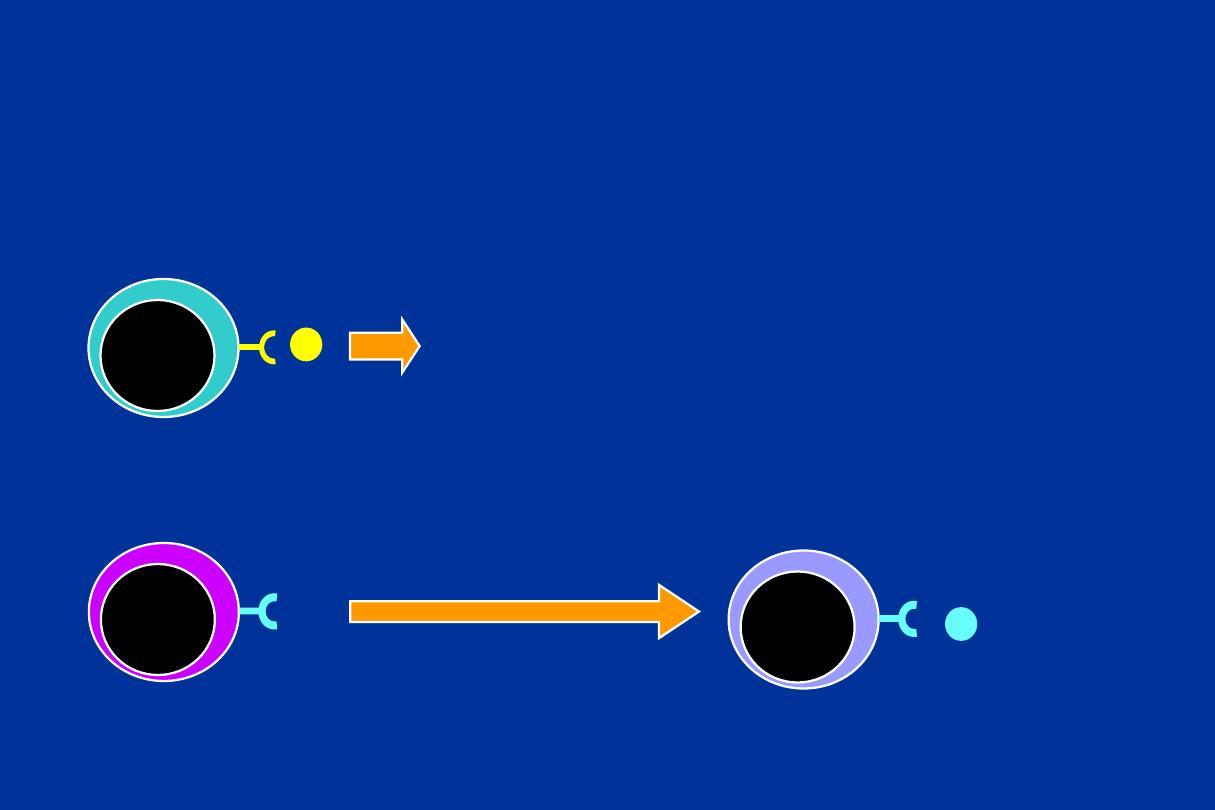
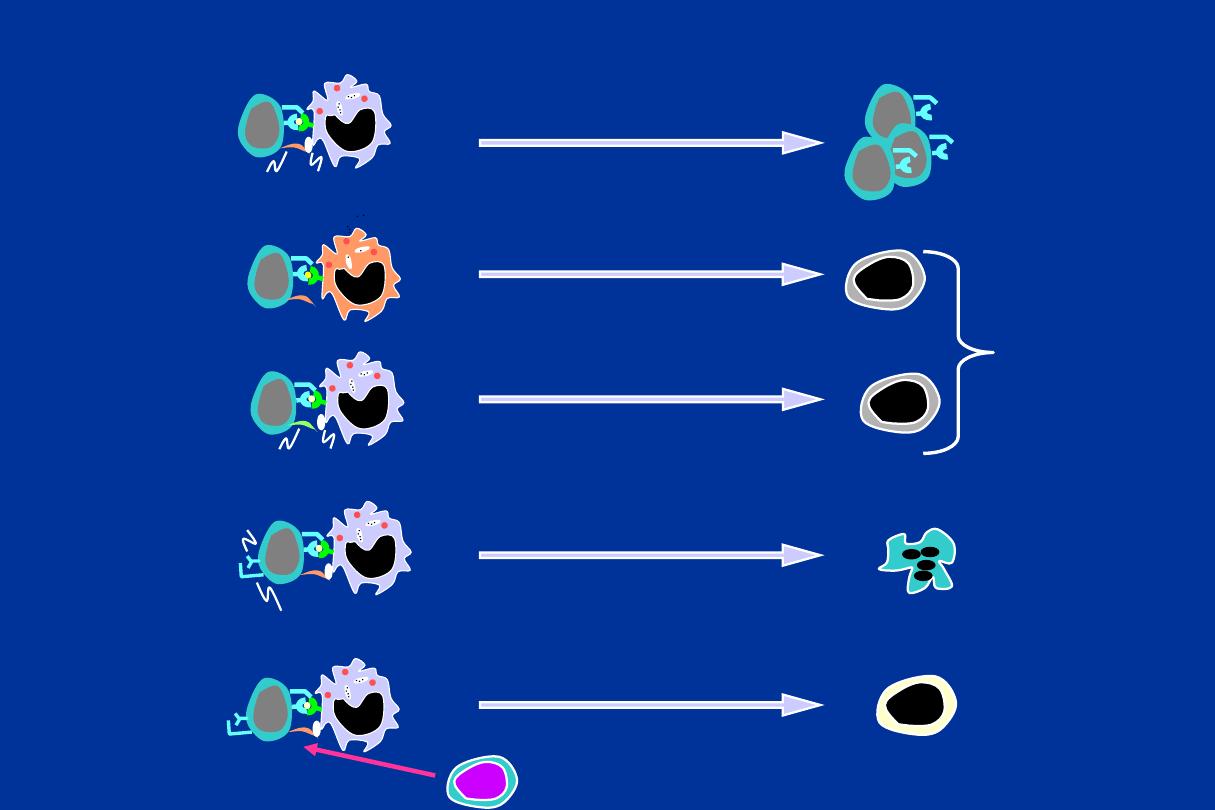
Central Tolerance
Anti-self
Lymphocyte
Self Ag
Clonal
Deletion
Anti-non-self
Lymphocyte
Activation
Foreign Ag + second signal
DEVELOPMENT MATURITY
Differentiation
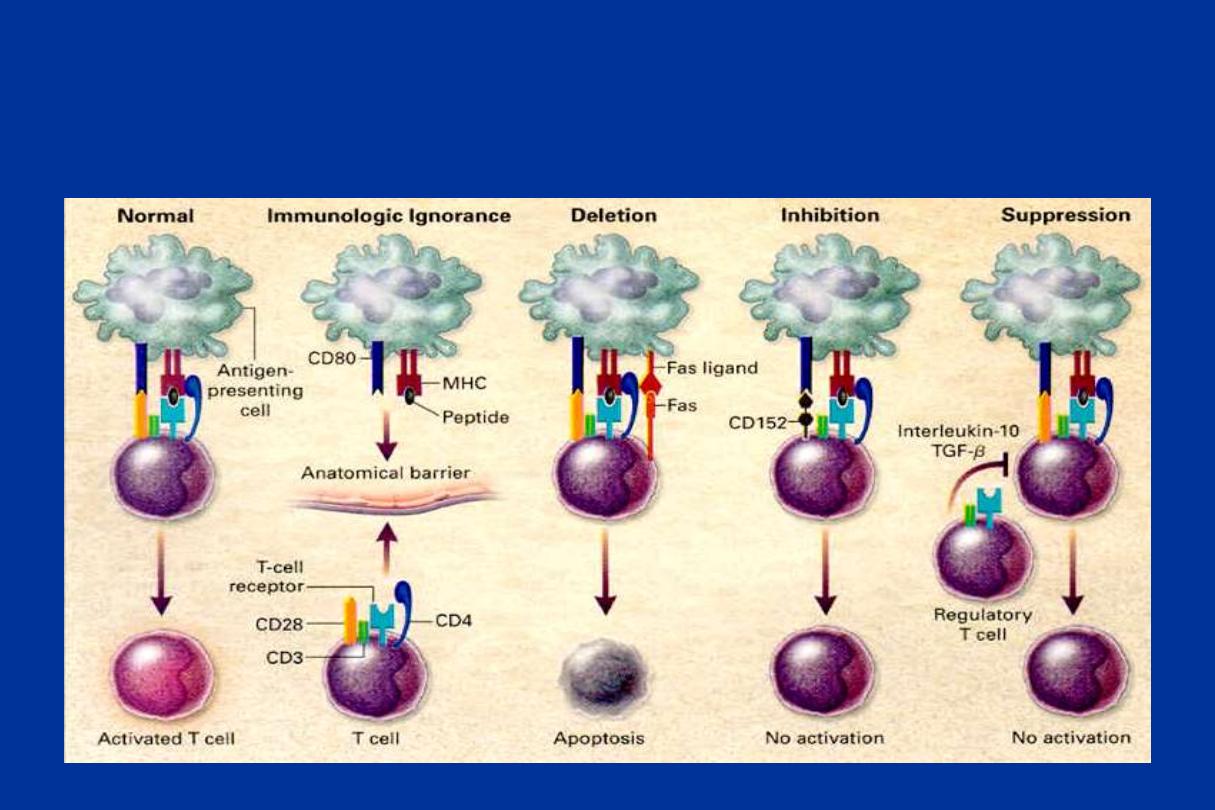
Pathways to Peripheral Tolerance
Fas
FasL
cytokines
Apoptosis
Inhibition of
proliferation &
effector action
Activated
T cells
Normal
Response
CD28 B7
Proliferation & differentiation
Antigen Recognition
without co-stimulation
Anergy
CTLA4
B7
Functionally
Unresponsive
CTL4-B7 interaction
Fas-FasL interaction
Cytokine-mediated suppression
Activation
induced cell
death
Cytokine
regulation
Pathways to Peripheral Tolerance

