
IMMUNOLOGY
ا.م.د.هيفاء الحديثي
Transplantation
OBJECTIVES:
1- Define graft rejection and discuss its bases.
2- List and define each class of graft.
3- Determine methods used for Donor-Recipient matching.
- Discuss the classification of rejection.
4
5- Explain the development of Graft versus host disease (GVHD).
6- List the commonly used Immunosuppressive drugs.
_________________________________________________________
Transplantation
Transplantation or grafting of organs and tissues is a common medical
procedure emerged in early 1970s. Although it is life giving, but it carry
the risk of damage and the bulk of damage that occur in graft rejections
can be attributed to expression of cytotoxic T-cells and other killer cells.
The bases for graft rejection:
In general, the genes and receptors in MHC classes I and II are extremely
important in recognizing self and in regulating the immune response. The
pattern of MHC genes can be similar in related siblings, but the more is
that the relationship, the less likely that MHC genes and receptors will be
similar when donor tissue (a graft) displays surface receptors of a
different MHC class, the T-cells of the recipient (called the host) will
recognize its foreignness and they release IL
2
this stimulus amplifies
helper and cytotoxic T-cell specific & the foreign Ags on the donated
cells. The cytotoxic cells bind to grafted tissue and secrete lymphokines
that begin rejection process within 2weeks of transplantation. Late in this
process Abs formed against the graft tissue contribute to immune
damage. Finally the destruction of the vascular supply promoting death of
the grafted tissue.
Classes of grafts:
Grafts are generally classified according the genetic relationship between
the donor and the recipient:
Autograft
tissue transplanted for one site on an individual’s
body to another site or his body skin replacement in burn repair.
Isograft
tissue from an identical twin.
Allografts
the most common type of grafts, are exchanges
between genetically different individuals belonging to the same
species (two human).
Xenograft
is a tissue exchange between individuals of
different species.
Donor-Recipient matching
- ABO matching must be done
ABO incompatibility contraindicate the transplantation, overcome
by removal of anti-A or anti-B isohemagglutinin from recipient.
- HLA matching done routinely, but the clinical significance depend
on the organ to be transplant
In kidney there is correlation between the common HLA and
the survival rate.
In bone marrow, it is very important to avoid (GVHD)
tested
by mixing culture of recipient lymphocyte with lymphocyte
from donor
should react minimally to each other (MLR).
It is not significant for liver transplantation the same for heart,
lung and bowel.
- Screening of the recipient serum for cytotoxic antibodies directed
against the donor lymphocyte (observing the lyses of donor
lymphocytes by the recipient serum plus complement- cross
matching)
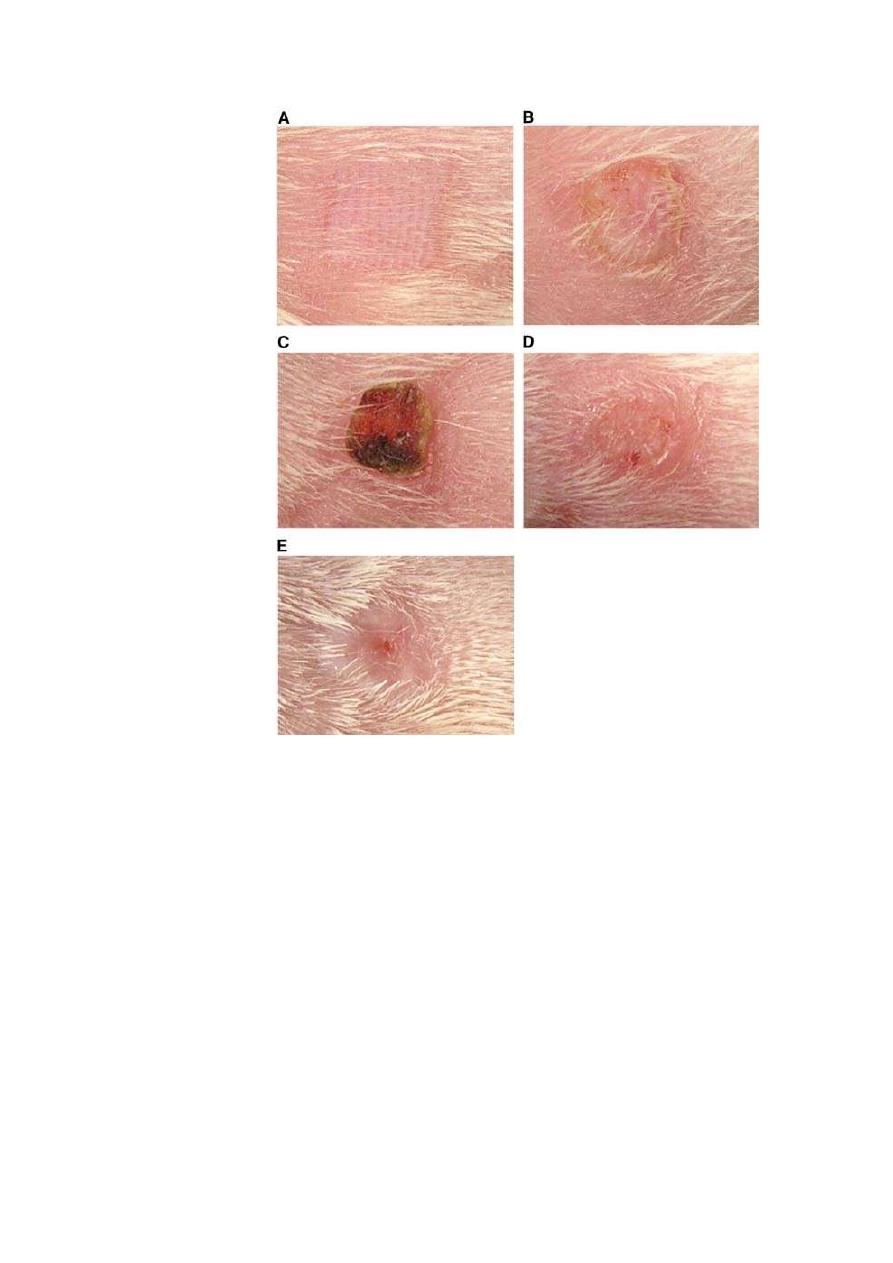
Graft rejection
It is a consequence of an immune response mounted by the recipient
