
Francisella tularensis
. Microbiology
Prof.Dr. mohammad alfaham
2014

Characteristics of the Organism:
1. Gram-negative rods “Shows variable shapes ranging from
coccobacilli, to cocci”.
2. Strict aerobe.
3. Requires enriched medium for growth Cystine-Glucose-
Blood Agar “CGBA”
4. Non-motile.
5. Remain viable for long periods in water, soil......etc.
6. Highly infectious. Specimen and cultures must be handled
with great care.
Gram stain Poorly staining, tiny Gram-negative coccobacilli
Clinical Manifestation:
Tularemia in human vary according to:
1. Route of infection
2. The infecting dose
3. The type of organism (A or B strain)
The disease may be transmitted through the skin and mucus
membrane including the conjuctiva through the bite of infective
ticks.
Transmission may also occur through the respiratory route or
gastrointestinal tract through ingesting contaminated meat of
infected animals.
l
THE ULCEROGLANDULAR:
The most common, with slowly healing ulcer at the site of
entry and regional lymph nodes involvement is observed.
This infection results from injury while handling infected animal
carcasses or from the bite of a bloodsucking arthropod such as
ticks and flies.
OCULOGLANDULAR:
Can result from rubbing contaminated materials into the eye.
Conjuctivitis occur and regional lymph node may be enlarged
and suppurate.
THE PULMONARY OR PNEUMONIC:
Can result from inhaling infectious aerosols or dust. Pneumonia
and pleuritis are associated with severe tularemia.

TYPHOIDAL, GIT & OROPHARYNGEAL INFECTION:
Results from the ingestion of contaminated food. Symptoms begin
as flu-like associated with vomiting, headache, fever and
prostration. Diarrhea usually accompany these symptoms.
Subspecies of F. tularnsis
1. F. tularensis A :
More virulent than B. It is also referred to as
tick-deerfly-sheep type and occurs naturally in North America.
Fatality rate among untreated patient is 5-7%.
2. F. tularensis B:
It is referred to as the Beaver-Muskrat water
type. It produces mild (Subclinical) infection in human. It have
frequently been isolated from natural running water.
NB: To differentiate between the two, 1% glycerol is added to
Cystin-glucose-heart
agar
without
blood
and
enough
bromothymol blue indicator.
TYPE A: Turns the medium yellow (acid)
TYPE B:
Turns the medium dark blue (alkaline)

Collection of specimen:
1. Exudates from cutaneous or mucosal ulcers or lymph node
aspirate.
2. Blood or sputum for pulmonary infection
3. Blood specimen for serologic for measuring antibody titer
4. Specimens (biopsy) from enlarged liver or spleen.,
Diagnostic procedures:
A. Microscopic appearance:
- Short gram-negative non-motile bacilli
- Morphologically may be similar to Yersinia species and shows
bipolar reaction.
B. Cultural Characteristics
-On CGBA: colonies resemble a medium sized mercury droplets
surrounded by a small zone of partial hemolysis.
- Colonies often requires 2-4 days at 37 oC to reach a diameter
of 1 mm.

C. Inoculation of the specimen:
•Primary isolation from specimen may be difficult even though
it may contain large numbers of F. tularensis.
•Contaminating organisms can easily overgrow cultures or
produce large amounts of acids to prevent the growth of F.
tularensis on the enriched media needed for isolation.
•Cystine glucose blood agar is the medium of choice. It is
commercially available or can be prepared in the laboratory.
D. Biochemical Identification:
•Biochemical tests are of a little value in identifying the
organism.
1. Tube agglutination test:
2. The slide agglutination method:

3. The precipitin test:
Can be used to measure antibody titer and demonstrate the
presence of antigen. This test is useful for grossly contaminated,
even decayed specimen such as liver and
spleen of naturally infected, field-collected animal specimen,
4. Hemagglutination and complement fixation tests are of
limited use.
5. Skin test have been used for prevalence of past infection in
large population.
Treatment and antibiotic sensitivity:
Streptomycin, Chloramphenicol and tetracycline are used to
eradicate this organism.

Outbreaks
Chest X-ray of patient demonstrating complete whiteout of
the left lung

Tularemia Lesion
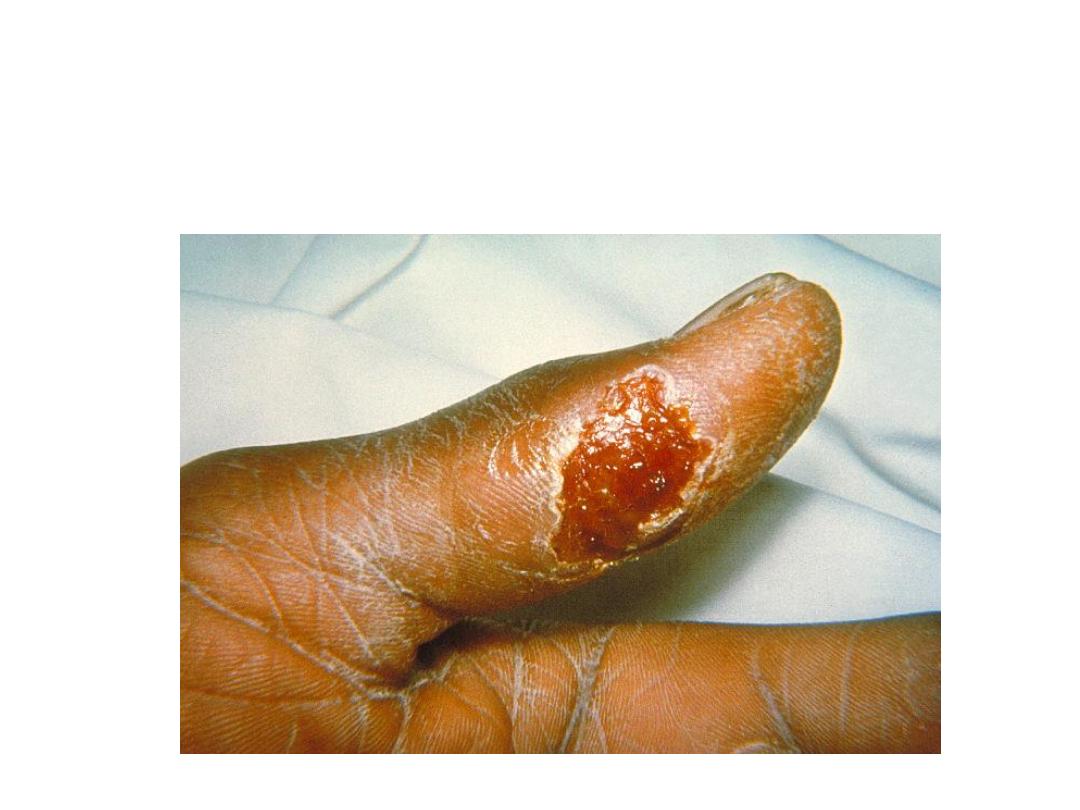
Skin Ulcer of Tularemia

END of LECTURE