Properties of regulatory T cells Th 3 (T reg)
• Phenotype
: CD4, high IL-2 receptor
(CD25), low IL-7 receptor, other
markers
• Mechanisms of action
: multiple
– secretion of immune-suppressive cytokines
(TGF
, IL-10, ),
– inactivation of dendritic cells or responding
lymphocytes
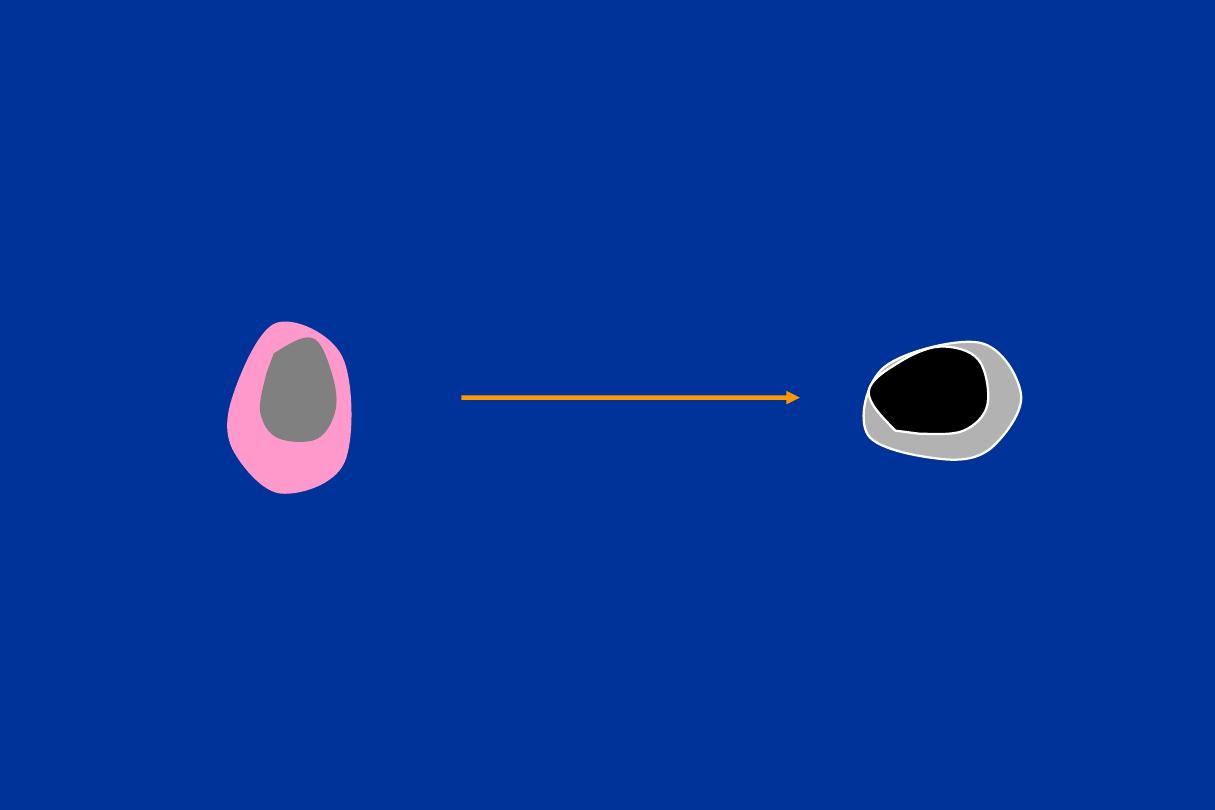
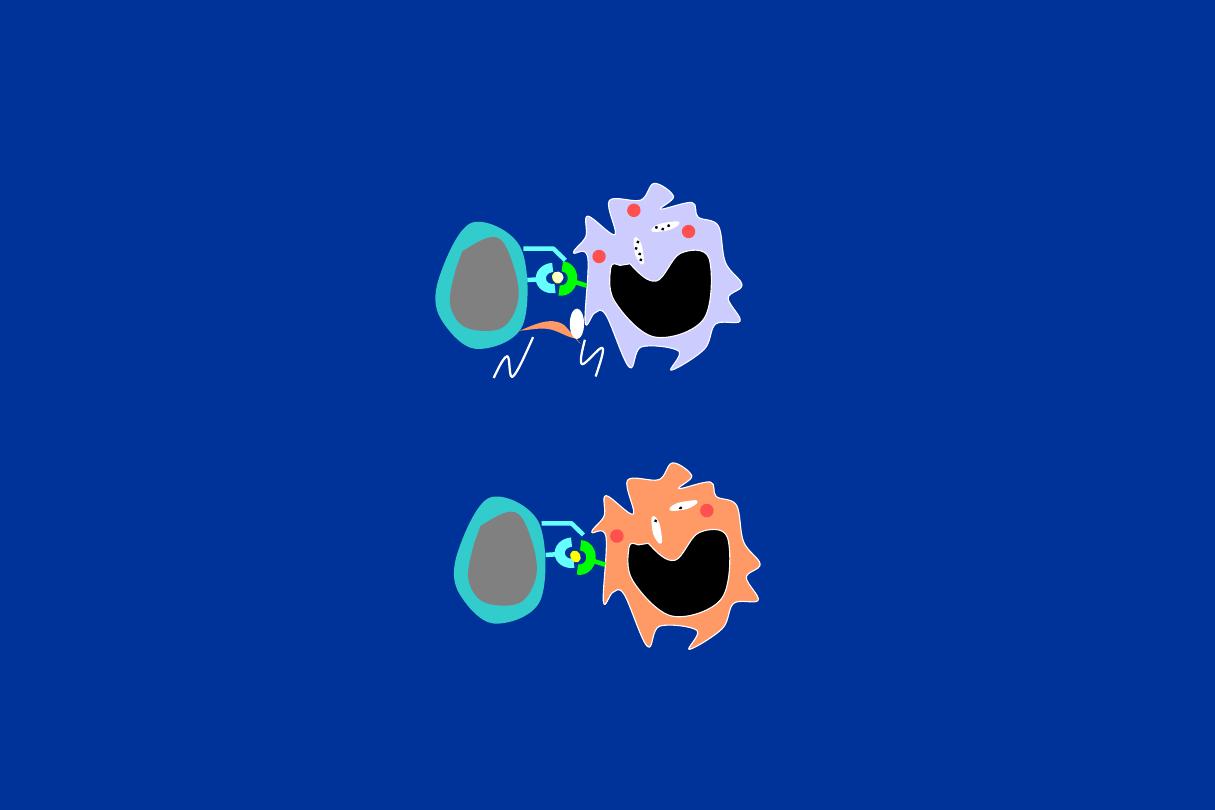
Regulatory T cells
Functionally
Unresponsive T cell
Production of IL-10 or TGF-
Regulatory
T cell
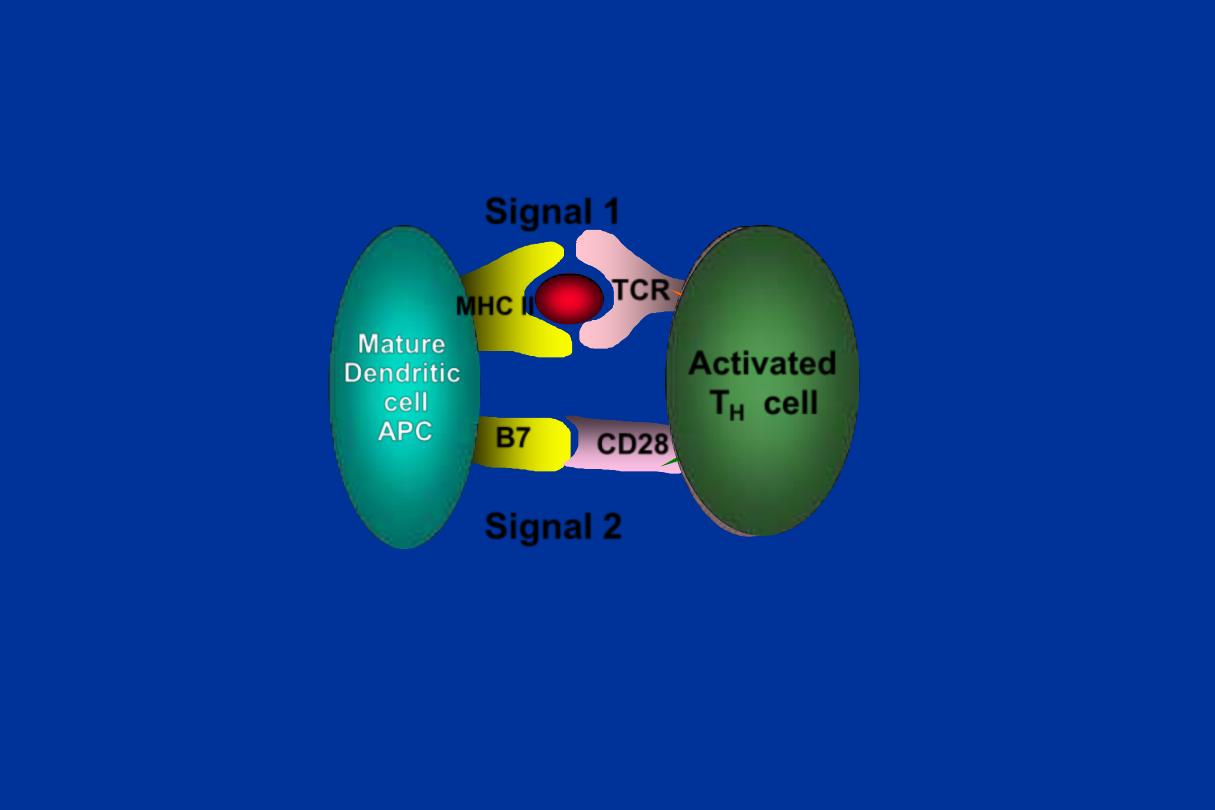
The Two Signal Hypothesis for T-cell Activation
Mature
Dendritic
cell
APC
T
H
cell
CD28
B7
MHC II
TCR
Signal 2
Signal 1
Activated
T
H
cell
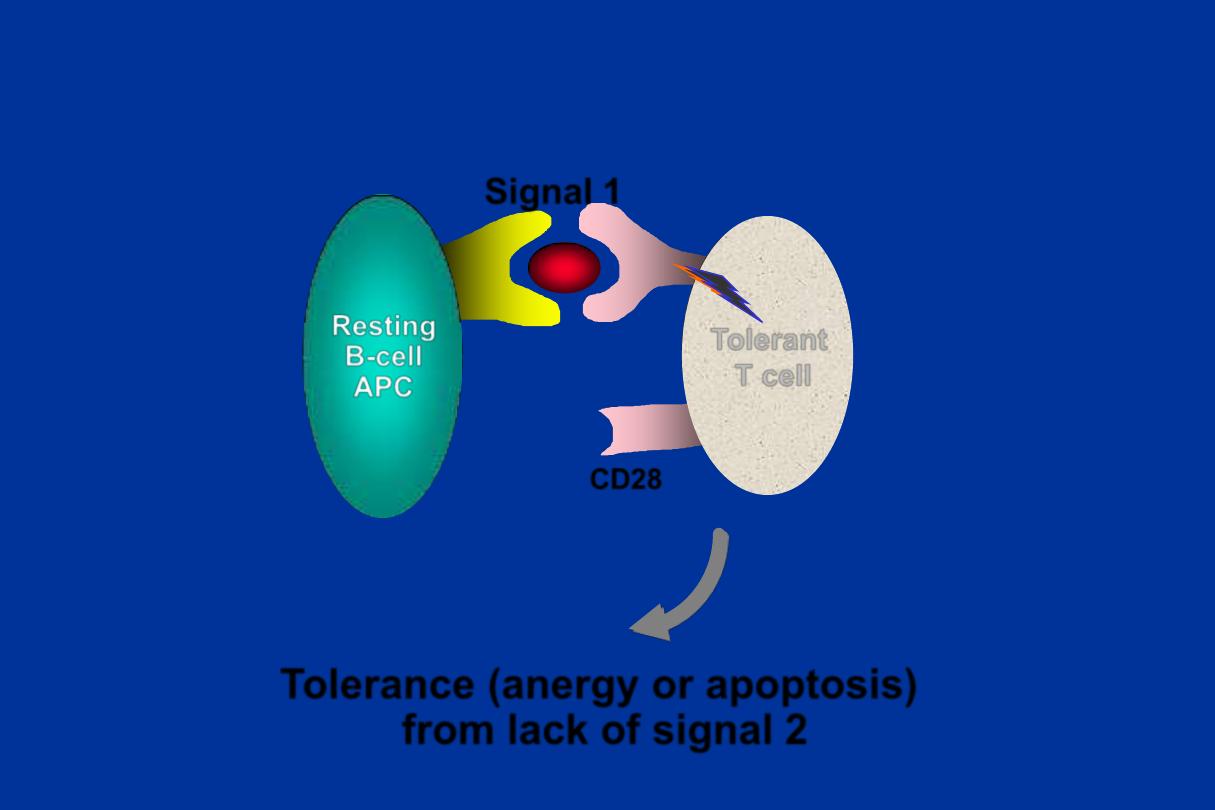
Hypothetical mechanism of tolerance in mature T cells
