
MYCOBACTERIA
Prof. Dr .Mohammad Alfaham
2014
1
2

SPECIES OF MEDICAL IMPORTANCE:
1. Mycobacterium tuberculosis complex
• M. tuberculosis
• M. bovis
• M. africanum
2. Non-tuberculosis mycobacteria (NTM)
a) Atypical mycobacteria
• M. avium-intracellular
• M. marinum
• M. scrofulaceum
b) Non-cultivable
• M. leprae
3

General Characteristics of Mycobacteria:
1. Acid fast straight or slightly curved rods.
2. Non- motile.
3. Non-spore forming.
4. Aerobic (growth is enhanced by the presence of 5-10% CO2.
5. Slow growing bacteria (Average doubling time is 12 hours),
fastidious in nutrition.
6. Resist staining with basic dyes as a result of their high-cell wall
lipid contents.
4

Mycobacterium tuberculosis
Clinical Manifestation:
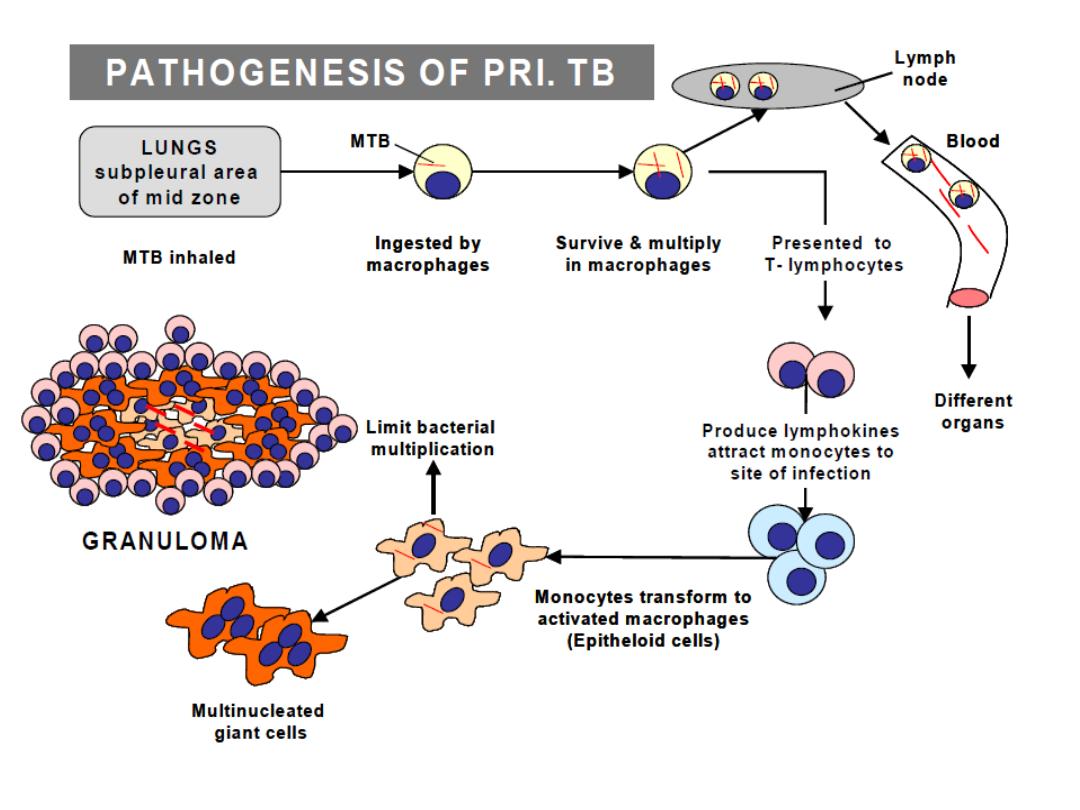
• Organisms is droplets of 1-5 um are inhaled and
reaches alveoli.
• The disease results from establishment and
proliferation of virulent organisms and interaction with
the host.
• The production and development of lesions and their
healing or progression are determined chiefly by the
number of mycobacteria and their multiplication and
the resistance and hypersensitivity of the host.
• Two types of lesion are produced as a result of M.
tuberculosis infection:
5