against the graft due to incompatibility. Rejection episodes classified
according to time between transplant and start of episodes:
1. Hyper acute rejection (early rejection)
2. Acute rejection
3. Chronic rejection
Hyperacute rejection: within minutes due to
pre-existing Ab
Activation of complement system
chemotactic attraction
triggering the inflammatory cascades
or by ADCC.
- This is usually irreversible and avoided by proper matching.
- The transplant must be immediately removed.

Acute rejection
- If occur within few days
secondary immune response.
- If occur beyond 1
st
week
primary immune response mediated
by CD8
+
, CD4 & Thl
- Can be reversed by increasing immunosuppressive agents.
Chronic rejection
Insidiously progressive loss of function of grafted organ due to
non-immune (prolonged use of immunosuppresion or due to
vascular endothelial injury).
Poor immune responses against transplanted tissue associated
with fibrosis of internal blood vessels.
Graft versus host disease (GVHD)
In sever ID, the host cannot reject a graft, but graft incompatibility is a
two-way phenomenon. Some grafted tissues (especially bone marrow)
contain indigenous population (passenger lymphocytes) which attack and
destroy recipient’s cells.
The 3 components for GVHD:
- Graft immune competent T-cells.
- Immune compromised recipient.
- The recipient must express Ags foreign to the donor.
GVHD can be reduced by treating the donor tissue with antithymocyte
globulin or monoclonal Ab before grafting to eliminate mature T-cells
from the graft.
Types of transplants
Transplantation surgery has been performed on every major organ
including parts of the brain.

The most frequent transplant operations include skin, heart, kidney,
coronary artery, cornea and bone marrow.
The source of organs and tissues are
- Live donors (kidney, skin, bone, marrow, liver).
- Cadavers (heart, kidney, corneal, and fetal tissues as fetal pancreas
in DM or fetal brain in parkinson disease, and parent liver, lobe of
lung).
Recent advances made it possible to isolate stem cell directly for the
blood of the donors without bone marrow sampling.
Immunosuppressive drugs
Drugs that suppress allograft rejection & prolong immunosuppression,
greatly enhances the recipient’s susceptibility to opportunistic infections
and neoplasms in addition to bone marrow suppression and neutropenia.
- Corticosteroids (Prednisolone)
- Inhibitors of signal transduction (Cyclosporin A)
Which is a polypeptide isolated from fungus, interfere with release of IL
2
and block activation of T-cells it also reduce incidence of fatal infections
what makes this drug so valuable is that it does not inhibit important
lymphoid cells & phagocytes and its adverse is kidney toxicity &
BP.
Used in treatment of DM
-1
& RA.
- Some antimetabolites (Azathioprine) which block DNA synthesis.
- Polyclonal Ab (anti-T-cell Ab) (anti-thymocyte globulin).
- Monoclonal Ab. (anti CD3 [OKT
3
]) (anti-IL
2
receptors) those with
a lesser side effects.
Brought to you by :
Ali Kareem