CD28
Resting
B-cell
APC
T
H0
cell
Tolerance (anergy or apoptosis)
from lack of signal 2
Signal 1
Tolerant
T cell
Regulation by CTLA-4
CTLA4
B7
Functionally
Unresponsive (Anergic) T cell
CTLA4-B7 interaction
Activated T cell
Activated
T cells
Normal
Response
CD28
B7
Proliferation &
differentiation
Summary: Lack of co-stimulation
can lead to tolerance (anergy)
Antigen Recognition
without co-stimulation
Anergy
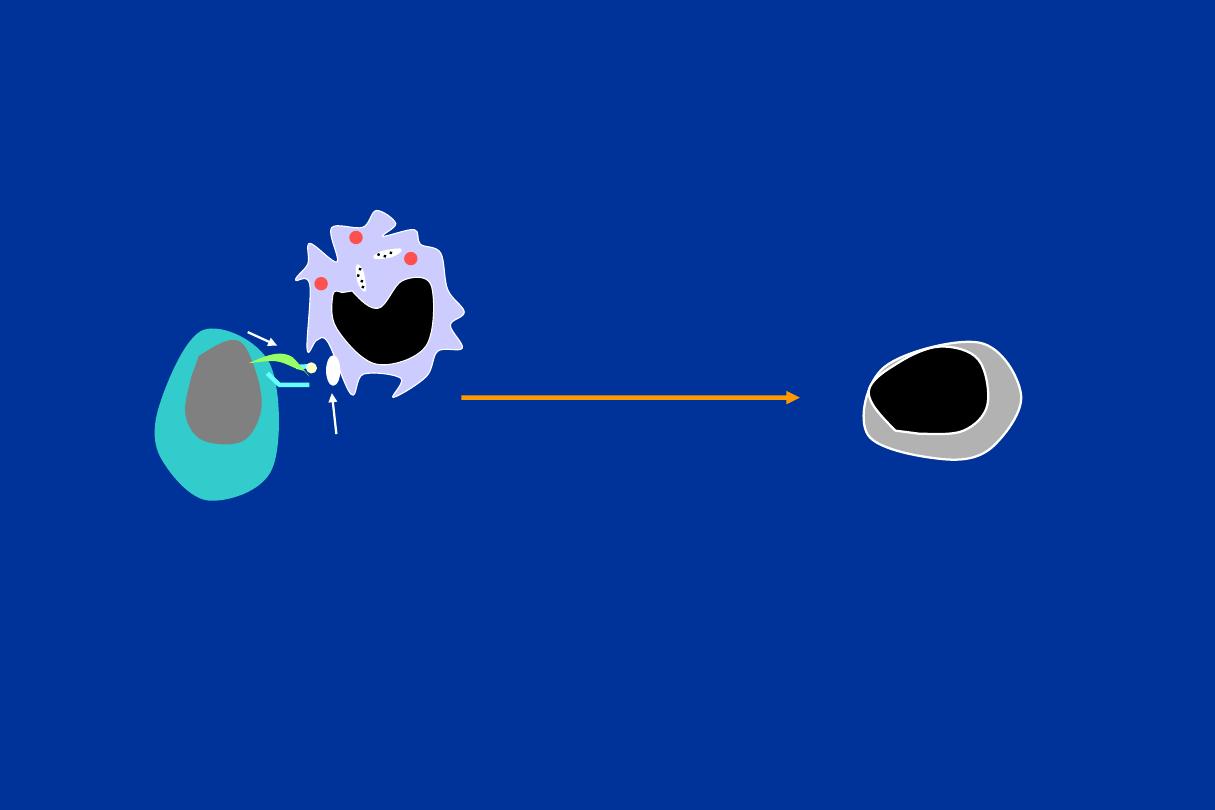
Generation of immune repertoires
Central Tolerance
Peripheral Tolerance
Autoimmune Diseases
Tolerance fails
Wrong environment
(viral infection?)
Wrong genes
or mutations
Bone Marrow
Thymus
Self-reactive lymphocytes
Deleted by negative selection