1. Exudative type:
This consist of an acute inflammatory reaction, with edema fluid,
polymorphonuclear cells, and later, monocytes around the tubercle
bacilli.
This type is particularly seen in lung tissues, where it resembles
bacterial pneumonia.
2. Productive type:
When fully developed, this lesion, a chronic granuloma, consist of
three zones:
A. A central area of large multinucleated giant cells containing M.
tuberculosis.
B. A mid-zone of pale epithelial cells
C. A peripheral zone of fibroblast, lymphocytes and monocytes.
This lesion is called a tubercle.
Septicemia usually occur early in the course of infection and
meningitis is not uncommon.
6
7

Symptoms:TB
• Fever
• Chills
• Sweating
• Night sweats
• Flu-like symptoms
• Gastrointestinal symptoms
• Weight loss
• No appetite
• Weakness
• Fatigue

Specimen:
Fresh sputum, gastric aspirate or washing, urine, pleural fluid,
cerebrospinal fluid, joint fluid, biopsy materials.
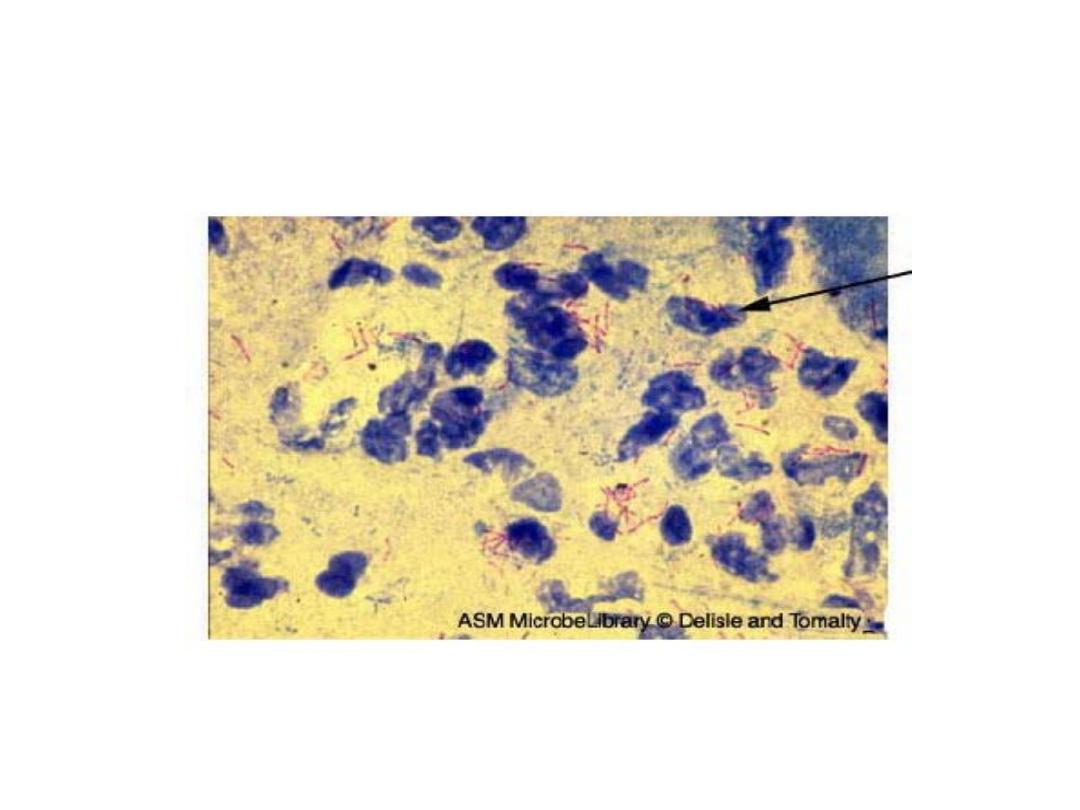
Stained smears:
Sputum or sediments from other body fluids is stained for acid
fast bacilli by Ziel- Neelsen technique.
Culture:
Sputum must undergo concentration procedures prior culturing:
Procedures:
1. Mix an equal volume of sputum with 4% sodium hydroxide
containing 0.004% phenol red in 100 ml tube containing glass
beads. Homogenize by shaking for few minutes.
2. Centrifuge at 3000 rpm for 20-30 minutes.
3. Decant the supernatant fluid into a disinfectant, leaving little
fluid to resuspend the sediments. Add one drop of phenol red
indicator.
9