Leakage of self-reactive
lymphocytes controlled
Tolerance: Establishment and Failure

Autoimmune Diseases
• Immune reaction against self-antigen which
present in own tissues, they are
characterized by tissue damage, disturbed
physiological function, chronicity & usually non
reversible
• Affect female > male
• Usually started at 20-40 years of age

Autoimmune Diseases
Predisposing Factors:
1- Advancing age
2- Hormonal factors (more common in females)
Female: male ratio = 10 : 1
3- Genetic predisposition
4- Environmental factors (infection, drugs, U.V
light, psychological stress, dietary factors)

Mechanisms of Autoimmune
Disease (Loss of self-tolerance)
1- Emergence of sequestered antigens (e.g.,
eye, brain ,thyroid , sperm )
2- Molecular mimicry
–Microbes share epitopes with self-antigens
Ex. Streptococci and rheumatic heart
disease
3- Polyclonal lymphocyte activation
(Endotoxin, EBV , AIDS , CMV)

4- Alteration of normal proteins
•
Procainamide induces SLE
5- Inappropriate expression of class II MHC molecules
•Normally only on APC s
•After viral infection or trauma the released gamma IFN
leads to
expressing class II MHC molecules on some cells like
Pancreatic beta cells ---IDDM or thyroid cells
6- Genetic predisposing (association with MHC gene)
•Ankylosing spondylitis (HLA- B27)
•SLE DR- 2,3
•IDDM DR- 3,4

7-Cytokine dysregulation &Break down
(FAILURE) of suppressor mechanisms