4. Using sterile pipette, add 2N HCl drop by drop to a definite
yellow end point.
5. Inoculate the sediments to egg media. Two Lowenstein-Jensen
slopes.
6. Prepare a smear from sedimented materials and stain with
Acid-Fast staining procedures.
NB:
Incubation of the un inoculated media is continued for up to
8 weeks.
Increased CO2 tension enhances growth.
NB:
Colony morphology: Bread-crumbs appearance.
Lowenstein Jensen Medium – growth in 4-6 weeks
Middlebrook Agar (7H11) – growth 2-3 weeks
10

Biochemical Identification:
1. Niacin test:
Only M. tuberculosis and M. simiae are positive for this test
PROCEDURES:
1. Add one ml of sterile distilled water to a 3-4 weeks old culture
on L.J medium and hold the tube so that the water covers the
medium around the colonies.
2. After 15 minutes, remove 0.5 ml of the liquid containing
extracted niacin, and transfer it to a clean, screw-capped test
tube.
3. Add 0.5 ml of 4% aniline solution and 0.5 ml of 10% cyanogen
bromide.
4. If yellow color appears immediately, niacin is present.
NB:
To differentiate M. tuberculosis from M. simiae. M.simiae
produces pigment while M. tuberculosis does not.
11
Other Biochemical Tests:
1. Nitrate reduction test +ve
2. Urease test + ve
3. Tellurite reduction test -ve
4. Sodium chloride tolerance test -ve
5. Pigment production test -ve
6. Catalase test +ve
7. Arylsulfate test -ve