8-Thymus defect (Increasing with age)
9-Hormonal factor ( more in females)
10-Complement deficiency
11-
Idiotype antiidiotype network defect
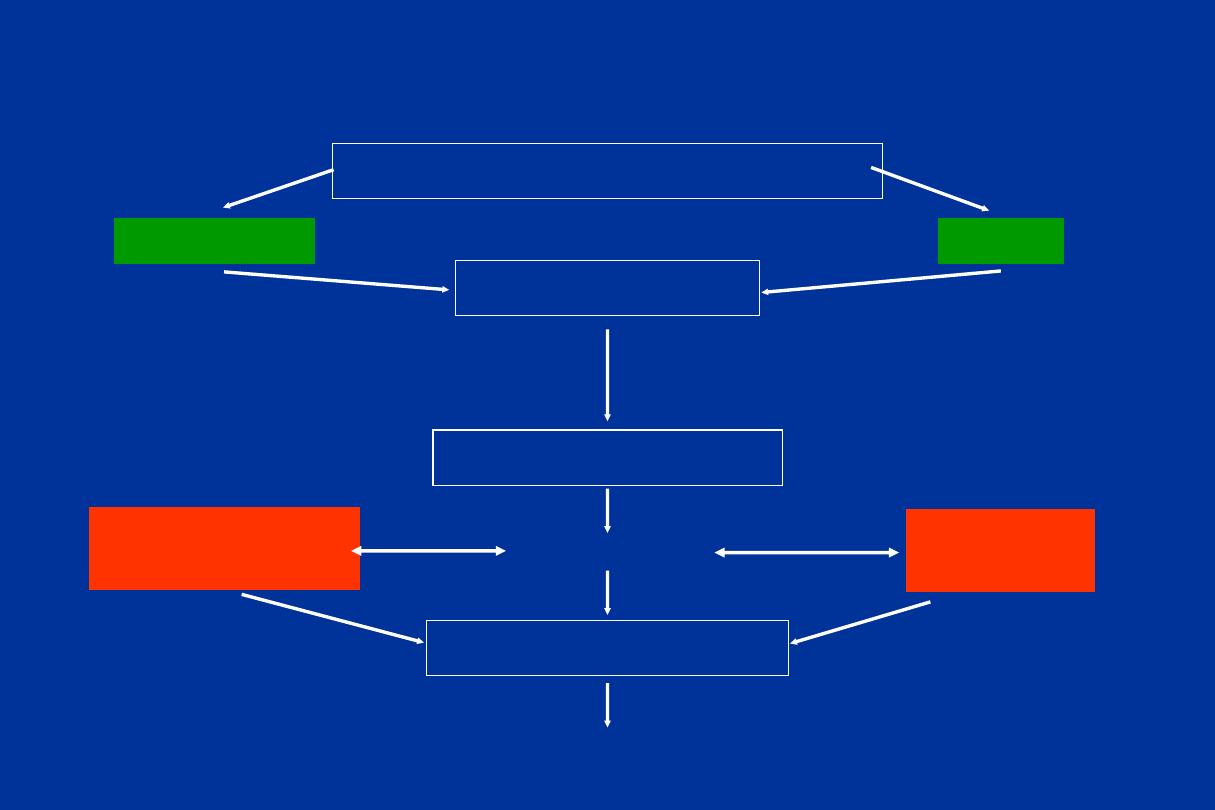
Pathogenesis of autoimmunity
Susceptibility genes
Environmental trigger
(e.g. infections, chemicals
tissue injury)
Failure of
self-tolerance
Activation of
self-reactive
lymphocytes
Immune responses against self tissues
Persistence of functional
self-reactive lymphocytes

-Clinical types of auto immune diseases
Organ specific
Graves’ disease
Myasthenia gravis
Systemic
SLE
-Ab non specific but organ specific as
primary biliary cirrhosis
-Multiple autoimmune diseases can be
occurred in the same patient
• Type II — Antibodies react with cell-surface
antigens in specific organs
Ex.
auto-immune Hemolytic anemia
• Type III (Immune Complex) — IgM and/or IgG
react with soluble cell material, complexes are
deposited, initiate complement activation,
inflammation
Ex. SLE
• Type IV — Mediated by cytotoxic & CD4 + T
cells
Ex. MS
25
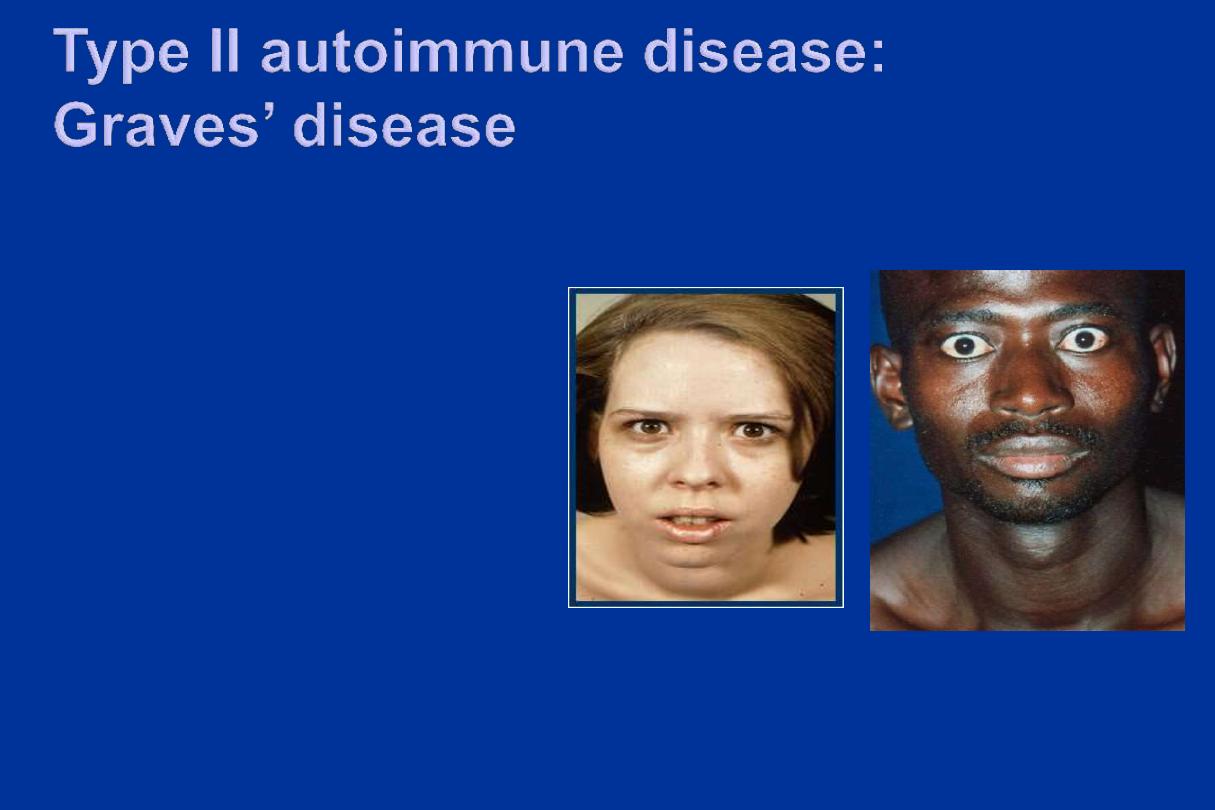
• Stimulating auto-
antibodies against
growth receptors on
thyroid gland
• Cross reactive
autoantigens in the
eyes
• Patients develop
goiter, bulging staring
eyes
26

Systemic Lupus Erythematosus
• Incidence 1:2500
• Female: male 10:1
• 2
nd
/3
rd
decade of life
• Skin, kidney, serosal membranes, joints,
heart
• Many autoantibodies
• Failure to maintain self-tolerance