8. Growth on MacConkey agar -ve
SEROLOGICAL TEST:
1. Skin test: Tuberculin test:
An intradermal injection composed
of one of these extracts:
1. Old tuberculin: Crude extract from the filtrate of M.
tuberculosis broth culture. Also known as Tuberculin-Koch.
2. Purified Protein Derivatives: (PPD): Purified extract.
12
-
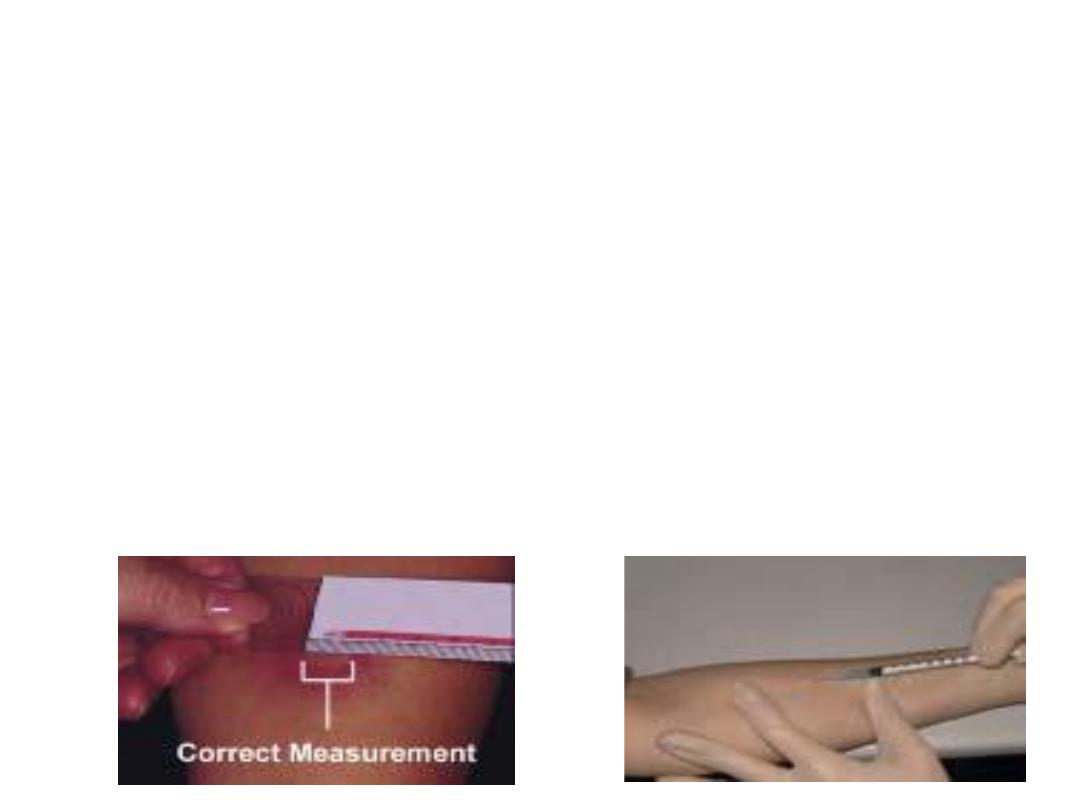
TUBERCULIN (MONTOUX) TEST
Purified Protein Derivative (PPD) from tubercle bacilli
(standardized) in Tuberculin Units - TU) is injected intradermaly
DOSE
5 TU is usual dose – if test negative; increase dose to 250 TU
POSITIVE TEST
The test is read after 48 – 72 hours.
Induration of ≥ 10 mm with erythema.
Induration of 5-9 mm – low level sensitization with tubercle
bacilli or cross reacting mycobacteria.
In AIDS patients: 5 mm induration – positive test.
13
INTERPRETATION OF TUBERCULIN TEST
Positive Test
• Active disease
• Person infected by M. tuberculosis at sometime in life
• Person infected with strongly cross reacting other mycobacteria
• Previous vaccination with BCG
• Child < 5 years if not vaccinated: active disease.
Negative Test
• No induration or < 5 mm
• In healthy individual – not infected with MTB
• Pre-hypersensitivity stage of primary infection
False negative test
• Early TB (test becomes positive after 4-6 weeks of infection)
• Immunosuppression (AIDS).
• Steroid therapy
14