Anti-Nuclear Antibodies (ANA)
• Abs to DNA
• Abs to histone
• Abs to non-histone proteins bound to RNA
• Abs to nucleolar antigens

Systemic Lupus Erythematosus
• Genetic factors
– 30% concordance in monozygotic twins
– Increased risk in family members
– HLA-DQ & DR locus and SLE
association
– Complement deficiency
• Non-Genetic factors
– Drugs: procainamide, hydralazine
– Sex hormones (estrogens>androgens)\
– UV light
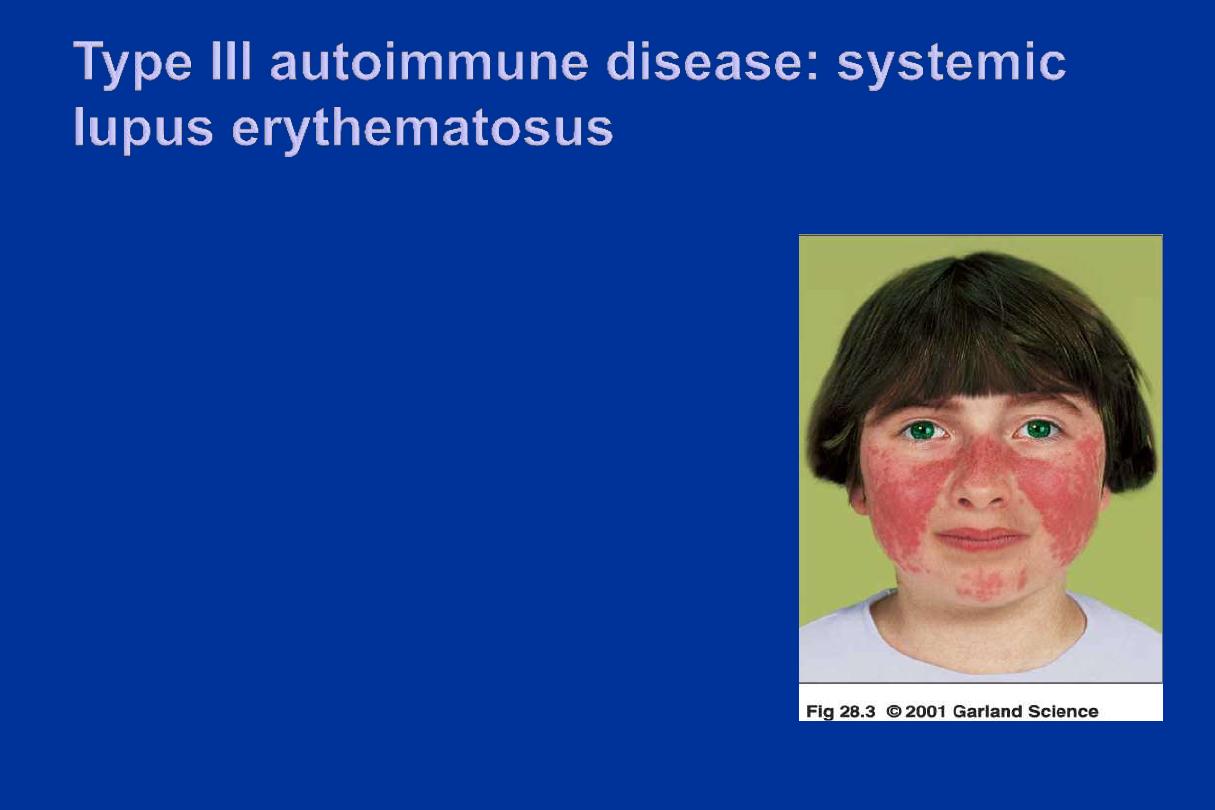
• Auto-antibodies against nuclear
components
• RBC, Platelets, clotting factors
• Immune complexes activate
complement
• Excess complexes are deposited in
small blood vessels
• Local inflammation in skin, joints and
kidneys, multi-organ damage
30