Treatment:
Because M. tuberculosis infections are hard to treat and only few
antibiotics has activity against it, and because of the fear of
emerging of resistant strains, tuberculosis is treated with 2 or 3
antibiotics given as combined therapy.
Active antibiotics against M. tuberculosis include:
1
. Isonizide (INH) 2. Rifamycin
3. Streptomycin 4. Ethambutol
5. Para-aminosalicylic acid PAS 6. Cycloserine
7. Pyrazinamide 8. Viomycin
Treatment for complete recovery may take as long as one year. The
shortest term may be of 6 months with the administration of
combined drugs (Isonizid, rifamycin, streptomycin).
15

ATYPICAL MYCOBACTERIA
•M. avium – interacellulare complex
•Worldwide distribution
•Source – natural water
•Diseases TB in birds
Cervical lymphadenitis in children
Disseminated TB in AIDS patients
DIFFERENCES OF ATYPICAL FROM TYPICAL MYCOBACTERIA
•Colonial morphology
•Niacin test – negative
•Relatively more resistant to anti-TB drugs
•Less acid fastness
•Diseases less invasive
16
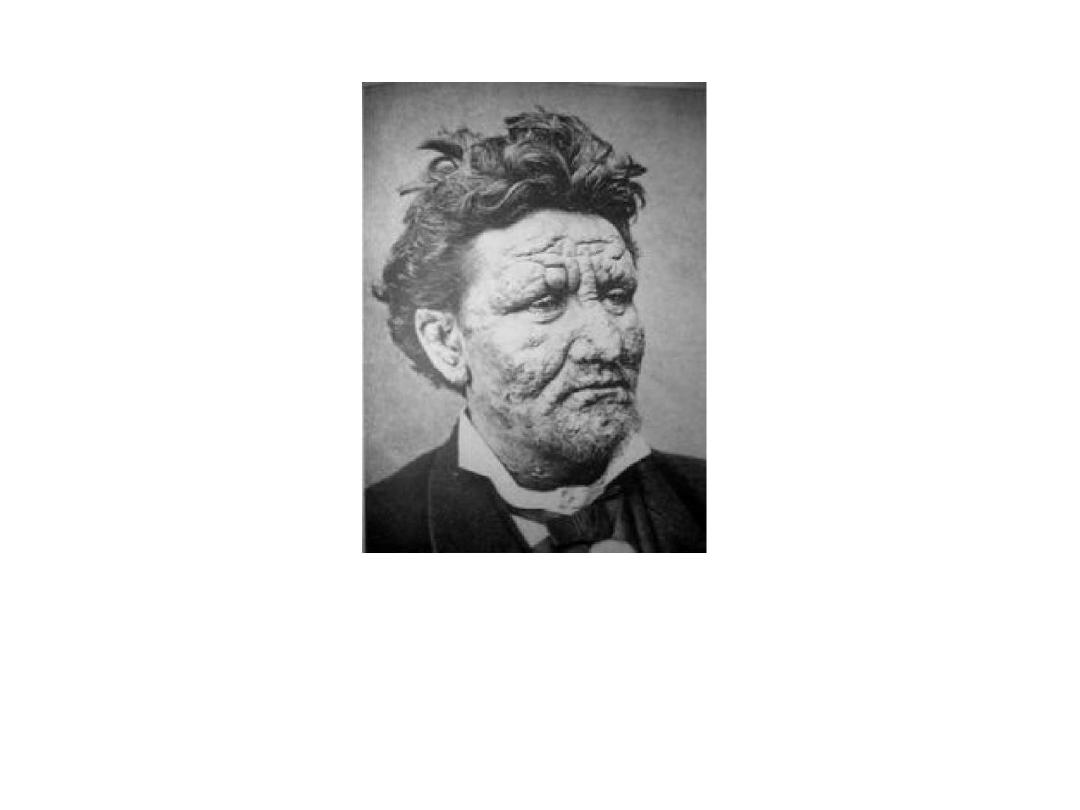
Mycobacterium leprae Leprosy
General Characteristics:
• Typical acid fast bacilli, singly or in parallel bundles.
•Regularly found in smears or scrapings from skin or mucus
membrane in lepromatous leprosy.
•The organism have not been grown on artificial media.
Clinical manifestation:
•The lesions involve the cooler tissue of the body, skin,
superficial nerves, nose, pharynx.
•The skin lesions may occur as pale, anesthetic 1-10 cm in
diameter.
•Neurologic disturbances are manifested by nerve infiltration
and thickening
.
17

The disease is divided into two distinct types:
1. Lepromatous leprosy:
The course is progressive, with nodular skin lesions; slow,
symmetric nerve involvement, abundant acid-fast bacilli in the skin
lesion; continuous bacteremia and negative skin test (lepromin
test).
2. Tuberculoid leprosy:
The course is non-progressive with macular skin lesions,
severe asymmetric nerve involvement of sudden onset with few
bacilli present in the lesion.
Diagnosis:
Scrapping with a scalpel blade from skin, nasal mucosa, or from a
biopsy of ear lobe skin are smeared on a slide and stained by Zeil-
Neelsen technique, and the demonstration of typical acid fast
bacilli.
Treatment: C
ombined therapy of dapsone, rifamycin & clofazimine
18

19
20
